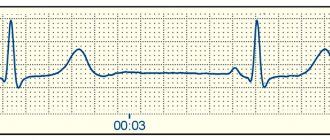
P wave
The sinus node is located at the junction of the vena cava. During depolarization, the impulse travels through the right atrium, thus forming the ascending limb of the P wave. Thus, if any changes occur in the ascending limb of the P wave, then the problem is in the right atrium.
Next, the impulse travels through the left atrium; on the ECG it is the descending limb of the P wave.
Typically, the ascending and descending limbs of the P wave are symmetrical.
The P wave is responsible for the atria:
- it is always positive, except for those leads where all the waves are negative (aVR, V1)
- height up to 2 mm
- duration up to 0.1 sec
If the P wave grows in the right knee, this is hypertrophy of the right atrium, if in the left knee, this is hypertrophy of the left atrium.
If the P wave is reduced, this indicates atrial dystrophy (decreased atrial myocardial mass).
There is no P wave – the sinus node is not working.
The impulse then goes to the AV junction. There is no depolarization or repolarization. On the ECG this corresponds to the PQ interval - resting potential.
The impulse then goes to the interventricular septum.
Classification and types
There are several types of classifications to determine the type of arrhythmia
They are important for establishing the cause of the pathology, accurate diagnosis, treatment approach and further prognosis.
According to the frequency of occurrence, the following ventricular extrasystoles are distinguished:
- rare (less than 5 per minute);
- medium frequency (up to 16/min);
- frequent (16 or more).
By density:
- single;
- pairs;
- group.
By localization:
- right ventricular;
- left ventricular.
By localization of excitation:
- monomorphic (arise from one focus, have the same appearance on the ECG);
- polymorphic (different places of origin, complexes differ markedly when registered).
According to the rhythm of appearance:
- bigeminy (every second contraction is an extrasystole);
- trigeminy (every third);
- quadrigeminy (fourth);
- sporadic (excitations without a clear sequence).
According to the degree of danger, there are the following classes:
- Benign ventricular extrasystoles. They occur in the absence of myocardial damage or hypertrophy, their frequency does not exceed 10 per hour, and are not accompanied by impaired consciousness.
- Potentially malignant. Against the background of left ventricular dysfunction, with a frequency of 10 or more per minute. No fainting or cardiac arrest.
- Malignant. Frequent, polymorphic and polytopic, against the background of significant deviations (ejection fraction of 40% or less), turn into stable ventricular tachycardia. The medical history contains a description of impaired consciousness and (or) cardiac arrest.
Ryan gradation
My colleagues and I still use the classification of ventricular extrasystole (VC), proposed by M. Ryan in 1975; it is intended for patients who have a history of myocardial infarction. According to this gradation, the following degrees of arrhythmia development are distinguished:
| Stage | Description of extrasystoles |
| There are no episodes of sudden contractions | |
| 1 | Number does not exceed 30 per hour, monotopic |
| 2 | More than 30 extrasystoles in 60 minutes, monotopic |
| 3 | Multifocal, frequent |
| 4a | Paired monotropic |
| 4b | Polymorphic, paired and grouped with flickering and fluttering |
| 5 | Early, salvo, polymorphic, turning into paroxysm of ventricular tachycardia |
S wave
S wave:
- depth up to 8-12 mm
- duration 0.03 sec
The S wave is the potential being tested; this is the time when the ventricles are completely engulfed in excitation. It has no independent meaning.
The QRS complex is of great importance, which corresponds to intraventricular conduction equal to 0.1 sec, and with hypertrophy it can be up to 0.12 sec. If the QRS complex is more than 0.12 seconds, this is an intraventricular block or a violation of intraventricular conduction.
Next, the depolarization process is completed; on the electrocardiogram this corresponds to the ST interval. This means that the cell membrane is completely recharged.
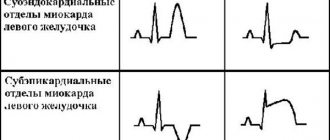
How to “read” myocardial infarction on an ECG?
Students starting to study cardiology often have a question: how to learn to read a cardiogram correctly and identify myocardial infarction (MI)? You can “read” a heart attack on a paper tape based on several signs:
- ST segment elevation;
- peaked T wave;
- deep Q wave or lack thereof.
When analyzing electrocardiography results, these indicators are first identified, and then the others are dealt with. Sometimes the earliest sign of acute myocardial infarction is only a peaked T wave. In practice, this is quite rare because it appears only 3-28 minutes after the onset of a heart attack.
Peaked T waves should be distinguished from peaked T waves associated with hyperkalemia. In the first few hours, the ST segments usually rise. Pathological Q waves may appear within a few hours or after 24 hours.
