- home
- Articles about cholelithiasis
- This is useful to know
- About the structure of the human body
- Catalog of useful medical articles
›
›
›
›
In this article I will tell you about the blood supply to the heart.
About the blood supply to the organ that supplies blood to the entire body, all its organs, all tissues and all its cells. Sections of the article
Blood supply to the heart
Coronary circulation
About the features of coronary circulation
Structure of the vascular bed of the heart
You have questions?
What is coronary heart disease
Disease of the coronary or coronary artery of the heart and its branches is caused by decreased blood flow, often due to atheroma. Clinically, this can manifest as silent ischemia, angina, ACS (unstable angina, myocardial infarction) and sudden cardiac death. Diagnosis is made based on symptoms, ECG recordings, stress testing, and sometimes coronary angiography. Prevention consists of influencing risk factors, for example:
- hypercholesterolemia;
- lack of physical activity;
- smoking.
It is treated with pharmacotherapy and interventions that reduce ischemia and improve blood flow through the coronary arteries.
Features of the structure of the coronary vessels
Very thin and fragile vessels responsible for the flow of arterial blood to the myocardium, or heart muscle, are the coronary arteries.
This concept is very general; blood vessels are part of the circulatory system of the human body. The vessels mainly provide the flow of oxygen and nutrients to the heart muscle. Both the right and left arteries are involved in supplying the body with oxygen and nutrients. The anatomy of the vessels is such that they have a small number of large branches, mainly two or three branches and several small ones. Arterial branches provide blood flow to various parts of the heart. The vessels originate from the bulb of the artery, behind the valve leaflets.
Considering the blood supply system of the human body, it makes sense to analyze the concept of dominance. When determining dominance, it is necessary to identify the vessel from which the posterior descending branch arises. In 70 percent of cases, there is a right dominant blood supply. In 10 percent of cases we are talking about the left dominant type of blood supply.
If both the right artery and the circumflex coronary artery are fully involved in the process of supplying the body with blood, then we are talking about a symmetrical type of blood supply, which occurs in 20 percent of cases.
The outflow of venous blood is carried out, for the most part, by the great vein, the middle vein and the small vein. These vessels intertwine with each other and form the coronary sinus, which in turn opens into the right atrium. The outflow of blood through these veins is 2/3, the remaining blood flows out through the anterior cardiac and thebesian veins.
The walls of the coronary vessels are dense and elastic, they have three layers. The first layer is called the endothelium, the second layer is formed from muscle fibers, and the third layer is the adventitia. The elasticity of the veins is necessary for normal blood flow, because a large load is placed on the vessels. During physical activity on the body, the speed of blood flow increases five times.
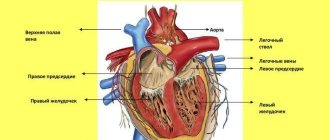
The heart is a muscular organ that circulates blood in the body like a pump. The heart is provided with autonomous innervation, which determines the involuntary, rhythmic work of the muscular layer of the organ - the myocardium. In addition to nerve structures, the heart also has its own blood supply system.
Most of us know that the human cardiovascular system consists of two main circles of blood circulation: large and small. However, specialists in cardiology consider the vascular system that nourishes the tissues of the heart as the third or coronary circulation.
If we consider a three-dimensional model of the heart with the vessels supplying it, we can see that a network of arteries and veins surrounds the heart like a crown. This is where the name of this circulatory system comes from - coronary or coronary circle.
Circles of blood circulation
The coronary circle of hemocirculation consists of vessels, the structure of which is not fundamentally different from other vessels of the body. The vessels through which oxygenated blood moves to the myocardium are called coronary arteries.
Vessels providing outflow of deoxygenated, i.e. venous blood are coronary veins. About 10% of all blood passing through the aorta enters the coronary vessels.
The anatomy of the vessels of the coronary circle of hemocirculation is different for each person and is individual.
Schematically, the coronary circulation can be expressed as follows: aorta - coronary arteries - arterioles - capillaries - venules - coronary veins - right atrium.
Let's consider the hemocirculation scheme along the coronary circle in stages.
