Causes of extrasystole during VSD
Increased sensitivity
Arrhythmia, similar to that which occurs with VSD, is characteristic of absolutely all people. Everyone misses a beat from time to time. People just don't notice it. Neurotics, on the other hand, notice all, even the most insignificant, changes in their physical condition. Therefore, the presence of extrasystoles is very clearly monitored. They are afraid of them. They begin to constantly think about them, thereby increasing both their anxiety and the number of missed shots.
Hyperventilation
Hyperventilation is one of the most common physiological manifestations of anxiety.
In this condition, there is a lack of carbon dioxide in the blood, which causes the blood to flow more slowly. To speed up blood flow, the heart begins to contract faster. This can lead not only to tachycardia, but also to an increase in the normal number of skipped beats.
Reaction to adrenaline
VSD is a physical manifestation of chronic anxiety. And anxiety is always a release of additional adrenaline.
The heart's reaction to this additional amount may be expressed in an increase in the number of extrasystoles.
Biliary dyskinesia
Various problems in the abdominal area, primarily problems with the gallbladder, can negatively affect the functioning of the heart. In particular, increase the number of extrasystoles.
Since people suffering from neurotic disorders very often have biliary dyskinesia, which is also of a nervous nature, they may also experience additional extrasystoles.
Signs of improper therapy
Are the symptoms of the disease disappearing too slowly or not at all? This is a sign that the therapy is not being carried out correctly. The slow recovery may be due to weak drugs or an incorrectly chosen method. The doctor will understand how to change the course, but the main thing for the patient is to notice the deviation in time. The main symptoms of improper treatment:
- The nervous agitation has subsided thanks to antidepressants, but the patient still suffers from attacks or isolated manifestations of arrhythmia.
- There is lethargy, problems with body control and intelligence, and the patient does not take a sedative.
- Cardiograms show the simultaneous arrival of an impulse in the ventricles and atria, while a “burst” is noticeable - an extraordinary blow.
- The hormones that trigger the development of the disease are still outside the normal range (increased).
Occasionally, a period of remission can be confused with a simple period of time when the disease is not expressed. This error is typical for patients who suffer from attacks very rarely. Once they start taking medication, they may decide that the disease has subsided, but the disease will still be active. And in some cases, patients stop noticing minor deviations from the norm and do not feel single premature contractions. That is why during therapy it is very important to be observed by a doctor who will regularly do a cardiogram to determine progress.
Psychogenic attacks can be easily cured if you consult a doctor in time and follow all the recommendations of a cardiologist. A patient with such a disease should be especially attentive to himself, since failures with mild severity can be confused with ordinary signs of fatigue, poisoning or other minor ailment. The symptoms described above will help you distinguish extrasystole from similar heart ailments and promptly seek medical help. Under no circumstances should you delay visiting a therapist if you have persistent problems caused by systematic stress and nervous problems. This can lead to early death or severe disability.
Supraventricular extrasystole and its treatment
Extrasystole is a condition related to heart rhythm disturbances, or arrhythmias, which are expressed by extraordinary contractions of the heart or its parts. Depending on the location of the source of excitation, it can be ventricular, atrial, atrioventricular.
Supraventricular extrasystole, or supraventricular, is characterized by the fact that premature impulses arise in ectopic foci located in the upper parts of the heart (atria) or in the septum between the ventricles and atria, which is called the antiventricular. As a result, incomplete additional contractions of the heart occur.
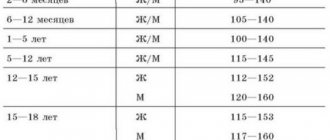
Frequency per minute
- single (up to five extraordinary reductions),
- multiple (more than five),
- group (several extrasystoles in a row),
- doubles (two in a row).
By time of appearance
- early (with atrial contraction),
- average (between the time of contraction of the atria and ventricles),
- late (with contraction of the ventricles or with complete relaxation of the heart).
By order
- ordered (alternating normal contractions with extrasystoles),
- disordered (there is no pattern).
Signs
With supraventricular extrasystole there are often no complaints. In some cases, the disease causes the following symptoms:
- lack of air, shortness of breath;
- interruptions in the work of the heart: a feeling of “reversals” of the heart or beats out of rhythm;
- dizziness;
- general weakness.
In children, supraventricular extrasystole most often occurs without any symptoms. Complaints usually come from older children. The child may experience weakness, irritability, fatigue, dizziness, and a feeling of heart failure.
Treatment
If there are no organic heart diseases and the patient has no complaints, then specific treatment for supraventricular extrasystole, as a rule, is not carried out. Therapy is usually indicated when symptoms are present and poorly tolerated.
