An analysis such as a coagulogram
It is quite widely known, but is not prescribed during a standard medical examination. Therefore, patients are sometimes surprised by the doctor’s proposal to conduct this study. More often, a blood coagulogram is performed in patients with pathology of the cardiovascular system, as well as before a planned operation or in pregnant women. In the latter case, it is done every trimester without fail.
What is hidden under the mysterious term? Coagulogram (another name for the study is hemostasiogram
) is carried out to study the patient's blood clotting
. Analysis can be basic
or
advanced
. Typically, a baseline study is ordered first. It helps to understand where in the system the deviation from the norm occurred. And if a pathology is detected, a detailed study is carried out, as a result of which not only qualitative changes are determined, but also quantitative ones.
Main indications for analysis
- Planned operations. There is always some risk of bleeding during surgery. Therefore, knowledge about the state of the blood coagulation system is important.
- Pregnancy. During this period, changes can occur in the female body, both positive and negative. It is usually carried out once every trimester. If fetoplacental insufficiency or gestosis is diagnosed - more often.
- Vascular disorders (increased thrombus formation, varicose veins).
- Liver diseases.
- Autoimmune pathologies.
- Blood clotting disorder.
- Cardiovascular pathology (heart attack, stroke, ischemic heart disease).
- When prescribing anticoagulants.
- For the correct selection of the dose of acetylsalicylic acid and drugs based on it.
- Prescription of contraceptive drugs. In this case, the analysis is done once every 3 months.
- Treatment with leeches (hirudotherapy). A coagulogram is performed to prevent hemorrhages.
Treatment
The uncontrolled destruction of red blood cells must be treated immediately. If the cause of the pathology is an error during blood transfusion, therapeutic methods are used aimed at stopping the infusion of red blood cells from incompatible blood.
To prevent the occurrence of hyperfusion in the kidneys and hypovolemia, special solutions are administered. A blood purification procedure is carried out using plasmapheresis, with the intravenous administration of Heparin. The procedure is aimed at removing free hemoglobin from the blood. Prednisolone is also used in the treatment of acute hemolysis.
Heparin injections
Drug treatment of acute hemolysis is prescribed by the attending physician, based on the clinical picture and symptoms of each individual case.
It is important to know exactly when the pathological process began to develop in the patient’s body.
In particularly severe cases, treatment requires urgent hemodialysis, especially in the presence of renal failure.
One of the reasons for the rapid destruction of red blood cells is long-term use of certain medications. These are mainly anti-tuberculosis drugs, drugs from the sulfonamide group and hypoglycemic antibiotics.
With this clinical picture, hemolysis of the destruction of blood cells is not a pathology, and does not indicate the presence of serious diseases - it is just a natural reaction of the body to taking certain medications, the patient’s condition normalizes after completing the course of taking them.
Natural hemostasis system
Blood clot formation
In a healthy body, a normally functioning hemostasis
- natural protection against excessive blood loss when the integrity of the vascular wall is violated. Many people know about the danger of blood clots to human health and life, but nature does not create anything in vain: thrombus formation is the very protection against blood loss. Let's try to find out how the natural hemostasis system works.
Blood is constantly in a liquid state. Moreover, this liquid has a certain composition and physical parameters. The body's systems tirelessly maintain this state throughout life. However, various situations occur: for example, as a result of damage to the vessel wall, bleeding occurs. The first substance that is released in the blood is thromboplastin.
.
It starts the coagulation system: it activates proteins that are normally present in the blood. These proteins form a clot at the site where the integrity of the vessel is damaged. A chain is carried out leading to thrombus formation:
thrombin is synthesized
prothrombin fibrinogen
, from which, in turn,
fibrin .
It is in fibrin, like insects in a spider's web, that platelets get stuck, forming a blood clot. The fibrin clot “patches” the wound in the vessel, and the bleeding stops.
In a healthy body, both systems - coagulation and anticoagulation - are in balance. But there is also a third system - resorption (fibrinolysis). It is this that ensures the dissolution of the blood clot after the integrity of the vessel is restored. Coagulogram indicators allow us to draw a conclusion about the state of all systems.
Impaired hemostasis
Causes of impaired hemostasis:
DIC syndrome. A common type of hemostasis pathology. Blood clotting is impaired due to the massive release of thromboplastic substances from tissues. May be asymptomatic.
