Endocarditis is an inflammation of the inner lining of the heart, which negatively affects the smoothness and elasticity of the muscle chambers. This disease has many causes, including rheumatism. In this case, the inflammatory process affects the parietal endocardium, connective tissue of the valves, and tendons. Any rheumatism always negatively affects the condition of the heart, and this condition is especially common in young people and children.
Characteristics of the pathology
Rheumatic endocarditis mainly progresses in the valvular apparatus of the myocardium. Over time, the pathology can spread to the chordal filaments and the parietal endocardium of the ventricles or atria. This disease belongs to rheumatism syndromes. Endocarditis, if not treated promptly, during scarring can change the appearance of the valve, disfiguring it for the worse. In this case, problems may arise with closing the special hole, which leads to valve insufficiency, that is, blood circulation becomes more difficult. Subsequently, such a pathology can cause stenosis of the orifice, which also negatively affects the full flow of blood.
The rheumatoid process very often leads to shortening of the tendon threads, which also ends in valve insufficiency. The narrowing of the openings is mainly a consequence of the fusion of individual leaflets or valves. Experts have found that endocarditis is always accompanied by similar myocarditis.
Rheumatic endocarditis is one of the most common heart diseases; only congenital myocardial defects are more common.
Types of disease
Experts divide the disease into 4 types:
- Acute warty endocarditis. In this case, the deep layers of the endothelium are affected. Gray-brown formations, similar to warts, begin to appear on certain areas of the organ. If therapy is not started in time, these formations become larger and merge with each other, which leads to the occurrence of polypous endocarditis.
- Recurrent wart. This type of endocarditis differs from the previous one in that it progresses on valves affected by sclerosis.
- Simple endocarditis is characterized by tissue swelling and does not have deep lesions. Timely therapy guarantees rapid recovery of the myocardium and its structures without complications and consequences.
- Fibroplastic endocarditis is a consequence of any of the above types of diseases that were not treated in time. In this case, complications and negative consequences are possible.
Fibroplastic, simple, recurrent and acute wart endocarditis are diseases that require only diagnosis from a specialist and do not accept self-medication.
In patients over 30 years of age, the valves are damaged in 30% of cases after a rheumatic attack on the heart, and in children - in 90%.
Symptoms of rheumatic endocarditis
Due to the progression of rheumatism, a person develops a number of symptoms that indicate the occurrence of disturbances in the structure of the heart structures. Most often, the patient begins to complain of the following symptoms:
- increased heart rate;
- the appearance of pain in the heart;
- deterioration of general condition;
- increased temperature for a long time;
- the appearance of systolic, protodiastolic murmur in the bicuspid valve or diastolic murmur in the aorta;
- increased heart rate;
- the appearance of various forms of arrhythmia.
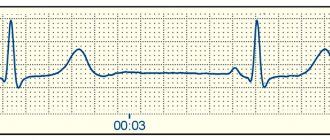
When conducting an examination of the body, the presence of atrioventricular blockade of varying degrees is revealed. This symptom is quite easily detected by taking an electrocardiogram of the heart. Sometimes auscultation may reveal a pericardial friction rub. There are cases of disease progression when this symptom is the main one that determines the presence of the disease in the body.
The progression of rheumatic endocarditis can provoke the appearance of various disturbances in the functioning of different organs of the body, however, these symptoms, as a rule, have little effect on the formation of the clinical picture of the disease.
One of the most significant changes detected during the examination is moderate leukocytosis and an increase in the erythrocyte sedimentation rate. Patients, as a rule, recover, but as a result of the development of rheumatic endocarditis, a defect in the valve mechanism of the heart remains.
Sometimes recurrent endocarditis can develop, which is an acute outbreak of the disease. The clinical picture of this type of disease is practically no different from that described above. The only difference is the possible appearance of pain in the joints. As the disease develops, the temperature may rise, which can last from half a week to two weeks. Sometimes there are cases of damage to the endocardium without an increase in body temperature.
It is quite difficult to recognize rheumatic endocarditis in the first 4-6 weeks of development even with additional studies. This is due to the fact that all identified symptoms are also characteristic of rheumatism, which develops without damage to the endocardium. The appearance of diastolic murmur indicates that valvulitis is developing in the body.
What is the basis of pathology
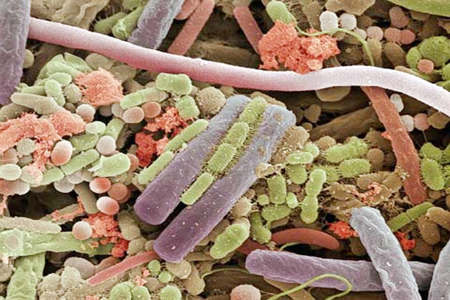
Streptococcus bacteria are the cause of the disease
The main and main cause of rheumatic endocarditis is group A streptococcus. This is especially a common manifestation of endocarditis in children, since they can get tonsillitis or pharyngitis, if treatment is not started in time, the disease can cause serious complications.
To cope with the infection on its own, the body begins to actively produce antibodies that can attack the cardiovascular system, which causes an inflammatory process and leads to rheumatism.
The parts of the heart affected by the disease include:
- Tendon chords.
- Aortic valve.
- Deep layers of the heart.
- Mitral valve.
- Parietal endocardium.
- Tricuspid valve.
In this regard, rheumatic inflammation of the heart tissue proceeds differently than the infectious and septic varieties of the disease, but the main cause is still streptococcus that has entered the body.
What it is?
In general, endocarditis is a pathology of the valve apparatus of the endocardium, in which inflammation of the connective tissue develops.

The rheumatic variety is a common manifestation of rheumatism and has an infectious-allergic mechanism.
