Mitral valve reconstruction - how the operation is performed
Two newer procedures are mitral valve reconstruction using polytetrafluoroethylene sutures and mitral valve ring buckle assembly.
1. Reconstruction (Mitralklappenrekonstruktion durch Implantation von PTFE-Fäden). A special rim of polytetrafluoroethylene threads is sutured to the cuff (ring) of the mitral valve. As a result, the closing function of the mitral valve is enhanced and reverse blood flow is cut off during systolic contraction of the heart muscle. Heart activity and blood circulation are normalized. All tissues and organs receive enough oxygen from the blood. “Left heart syndrome” and symptoms of mitral regurgitation are eliminated. All actions for implantation of polytetrafluoroethylene threads are performed with a catheter, under continuous visual control (echocardiography). The operation can be performed under full anesthesia, but recently partial analgesic anesthesia is increasingly used - this is sufficient. Polytetrafluoroethylene is better known as Teflon - a polymer with rare physical and chemical properties that determine its biological purity and good survival rate.
2. Assembly on the mitral ring buckle (perkutane Mitralklappenanuloraphie mit Spange). Assembly is carried out not in the “assembly and construction” sense, but in the “sewing” sense. The weakened cuff (ring) of the mitral valve is pulled into the assembly, like fabric on a thread, onto a special implanted buckle (Spange). German seamstresses call this assembly Raffung, and in vascular medicine of the 21st century the term Anuloraphie has taken root, meaning assembly of the mitral valve ring. As a result, the diseased valve becomes “strong” and does not allow blood to flow in the opposite direction. The most promising anatomical “buckles” make it possible to strengthen both the valve and the coronary sinus within a single implantation. The nature of the operation is the same as described above.
Your questions will be answered by:
Introductory part
Before heart surgery, a person has many questions. Some of them we ask the doctor, and some we cannot even formulate. When we understand what is happening to our body and what we can do to restore health, it is easier for us to endure all procedures.
Acquired heart valve defects
- these are diseases that are based on morphological and/or functional disorders of the valve apparatus (valve leaflets, annulus fibrosus, chordae, papillary muscles), developed as a result of acute or chronic diseases and injuries, disrupting the function of the valves and causing changes in intracardiac hemodynamics.
Valve defects can be congenital or acquired.
Congenital defects occur when the structures of the heart are formed incorrectly during intrauterine development; sometimes they do not make themselves felt until adulthood. Acquired defects arise due to rheumatism, infection, metabolic disorders (when calcium is deposited in the valves), trauma and other reasons.
The main types of heart valve defects:
- mitral stenosis
- mitral valve insufficiency
- mitral valve prolapse
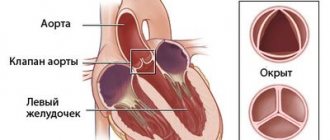
- aortic stenosis
- aortic valve insufficiency
- tricuspid stenosis
- tricupidal insufficiency
The normal functioning of the heart largely depends on the functioning of its valve apparatus.
Obstacles to the passage of blood cause overload, hypertrophy and expansion of the structures above the valve. Obstructed heart function disrupts the nutrition of the hypertrophied myocardium and leads to heart failure.
Etiology and pathogenesis
Etiology of stenosis
and combined rheumatic disease,
insufficiency
- usually rheumatic, rarely septic, atherosclerotic, traumatic, syphilitic.
Stenosis is formed as a result of cicatricial fusion or cicatricial rigidity of the valve leaflets and subvalvular structures; valve insufficiency - due to their destruction, damage or scar deformation.
Failure
valve damage occurs due to destruction or damage to its valve flaps. Valve insufficiency is characterized by incomplete closure of the leaflets and occurs as a result of their wrinkling, shortening, perforation or expansion of the fibrous valve ring, deformation or separation of the chordae and papillary muscles. In some cases, valve insufficiency develops as a result of dysfunction of the valve apparatus, in particular the papillary muscles.
Often stenosis and insufficiency develop on one valve (the so-called combined defect
).
In addition, there are cases when the defects affect two or more valves - this is called combined
heart disease.
Affected valves form an obstacle to the passage of blood - anatomical in case of stenosis, dynamic in case of insufficiency. The latter is that although some of the blood passes through the hole, it returns back in the next phase of the cardiac cycle.
A “parasitic” volume is added to the effective volume, performing a pendulum-like movement on both sides of the affected valve. Significant valvular insufficiency is complicated by relative stenosis (due to increased blood volume). Obstruction to the passage of blood leads to overload, hypertrophy and expansion of the overlying chambers of the heart.
The expansion is more significant with valve insufficiency, when the overlying chamber is stretched by additional blood. With stenosis of the atrioventricular orifice, the filling of the underlying chamber is reduced (left ventricle with mitral stenosis, right ventricle with tricuspid stenosis); There is no hypertrophy or expansion of the ventricle.
With valve insufficiency, the filling of the corresponding ventricle is increased, the ventricle is dilated and hypertrophied. Difficulty in the functioning of the heart due to improper functioning of the valve and degeneration of the hypertrophied myocardium leads to the development of heart failure.