Impaired hemostasis (coagulopathy). Violation of the functions of the blood coagulation and anticoagulation systems. Pathological condition of the body. It is possible to distinguish immune, acquired and genetic forms of coagulopathies.
Thrombotic syndrome (thrombophilia). It is characterized by inadequate blood coagulation and thrombus formation, leading to ischemia of tissues and organs.
Hypocoagulative-hemorrhagic condition. Accompanied by a pathological process of reducing blood clotting.
Classification of hemostasis disorders:
hereditary or acquired;
hypocoagulative (decreased blood clotting) or hypercoagulative (increased blood clotting);
local (thrombosis) or global (DIC syndrome).
Reduced blood clotting
Causes of decreased blood clotting:
Immune reactions (viruses, drugs);
Deficiency of cyanocobalamin and folic acid;
Effect of toxic drugs;
Hormonal disorders (hypothyroidism);
One of the possible causes of bleeding may be a decrease in the production of von Willebrand factor by the endothelium of the vascular wall - a large molecular component of blood coagulation factor VIII (hereditary von Willebrand disease). This factor accumulates in platelets and is released during their degranulation.
Hemorrhagic syndrome
Hemorrhagic syndrome is characterized by a state of increased bleeding and disturbances in one of the links of the blood coagulation system. It can be either an acute or chronic disease.
Characteristic symptoms:
Rash in the form of small dots;
spots up to 3 mm in diameter (petechiae);
bruises on the skin and mucous membranes (eczymoses);
Ecchymoses are not just bruises, but characteristic signs of hemorrhage into the skin or mucous membrane
If the above symptoms are detected, it is important to conduct laboratory diagnostics. It will show indicators of a decrease in the number of platelets and an increase in the bleeding time
von Willebrand disease
Symptoms of von Willebrand disease:
Tendency to subcutaneous hemorrhages;
prolonged bleeding of small cuts;
prolonged menstruation (in some cases);
abnormal bleeding after surgery.
Thrombocytopenia due to impaired hemostasis
Thrombocytopenia is characterized by a decrease in the number of platelets and is accompanied by increased bleeding and problems with bleeding. It can accompany any hematological diseases as one of the main symptoms.
As an independent disease, it is sometimes diagnosed as Werlhof's disease. The main causes of thrombocetopenia are impaired platelet production, as well as their increased destruction. Also among the possible causes are infectious and epidemiological:
acute manifestations of herpes infection;
Impaired hemostasis and the development of bleeding during thrombocytopenia are caused by the following mechanisms:
increasing the permeability of microvessels for red blood cells and other components of the blood;
fragility of blood vessels due to wall degeneration;
decrease in the adhesive-aggregation function of platelets;
violation of the reaction of release of platelet coagulation factors;
decreased clot retraction as a result of decreased activity of platelet contractile protein.
Coagulation hemostasis
Along with the primary, vascular-platelet hemostasis, a secondary hemostasis develops - coagulation. It plays the role of additional support and regulation of blood loss from the vessels. Violation of coagulation hemostasis can be caused by the following factors:
activation of the fibrinolytic system;
increase in endogenous anticoagulants;
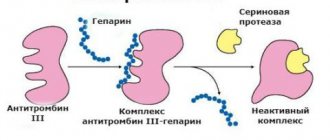
Anticoagulants inhibit the formation of fibrin threads; they prevent thrombus formation, help stop the growth of existing blood clots, and enhance the effect of endogenous fibrinolytic enzymes on blood clots.
Causes of phase I disorders of blood coagulation
The causes of impaired thromboplastin formation may be the following:
decreased production of factors (IX, X) in liver pathology;
formation of antibodies in leukemia;
overdose of the anticoagulant heparin;
genetic defects in the synthesis of factors VIII, IX and XI.
Basic hemostasiogram parameters
- Fibrinogen
. The most important test of the state of the coagulation system. - Prothrombin index (PTI), INR (international normalized ratio), PTT (prothrombin time).
Usually one of these tests is performed, based on the equipment available in the laboratory. The most universal test is INR. All of these studies show an extrinsic clotting pathway. - Activated partial thromboplastin time
.
In the test you can find the abbreviation - APTT
. - Thrombin time.