The most often affected are the mitral and aortic (separately or both at the same time) valves, somewhat less frequently – the tricuspid, and very rarely – the pulmonary trunk. The causative agent of rheumatic endocarditis, as a rule, is beta-hemolytic type streptococcus. When it enters the body, an immune response begins in the form of antibodies. In cases where the body's sensitivity is increased, the process of producing antibodies is overly active. They begin to attack not only the infection, but also connective tissue cells, often in the cardiovascular system. This is how the inflammatory process (rheumatism) begins.
As a result of this failure of the immune system, the heart valves are often damaged. At the initial stage, damage to the surface tissue occurs (swelling of collagen fibers, proliferation). Fibrin and platelets accumulate in areas of the valves, and tissue edema occurs. Gradually, the walls of the valves thicken, become deformed and scar, which leads to various heart defects.
Clinical picture as a fact
Endocarditis very often begins completely unexpectedly and may not manifest itself for a long time. In most cases, the disease is long-term and acute, has different types of manifestations, which very often complicates diagnosis.

When the body becomes very weak, you should immediately see a specialist!
Over the course of two weeks, the clinical picture of the disease develops, at which time the patient notices fever, chills and excessive sweating. Body temperature constantly changes its values; it can be quite high for a long time and slightly elevated for several days, followed by normalization. During endocarditis, the following symptoms are noted:
- Decreased appetite, red eyes.
- Muscle, chest, abdominal and joint pain.
- Arthritis of the joints of all extremities and visible changes in the phalanges of the fingers and nails.
- Progressive heart failure, heart murmurs.
- Renal dysfunction caused by nephritis or heart attack.
- Enlarged lymph nodes and damage to the central nervous system.
- Pericarditis, damage to the aortic or mitral valve.
- Increased heart rate, arrhythmia and increased heart rate.
Intoxication of the body is noted: loss of strength, decreased performance, weight loss, anorexia, headaches, arthralgia. Changes that appear on the skin are hemorrhagic rashes, redness on the palms of the hands, soles of the feet and body, pale skin with yellowing.
The consequences of the disease depend on its course and what form the pathology is in. Experts include children under 7 years of age, adolescents and older people who have had infectious diseases at risk.
Read also: Infectious endocarditis abstract
Causes
Endocarditis is largely associated with a variety of infections that can be acute or chronic. There are also secondary endocarditis, which are usually combined with diffuse connective tissue diseases. Today, ICD-10 lists the following groups of infections that most often lead to the development of endocarditis:
- candida;
- gonococcal;
- meningococcal;
- tuberculosis;
- syphilis;
- typhoid fever;
- Libman-Sachs disease.
Many changes in the endocardium are associated with rheumatism and rheumatoid arthritis. These diseases often develop due to streptococcal infection, which spreads throughout the body and settles in various organs and tissues. Under favorable conditions, streptococci on the endocardium cause inflammation with all the ensuing consequences.
Staphylococcus aureus and enterococcus often act as etiological factors. They are mainly isolated in acute endocarditis. Pathogens that cause endocarditis also include beta-hemolytic streptococcus, Escherichia coli and Pseudomonas aeruginosa.
The causative agents of the disease can be ordinary “residents” of the skin, mucous membrane, and gastrointestinal tract, which, with weakened immunity or changes in internal environmental conditions, begin to behave as pathogenic microflora.
Development factors
One of the conditions for the development of endocarditis is bacteremia, which is detected over a long period of time. Its occurrence may be associated with chronic foci of infection such as periodontitis, tonsillitis, and furunculosis. Manipulations could also be carried out that introduced pathogens into the body. This happens during surgical interventions, catheterization, bronchoscopy, intravenous administration of drugs or drugs.
The process is more active if the valves were previously changed due to rheumatism or congenital defects. The use of prosthetic valves also contributes to the development of endocarditis.
The pathological process is directly related to destructive ulcerative inflammation of the endocardium, which is accompanied by the deposition of platelets along with fibrin, bacteria and tissue particles. As a result, in addition to EC, a disease such as thromboembolism may develop. The addition of autoimmune mechanisms associated with the circulation of immune complexes and the development of an appropriate response to them to the inflammatory process leads to aggravation of the course of endocarditis.
What does the outcome depend on?
Before you find out what the outcome of rheumatic endocarditis depends on, you need to understand what this pathology is. Pathological disorders are localized in the myocardial valves at the initial stages of development, and as they progress, they spread to the atrium ventricles (the region of the parietal endocardium) and chordal filaments. The disease is a rheumatism syndrome that appears against the background of infection. Over time, tissue scarring occurs, which leads to deformation of the valve. In this case, the hole is blocked, organ failure occurs, and blood circulation is disrupted. There is a risk of developing stenosis. Next, the tendon threads begin to shorten, and the flaps or valve fuse.
Why is this happening? The fact is that at the very beginning of the development of pathology, collagen fibers undergo swelling, which causes a proliferative reaction. This leads to a change in the surface of the valve, and in places where the valves touch, fibrins and platelets accumulate and settle. As a result, warty growths are formed. Under these warts, swelling of the tissue occurs, leading to scarring.

The prognosis largely depends on the symptoms that appear, which may indicate certain pathological changes. The patient may experience the following:
- increased heart rate;
- pain in the heart area;
- acceleration of pulsation;
- shortness of breath and impaired breathing abilities;
- weakness and fatigue;
- high body temperature;
- diastolic, protodiastolic and systolic murmurs.
If the body of such a patient is examined, atrioventricular blockade and friction noise of such an element as the pericardium are detected. To do this, it is enough to do an electrocardiogram.
Endocarditis - symptoms, types, causes and treatment of endocarditis
Good day, dear readers!
In today's article we will look at a heart disease such as endocarditis, and everything that is associated with it - symptoms, signs, causes, classification, treatment, folk remedies, prevention and other information. So…
What is endocarditis?
Endocarditis is a heart disease characterized by inflammation of its inner lining (endocardium).
The endocardium is the inner layer of the lining of the heart, consisting of endothelium, lining the cavities of the heart - the atria and ventricles.