You can also read: Permanent form of atrial fibrillation
First of all, the doctor assesses the number of extraordinary heart contractions per day. A single extrasystole does not pose a health hazard. Then you need to make sure that there are no organic heart diseases. If the patient has subjective complaints and does not tolerate them well, sedatives may be used.
The doctor should evaluate the advisability of taking antiarrhythmic drugs. The fact is that they have many side effects, and therefore the treatment can become more dangerous than the disease itself. Rare supraventricular extrasystole (several tens or hundreds of contractions per day) does not require taking such serious medications.
Thus, in the absence of complaints and diseases, the patient is recommended:
- Eat right, that is, exclude preservatives, fatty, fried, spicy, hot foods. Eat more plant foods rich in fiber.
- Eliminate bad habits (alcohol, smoking, energy drinks).
- Avoid stress and exercise in moderation.
- Ensure restful and sufficient sleep.
- Spend more time outside.
In the presence of heart disease and severe symptoms, conservative treatment with glycosides and antiarrhythmic drugs is indicated, which are selected strictly individually.
If medications do not help and the patient does not tolerate extrasystole, surgical treatment is performed.
This may be an open operation in which ectopic lesions are removed. As a rule, it is performed when intervention for heart valve replacement is required.
Another type of surgical treatment is radiofrequency ablation of lesions using a catheter, which is inserted into a large blood vessel, an electrode is passed through it and the area where the pathological impulse occurs is cauterized.
Possible complications
There is an opinion that frequent supraventricular extrasystole, characterized by a large number of extraordinary contractions of the heart, can lead to heart failure, changes in atrial configurations, and atrial fibrillation after several years. According to some reports, convincing evidence on this matter has not yet been received. In rare cases, supraventricular tachycardia may develop.
Forecast
Supraventricular extrasystole usually indicates a good prognosis. It does not lead to sudden death, like ventricular death, in which such a risk exists in the presence of organic heart disease.
Treatment
Some patients are interested in whether they need to be afraid of extrasystole that occurs with vascular dystonia if an attack occurs on the street or in public transport. A person taken by surprise is frightened by the appearance of an extrasystole, and he complains of such unpleasant sensations as:
- pause in heartbeat;
- swipe;
- irregular rhythm.
The patient pays attention to the heart rate, duration of the heartbeat, and the appearance of symptoms of vascular insufficiency.
If a person's pulse is at least 50 beats per minute, β-blockers are prescribed for treatment. To eliminate palpitations with the correct rhythm and single extrasystoles, it is recommended to massage the carotid sinus and immerse the face in cold water.
Patients with extrasystole are prescribed:
- Verapamil;
- Diltiazem;
- Metoprolol.
An ECG is used during drug administration.
Antiarrhythmic drugs are prescribed by a doctor in the absence of severe heart disease. If a patient is diagnosed with vascular insufficiency, Amiodarone, which does not cause arrhythmia, is included in the treatment regimen.
Some patients may be diagnosed with inadequate sinus tachycardia, the appearance of extrasystoles at rest, outside of physical activity or emotional stress. In this case, the patient is prescribed symptomatic therapy with β-blockers.
Extrasystoles can occur during pregnancy. In the absence of heart disease, treatment is not carried out. A woman is prescribed antiarrhythmic drugs if she does not tolerate the symptoms of tachycardia or if hemodynamic disturbances occur. Preference is given to Adenosine. If the effect cannot be achieved, the patient is given intravenous Propranolol or Metoprolol. The popular drug Verapamil is not recommended for treatment, because it has a negative effect on the fetus.
To prevent extrasystole, a woman is recommended Digoxin or β-blockers. In the 1st trimester of pregnancy, Metoprolol and Anaprilin are not prescribed. In this case, the doctor treats with cardioselective β-blockers.
Symptoms
Extrasystoles during VSD are associated with a nervous disorder and manifest themselves:
- in an anxious state;
- irritability:
- increased excitability;
- panic attacks;
- shortness of breath and lack of air;
- general weakness and dizziness.
If, during VSD, patients have bouts of fever often followed by chills, then in combination with an abnormal heart rhythm, these phenomena are further aggravated, exhausting the body.
A common symptom that develops against the background of extrasystoles in dystonia is insomnia. It occurs against a background of anxiety, and together with nightly interruptions in heart rate, leads to panic attacks. In this case, sedatives are used to relieve this condition.
Arrhythmia with VSD is accompanied by both tachycardia (rapid heart rate) and bradycardia (slow heart rate). Extrasystole varies according to the area in which the source of excitation is located: ventricular, atrioventricular, atrial.