Additional hemostasiogram parameters
Yandex.Direct
| Pregnancy blood test. Exactly. Tests for genetic risks using blood from a vein. 100% accuracy. prenetix.ru There are contraindications. Consult your doctor. |
- Protein
C. An insufficient amount of this parameter leads to thrombosis. - Antithrombin
. Like protein C, it is a factor in the anticoagulation system. - D-dimer
. Formed as a result of the destruction of a blood clot. - Lupus anticoagulant
. - Plasma tolerance to heparin
. - AVR (Activated recalcification time).
- RFMC (soluble fibrin-monomer complexes).
- Plasma recalcification time.
Coagulation system
The hemostasis system is considered one of the most important systems ensuring the vital functions of the human body. It prevents the loss of the most precious biological substance - blood in case of damage to the integrity of blood vessels. It also ensures rapid restoration of blood flow by dissolving fibrin clots - thrombi.
There are two mechanisms for achieving hemostasis:
- Primary, called vascular-platelet hemostasis, the indicators of which determine the properties of platelets, bleeding time and capellar resistance. Its activation occurs under the influence of tissue cells of blood vessels.
- Secondary (also called coagulation), depending on plasma blood clotting factors.
After damage to the walls of blood vessels, a microspasm occurs, which activates endothelial cells, as a result of which the body begins to intensively produce biologically active substances. Under their influence, platelet adhesion begins, which leads to the formation of a platelet plug. At the same time, the process of activation of plasma blood factors is launched, under the influence of which a fibrin clot is formed, stopping blood loss.
Factors that ensure blood clotting and subsequent fibrinolysis (dissolution of a blood clot) are produced by the liver. They constantly circulate in human blood, but are in an inactive state. A prerequisite for their activation is damage to the blood vessel and the interaction of tissue cells with blood cells.
Unfortunately, in some cases the blood clotting system does not function properly. As a result, the blood has too low coagulability, or, conversely, increased. Impaired hemostasis can be caused by various reasons. They are conventionally divided into three groups:
- hereditary - caused by gene mutations;
- autoimmune - accompanying the course of a number of systemic autoimmune diseases;
- acquired - resulting from the use of certain medications, hormonal imbalances, liver disease, tumor diseases of the hematopoietic organs.
Pathology of hemostasis includes the following disorders:
- Coagulopathy is a condition in which the blood coagulation system does not function properly due to the factors listed above.
- DIC syndrome, in which the level of blood cell aggregation is increased, which leads to intravascular thrombus formation and circulatory disorders.
- Hypocoagulation, in which the activity of tissue and plasma coagulation factors is reduced, which causes increased bleeding.
- Hypercoagulation, in which the level of activity of tissue and plasma factors and the rate of platelet aggregation are increased, which causes intense formation of fibrin and platelet clots.
Carrying out a coagulogram during pregnancy
Who, while completely healthy, gets the most research? Undoubtedly, these are pregnant women. Numerous ultrasounds, tests, tests, examinations - all these tests must be passed by the expectant mother to give birth to a healthy child. The list of necessary tests for pregnant women includes a coagulogram. These analyzes characterize hemostasis and allow early detection of disturbances in this system. In the body of the expectant mother, many processes go differently than before pregnancy. In particular, the activity of hemostasis increases, which is normal.
However, there are also deviations from the norm. And this is already becoming dangerous for both mother and child. Disturbances in the functioning of blood systems can lead to irreparable consequences. In order to detect and neutralize all kinds of problems in time, a hemostasiogram is performed.
What is the activation of the hemostatic system associated with during pregnancy?
- Firstly, a woman’s hormonal background changes.
- Secondly, a new (uteroplacental) circulation appears.
- Thirdly, the pregnant woman’s body prepares for inevitable blood loss during the birth of the child.
If there is a blood clotting disorder during pregnancy, there is always a danger of developing the so-called DIC syndrome (disseminated intravascular coagulation), which is characterized by hypercoagulation in the first stage and hypocoagulation in the second, that is, leading to massive blood loss. DIC syndrome is considered one of the most serious complications in obstetrics, is often uncontrollable and poses a danger not only to the life of the fetus, but also to the life of the woman.
The opposite situation is possible. Due to a violation in the anticoagulant system, the blood becomes very thin. As a result, the risk of bleeding increases, especially during childbirth. In order to restore hemostasis, an analysis and further interpretation of the coagulogram is carried out. Based on the results of the study, treatment is prescribed.
Normally, this test is performed in each trimester of pregnancy. Unscheduled if:
- The woman had miscarriages.