In most cases, endocarditis is not an independent disease, but acts as a concomitant pathological process of another disease.
The most common cause of endocarditis is infection - bacteria, fungi and other pathogens, and therefore, many sources consider this disease as infective endocarditis. However, pathologies (congenital or acquired) of the heart valves can be considered an equally important cause of the disease.
The main symptoms of endocarditis are increased and high body temperature, general pain and malaise, chills, weakness, shortness of breath, pain in the heart and other signs characteristic of infectious and heart diseases.
Development of endocarditis
The pathogenesis of endocarditis has not been fully studied, but we will try to describe it in general terms, focusing on the development of infective endocarditis (IE).
The development of the disease is based on two fundamental factors - damage to the endocardium and heart valves, as well as bacteremia.
1.
Destruction of valves and damage to the endocardium leads to turbulence in the transvalvular blood flow, which changes the structure and shape of endothelial cells, between which pores are formed, which later become the “gate” for the penetration of lymphocytes and macrophages. Adhesion processes occur. Thrombosis develops on the endothelium of the damaged area of the myocardium, and the endocardium is penetrated by fibrin threads. This process leads to inflammation of the endocardium, destruction of the valves and the development of heart failure.
2. When the body becomes infected, pathogenic microorganisms often enter the bloodstream, where they can “travel” for quite a long time, infecting more and more tissues and organs. No exception is the infection getting into the heart muscle (myocardium), which actually sets the blood in motion.
The main factors contributing to the development of bacteremia: infectious diseases, especially chronic ones (acute respiratory infections, meningitis, caries and others), surgical treatment (adenoidectomy, tonsillectomy, cardiac catheterization, dental procedures), various examination methods (colonoscopy, bronchoscopy, gastroscopy).
It is also important to note that increased resistance of the body to bacteremia is observed in people with impaired immune function, people with alcohol or drug addiction, hypothermia, frequent stress, during immunosuppressive therapy, as well as the elderly.
3. The entry of bacteria into the area of already damaged valves and inflamed endocardium increases adhesion. Microbes adhere to thrombo-fibrin overlays, settle in this place and increase their popularity.
Thus, we can conclude that the development of infective endocarditis is caused by primary or secondary damage to the inner wall of the myocardium (endocardium), impaired functioning of the immune system, and bacteremia.
Endocarditis - symptoms
The course of the disease can occur with minimal symptoms, or even without them, which largely depends on the state of the person’s health and the severity of the pathological factors involved in the development of endocarditis.
The main signs of endocarditis are:
General – weakness, malaise, soreness, increased and high body temperature (38.5-39.5 ° C), severe chills, profuse sweating, rheumatism, headache, muscle and joint pain, anorexia, arthralgia.
From the cardiovascular system - heart pain, pronounced heart murmurs, myocarditis, pericarditis, abscesses, damage to the aortic and mitral valves, cardiac decompensation, thrombosis, thromboembolism, vasculitis, aneurysm, increased fragility of blood vessels, minor hemorrhages in the mucous membranes (conjunctiva and etc.).
From the central nervous system - meningitis, cysts, acute cerebrovascular accidents (ACVA), psychosis.
On the part of the skin - the skin acquires a pale gray-yellow color, abscesses, purpura, Osler's nodes, hemorrhages.
From the kidneys - nephritis, glomerulonephritis, hematuria, proteinuria, abscesses.
From the lungs - abscess, pleurisy, pneumonia, polyserositis, empyema.
Other signs are enlarged lymph nodes, arthritis of the joints of the hands and feet, polyarthritis, changes in the structure of the nail plates and phalanges of the fingers (symptom of “drum fingers”), infarctions (myocardium, kidney, spleen, lungs, intestines), angina pectoris.
Blood tests show leukocytosis, increased ESR, severe hypochromic anemia, circulating immune complexes. Monocytosis, increased α2- and γ-globulinemia, C-reactive protein, thrombocytopenia may also be observed.
Endocarditis - complications
Source: https://medicina.dobro-est.com/endokardit-simptomyi-vidyi-prichinyi-i-lechenie-endokardita.html
In adults
If rheumatic endocarditis progresses and there is no adequate treatment, pathological disorders affect not only the cardiovascular system, but also other internal organs. But it is known that the main cause of this disease is infection with streptococci from group A. Consequently, infection of the entire body is possible. Therefore, it is not surprising that such a complication as valvulitis is discovered.
During the course of the disease, the erythrocyte sedimentation rate increases, and leukocytosis becomes moderate. After therapy aimed at restoring these processes, the patient is cured of endocarditis, but the defect still remains in the valve mechanism of the heart.
If the treatment of rheumatic endocarditis was not carried out in a timely manner, or the patient simply did not complete treatment, secondary endocarditis (recurrent) occurs in the future. If we talk about the clinical picture, it does not differ from the primary manifestation of the pathology, but is aggravated by the fact that the joints begin to be affected, which is why severe pain appears in them.
The most common outcomes of rheumatic endocarditis in the adult population:
- Congestive heart failure (HF) develops due to valvular incompetence. If the mitral and aortic valves are affected, and an acute and subacute course of the pathology is noted, then congestive heart failure develops very rapidly. This outcome is observed in 55-60 percent.
- Embolism occurs in 40% of all cases of rheumatic endocarditis. The blood vessels of the brain, kidneys, spleen, retina of the visual apparatus, and mesentery are affected. As a result, partial or complete blindness, stroke and heart attack, kidney failure, and acute abdominal syndrome occur.
- 25% is given to diseases of an autoimmune nature - allergic myocarditis, pericarditis, glomerulonephritis, inflammatory pathologies of the joints, effusions in the joint capsules.
- In only 10 percent, peripheral arteries are affected, resulting in an aneurysm in the vessels of the brain. And this is fraught with bleeding, ruptures and death.