Extrasystoles are rare - up to 5 times/min; medium – up to 15 times/min; frequent – more than 15 times. In addition, they also differ in rhythm, when extrasystoles alternate with normal heart beats (bigemia), there are two heartbeats per extrasystole (trigemia) and it rarely happens that an extrasystole follows every third beat
This is important because when prescribing treatment, the area of localization and the shape of the systole are taken into account
Interruptions of the heart rhythm during VSD are functional in nature, therefore, not cardiac drugs, but sedatives and sedatives are used for treatment. But this is only true if the heart is completely healthy. If deviations in the cardiovascular system are observed, then complex therapy is carried out to support the heart and normalize the nervous system.
Possible preventative measures
To prevent such an illness from occurring, pay closer attention to your health. Because VSD disrupts not only blood circulation, but also the work of various organs, and the heart is no exception.
Violation of heart contractions occurs due to severe or prolonged nervous tension, anxiety and frequent sleepless nights. Patients diagnosed with VSD are more likely to be attacked by panic attacks, fears and various stresses, because their nervous system is not as strong as others.
Very often, after the end of therapeutic treatment, the patient may experience repeated attacks of extrasystole. To prevent this from happening, you should follow these fairly simple rules:
- Repeat the course of physiotherapeutic procedures regularly.
- Do therapeutic exercises.
- Maintain an active lifestyle.
- Balance your daily menu.
- Take walks in the fresh air.
- Maintain a work/rest schedule.
- Do exercises regularly to normalize breathing.
In addition, you need to give up all bad habits. You also don’t need to drink a lot of coffee and strong tea and eat fatty and fried foods.
Features of extrasystole in dystonia

Extrasystoles accompanying VSD are predominantly episodic. As a rule, they appear in people with a healthy heart. The main sign of an extraordinary contraction is the appearance of a sharp “failure” in the chest, and then a jolt, sudden weakness.
Doctors believe that several dozen extrasystoles per day during exacerbation of VSD are normal. But the frequency also depends on the influence of external factors. Hot weather and overeating increase the autonomic reaction of the heart.
The peak appearance of the first signs of VSD occurs during periods of increased hormonal activity:
- adolescence in adolescents;
- pregnancy;
- the onset of menopause in women.
Symptoms of extrasystole
This disease may be accompanied by a delay in the functioning of the ventricles, causing their accelerated contraction. By the way, the patient may feel rhythmic tremors in the chest. He can notice inversions or somersaults, feel the gaps between pulsations. People generally describe functional arrhythmia as a feeling of increased anxiety, weakness, lack of oxygen, and increased sweating.
Group extrasystoles can turn into coronary arrhythmia, causing the development of paroxysmal ventricular tachycardia, and with pericardial tachycardia - contraction of the atrium. The disease can also develop into atrial fibrillation, especially if the patient was previously diagnosed with pericardial node overload or dilatation.
Neither extrasystole nor VSD detected in a person poses a real threat to the patient. But, undoubtedly, such conditions will significantly reduce the quality of normal life. Extrasystole manifests itself:
- increased sweating;
- general weakness;
- inability to breathe completely;
- pallor of the limbs, skin of the body and face;
- anxiety;
- fainting as a result of developed oxygen starvation of brain cells, as well as a reduced amount of blood that is ejected by the heart.
Complications and prognosis
It was mentioned above in the article that the disease is not life-threatening. Therefore, patients have no particular cause for concern. However, this does not mean that you can not take care of your own health at all. If you do not take any measures to get rid of extrasystole, then in the future this is fraught with the development of such unpleasant diseases as paroxysmal tachycardia, atrial flutter and atrial fibrillation.
But this is not the only danger of this condition. After all, it can provoke the development of circulatory disorders . And if such diseases are discovered in you over time, you will have to spend a lot of time in the clinic to be cured. That is why it is recommended not to delay treatment and immediately contact the clinic for help as soon as signs of developing extrasystole are noticed.
Extrasystoles are cardiac companions of VSD
Extraordinary contraction of the heart muscle (extrasystole) is a subtype of arrhythmias that are harmless if they are born in the sinus node and do not occur frequently.
Extrasystole often appears for no apparent reason, unexpectedly. People suffering from VSD often encounter its manifestations after:
- intense physical activity or during periods of rest;
- drinking drinks containing large doses of caffeine;
- stressful situations, emotional stress.
The physiological reason is the appearance in the heart of an additional source of excitation, in which electrical impulses are generated. They cause extrasystoles, “wedging” between the impulses emanating from the sinus node.