Arteries
The coronary arteries arise from the so-called sinuses of Valsalva. This is an enlarged portion of the aortic root located just above the valve.
The sinuses are named according to the arteries emerging from them, i.e. the right sinus gives rise to the right artery, the left sinus gives rise to the left artery.
The right one runs along the coronary groove on the right, then stretches back to the apex of the heart.
Through the branches extending from this highway, blood rushes into the thickness of the myocardium of the right ventricle, washes the tissues of the posterior part of the left ventricle and a significant portion of the cardiac septum.
Human arteries
The left coronary artery, leaving the aorta, is divided into 2 and sometimes 3 or 4 vessels. One of them is ascending and runs along the groove dividing the ventricles in front.
Multiple small vessels extending from this branch provide blood flow to the anterior walls of both ventricles. The other vessel is descending and runs along the coronary sulcus on the left.
This line carries enriched blood to the tissues of the atrium and ventricle on the left.
Next, the artery goes around the heart on the left and rushes to its apex, where it forms an anastomosis - the fusion of the right cardiac artery and the descending branch of the left. Along the descending anterior artery, smaller vessels branch off, providing blood to the anterior region of the myocardium of the left and right ventricles.
The third coronary artery occurs in 4% of the population. An even rarer case is when a person has only one heart artery.
Feedback from our reader – Alina Mezentseva
I recently read an article that talks about the natural cream “Bee Spas Kashtan” for treating varicose veins and cleaning blood vessels from blood clots. With this cream you can cure VARICOSIS FOREVER, eliminate pain, improve blood circulation, increase the tone of veins, quickly restore the walls of blood vessels, clean and restore varicose veins at home.
I’m not used to trusting any information, but I decided to check and ordered one package. I noticed changes within a week: the pain went away, my legs stopped “humming” and swelling, and after 2 weeks the venous lumps began to decrease. Try it too, and if anyone is interested, below is the link to the article.
A powerful motor that drives blood through vessels, arteries and veins, thereby supplying the human body with oxygen and nutrients - that’s what the heart is.
It is the coronary arteries that supply the heart muscle with oxygen and ensure the outflow of venous blood. If the patency of blood vessels is impaired, this can lead to various diseases of the cardiovascular system.
Review from our reader Victoria Mirnova
I recently read an article that talks about the drug Choledol for cleaning blood vessels and getting rid of CHOLESTEROL. This drug improves the general condition of the body, normalizes the tone of the veins, prevents the deposition of cholesterol plaques, cleanses the blood and lymph, and also protects against hypertension, strokes and heart attacks.
I’m not used to trusting any information, but I decided to check and ordered a package. I noticed changes within a week: the constant pain in my heart, heaviness, and pressure surges that had tormented me before receded, and after 2 weeks they disappeared completely. Try it too, and if anyone is interested, below is the link to the article.
Very thin and fragile vessels responsible for the flow of arterial blood to the myocardium, or heart muscle, are the coronary arteries. This concept is very general; blood vessels are part of the circulatory system of the human body.
Arteries of the heart
If both the right artery and the circumflex coronary artery are fully involved in the process of supplying the body with blood, then we are talking about a symmetrical type of blood supply, which occurs in 20 percent of cases.
Anatomy of the coronary arteries and types of blood circulation
There are two coronary arteries, their origin is located just above the mouth at the beginning of the aorta, the large arterial vessel of the human body that comes from the left ventricle of the heart. There are right and coronary arteries, they work according to the scheme. They originate from the aortic sinus. The right coronary artery begins in the right sinus and is responsible for supplying blood to the right ventricle and the inferior posterior wall of the left. The other, the left coronary artery, begins in the left and is divided into several small arteries (2-4).
Of these, the most important are the circumflex and anterior descending arteries with a special structure. The circumflex artery is always located on the posterior surface of the heart. In its proximal part, a branch of the obtuse edge (BMA) departs from the artery, also known as the artery of the obtuse edge and many smaller vessels.
On a note! There are large and medium-sized coronary arteries that run along the surface of the heart (epicardial) and send smaller arterioles into the myocardium.