Pediatric endocarditis is considered a dangerous condition because it is difficult to treat. Children get sick much more often than adults because their immune system is not yet fully developed. Because of this, the body is exposed to colds and infections, against which rheumatic endocarditis develops.
Early diagnosis is complicated by the fact that the main symptoms are similar to those of many other pathologies. In preschool age, healthy valves are most affected, and in older age, heart disease is also detected.

As a rule, such children are constantly monitored by doctors. In addition, they must periodically undergo prophylaxis.
If we talk about the recovery rate in childhood, it is a minimum of 35-40%, and a maximum of 85. This depends on the severity of the disease, the type of infection and many other factors. If treatment is not started in a timely manner or the wrong drugs are used, the prognosis will be worse. Therefore, it is strictly forbidden to engage in independent therapy. In this case, you need to completely rely on the opinion of doctors.
Read also: Staphylococcal endocarditis
Prognosis and Prevention
The prognosis of endocarditis depends on the degree of damage to the endocardium, especially the valve apparatus, as well as the timeliness of treatment.
Prevention coincides with the prevention of those diseases in which inflammation of the endocardium is observed. Prevention of bacterial endocarditis - see Subacute bacterial endocarditis.
Bibliography:
Anokhin V.N. et al., Infectious endocarditis - diagnosis, features of the current course and issues of therapy, Ter. arkh., t. 53, no. 7G p. 53, 1981; Gritsman H. N. Heart lesions in collagen diseases, M., 1971; Kopyeva T. N. Pathology of rheumatoid arthritis, M., 1980; Kurashova M.V. and Belova E.V. Leffler's syndrome, Klin, med., t. 53^ No. 3, p. 13, 1975; Permyakov N.K. About some features of septic endocarditis after abortion during treatment with antibiotics, Sov. med., No. 1, p. 50, 1957; Popov V. G., Aksenova G. A. and Tribunov Yu. P. Features of the clinical picture and course of infective endocarditis in elderly and senile patients, Ter. arkh., t. 53, no. 5, p. 81, 1981; Private allergology, ed. A. D. Ado, p. 293, M., 1976; Yarygin N. E., Nasonova V. A. and Potekhina R. N. Systemic allergic vasculitis, M., 1980; Infections of prosthetic heart valves and vascular grafts, ed. by RJ Duma, Baltimore ao, 1977; Major RH, Notes on history of endocarditis, Bull." Hist. Med., v. 17, p. 351, 1945; About 1-ney BA ao The consequences of the inconsequential: Marantic (nonbacterial thrombotic) endocarditis, Amer. Heart J.* v. 98, p. 513, 1979; W a 1 sh TJ ao Fungal infections of the heart, Amer. J., Cardiol., v. 45, p. 357, 1980; Weinstein L. a. Schlesinger J. J* Pathoanatomic, pathophysiologic and clinical correlations in endocarditis, New Engl. J. Med., v. 291, p. 832, 1974.
A. V. Sumarokov; A. B. Shekhter (pat. an.), H. E. Yarygin (all.)
Does the outcome of the disease depend on its type?
The outcome of rheumatic endocarditis depending on the type of disease:
- In the acute warty form of the pathology, the deepest layers of the endothelium are affected, resulting in growths of considerable size. They have a gray-brown tint and a dense structure. Over time, the warts grow and stick together, developing polypous endocarditis.
- In the recurrent warty form of rheumatic endocarditis, the valves are affected by sclerosis.
- If the disease is simple, there is no deep damage, then the tissues swell. As a rule, the outcome is quite favorable, subject to adequate and timely treatment.
- With the fibroplastic form of rheumatic endocarditis, there is a risk of all complications. Therefore, this type requires special therapeutic intervention.
Treatment of Loeffler's endocarditis
Treatment of fibroplastic endocarditis involves the use of the following groups of drugs:
- diuretics, ARBs, ACEs - reduce afterload;
- beta blockers are used to control heart rate;
- cardiac glycosides;
- to reduce the risk of blood clots and stop this process, heparin-based drugs and anticoagulants are prescribed;
- if there are diseases of an autoimmune nature, the doctor will definitely prescribe glucocorticoid medications, as well as immunosuppressive therapy;
- if rheumatoid arthritis is observed, then antibodies to necrosis are administered;
- cytostatic therapy is used in the presence of eosinophilic leukemia.
If drug therapy does not give a positive result or there are contraindications to taking the necessary groups of drugs, as well as in advanced cases of the disease, surgical intervention . Endocardial decortication is performed in one or two ventricles, depending on the lesion. The operation makes it possible to alleviate the patient’s condition and neutralize the main symptoms. The fatality rate is decreasing. An endocardectomy may also be prescribed, during which plastic surgery of the atrioventricular valves is also performed.
How to increase the chances of a favorable outcome?
In order to achieve a favorable outcome, it is necessary to promptly pay attention to symptoms, undergo diagnostic measures and carry out appropriate treatment.

In general, you need to do the following:
- Physical activity is limited, in some cases eliminated altogether.
- Stressful situations must be avoided.
- You will have to adhere to the diet prescribed by your doctor. Salty, fatty, fried, smoked and canned foods are excluded. You cannot drink alcoholic beverages or smoke.
- It is imperative to adhere to drug therapy. Most often, rheumatic endocarditis occurs against the background of beta-hemolytic streptococci, so benzylpenicillin solution is injected intramuscularly four times a day for at least 10 days. It is mandatory to take glucocorticosteroids, which eliminate the inflammatory process in the heart muscles. For this purpose, the drug Prednisolone is prescribed in tablet form. The tablets are taken on an empty stomach once a day.
- If there is a risk of an unfavorable outcome, the doctor prescribes surgery. Most often this happens in the presence of purulent accumulations, the rapid development of complications and massive growths. The operation is considered complex, since it is an open method - the chest cavity is opened, the patient is connected to the artificial circulation system, after which the surgeon cleans the valves and cuts out the damaged areas. If necessary, an organ is implanted.