Due to the extraordinary contraction, the “resting” phase of the heart muscle, diastole, decreases. The chambers of the heart do not have time to fill with enough blood. This can negatively affect the oxygen saturation of the body, which is undesirable in case of vegetative-vascular dystonia.
It has been noted that the shorter the time interval between normal systole and extraordinary systole, the lower the volume of cardiac output. Frequent extrasystoles lead to a decrease in cardiac output.
Symptoms and diagnosis
Patients suffering from a disorder of the autonomic nervous system consult a doctor with the following symptoms:
- With ventricular extrasystoles, the blows to the chest from the inside are strong, they are interspersed with long pauses. The patient experiences either cold sweat or fever. From the fear of death, numbness and panic sets in, because a comfortable position cannot be found. My heart jumps out of my chest.
- With supraventricular failure, increased heartbeat occurs in the supine position. It either freezes or gives out more shocks.
- Common symptoms are dizziness, lack of air and difficulty breathing, numbness of the limbs, and general weakness.
All these signs of tachycardia and bradycardia do not pose a risk of sudden death, since VSD is not associated with organic damage to the heart. Extrasystoles in dystonics are called functional, but diagnostics should be carried out.
It is important to determine what triggered the attack in order to choose treatment tactics and avoid negative consequences:
- cardioneurosis, which can occur in panicky people;
- sleep disorders that aggravate the health status of the patient with VSD;
- tissue hypoxia due to decreased cardiac output and insufficient oxygen supply to the entire body.
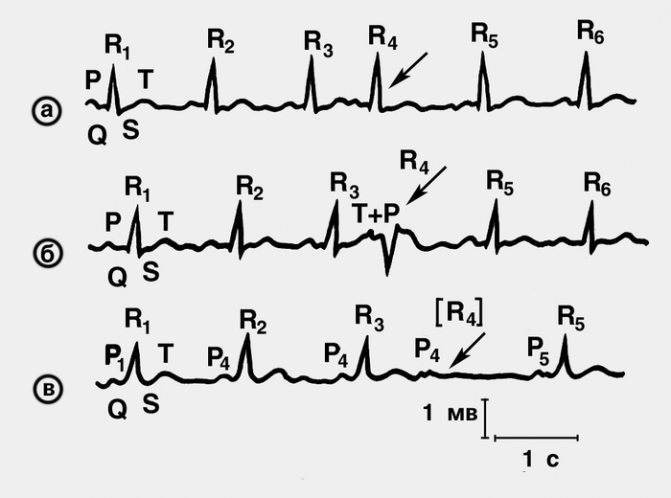
An objective diagnostic method is an instrumental examination of the patient - an ECG, then an echocardiogram, MRI, etc. are prescribed. A cardiogram will show the presence and location of extrasystoles; with the help of an ECG, the beat frequency, tachycardia, atrial fibrillation, and other heart diseases can be determined. The correct rhythm is determined by the duration of the intervals, the nature and size of the teeth.

During the diagnosis, the patient lies on the couch, undressed to the waist, the specialist attaches electrodes to points (leads) clearly established by the protocol, which read information about the functioning of all parts of the heart.
After the ECG, 24-hour Holter monitoring may be prescribed. Indicators in such a study are obtained using a portable device attached to the patient’s body. The patient himself should keep an activity diary.
Diagnosis of extrasystole
The greatest objectivity in diagnosing extrasystole is the method of ECG examination of the patient. Sometimes the presence of this pathology can be detected when a doctor analyzes the patient’s complaints and based on a physical examination.
When performed, the examination can reveal the reason why this disease occurred. It is worth noting that organic damage to the heart muscles requires a special approach to treatment.
Only when special examinations and an ECG are carried out can the presence or absence of extrasystole be refuted or confirmed. Usually, exclusively the above methods help to identify the pathological condition, even in cases where the patient has no special complaints.
ECG monitoring is a fairly long-term recording of an ECG. The procedure lasts approximately 24 hours and is performed using a portable device that is fixed to the patient's skin. A special diary records ECG indicators, as well as the person’s sensations.
ECG monitoring should be performed in all patients who have cardiac pathology, and it does not matter at all whether certain symptoms will be observed in this case, according to which extrasystole can be diagnosed.
Pathology that was not previously recorded on an ECG can be detected using a special treadmill test and bicycle ergometry. These are special tests that allow you to determine the existing arrhythmia under a certain load. To diagnose related pathologies of the cardiovascular system, the doctor may prescribe an MRI of the heart, Echo-CG, and ultrasound of the heart muscles.

Description
The normal rhythm of the heart is associated with the sinoatrial node, located in the right atrium, which acts as a natural pacemaker for the heart. This node generates electrical impulses that pass through the atria, the atrioventricular node and then spread along the His bundle and Purkinje fibers, exciting the ventricular myocardium.