The left coronary artery begins as a trunk and soon divides into:
- left anterior descending artery (LAD);
- peripheral (ACx).
The LAD usually follows the anterior interventricular artery and, in some individuals, continues beyond the apex. This artery supplies the anterior septum (including the proximal part of the conduction system) and the free anterior wall of the left ventricle. The circumferential artery, which is usually smaller than the LAD, supplies the free lateral wall of the left ventricle. Most people have a “right type” of blood circulation, the right coronary artery (RCA) crosses the atrioventricular groove and the right side of the heart. It supplies the sinus node (in 55% of people) of the right ventricle, usually the AV node and the inferior wall of the myocardium.
In approximately 10-15% of people, the “left variant” is active: the circumferential artery is larger and continues along the posterior AV groove, supplying the posterior wall and the AV node. There is also a balanced type of blood supply, which consists of uniform blood supply to the heart.
Types of blood supply to the heart
Blood flow to the anterior and lateral surfaces of the myocardium is quite stable and is not subject to individual changes. Depending on where the coronary arteries and their branches are located in relation to the posterior part or surface of the myocardial diaphragm, three types of blood supply to the heart are distinguished:
- Average. Consists of well-developed LAD, OB and RCA. The blood supply vessels entirely to the LV and from two-thirds to half of the IVS are branches of the LMCA. The pancreas and the rest of the IVS receive nutrition from the RCA. This is the most common type.
- Left. In this case, blood flow in the LV, the entire IVS and part of the posterior wall of the RV is carried out by the LCA network.
- Right. Isolated when the RV and posterior wall of the LV are supplied by the RCA.
These structural changes are dynamic and can only be accurately determined using coronary angiography. There is an important feature characteristic of cardiac circulation, which is the presence of collaterals. This is the name given to alternative routes formed between the main vessels that can be activated at the moment when, for some reason, the working one is blocked in order to take over the functions of the one that has become unusable. The collateral network is most developed in elderly people suffering from coronary pathologies.
That is why in critical situations associated with blockage of the main myocardial vessels, young people are at greatest risk.
Causes of coronary circulatory disorders
Atherosclerosis is a slowly progressive disease of the heart vessels that can begin in childhood. Although the exact cause is unknown, atherosclerosis can begin with damage to the inner layer of the artery. This is the main type of coronary circulatory disorders.
The occurrence of deviation is influenced by:
- high blood pressure;
- high cholesterol – eating too much saturated fat;
- high triglycerides;
- smoking (1 or more packs of cigarettes per day for several years increases mortality from coronary artery disease by 200%);
- diabetes;
- inflammation such as arthritis, lupus and others;
- hereditary predisposition.
Once the inner wall of an artery is damaged by cholesterol and other cellular products, fatty deposits accumulate over time, causing it to harden and narrow.
Attention! The organs and tissues associated with the blocked artery do not receive enough oxygen from the transferred blood to function normally.
A blood clot (plaque) forms, partially or completely blocking the blood supply to the arteries, thus preventing the flow of blood to a certain part of the body. This can cause a heart attack if the path to the heart is completely blocked. The clot can travel to other parts of the body and block the flow of blood in other organs (brain, kidney, intestines).
Possible pathologies
Coronary blood flow is justifiably of great importance for the entire body as a whole. After all, arteries of this kind are responsible for the blood supply to the main human organ – the heart.
Therefore, damage to these vessels and the development of abnormal processes in them leads to myocardial infarction or ischemic disease.
Blood flow may be impaired due to blockage of blood vessels by plaque or blood clots.
Insufficient blood flow to the left ventricle can result in disability and even death. Stenosis may also develop due to vasoconstriction.
Stenosis of the coronary vessels of the heart leads to the fact that the myocardium cannot fully contract the heart. The doctor usually uses a bypass to restore blood flow.
It is advisable to undergo periodic diagnostics in order to prevent the appearance of stenosis, as well as to promptly treat atherosclerosis. Coronary types of arteries provide blood supply to the main organ in the human body.
If the coronary vessels do not cope with the task and lose elasticity, then the heart experiences a deficiency of vital elements.
This can provoke various diseases of the “motor” of the human body and even lead to an attack.