- It is very important to strengthen the immune system, so the patient is recommended to take vitamin complexes and hardening.
- During treatment, the recovery period and further time, the patient must visit a doctor for a preventive examination.
The outcome for a person’s life with rheumatic endocarditis is quite favorable, but complete recovery is difficult to achieve. For older people, the prognosis is less favorable than for younger people. But the most important thing is timely and adequate treatment. Thus, the outcome largely depends on the patient himself and the prescribed therapy.
Features of the disease
It should be noted that patients initially experience swelling of collagen fibers followed by a proliferative reaction. In the early stages, the surface of the valve begins to change. At the points of contact of the valves, platelets and fibrin begin to accumulate and settle, which leads to the appearance of growths (warts). The valve tissue under the growths is swollen. The tricuspid valve leaflets are subject to rheumatoid changes half as often as those of the mitral valve. Subsequently, the valves become scarred, wrinkled and deformed, and thickening or fusion of the walls is observed. This leads to the development of heart disease.
As a result of rheumatic endocarditis, valve insufficiency or stenosis may develop. Insufficiency is the incomplete closure of the valve leaflets, and stenosis is the narrowing of its opening. The most common complication is mitral valve insufficiency of the heart muscle.
Most often, rheumatic endocarditis develops between the ages of six and sixteen years, but recently there has been a decrease in the incidence in children. There are no specific features of the disease in children and adults; it progresses in exactly the same way.
Clinical picture of rheumatic endocarditis

Types and forms
According to the foci of occurrence, rheumatic endocarditis can be:
The valve is considered the most common. In turn, it is divided into four categories:
- diffuse (valvulitis according to the classification of V. T. Talalaev). Affects the valve leaflets, but without the formation of growths;
- sharp warty. It occurs with damage to the endothelium and the formation of warts on the trailing edge of the valve leaflets;
- fibroplastic. Appears as a consequence of the two forms described above and is characterized by fibrosis and scarring;
- recurrent verrucous. Occurs repeatedly on altered valve flaps. Accompanied by the new appearance of growths.
Causes of rheumatic endocarditis
Doctors believe that the main cause of rheumatism is group A beta-hemolytic streptococcus. In childhood, a patient who comes into contact with it can develop pharyngitis or tonsillitis. Without consulting a doctor for qualified help, the disease goes away on its own, but causes consequences.
Heart structures most often affected by rheumatic endocarditis:
- mitral valve;
- tricuspid valve (usually in combination with other localizations);
- aortic valve;
- parietal (parietal) endocardium;
- chordae tendineae;
- deep layers of the myocardium.
Therefore, with rheumatic endocarditis, inflammation occurs a little differently and differs from the infectious and septic varieties, although the initial cause of its appearance was the entry of streptococcus into the body. Read more about the symptoms and signs of endocarditis in children and adults.
Read also: Tricuspid valve endocarditis
The symptoms of all forms of endocarditis are very similar and very often do not indicate its rheumatic variety. When examining a patient, a cardiologist usually reveals:
- shortness of breath. Especially during physical activity;
- pain in the heart area. This is not such a common symptom and may appear in the later stages of the disease;
- increased heart rate (tachycardia). The main distinguishing feature of endocarditis is that it has nothing to do with physical stress and is completely independent of body temperature;
- nails in the shape of watch glasses. The nail formations on the fingers expand and become more rounded, the central part of the nail plate rises, forming a dome;
- drumstick-shaped fingers (Hippocratic fingers). A similar symptom may occur in patients at a late stage of the disease. Characterized by the fact that the fingers become narrower, and the last phalanx widens. With rheumatic changes it appears most often. But it also happens with other diseases;
- pale skin. In advanced stages of the disease, blue discoloration of the fingertips and nose may occur;
- fast fatiguability. It appears in the initial stages, especially during physical activity.
One of the main symptoms when diagnosing rheumatoid endocarditis can be a pronounced heart murmur, which appears in the fifth week after the onset of the process.
When taking a blood test, an increased number of leukocytes is detected. C-reactive protein appears and fibrinogen levels increase. Distinct conduction disturbances appear on the ECG.
ENDOCARDITIS
INFLAMMATORY DISEASES OF THE HEART
The wall of the heart consists of three different layers, this explains the frequent development of isolated inflammation of one of them - endocarditis, myocarditis or pericarditis. Under certain conditions, it is possible that all the membranes of the heart may be involved in the inflammatory process (pancarditis).
Endocarditis is inflammation of the inner lining of the heart of various etiologies. It ranks 4th among heart diseases after ischemic myocardial damage, changes that occur with hypertrophy and cor pulmonale.
Men get sick three times more often than women.
The following types of endocarditis are distinguished: infectious septic, non-infectious thromboendocarditis, rheumatic endocarditis, parietal fibroplastic eosinophilic Loeffler endocarditis.
The most common is endocarditis of the heart valves, less often inflammation of the parietal endocardium and endocardium of the chordae tendineae. Often there is a combination of inflammation of these parts of the endocardium.
Infectious septic endocarditis
Infectious septic or bacterial endocarditis morphologically corresponds to ulcerative or polyposis-ulcerative endocarditis. This form of endocarditis occurs with a pronounced hyperergic reaction, until recently it was considered a form of sepsis.
Almost always the cause of septic endocarditis is bacteremia, especially with septicopyemia. In 60–80% of cases, the disease is caused by streptococci and enterococci, in 30% by staphylococci, gram-negative bacteria, pathogenic fungi, and rickettsia.
However, in approximately 10–30% of patients with infective endocarditis, infectious agents are not found in the blood.
Localization of inflammation is the heart valves, much less often - the parietal endocardium. In 70% of cases, infective endocarditis is preceded by other diseases (scarlet fever, diphtheria, pneumonia, tonsillitis, typhoid and typhus, tuberculosis, syphilis, etc.), as well as diseases that cause severe changes in the heart valves.