- Symptoms of gestosis
: arterial hypertension, swelling of the extremities, protein in the urine. - Uterine hypertonicity (threat of miscarriage) is diagnosed.
There are many reasons for impaired hemostasis, but women whose relatives have had a heart attack, stroke, thrombosis, varicose veins, or diseases of the blood system should pay special attention to their condition.
Important! Among pregnant women, there is a widespread belief that any medications are harmful to the unborn child. But you can’t joke with the hemostasis system. A timely study and taking the necessary medications will help a woman carry and give birth to a healthy child.
Physiology
Extravascular tissue, the vessel wall, plasma blood coagulation factors, platelets, and other blood cells take part in the G. process. An important role in G. belongs to physiologically active substances (adrenaline, norepinephrine, serotonin, etc.), local changes in ionic ratios, blood pH, and zeta potential (the potential difference between the dispersed phase and the dispersed medium, platelets and the vascular wall).
Different tissues surrounding an injured vessel have different thromboplastic activity; biol, the significance of these differences for local G. is not yet clear. As a result of the interaction of tissue and plasma factors of the blood coagulation system, active tissue thromboplastin is formed at the site of damage to the vessel wall, which is included in a chain of subsequent reactions, the final product of which is fibrin. However, tissue thromboplastin (less active than blood thromboplastin) is probably of less importance in G. when large vessels are injured. The tissues surrounding the vessel also provide mechanical resistance to the release of blood from the damaged vessel, thus influencing the amount of blood loss.
The role of the vessel wall in blood flow is determined by the presence in it of a number of factors that influence the process of blood coagulation, adhesion and aggregation of platelets; When injured, the vessel wall contracts and blood flow to the wound site decreases. The vessel wall is an efferent regulator of the rate of blood coagulation and fibrinolysis (see). The vascular intima is charged negatively in relation to the adventitia. When the vessels are damaged, the potential is reversed and the intima becomes positively charged, the zeta potential changes, which is important for the interaction of platelets with the wound surface.
Plasma blood coagulation factors in the body of a healthy person are in an inactive state. The International Committee on Blood Coagulation Factors introduced the designation of plasma procoagulants in Roman numerals; their number is thirteen (from I to XIII).
Plasma coagulation factors
Factor I - fibrinogen
Factor II - prothrombin
Factor III - thromboplastin
Factor IV - calcium
Factor V - accelerator (accelerator) of prothrombin conversion (Ac-globulin)
Factor VI - removed from the classification Factor VII - proconvertin Factor VIII - antihemophilic globulin
Factor IX is a plasma component of thromboplastin (Christmas factor)
Factor X - Stewart - Prower Factor
Factor XI - plasma precursor of thromboplastin Factor XII - contact factor (Hageman)
Factor XIII - fibrin stabilizing factor, fibrinase
Activation of the blood coagulation system occurs upon contact with a foreign surface, which is the trigger of the internal blood clotting system (active blood coagulation factors are indicated by adding the letter “a” to the corresponding Roman numeral). G. ends with the formation of a blood clot at the site of damage to the vessel wall.
The participation of platelets in blood clotting is due to their properties such as adhesion and aggregation, the content of their own and adsorbed blood coagulation factors, as well as physiologically active substances.
The role of erythrocytes and leukocytes in blood flow is determined by the content of the majority of blood clotting factors in them. When the vascular wall is damaged, these factors are included in the fibrin formation reaction. During blood clotting, red blood cells are retained in the fibrin network, promoting the formation of a blood clot and an increase in its mass.
G.'s process has neurohumoral regulation: extreme factors cause an increase in the tone of the sympathetic department. n. pp., increase the flow of adrenaline and norepinephrine into the blood, which accelerates the adhesion and aggregation of platelets and activates the blood coagulation process as a whole. The spread of thrombus formation along the vascular bed is prevented by circulating anticoagulants, fibrinolytic agents and inhibitors of platelet adhesion and aggregation - adenosine and adenosine monophosphate, which are formed during the breakdown of ADP.
Depending on the size of the damaged vessel and the role of individual factors in limiting blood loss, two main mechanisms of blood loss are distinguished: vascular-platelet (or microcirculatory) and coagulation. In the first, the leading role in stopping bleeding is assigned to the vascular wall and platelets (see), in the second - to the blood coagulation system (see Blood coagulation system). In addition, DIC syndrome (disseminated intravascular coagulation) may occur.