Diagnostics of heart vessels
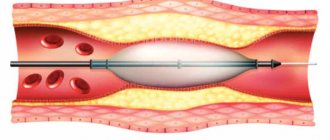
Coronary angiography is the most commonly performed invasive diagnostic method in cardiology, with which you can get a detailed picture of the condition of the coronary vessels, you can perform stenosis (narrowing) of blood vessels and evaluate their degree. Coronary angiography is performed by inserting a catheter into a person's arterial system, which is slowly guided towards the heart.
There are:
- coronary angiography of the heart through the arm (through the radial artery in the wrist);
- coronary angiography of the heart through the leg (through the femoral artery in the groin area).
To ensure painlessness, a local anesthetic is first applied to the catheter site. Special techniques are used to place the gland and catheter, which are slowly directed towards the heart.
The procedure is performed when the heart is beating normally and the patient is conscious and lying on the table. When the cardiologist reaches the coronary arteries, he injects contrast into the blood vessels, and the X-ray detector creates a real-time view of the coronary arteries on the screen. Radiation doses from coronary angiography are equivalent to those from a chest CT scan (which is similar to 150 conventional chest X-rays).
The procedure takes about 20 minutes if there are no complications. The most important feature of this method (besides the definitive diagnosis of CAD) is that intervention for treatment can be performed during coronary angiography.
The procedure could be:
- Concerted coronary angiography – for people suffering from angina pectoris and wishing to determine the exact condition of the coronary vessels and draw up a treatment plan.
- emergency coronary angiography - in people having a heart attack, when it is necessary to urgently transport the patient to a center that can perform intervention - swelling of the blood vessels and placement of a stent.
The compression bandage should be kept in place for 24 hours. The procedure takes about 20 minutes if there are no complications.
Angina pectoris
Angina is a disease characterized by chest pain that occurs when the muscle wall of the heart temporarily runs out of oxygen. With thoracic angina, the coronary arteries narrow, as a result of which they cannot fully supply the heart with oxygen during physical or emotional stress. Problems disappear with rest or after taking medications - nitroglycerin (causes dilation of blood vessels).
In stable angina, myocardial necrosis (loss of heart muscle tissue) does not occur because ischemia (decreased oxygen supply) does not last long.
Patients may experience pain that they describe as:
- chest pain;
- burning in the chest;
- chest pressure;
The pain often spreads to the left, less often to the right arm, neck, lower jaw or abdomen. Patients are pale, sweating, and shortness of breath may occur.
The first appearance of pain during an illness will frighten every person, but after examination by a doctor and the disease has been established, patients react more calmly to the pain and take a nitroglycerin tablet. Then the pain stops and you can return to normal activities.
Myocardial infarction
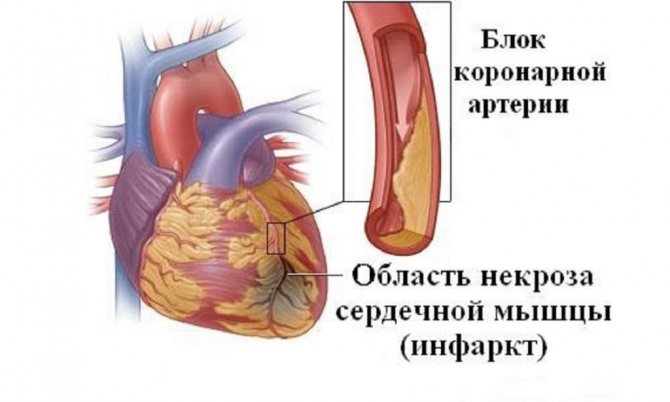
An infarction (heart attack) occurs when a blood clot blocks a coronary artery and completely blocks the blood supply to the myocardium. Due to clogged blood vessels around the heart, cardiac muscle cells do not receive oxygen and die, that is, myocardial necrosis develops.
On a note! Myocardial infarction is a disease of old age, and more than half of all patients are over 65 years of age. By the age of 60, men get sick 4-5 times more often than women, but later this difference becomes less noticeable.