In 6.5% of cases, endocarditis occurs against the background of congenital heart defects, in 10% - on valves affected by rheumatism, in 6% - with prolapse of the mitral valve leaflets, in 5-9% - with hypertrophic obstructive cardiomyopathy, in 2% of cases - after heart surgery.
Often this endocarditis occurs in those suffering from alcoholism and substance abuse, in patients receiving hemodialysis or immunosuppressive therapy.
Pathogenesis . Immune complex mechanisms play a leading role in the development of acute infective endocarditis. According to the nature of the course, the following forms of infective endocarditis are distinguished: acute bacterial endocarditis (duration about 2 weeks), subacute infective endocarditis (up to 6 weeks, occasionally up to 3 months), prolonged septic endocarditis (for many months and years).
● Acute bacterial endocarditis usually occurs on intact heart valves with severe infections and septicopyemia. In 80% of cases it is caused by Staphylococcus aureus, in 20% by other pathogens - pneumococci, gonococci, pathogenic fungi, rickettsia. Ulcerative or ulcerative-polyposis changes occur on the endocardium of the valves, quickly forming a heart defect.
◊ Macroscopically, at the beginning of the process, small granular formations ranging in size from several millimeters to a centimeter or more, yellow or dark brown in color, are visible along the edges of the cusps of the mitral and sometimes aortic valves.
Beneath them, ulcerative defects of the valves are found. With enlargement, these defects spread deeper and can spread to the tendon chords and parietal endocardium.
Often, ulceration of the valve leaflets leads to the appearance of their aneurysm, and in 50% of deaths - perforation of the valve leaflets. Blood clots appear along the edges of ulcerative defects (polyposis-ulcerative endocarditis).
In acute endocarditis caused by bacteria or rickettsia (for example, with Q fever), the volume of thrombotic masses is relatively small, and in fungal endocarditis, polypous growths can be large and loose.
◊ Microscopically, colonies of bacteria and thrombotic masses are often visible on the necrotic surface of the valve.
The valve tissues are swollen, permeated with fibrin, often infiltrated with neutrophilic leukocytes (the latter are sometimes absent). Occasionally, histiocytes and fibroblasts are found in the infiltrate.
When the process subsides, the organization of thrombotic masses, petrification of bacterial colonies, wrinkling and deformation of the valve leaflets usually occurs (Fig. 10-15).
Rice. 10-15. Polypous-ulcerative endocarditis of the sclerotic valve. Hematoxylin and eosin staining (x40).
◊ Complications of acute bacterial endocarditis: separation of part of the valve, chordae tendineae, pieces of blood clots with the development of thromboembolic syndrome, including myocardial infarction.
During embolism with infected thrombotic masses, small abscesses may occur in the myocardium.
It is possible to develop diffuse proliferative glomerulonephritis and Osler's nodes in the skin as a manifestation of hypersensitivity.
● Subacute infective endocarditis is diagnosed in 50% of cases of septic endocarditis, less frequently in recent years. The process occurs on both sclerotic and unchanged heart valves.
Inflammation is often isolated in the aortic, less often in the mitral valve and leads to the development of a corresponding heart defect. Morphologically, it is usually polyposis-ulcerative endocarditis.
Foci of necrosis with mononuclear infiltrates around them are also found in the parietal endocardium and trabeculae.
● Prolonged septic endocarditis, or sepsis lenta
accounts for 45% of all infective endocarditis. In 50% of cases it is associated with viridans streptococcus.
As a rule, prolonged septic endocarditis occurs on valves that are sclerotic and deformed as a result of atherosclerosis or syphilis, sometimes with congenital valve defects (secondary endocarditis). However, in 18–25% the disease occurs on unchanged valves (primary endocarditis, or Chernogubov’s disease). At the end of the twentieth century.
Primary endocarditis has become more common than secondary endocarditis. Primary endocarditis is observed in younger people, while secondary prolonged septic endocarditis occurs more often in people over 50 years of age. Isolated valve damage is diagnosed in 73% of cases.
Of these, the aortic valve is affected in 53%, and the mitral valve in 16% (usually with sepsis in drug addicts or as a complication of intracardiac catheterization). Combined damage to the mitral and aortic valves is noted in 27% of cases, tricuspid - in 19%.
◊ Protracted septic endocarditis is characterized by ulcerative defects of the valve leaflets, chordae tendineae, and sometimes the parietal endocardium with massive dryish crumbling thrombotic deposits.
There are lymphohistiocytic infiltrates around the foci of necrosis, sometimes giant cells and colonies of microorganisms are visible in thrombotic overlays, but there are no neutrophils in the infiltrate. Then, under thrombotic deposits, granulation tissue appears, which, as it matures, wrinkles the valve.
Valve deformation is enhanced by the organization of thrombotic masses. The disease is characterized by a chronic relapsing course, so in the valve one can simultaneously see organized and fresh blood clots, scarring and fresh areas of necrosis and ulceration.
There are changes in the valves, chordae tendineae, and parietal endocardium that reflect immune inflammation: areas of swelling and disorganization of connective tissue, lymphomacrophage infiltration, and sometimes small thrombotic deposits on the unchanged endocardium.
◊ Complications and causes of death of patients are the same as for subacute infective endocarditis. Typically, these two forms of endocarditis are clinically considered as one disease.
Non-infectious thromboendocarditis
Non-infectious thromboendocarditis (abacterial thromboendocarditis, minimal endocarditis) morphologically occurs as polypous or warty. It develops in severely weakened patients, as well as during intoxication.
Characteristic is the formation of sterile thrombotic deposits on the endocardium of valves, mainly of the left ventricle, without signs of inflammation. Therefore, the name “endocarditis” has only historical significance.