Scheme 1. Vascular-platelet mechanism of hemostasis.
Vascular-platelet mechanism
(Scheme 1) occurs when bleeding from small vessels is stopped: arterioles, precapillaries, capillaries and venules. It consists of the following stages: 1) short-term vascular spasm, 2) adhesion of platelets to the wound surface, 3) accumulation and aggregation of platelets at the site of injury, 4) viscous metamorphosis and platelet release reaction, 5) secondary vasospasm, 6) formation of fibrin and fiziol, hemostatic thrombus (see).
Under the influence of injury, the tone of the sympathetic department increases. n. With. and local vasospasm occurs, reducing blood flow. Vasoconstriction is also facilitated by the reflex release of adrenaline into the bloodstream and the release of cholinesterase, which blocks acetylcholine. Platelets adhere to damaged endothelial cells and tissue fibers of the vascular wall on the wound surface: the formation of a hemostatic platelet thrombus begins.
The main structures of the vascular wall with which platelets interact are collagen fibers, microfibrils and basement membrane. The adhesion of platelets to collagen fibers is apparently not associated with the process of blood coagulation, since when the blood is completely incoagulable (for example, as a result of heparinization), it is not disturbed. Thrombin does not cause platelet adhesion, but enhances it, promoting the release of ADP from platelets. In the mechanism of interaction of platelets with the damaged vessel wall in the process of G., electrostatic forces that enhance the adhesion of platelets to the wound surface are probably important. Slowing blood flow and blood movement contribute to the interaction of platelets with the damaged vessel wall.
Following adhesion, platelet aggregation occurs at the site of injury to the vessel wall. ATP is released from damaged endothelial cells, as well as from erythrocytes and platelets, which is converted into ADP under the action of cellular adenosine triphosphatase. Under the influence of the latter, platelet aggregation occurs (reversible); The effect of ADP on platelets is manifested in the presence of calcium ions and a plasma cofactor in the medium - von Willebrand factor, factor XIII (fibrin-stabilizing factor) or factor I (fibrinogen). A number of hypotheses have been proposed to explain the mechanism of platelet aggregation; The most widely recognized hypothesis is that of Gaarder and Laland (A. Gaarder, J. Laland), who believe that the platelet-aggregating activity of ADP is due to three free negative valences: two valences bind one calcium ion, and the third, together with the same valency of the neighboring ADP molecule, attaches another calcium ion; platelet aggregation occurs as a result of the formation of calcium “bridges” between platelet-nucleotide complexes.
Platelets that aggregate at the wound surface undergo viscous metamorphosis under the influence of thrombin. During the process of viscous metamorphosis, blood clotting factors, serotonin, histamine, adrenaline, kinins, nucleotides, and enzymes are released from platelets; platelet aggregation Becomes irreversible. The release of these factors from platelets promotes secondary narrowing of the damaged vessel. In parallel, the reaction of fibrin formation occurs. Fibrin fibers and subsequent retraction of the blood clot compact the hemostatic thrombus, which leads to the final cessation of bleeding.
Scheme 2. Coagulation mechanism of hemostasis.
Coagulation mechanism
(Scheme 2) occurs with injury to large arteries and veins following the limitation of blood loss as a result of vascular spasm, especially of the muscular type. However, in this case, platelets are the first to attach to the site of damage to the vessel wall. At the same time, the blood coagulation system is activated as a result of the complex interaction of plasma and cellular procoagulants, which occurs as a proenzyme-enzyme cascade transformation, and fibrin is formed. Blood cells are drawn into the fibrin network, a blood clot is formed, which reduces or completely prevents blood loss). The final stage is retraction of the blood clot, which lasts several hours. As a result of retraction, the hemostatic thrombus becomes more reliable. In this case, serum rich in thrombin is released from the clot.
Disseminated intravascular coagulation (DIC) is a syndrome that can occur in various pathological conditions (acute hemolysis, infectious processes, intoxication, antigen-antibody reaction, etc.). Both vascular-platelet and coagulation factors take part in its development.
Impaired hemostasis due to defects in individual components of its system - see table.
Study of hemostasiogram
After a blood test, the coagulogram is deciphered. What indicators can be seen in a laboratory report, and what do they mean?