Heart attack is more common in people who have risk factors:
- family predisposition to heart disease and atherosclerosis;
- diabetes;
- obesity;
- smoking cigarettes;
- sedentary lifestyle without physical activity;
- too much nervous tension;
- hypertension, high blood pressure.
In more than 95% of cases, myocardial infarction is caused by atherosclerosis of the coronary artery.
The main symptom of a heart attack for most people is pain in the middle of the chest. It is described as chest tightness or a burning sensation. May spread to the arm, neck, lower jaw, back or abdomen.
In addition to chest pain, the following symptoms occur:
- nausea;
- vomit;
- general weakness;
- feeling of anxiety;
- cold sweat;
- rapid heartbeat - tachycardia;
- heartbeat;
- shortness of breath, lack of air;
- dizziness.
Unlike angina, the pain is not relieved by rest when nitroglycerin is administered.
Heart rhythm disturbance
Against the background of coronary diseases, the occurrence of atrial fibrillation is characteristic. The development of AF in patients with ACS - acute coronary syndrome is correlated with problems such as atrial ischemia or infarction, atrial stretch due to volume overload:
- atherosclerosis;
- increased levels of catecholamines;
- improper metabolism;
- degradation of heart valves.
Heart failure
Congestive heart failure is a problem with the functioning of the heart when the organ loses its ability to pump blood effectively, leaving the body's oxygen needs unmet.
Heart failure is not a specific disease, but a clinical syndrome. The difference is that any heart or vascular disease can eventually lead to heart failure as a symptom.
The most common causes of heart failure are:
- long-term arterial hypertension (high blood pressure);
- coronary heart disease - heart attack;
- heart valve disease;
- congenital heart defects;
- cardiomyopathy;
- toxic heart damage from alcohol and certain drugs.
A person who has suffered from one of these diseases for many years will eventually develop heart failure.
Symptoms of heart failure:
- Dyspnea. Caused by an increase in pressure in the pulmonary circulation due to congestion caused by heart failure. This occurs initially during heavy physical work and in an expanded state it also occurs at rest.
- Orthopnea. Shortness of breath that occurs when lying on your back. Worsens when lying on your back due to the accumulation of blood in the chest, further aggravating congestion (stagnation of blood). People with heart failure and shortness of breath should sleep in an elevated position to help them breathe easier.
- Paroxysmal nocturnal dyspnea (cardiac asthma). This is heart failure during sleep - severe attacks of shortness of breath at night and awakening from sleep. The patient wakes up with choking, coughing and wheezing, which is usually accompanied by a feeling of fear. A person cannot help himself by adopting an elevated position during sleep (as with orthopnea).
- Palpitations, especially palpitations when lying on your back.
- Arrhythmia, palpitations.
- Fatigue and weakness are a consequence of a lack of oxygen and nutrients in all parts of the body.
- Nocturia is increased frequency of urination at night.
- Oliguria - decreased urination occurs at a later stage of cardiac decompensation due to a decrease in cardiac output.
- Cerebral symptoms: irritation, forgetfulness, insomnia, headache, disorientation - a consequence of cerebral hypoperfusion.
- Cardiac cachexia – in chronic heart failure, loss of appetite is expressed.
- Pale skin, feeling of coldness in the extremities.
- Cyanosis of the extremities (acrocyanosis) is a bluish color of the skin and mucous membranes caused by an excess of oxygenated hemoglobin in the blood.
- Excessive sweating, varicose veins of the legs.
- Varicose veins due to accumulation of venous blood (stagnation);
- Enlarged liver, hepatomegaly.
- Swelling of the legs, swollen ankles.
Coronary insufficiency
Ischemic disease can occur in several clinical forms. The most noticeable is the appearance of chest pain. Short-term pain in the heart that stops after the provocative causes that cause it, such as:
- exercise stress;
- excitation;
- exposure to cold;
- after taking medications.
These are signs of a short-term decrease in blood flow or ischemia of part of the heart muscle. Severe, persistent chest pain always raises suspicion of a heart attack. Chest pain is not a permanent sign of coronary heart disease. Ischemia may be silent, present but painless, and may be diagnosed only temporarily during its duration or as a permanent scar change (as a result of a heart attack) based on characteristic changes in the ECG.