Under the thrombotic warty deposits along the edge of the cusps of the mitral or aortic valves (less commonly, the tricuspid valve), small accumulations of fibroblasts, monocytes and macrophages are visible.
Rheumatic endocarditis
The morphological manifestation of this disease is warty or fibroplastic endocarditis. Rheumatic endocarditis, as well as atypical non-bacterial verrucous Libman-Sacks endocarditis in systemic lupus erythematosus and endocarditis in rheumatoid arthritis, is part of the pathogenesis of the corresponding diseases and the cause of the development of valve defects (see Chapter 16).
Parietal fibroplastic eosinophilic Loeffler's endocarditis
Other names for the disease are fibroplastic parietal endocarditis with eosinophilia, Loeffler's endocarditis. The etiology is unknown. The disease was described by Loeffler in 1936 as a combination of endomyocarditis, blood eosinophilia, eosinophilic vasculitis of the skin and internal organs.
The pathogenesis of Loeffler's endocarditis is associated with immune disorders.
Characteristic is a combination of blood eosinophilia and damage to the parietal endocardium with the subsequent development of its pronounced fibrosis, thickening, and narrowing of the chambers of the heart. The disease ends in heart failure.
It is more correct to talk about endomyocarditis, since the myocardium is almost always involved in the process, especially its subendocardial sections.
The morphogenesis of Loeffler's endocarditis consists of an acute stage, a thrombotic stage and a fibrosis stage.
● The acute (necrotic) stage lasts 5–6 weeks. Inflammation of the parietal endocardium with thrombotic deposits in both ventricles, mainly in the left, especially in the apex region, is characteristic.
Inflammation spreads to the subendocardial parts of the myocardium, where foci of necrosis occur. The infiltrate contains many eosinophils, lymphocytes, plasma cells, and neutrophilic leukocytes.
In addition, endarteritis or panarteritis of the coronary arteries, as well as blood vessels of the skin and internal organs, are possible.
● Thrombotic stage. The cavities of the heart are somewhat narrowed, slight eccentric hypertrophy of the myocardium is possible. Organizing thrombi are visible on the parietal endocardium of the left ventricle, especially in the apex, and in the right ventricle along the afferent tract.
Microscopically, fibrosis of the endocardium of both ventricles is detected. Between the thickened endocardium and myocardium there is a granulation zone. Some muscle fibers are hypertrophied, some are atrophied.
At the site of necrosis, mesh or focal fibrosis occurs, especially in the subendocardial and middle layers of the myocardium, as well as perivascular sclerosis.
● Stage of fibrosis. The chambers of the heart are narrowed, the parietal endocardium of both ventricles is whitish, dense, especially along the afferent tracts and in the region of the apex of the heart. Severe fibrosis of the papillary muscles and chordae tendineae, especially the posterior leaflet of the mitral valve, is often noted, which can result in heart disease.
Possible development of aortic valve disease. Microscopically, pronounced thickening of the endocardium due to sclerosis is noted. Sclerosis in the form of finger-shaped scars extends to the subendocardial and middle layers of the myocardium. Around the sclerotic areas there is moderate lymphohistiocytic infiltration with the presence of individual eosinophils.
The vessels are sclerotic.
Source: https://studopedia.su/18_83364_endokarditi.html
Diagnostics
When diagnosing rheumatic endocarditis, several methods are used:
- examination of the patient. Performed by a therapist or cardiologist. No preliminary diagnosis is made. Necessary for detecting non-cardiac symptoms of the disease and an initial examination of the state of the cardiovascular system;
- analysis of laboratory results. Thanks to the tests, the cause of the disease is mainly revealed. They can be a sufficient argument for making a diagnosis and prescribing treatment. To confirm rheumatic endocarditis, tests must be taken for the titer of streptococcal antibodies and rheumatoid factor;
- bacteriological tests. Blood tests to detect the causative agent of endocarditis;
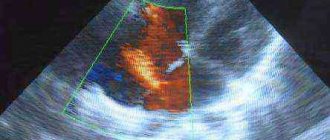
- examination using medical equipment. Cardiac examinations are performed using electrocardiography, echocardiography, radiography, ultrasound, magnetic resonance therapy and computed tomography.
Treatment of rheumatic endocarditis is carried out by all known methods and includes taking medications and following doctor’s orders. If heart failure continues to develop, surgical intervention is performed.
Therapeutic method
Includes fulfillment of such doctor’s requirements as:
- limiting physical activity or completely refusing it;
- avoidance of stress;
- diet, avoiding salt, alcohol, spicy and fatty foods;
- to give up smoking.
Medication method
This method of treating endocarditis involves the use of antibiotics, which are aimed at the complete destruction of beta-hemolytic streptococcus. As we have already mentioned, it is he who causes rheumatic changes in the heart. An intramuscular injection of benzylpenicillin is prescribed. It must be done four times a day for ten days.
After this, treatment with glucocorticosteroid drugs is prescribed. It is aimed at relieving inflammation of the heart muscle. Prednisolone tablets of 20 mg per day are used, you need to drink them one at a time after your morning meal. The main purpose of the patient taking these drugs is to prevent the development of heart disease.
Surgical intervention is performed only in case of unfavorable development of the disease and if the patient’s condition allows. Indications:
- formation and accumulation of pus in the endocardial area;
- heart failure continues to worsen;
- massive growths on the valve flaps;
The operation is performed by opening the chest and connecting the patient to a heart-lung machine. The heart surgeon cleans the valves and removes the affected areas. If necessary, a decision is made to replace severely damaged valves with artificial ones, but this is a separate operation.
Bacterial endocarditis: causes, symptoms and treatment
The development of bacterial endocarditis is mainly associated with other diseases of infectious origin. Sometimes damage to the inner lining of the heart is considered an independent disorder. The development of the disease can occur at any age, even in children, and it is important to start treatment in a timely manner to avoid serious complications.