Fibrinogen
This enzyme is synthesized in the liver. Normally, this figure ranges from 2 g/l to 4 g/l. For pregnant women, its increase is considered normal, but the fibrinogen content, even in the third trimester, should not exceed 6 g/l. This is a very sensitive factor. Its reaction to inflammation and tissue necrosis has been established. An increase may also indicate infections, acute inflammatory processes (pneumonia), the onset of a heart or brain infarction, hypothyroidism, burns, or contraception. If the amount of fibrinogen decreases, one may suspect a lack of vitamins (C, B 12), hepatitis, toxicosis, taking certain medications, or cirrhosis of the liver. And, of course, the infamous DIC syndrome.
APTT
The time it takes for a blood clot to form is examined. This indicator reacts sharply to changes in other coagulation factors. The normal APTT is from 30 to 40 seconds. An increase in the parameter may indicate hemophilia, vitamin K deficiency, or liver disease.
Prothrombin
Thrombin is synthesized from this protein in the liver when exposed to vitamin K. By changing the value of this factor, the state of the gastrointestinal tract and liver is judged.
Lupus anticoagulant
This indicator is assessed mainly during a hemostasiogram in cases of suspected antiphospholipid syndrome, systemic lupus erythematosus or other autoimmune disease. IgM and IgG antibodies to phospholipids are produced in the blood (normally they are absent), which contribute to an increase in the aPTT rate. Their appearance indicates gestosis or autoimmune diseases. Usually this situation ends in failure: the woman loses her child.
table: normal values of the basic coagulogram
Thrombin time
Shows the time it takes for fibrinogen protein to be converted to fibrin. The normal setting is from 11 to 18 seconds. Since the amount of fibrinogen increases during pregnancy, it is logical to assume that thrombin time also lengthens. However, the indicator still does not go beyond the norm. If the data is deviated from the norm, then this may indicate a lack or excess of fibrinogen in the blood.
Prothrombin time
This indicator means the time of thrombin formation from its inactive form (prothrombin protein). Thrombin is needed to form a blood clot, which helps stop bleeding. If this indicator is increased, hypovitaminosis K, deficiency of coagulation factors, and liver disease can be diagnosed.
Prothrombin index
One of the most important indicators. The clotting time of normal plasma is compared to the same time in the patient. PTI is expressed as a percentage. The normal rate should be between 93-107%. A change in PTI can signal liver disease and risk of thrombosis. An increase in the rate may occur during pregnancy or when taking contraceptives. If blood clotting properties deteriorate, the PTI will be lowered. Since the prothrombin index is directly related to vitamin K, a decrease indicates a lack of this vitamin or poor absorption in the intestine (for example, with intestinal ailments). Taking aspirin or diuretics also reduces PTI levels.
Platelets
Blood cells that are directly involved in maintaining hemostasis. The norm in the blood of these cells is from 150,000 to 400,000 per μl. If the indicator decreases, thrombocytopenia is diagnosed. This may indicate that the mother is undernourished. Platelets are synthesized in the bone marrow.
Antithrombin-III
It is protein in nature and is an antagonist of the thrombin enzyme. Its role is to inhibit the action of the coagulation system. This parameter is expressed as a percentage. The norm is from 71 to 115 percent. If the parameter decreases by half, the risk of thrombosis increases. In case of increased blood clotting, anticoagulants are prescribed. In this case, monitoring of the indicator is also necessary.
DIC syndrome
Normally, the coagulation and anticoagulation systems are in balance. If any of the factors of these systems is disturbed, the entire hemostasis becomes unbalanced. This is especially dangerous in pregnant women. The most serious complication is disseminated intravascular coagulation. Activation of the coagulation system and fibrinolysis stimulates the development of DIC syndrome. As a result of the development of pathology, a pregnant woman may experience placental abruption, endometritis, or amniotic fluid embolism.
D-dimer
As a result of incomplete disintegration of fibrin fiber, rather large “fragments”—D-dimers—appear. This is one of the main indicators of a coagulogram for pregnant women. The general norm is less than 500 ng/ml. However, other parameters are considered normal in pregnant women. Already at the beginning of pregnancy, the indicator begins to increase, and before childbirth it exceeds the norm several times. An increase may also be observed in patients with diabetes mellitus, with kidney disease, during complicated pregnancy (preeclampsia), and in old age.
standard form of unexpanded coagulogram
Antibodies to phospholipids (Antiphospholipid syndrome)
The disease is autoimmune. The amount of antibodies to phospholipids begins to increase in the body. This is a series of symptoms that characterize arterial and venous thrombosis. Pregnant women diagnosed with APS are at risk of losing their baby due to fetaplacental insufficiency.