Attention! Coronary disease in developed countries is one of the most important causes of mortality, which can be significantly reduced through timely diagnosis and treatment.
That is why it is necessary to promptly recognize signs that cast doubt on the existence of the disease.
Disorders of the coronary arteries
Coronary arteries with abnormal structure are not uncommon. People do not have complete identity in the structure of blood circulation either with the standards of anatomy or with each other. Differences arise for many reasons. They can be divided into two groups:
The former may be the result of abnormal variability, while the latter include the consequences of injuries, operations, inflammation and other diseases. The range of consequences from violations can be enormous: from asymptomatic to life-threatening. Anatomical changes in the coronary vessels include their position, direction, number, size and length. If congenital abnormalities are significant, they make themselves felt at an early age and are subject to treatment by a pediatric cardiologist.
But more often such changes are discovered by chance or against the background of another disease. Blockage or rupture of one of the coronary vessels leads to consequences of poor circulation proportional to the size of the damaged vessel. The normal functioning of the main myocardial vessels and problems in their functioning are always reflected in typical clinical symptoms and ECG recordings.
Problems with blood supply to the myocardium make themselves felt when physical or emotional stress is exceeded. This is especially important to remember because some coronary anomalies can cause sudden cardiac arrest in the absence of underlying medical conditions.
Reducing the risk of complications
Some risk factors for heart disease cannot be controlled, such as a family history of the disease. But it's still important to reduce your chances of developing heart disease by reducing risk factors that you can control. To do this you need:
- Maintain healthy blood pressure and cholesterol levels.
- Find ways to cope with stress.
- Maintain a healthy weight.
- Lead a healthy lifestyle (eat healthy foods and exercise regularly).
- Avoid foods rich in saturated fat and salt. Doctors recommend just 2 hours and 30 minutes of exercise every week.
Smoking should be avoided. Nicotine in cigarettes causes constriction (shortening) of blood vessels, which impairs blood circulation with oxygen. This can lead to atherosclerosis.
How to fight
The very first question patients ask is whether atherosclerosis can be cured. Definitely not. There is no medicine that would reverse the process, reduce or disappear the plaque. Treatment is to stabilize the situation. Slow down the growth of atherosclerosis, and in the most successful case, stop it altogether. Ideally, you need to think about this before symptoms appear. However, later this literally becomes a vital necessity.
In addition to nutrition, metabolism is of great importance. A person with increased body weight is at much greater risk of developing coronary heart disease. In addition, diabetes mellitus, especially poorly treated diabetes with high blood sugar levels, increases the tendency to atherosclerosis.
Drug treatment
Prescription and dose selection of medications of this kind should only be carried out by a doctor. Like any other medications, they have a number of side effects, for example, they affect liver function. For this reason, they are prescribed strictly according to indications, focusing on tests and the severity of the disease. Timely intake of statins in appropriate dosages is one of the most powerful means of preventing atherosclerosis.
It would seem that the size of the affected vessels in coronary heart disease is quite small for surgery. But fortunately, modern medicine can even do this. In case of severe angina or acute heart attack, a special intervention is performed - coronary angiography. A microscopic probe is inserted into the heart vessel and contrast is injected. Under high magnification, doctors can see where blood flow is obstructed and correct the problem. Using a special balloon, the narrowing site is expanded and a stent is installed - a mesh-shaped structure that increases the lumen. This operation is performed under local anesthesia. Moreover, opening the chest is not required, only a small puncture on the arm or thigh.
Stenting could have been considered a salvation, if not for one thing. The vessels on which the intervention occurred are again affected by atherosclerosis if statins and a number of other medications are not taken. After the operation, the patient is simply obliged to take medications for life, according to a certain scheme.
To summarize, we can say that atherosclerosis is really enemy number one. But having looked at it from all sides, we can successfully repel attacks. The main thing is to act on time and wisely.
Coronary arteries are vessels that provide the heart muscle with the necessary nutrition. Pathologies of these vessels are very common. They are considered one of the main causes of death in older people.