Bacterial endocarditis (BE) is an inflammation of the heart endothelium (the inner lining of the heart), which often spreads to the heart valves. In severe cases of the disease, a complication such as heart disease often occurs, which in turn can lead to heart failure.
Endocarditis with novolat. endocarditis from ancient Greek. ἔνδον “inside” + καρδία “heart” + itis “inflammation”. Literally means inflammation of the inner lining of the heart - the endocardium.
According to the encyclopedic dictionary of Brockhaus and Efron: in 86 volumes (82 volumes and 4 additional). – St. Petersburg, 1890-1907.
Various diagnostic methods are used to examine patients with suspected EB. First of all, an ultrasound of the heart is done, and this study, if necessary, is supplemented by bacterial blood tests, electrocardiography, and phonocardiography.
: Bacterial endocarditis
Statistics on bacterial endocarditis
- The annual incidence is 5-7 cases per 100,000 (Fraimow 2013).
- In the United States, there are between 40,000 and 50,000 new cases per year, with average hospital charges exceeding $120,000 per patient (Bor 2013).
- It develops more often in men than in women (approximately 1.5:1 – 2:1) (Moreillon 2010).
- In-hospital mortality is 14-22%, with a 1-year mortality rate of 20-40% (Gomes 2017).
- Before the widespread use of antibiotics and surgical treatment, bacterial endocarditis was an almost universally fatal disease (Aretz 2010, Osman 2013).
Description
Bacterial endocarditis can manifest itself in various forms, which largely depends on the nature of the disease:
- Acute form - lasts several weeks.
- Subacute form - lasts for 2-3 months.
- The chronic form can develop over several years and is quite difficult to treat.
Depending on the concomitant disease, there are:
- Primary BE is determined by direct damage to the heart valves.
- Secondary EB develops on previously damaged heart valves or as a result of the development of rheumatic heart disease.
Pathophysiology
In normal condition and in the absence of damage, the endothelium of the valves is very resistant to colonization and infection by bacteria circulating in the blood.
Various microtraumas caused by turbulent flow, intracardiac disorders, etc., or chronic diseases (rheumatic heart disease, congenital heart defects, use of prosthetic valves, previously experienced EB) can damage the endothelium.
Damage to the endothelial membrane causes the formation of a thrombus of fibrin and platelets on it. Microbes can colonize this thrombus during transient episodes of bacteremia, fungal infection, and viremia.
The most common risk factors:
- Heart disease/damage (highest risk).
- Drug use.
- Low immune defense.
- Poor oral hygiene.
- Nosocomial infection.
Causes
Most often, the development of bacterial endocarditis is facilitated by microorganisms that settle with the bloodstream on the valve leaflets and infect them. The following bacteria are mainly of clinical importance:
- S. aureus (Staphylococcus aureus). The most common microorganism that causes EB. Patients usually get sick more severely and faster. The mortality rate associated with this bacterium has been reported to be as high as 47% (Moreillon 2010, Fraimow 2013). May affect normal and abnormal valves.
- S. viridans (streptococcus). It only damages the valves. The mitral and aortic valves are most often affected in cases of BE, accounting for 90% to 95% of cases.
- S. epidermidis (staphylococcus epidermidis). Associated with defects, usually within 1 month of onset of illness.
- S. bovis (streptococcus) – more common among older people.
- S. pnuemoniae (pneumococcal infection). An acute, lightning-fast disease. Often affects the structure of the aortic valve. High risk of developing perivascular abscess and pericarditis.
- P. aeruginosa (Pseudomonas aeruginosa).
- HACEK – Hemophilus spp., Actinobacillus spp., Cardiobacterium hominis, Eikenella corrodens and Kingella kingii. Slow-growing gram-negative bacilli that may take several weeks to be detected in culture. Accounts for 1-3% of all cases of EB, with an average delay in diagnosis of 1-3 months.
: Endocarditis (infective, libman-sacks) – causes, symptoms, treatment & pathology
Symptoms
Bacterial endocarditis most often develops atypically (without fever or other systemic disorders): This mainly affects the elderly with weakened immune systems and people with endocarditis of the right side of the heart.
May develop as bacteremia or sepsis for an unknown reason. Also, BE is often associated with a fulminant form of sepsis and cardiogenic shock. Such conditions are considered critical and require immediate medical attention.
During an objective examination, the first thing that attracts attention is heart murmurs. For example, in 50% of cases, new noises, sounds of blood regurgitation, are detected. At an early stage of the disease, murmurs are usually absent.
In some patients, atrioventricular abnormal conduction of cardiac impulses is determined. These may be accompanied by a prolonged PR interval and heart block.
Heart failure (HF) is a complication of EB, but often symptoms such as edema and shortness of breath are the first to be identified during the development of the disease. In particular, HF can occur due to valvular stenosis, valvular regurgitation, rupture of an infected valve, and abnormal conduction system function.
- Valve insufficiency
It is considered the most common complication of BE. Develops due to destruction of the valve as a result of rupture or penetration. Also, the cause of the pathological condition may be loss of support from the chordal components or the valve ring.
This is often the direct cause of the development of EB. Such embolic complications can occur at any time throughout the course of BE.
The overall prevalence of embolic manifestations ranges from 20% to 50%. After starting antibiotic treatment, such risks are reduced, but pathology can still occur.
Factors that increase the risk of thromboembolic events:
- Determination of pathological microorganisms by type S. aureus, Candida and Abiotrophia.
- The presence of vegetation more than 10 mm.
- Mitral valve dysfunction.
In the presence of renal embolism, an abscess, ischemia and infarction may form, flank pain, pyuria or hematuria may appear. This condition is often confused with simple pyelonephritis, urinary tract infection or ureterolithiasis.
Pulmonary valve infection occurs in
Source: https://arrhythmia.center/bakterialnyiy-endokardit-prichinyi-simptomyi-i-lechenie/