The conduction system and myocardium are controlled by the autonomic nervous system and are sensitive to hormones (catecholamines), allowing the heart rate to speed up or slow down in response to various activities, stress and arousal.
Extrasystoles are essentially extra beats or contractions that interrupt the normal rhythm of the heart. They occur with electrical stimulation in any part of the heart except the sinoatrial node. There are many types of extrasystoles, but according to their place of origin, ventricular and atrial ES are distinguished.
In more than 60% of cases, ventricular extrasystoles develop, 25% occur in atrial extrasystoles, and 10% in combined variants of ES. Less often, in 2% of cases, ES from the atrioventricular junction are determined.
Both atrial and ventricular extrasystoles can develop at any age.
Additional classifications of extrasystoles:
- By number of ES: single, double and group (volley)
- By frequency of development: rare (up to 3 per minute), medium (6-15 per minute) and frequent (over 15 per minute)
- By the number of ectopic foci: monotopic and polytopic
- According to the form on the ECG: monomorphic and polymorphic
- According to the time of occurrence of an extraordinary impulse in diastole: early, middle and late
- Due to appearance: functional, organic and toxic.
There is also a separate classification of ventricular extrasystoles according to Laun and Wolf, according to which ES is divided into five classes, from which high-grade extrasystoles belong to class III and V, and complex ones belong to class IV.
Types of extrasystole
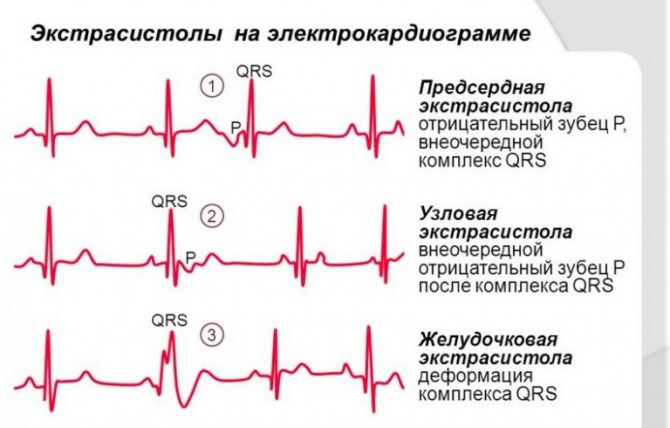
Depending on the location of the excitation of the cardiac muscle, ectopia can be of the following types:
- ventricular;
- atrioventricular;
- atrial;
- combined.
If there is an alternation of extrasystole and normal rhythm, then this condition is called parasystole. And also extraordinary contractions occur early or simultaneously with the T wave on the ECG, mid-formations - after this formation, and late ones occurring before R. Depending on the number of ectopic foci, monotopic and polytopic are distinguished.
How to diagnose and treat extrasystole
The easiest and easiest way to identify the disease is by performing an ECG. And if you contact a specialist, sometimes a simple examination and your complaints, as well as listening to the heart, are enough for him to make a diagnosis. First of all, extrasystoles are removed with the help of sedatives. Even ordinary herbs like chamomile and mint are suitable here. Special breathing exercises are also effective. General sedatives relieve symptoms. This is a disease that is best treated through preventive measures. These include:
- normalization of sleep and activity patterns;
- control over physical activity to prevent fatigue;
- correct diet;
- eliminating stress;
- giving up caffeine and cigarettes.
Why do extrasystoles occur during VSD?
Cardiac “dancing” in vegetative-vascular dystonia can occur when both parts of the autonomic nervous system are disrupted.
If the sympathetic department fails, extrasystoles appear after physical exertion. They are poorly controlled by sedatives, and may even intensify after taking them.
If the functioning of the parasympathetic system is disrupted, in addition to cardiac symptoms, digestive disorders are of concern: epigastric pain, diarrhea, bloating. A cup of coffee or sweet tea or a brisk walk will help relieve such an attack.
If the cause is psychological, treatment measures are directed in the other direction.
Most often, dystonics are bothered by two types of extrasystole:
- Ventricular. Usually makes itself felt in the first half of the day. It is caused by disturbances in mental balance, for example, great joy or grief. It also appears when the weather changes or when drinking strong drinks. Other provoking factors include magnesium and calcium deficiency, osteochondrosis. It all starts with an intense beat in the heart area, followed by a pause. The patient becomes covered in cold, sticky sweat and develops a feeling of fear. Despair sets in, he cannot choose a comfortable position for himself, becomes numb or begins to fuss. The violence of his heart leads him into an uncontrollable state, causing him a lot of suffering.