Plasma recalcification time
Indicator of fibrin protein clot formation. This parameter reflects the coagulation process as a whole.
Plasma tolerance to heparin
This test is carried out simultaneously with the previous one. Heparin is added to the plasma and the time of plasma recalcification is noted. If this indicator is less than normal, changes in other factors of the coagulation system are possible. Liver cirrhosis and hepatitis are suspected. When the parameter increases, it can be assumed that the body has diseases such as heart failure, prethrombosis, and malignant tumors. However, normally, an increase in the indicator can occur in the last stages of pregnancy.
Important! It should be noted that decoding of a coagulogram during pregnancy (as, indeed, for all other patients) can only be carried out by a specialist. It is unacceptable to diagnose yourself based on one data or another and prescribe treatment.
Gene mutation analysis
Hemostasis testing does not always make it possible to predict the risk of developing pathologies in the patient’s blood coagulation system. In this case, a study is carried out of genes that are responsible for the response of the hemostatic system, for example, during pregnancy or inflammatory processes. Testing for gene mutations is indicated for the following categories of people:
- Women choosing hormonal contraceptives.
- Suffering from infertility and recurrent miscarriage.
- Women who require hormone replacement therapy.
- Men who smoke and are under 50 years old.
- People under the age of 50 who have suffered thrombosis.
- Before gynecological surgery, transplantation, endoprosthetics.
- Anyone who has relatives who suffered thrombosis, strokes, pulmonary embolism, heart attacks under the age of 50, as well as those who died who have not reached this age.
- Young people with hearing impairment of unknown etiology.
- People who have undergone long-term infusion treatment (chemotherapy).
In these cases, you need to be tested for mutations in the genes of the coagulation system and folic acid metabolism.
Where can I get tested and how much does it cost?
Anyone can take a blood test such as a hemostasiogram at one of the nearest medical centers, if it has the necessary equipment and reagents at its disposal. The cost of a coagulogram depends on the range of services and equipment of the center. Basically, the price of the basic package varies from 700 to 1,300 rubles (in Moscow). An extended coaguloramma costs about 3,500 rubles.
However, for pregnant women, a coagulogram is included in a number of mandatory studies and is carried out free of charge. Under the compulsory medical insurance system, you can also get a test completely free of charge, having first received a referral from your attending physician.
Research methods
G.'s condition is identified by coagulogram indicators (see), as well as on the basis of tests that determine: the state of resistance of the vascular wall, bleeding time (see), both primary and secondary, the volume of blood lost, aspirin tolerance, the strength of early fixation platelet plugs in vessels, the number of platelets, their functional activity (ability for adhesion in vitro and in vivo, ADP-, collagen- and thrombin-aggregation).
The principle of restoring hemostasis is to strengthen the vessel wall, increase the adhesive and aggregation ability of platelets, and restore lost or reduced blood clotting ability.
The main principle of the medicinal method of stopping bleeding is the differentiated use of hemostatic agents, taking into account the mechanism of bleeding development. Therefore, before starting antihemorrhagic therapy, it is necessary to conduct a thorough laboratory study of the functional state of the blood coagulation system in order to identify the main cause of impaired hemostasis.
How to submit?
The question “how to take it” in the case of a coagulogram test is not at all superfluous. The results of the study depend on proper preparation of the patient. This analysis is performed in vitro
(in vitro - outside the body). Blood is taken from a vein.
Blood is donated on an empty stomach. The last meal should be no later than 8-12 hours before the test. You cannot drink any drinks (coffee, tea, and especially alcohol). Only clean water is allowed. The medications you are taking - especially those that affect the blood clotting process - must be indicated at the time of the test. The emotional state of the patient is very important. You need to try not to be nervous, to be calm and balanced. Muscle overstrain also negatively affects the results of the study. It is useful to drink an additional glass of cold water right before taking the test. Interpretation of the results is carried out only (!) by a specialist.
What is a hemostasiogram?