Long-term ECG changes such as persistent Q waves (93% of cases) and spiky T waves are common. Sustained ST segment elevation is rare except in ventricular aneurysms.
Indicators of myocardial infarction on ECG
There are widely researched clinical solutions, such as the TIMI score, that help predict and diagnose myocardial infarction based on clinical data. For example, TIMI scores are often used to predict the status of patients with symptoms of MI. Based on symptoms and electrocardiographic findings, practitioners can differentiate between unstable angina and MI in the emergency setting.
Diagnosis based on ECG data and types
The category of patients with symptoms of extrasystole requires a thorough study of the rhythm. A cardiogram is one of the main methods for diagnosing ventricular extrasystoles. The electrocardiography method makes it possible to take a detailed approach to the manifestation of disorders in the heart and identify the types of extrasystoles.
Usually, when atrial pathology appears in the cardiogram against the background of sinus rhythm, QRS complexes with changes in the P wave and prematurely occurring QRS complexes are found. After it, a compensatory pause occurs, which means atrial extrasystole.
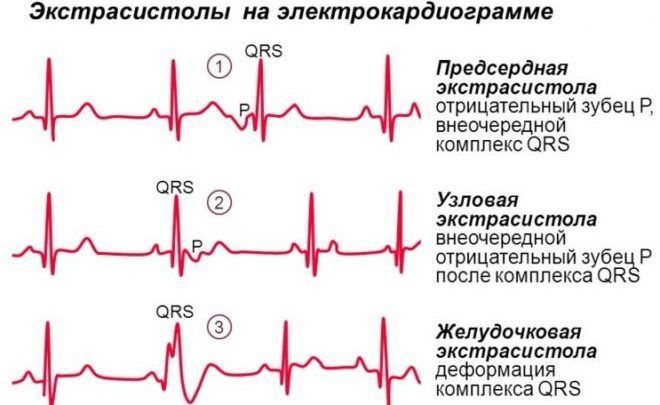
Supraventricular extrasystoles
Nodal contractions occur in the atrioventricular node. Such changes are called supraventricular extrasystoles. They are divided into:
- upper node;
- mid-nodal;
- inferior nodes.
Supernodal extrasystole on the ECG is characterized by the fact that the P waves before the premature QRS complex arise with a negative phase. After the QRS complex, an incomplete compensatory pause occurs.
Classification and differences between species, stages
Based on the number of extrasystolic contractions that occur one after another, single atrial extrasystoles, paired and triplets are distinguished, when three extraordinary contractions appear in a row. Triplets are considered as unstable tachycardia.
Extrasystoles that occur with a certain pattern are called allorhythmia, which is divided into the following types:
- bigeminy, in which a pathological impulse follows every normal one;
- trigeminy, when extrasystolic contraction is every third;
- quadrigeminy – every fourth.
Based on the place of origin, monotopic ones are distinguished - from the same area, and polytopic ones - from different ones.
According to the degree of extrasystole, extrasystole is distinguished, focusing on the relationship with the previous ventricular complex; early and late are distinguished.
The stages of atrial extrasystoles reflect the number of early contractions that occur in one hour: with the first, no more than 30 are allowed to appear, with the second - over 30, then polytopic and paired extrasystoles are considered.
Types of ECG tests
An electrocardiograph is used to perform the standard procedure. Such devices are widely used in cardiology hospitals, as well as in ambulances. Using suction cups, the electrodes are attached to the human body, and then electrical potentials flow through them.
The electrodes are usually called “leads”; a total of 6 of them are installed. The leads attached to the limbs are considered the main ones and are designated I, II, III and aVL, aVR, aVF. On the chest, the electrodes are marked V1-V6.

Each type of lead has a specific task, so individually the factors give different values. The doctor needs to combine all the information into one whole and decipher the cardiogram.
The graph is displayed on special graph paper. Each lead has its own schedule. In standard applications, the belt speed is set to 5 cm/s, which can be adjusted if necessary.
Holter monitoring
Unlike the standard procedure, which lasts several minutes, during Holter monitoring, information is recorded throughout the day. The duration of the procedure is explained by the need to obtain a complete picture of the processes occurring in the heart. This procedure can take readings not only when a person is calm, but also during physical activity.

Some diseases are difficult to detect during a regular cardiogram, since deviations can only appear during activity.
Other types of procedures
There are also specific procedures for obtaining a cardiogram:
- Monitoring with exercise. In this way, it is easier to establish pathologies in the functioning of the heart. A treadmill is used for such monitoring; it helps give the body the required load. The procedure is used in situations where pathologies appear only during accelerated heart function.
- Phonocardiography. Using this method, you can study not only electrical indicators, but also the noise that occurs in the cardiac region. This method is used to diagnose heart defects.