- Supraventricular. The most common type of arrhythmia in VSD. The causes of this condition coincide with those of the ventricular form. In addition, dystonics who are addicted to antiarrhythmic and diuretic drugs are at risk. Patients claim that the condition worsens when lying down. It is this sign that indicates that the cardiac failure is functional in nature.
Characteristic signs
When the heart contracts unevenly, a person characterizes his condition as arrhythmia. During it, a feeling of irregular rhythms arises in the chest, and anxiety is felt. The main muscle of the body beats too quickly or slowly, or throbs painfully. More complete list of symptoms:
- the heart skips beats;
- noticeable rhythm disturbance with systematic repetitions;
- it becomes more difficult to breathe;
- there is pain or a pulling sensation in the chest area;
- fear of death increases.
Patients themselves may describe their condition incorrectly from a medical point of view: the heart “jumps out of the chest,” turns over, beats painfully against the ribs, etc. The more excited the patient is during an attack, the more colorful and artistic he describes his condition, which can complicate diagnosis.
Reasons for extrasystel
Functional extrasystoles are provoked by stress, caffeine-containing drinks, intoxicants, and sometimes, which is very typical for VSD, by ordinary physical work that is undesirable for them.
Very often, in the absence of provoking factors, functional extrasystole is designated as idiopathic, that is, extrasystole with an unclear cause.
Extrasystole during physical activity can be provoked by metabolic and cardiac disorders (disturbances in the heart itself). In addition, oddly enough, physical activity often has a suppressive effect on extraordinary contractions of the heart, which are formed due to a violation of autonomic regulation. That is, with a single extrasystole, feasible physical work can be recommended.
Depending on the area where the focus of excitation is formed, extrasystoles are distinguished as ventricular, atrioventricular and atrial.
Depending on the frequency of formation of extrasystoles, rare extrasystoles (up to 5 per 1 minute), medium (6-15 per 1 minute) and frequent (more than 15 per 1 minute) are designated.
They also distinguish between a rhythm in which normal systoles alternate with extrasystoles (bigemia), and trihemia - in which two normal systoles alternate with an extrasystole. The rhythm is also determined when an extrasystole follows every third normal contraction.
An objective method for diagnosing extrasystole is an ECG study. However, it is possible to assume the possibility of the presence of this arrhythmia with the help of a physical examination, as well as complaints from the sick person.
When treating extrasystole, it is necessary to take into account the shape and area of its localization. Those extrasystoles that are not provoked by cardiac pathology, in particular, single extrasystoles, do not require specific therapy
And extrasystoles, which arose due to neurogenic factors, are stopped very quickly after the prescription of sedatives, special sedative herbal infusions, and breathing training.
Often, extrasystole in patients with autonomic disorders goes away after a session of breathing exercises (breathing with manual energy replenishment).
Prevention of extrasystole, which has developed against the background of autonomic disorders, is to streamline the work and rest regime, join physical education, maintain a rational, balanced diet, and give up bad habits.
But for any type of extrasystole, including neurogenic extrasystole, you cannot self-medicate and always, if this problem arises, you must seek help from a medical institution!
You might also be interested in:
- Tachycardia with VSD
- Arrhythmia with VSD
Diagnostics
Extrasystole is a disorder that cannot be determined and diagnosed solely on the basis of patient complaints. However, in the process of collecting anamnesis and communicating with the person, you can learn more about the disturbing symptoms, as well as the reasons for the deviations assumed by the patient himself.
To make a final diagnosis, the following diagnostic methods are used:
- ECG . It makes it possible to confirm or refute the presence of extraordinary contractions of the heart, as well as to establish the location of the occurrence of pathological impulses.
- ECG with physical tests . Determines the occurrence of disturbances during physical activity.
- Daily ECG recording . Allows you to determine the number of extraordinary contractions of the heart during the day, as well as their relationship with external influences.
- Electrophysiological study . It is performed only in those patients who have concomitant heart pathologies: heart failure, tachyarrhythmia, etc.
- EchoCG. A diagnostic method that allows you to determine the efficiency of all chambers of the heart, as well as identify the causes of disturbances in the rhythm of the heart muscle.
Is it possible to get rid of extrasystoles?
The mistake of the VSD person is that he is trying to cure his “heart” disease from a cardiologist, although he does not need this doctor at all. The only thing that can be done is to undergo a heart examination (ultrasound, ECG, Holter) and make sure that there was no cardiac pathology. It is useless to take antiarrhythmic drugs; they will only worsen the situation.