If a disorder in the blood coagulation system is suspected, the doctor prescribes a hemostasiogram ( coagulogram ) - a comprehensive analysis that allows identifying such disorders. A hemostasiogram (or hemostasis test) can be basic or extended. When planning a pregnancy, an extended pregnancy is usually prescribed.
Blood for analysis is taken in the morning on an empty stomach from a vein. It is not recommended to donate blood during menstruation, when blood clotting function is increased. Also, you should not take a hemostasis test after taking alcohol or aspirin, which thin the blood. Typically, test results are ready two hours after donating blood.
Functions of hemostasis
Hemostasis serves several functions in the body. The liquid state of blood ensures precisely this process. It also promotes its rapid coagulation during damage to arteries and large veins. It forms a platelet plug that clogs minor vascular damage.
After restoration of soft tissues, blood clots can lead to vascular pathology, so hemostasis breaks them down . Essentially, this is internal protection against significant blood loss. Only thirteen enzymes influence blood clotting: these proteins are called clotting factors.
The platelets become sticky and stick together. At this point, the process of hemostasis begins. The individual cells then join together to form a plug, which prevents blood loss. Coagulation proteins form a network of fibrin fibers: it covers the opening in the tissue.
During hemostasis, one passive enzyme is activated, which then causes other inactive proteins to work. This process continues endlessly. It is called the coagulation cascade. They are divided into two types. The first is carried out using substances that are already contained in the blood. And when blood vessels are injured, tissue thromboplastin is formed. It ensures the functioning of the external cascade.
Types of hemostasis
There are three types of hemostasis: vascular-platelet, coagulation, fibrinolysis. Depending on the severity of the bleeding, one or another mechanism is in the lead in the process of thrombus formation. Varieties of hemostasis are included in the work simultaneously, are in a state of constant interaction, complement each other from the beginning of the formation of a blood clot until its complete dissolution.
Vascular-platelet
Platelet hemostasis is aimed at stopping bleeding from small vessels. The primary reaction consists of phases:
- Reflex vasospasm.
- Attachment of platelets to the damaged area.
- Reverse accumulation of platelets.
- Irreversible platelet aggregation.
- Retraction of a platelet thrombus is the formation of a seal that stops blood in vessels with low blood pressure.
Coagulation
This mechanism ensures that blood stops in those vessels for which primary hemostasis is insufficient. During the coagulation mechanism of coagulation, the platelet thrombus turns into a final hemostatic plug that closes the vessel defect. Secondary hemostasis ensures complete cessation of blood in the arteries, veins and arterioles; thrombus formation occurs within a few minutes.
- Pain in the left hypochondrium
- Mackerel in foil in the oven: recipes with photos
- How to tan quickly in a solarium
Fibrinolysis
The mechanism is responsible for the breakdown of fibrin threads into soluble complexes, restores vascular patency, and maintains normal blood thickness. The fibrinolysis system consists of plasmin, plasminogen activators, and inhibitors. Fibrinolysis can be enzymatic and non-enzymatic, passing through external and internal activation pathways. The process involves the ability of leukocytes to destroy and digest pathogenic organisms, eliminate thrombosis and remove its remains.
In what cases is a hemostasis test prescribed?
The main reasons why a blood test for hemostasis may be required are:
- the need to establish the causes of increased blood loss, internal bleeding or manifestations of autoimmune diseases;
- diagnosis, prevention or treatment of thrombosis, heart attacks and strokes;
- regular measures to prevent internal bleeding in patients undergoing surgery;
- pregnancy planning stage;
- treatment of gynecological diseases in pregnant women.
These are the most common reasons why doctors send their patients to donate blood to check the functioning of the hemostasis system. But here it is important to understand that each specific case is individual, so this type of laboratory test can be prescribed in other situations.
Preparing for tests
View gallery
So, you are about to go to the doctor. How to take a blood test for hemostasis so that the results are reliable? It is important to understand that your body must first be prepared. You should go to the hospital on an empty stomach. Doctors recommend stopping eating approximately 10 hours before going to a medical facility. Only non-carbonated purified water is allowed to be consumed. In addition, the day before the test, it is recommended to minimize any physical activity, avoid stressful situations, and also get enough sleep.
The use of any alcoholic beverages and medications should be avoided, as they will negatively affect the composition of the blood, which will complicate the blood test for hemostasis. The decoding in this case will be incorrect, as a result of which it will be difficult for the doctor to assess the real condition of the patient and prescribe appropriate therapy.