Sometimes the only way out is the door to the therapist's office. Only there, with the help of conversations or special medications, can one influence the source of extrasystole - the patient’s subconscious. But often the patient is able to help himself. Many have noticed that there are fewer extrasystoles if a person:
- Tries to regularly switch to pleasant events in order to “turn off” his depressive part, which causes extrasystoles to appear;
- Improves your lifestyle by eliminating bad habits and adjusting your diet;
- Forces himself to be distracted from thoughts about the heart, stops painting the future with black colors;
Success attracts those who believe in it. There are many people on the planet who are much more hopeless before death than the typical VSD with his hypochondria and panic. Of course, this is not a reason to calm down and silently endure your fears. But this is a reason to think about the fact that the chances of recovery will be one hundred percent, if you just want to.
How to quickly get rid of symptoms and attacks
If a person is struck by an attack and does not go away for a long time, it is necessary to fight it in order to avoid serious disruptions in the functioning of the body. If you hesitate, death is possible.
The best option for quickly getting rid of an attack is to call an ambulance. Specialists will provide first aid by administering special beta blockers and monitor the restoration of heart rhythm while the patient is in the hospital.
If an ambulance is unavailable for various reasons, you will need to cope with the violation yourself. Patients who have already been diagnosed and started treatment are able to choose medications to relieve an attack at home. Arrhythmia can be stopped if the following medications are available at home:
- beta blockers;
- antiarrhythmitics of different classes (first, second and third);
- calcium antagonists.
It is important to use these medications correctly. If the attack has not yet begun, but will only appear in the near future, the drugs can be taken in tablet form. You must act according to the instructions and instructions of the doctor. If the disorder has already begun and is expressed in the form of serious rhythm disturbances, an intravenous injection is necessary. The patient is rarely able to do it himself due to the weakness of the nervous system. If the ambulance takes too long, you should ask your loved ones for help. In order to quickly relieve such attacks, the patient’s relatives are recommended to take medical courses to learn how to give injections correctly.
If one of the three drugs mentioned above is not at hand, you should proceed to infusion therapy. It is mostly carried out by qualified health workers; patients themselves rarely have the necessary equipment at home. This treatment is based on the use of a polarizing mixture with potassium. In other cases, specialists may use metabolic substances to improve the functioning of the heart and nervous system.
Treatment methods
Mint infusion is good at calming the nervous system.
To get rid of dystonia combined with extrasystole, you need to lead a healthy lifestyle with sufficient physical activity
It is important to exclude overwork and psycho-emotional shocks. Proper nutrition is necessary without excess fatty, fried, spicy and sweet foods
You need to get rid of bad habits and follow a daily routine. You will also need to consult a neurologist who will prescribe neuroprotective drugs, vitamins and sedatives. The most commonly used infusions of medicinal herbs are motherwort, mint and lemon balm. Also used are infusions of valerian, chamomile, lavender and peony flowers.
In addition, therapeutic breathing exercises and other physical procedures are used that calm the nervous system and improve blood circulation. For persistent extrasystole, which significantly affects the general condition of the patient, “Novocainamide”, “Cordarone”, “Amiodarone” or “Lidocaine” are used. If there is no effect from conservative therapy, surgery is performed in the form of radiofrequency ablation or excision of the heterotropic focus of excitation of cardiac impulses.
Extrasystoles as a symptom of VSD
Extrasystole is an abnormal heart rhythm and is a common type of arrhythmia. The disease manifests itself in attacks - one or more extraordinary contractions of the heart muscle. For healthy people, periodic disturbances in heart rhythm are not dangerous. But if extrasystoles occur in patients with cardiovascular pathologies, then the risk of complications increases significantly.
The occurrence of extrasystole attacks is explained by the appearance of highly active ectopic foci that are localized in the ventricles, in the atrioventricular node or in the atria. Extraordinary impulses are formed in the foci, spreading along the heart muscle and provoking premature contractions of the heart in the diastole phase.
With extrasystole, the volume of ejected blood decreases, so frequent extraordinary contractions of any part of the heart can lead to specific changes in the volume of blood circulation. The earlier the extrasystole began to develop, the less blood will be released during extrasystolic ejection. Such changes adversely affect the course of cardiac pathologies and often accompany the development of vegetative-vascular dystonia. With VSD, disturbances in the autonomic regulation of the heart muscle occur and the work of the parasympathetic division of the autonomic nervous system is activated. In this case, extrasystoles are a symptom of VSD, which must be combated by taking preventive measures and adhering to the recommendations of specialists.
Reasons for the development of pathology
You may be interested in: Removing belly fat using different methods: review, features and effectiveness
The occurrence of the disorder in question in patients can be facilitated by certain heart diseases - acquired, congenital or chronic. Extrasystoles formed during VSD are functional in nature, representing the result of a neurogenic factor.
Doctors identify the following reasons causing the development of the described condition:
- myocardial diseases;
- frequent consumption of drinks that have a high caffeine content;
- emotional or physical fatigue;
- diseases that are associated with the functioning of internal organs;
- smoking and drinking alcoholic beverages;
- nervous stress;
- menstrual cycle;
- damage to the central nervous system;
- infectious diseases that may be accompanied by fever;
- disruption of the nervous regulation of the functioning of the cardiac system.

In addition, possible progression of the disease cannot be ruled out, especially if the patient experiences degenerative changes, as well as inflammatory processes that are associated with insufficient blood supply to the heart.
Sometimes the disease can begin due to an intracellular ion imbalance resulting from a lack of the optimal amount of sodium, magnesium, potassium and calcium in the body. Extrasystole can develop during the formation of heart disease, myocardial dystrophy, myocarditis, as well as in ischemic diseases.
An additional source of development of extrasystole during VSD is called suppressed stress. Under the influence of accompanying symptoms, negative energy splashes out, which leads to destabilization of the functioning of individual organs or the entire organism. In neurotic conditions, extrasystoles, due to certain reasons, can “invade” the central nervous system, indicating the development in the patient:
- sudden attacks of anxiety;
- causeless manifestation of fear;
- unreasonable irritability.
You may be interested in: Endoprosthetics is... Types, preparation, surgery
Manifestations of irregular heartbeats usually do not pose any threat. The only exceptions will be people with existing cardiovascular diseases.
Acute circulatory failure can be caused by frequently recurring similar conditions. Thus, existing ventricular extrasystoles can pose a great danger, since there is a threat in which they often lead to ventricular fibrillation, which can cause sudden death.

Extrasystoles - what are they?
Extrasystole (“extra” - extra, “systole” - cardiac contraction) is an extraordinary, “extra” contraction of the heart, the causes of which are not always clear. Such a contraction is usually felt by the patient as a sharp push from the inside, immediately perceived as a threat to life: panic, cold sweat and heat at the same time, weakness, and disorientation in space may appear.
A pause in the work of the heart after this extraordinary beat “finishes off” a person’s endurance. The heart, which is just trying to even out its rhythm, seems confused and ready to stop at any moment. When, after such an extra beat with a pause seconds later, a new extrasystole follows, the patient completely surrenders to his panic and no longer knows what to do or how to calm down.
Sometimes extrasystoles during VSD become worse for the patient than the most severe adrenaline crises. Having once experienced this terrible symptom, a person with VSD is likely to acquire cardioneurosis and begin to listen to his pulse every minute, count its beats and evaluate their evenness. If anything deviates from the norm, the patient automatically attributes to himself a fatal heart disease and imagines the impending tragedy in horror. But why do extrasystoles occur so often during VSD?
- Failures in the central nervous system and chaotic nerve impulses that make the heart “dance.” This could be due to anything: a change in weather, a sudden change in body position, stress, anxiety, getting into a situation associated with a phobia. Sometimes the reasons lie deep in the subconscious, and the patient is inclined to think that his nerves went wild out of the blue, although this is not the case.
- Osteochondrosis, often in step with VSD. A pinched nerve can also send additional impulses to the heart. If extrasystoles during VSD occur after adopting a certain body position, and there is a suspicion that the spine is involved, it is worth checking with a neurologist.
- Cardioneurosis. It can arise both due to the first fear of extrasystoles, and due to excessive reading in medical literature. When a patient listens to his heart every now and then, it will definitely make itself known. And what “ordinary” people don’t pay attention to at all, for a VSD person can become the starting button for launching an entire panic attack.
Nervous disorders due to illness
The disease can be diagnosed not only through a blood test or a history of external signs. Studies of the functioning of nerve impulses, carried out using special devices, will also help make a diagnosis.
With extrasystole, the nervous system is characterized by disruptions and regular deviations. The impulse transmission mechanism is disrupted. They either follow the wrong path, encountering obstacles along the initially chosen nerve, or reach the heart with a delay. Most often, signals follow a shortcut, deviating from the true “road”.
Nerve impulses travel to the heart through a special complex - Purinier fibers. Sometimes malfunctions can occur in them (a healthy person cannot have errors; disturbances in signal transmission are a symptom of a deviation). Information from the brain travels along one of the fiber branches, but an error occurs and the impulse does not reach its destination. Then he crosses the bridge connecting the branches to another department and finishes his journey along it. Because of this, the heart contracts either delayed or premature.