Changes in hemodynamics
Hemodynamic changes are the main link in the pathogenesis of the disease. They largely depend on the amount of blood that returns from the aorta back to the left ventricle. That is, the left ventricle is filled from two sources, from the left atrium and from the aorta. This leads to an increase in the volume of its chamber.
The amount of blood that the ventricle must expel increases. By doing extra work, the left ventricle increases its mass - myocardial hypertrophy occurs.
Ultimately, dilatation of the left ventricle leads to an increase in the fibrous ring of the left atrioventricular valve and its relative insufficiency occurs. This is the so-called mitralization of the defect.
When the process decompensates, stagnation begins in the pulmonary circulation. The pressure in the pulmonary artery system increases. This leads to right ventricular hypertrophy and serious consequences from shortness of breath to pulmonary edema.
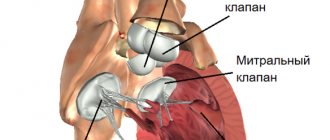
Anatomy of the heart
A healthy heart is a strong, continuously working organ, about the size of a fist and weighing about half a kilogram.
In addition to maintaining steady, normal blood flow, it quickly adapts and adapts to the body's ever-changing needs.
For example, the heart pumps more blood when it is active and less when it is at rest. During the day, the heart produces an average of 60 to 90 beats per minute - 42 million beats per year!
The heart is a two-way pump that circulates blood throughout the body. It consists of 4 chambers.
A muscular wall called the septum divides the heart into left and right halves. Each half has 2 chambers.
The upper chambers are called atria, the lower chambers are called ventricles. The right atrium receives all the blood returning from the upper and lower parts of the body.
Then, through the tricuspid valve, it sends it to the right ventricle, which in turn pumps blood through the pulmonary valve to the lungs.
In the lungs, the blood is enriched with oxygen and returns to the left atrium, which sends it through the mitral valve to the left ventricle.
The left ventricle pumps blood through the arteries through the aortic valve throughout the body, where it supplies the tissues with oxygen. Oxygen-depleted blood returns through the veins to the right atrium.
Four valves (tricuspid, pulmonary valve, mitral, aortic) act as a door between the chambers, opening in one direction.
These valves help blood move forward and prevent it from flowing in the opposite direction.
The petals of a healthy valve are thin, flexible tissue of perfect shape. They open and close when the heart contracts or relaxes.
Heart valves can become abnormal due to birth defects. They can become damaged or scarred due to rheumatic fever, infection, hereditary factors, age or heart attacks.
The mitral valves are most susceptible to such changes.
Regardless of the case, the heart valve can become stenotic (narrowed opening) or insufficient (does not close completely).
With valve stenosis, the heart must work harder to pump the required amount of blood through the narrowed opening.
Valve insufficiency causes blood to flow backwards through the valve after it closes. Once again, the heart has to work harder to pump enough blood for the body's needs to make up for the deficiency caused by the backflow of blood.
Both cases - stenosis and failure - force the heart to work harder to pump the required amount of blood. This extra work can weaken the heart, cause it to enlarge, and cause various diseases.
Reasons for development
The etiology of aortic insufficiency is quite diverse.
There are acquired and hereditary causes. Birth defects are represented by:
- Violations of the valve structure, in which the valve ceases to be double-leaf, and the number of valves changes up or down. Typically in the range of one to four.
- Marfan syndrome, which causes degeneration of all connective tissue, including the aortic valve. In addition to the heart, the pathology affects the eyes and joints, which is typical for the Marfan triad.
- Inhibition of protein synthesis, resulting in a lack of collagen and elastin, which makes the valve walls thin and easily distensible.
The list of acquired etiological factors includes:
- Infections that cause inflammation in the valve leaflets (syphilis, streptococcal and staphylococcal infections). They form peculiar warts on the walls of the aortic valve.
- It is possible for aortic atherosclerosis to spread to the valve walls and further progression of the plaque.
- Severe injuries leading to rupture of the valves. In this case, a transition immediately to the acute stage is possible.
- Increased blood pressure and compensatory left ventricular hypertrophy cause the valve to become too small to perform its functions. This is called relative deficiency. Because the valve dimensions are normal, but in conditions of ventricular enlargement they are insufficient.
- Systemic connective tissue diseases. As a result of autoimmune processes, the valve tissue is perceived as foreign and is destroyed by its own leukocytes. (systemic lupus erythematosus, rheumatoid arthritis).
It is important for the attending physician to determine the origin of the defect in order to prescribe the correct treatment.
Rheumatic etiology is most often confirmed by anamnesis, rheumatic damage to other organs, and specific changes in the blood.
The infectious nature is proven by blood cultures and immunological studies.
Deficiency of syphilitic origin is detected using serological tests or other manifestations of syphilis. There are also radiological signs of aortic dilatation.
Damage to the aortic valve may be the only manifestation of Marfan syndrome, so establishing this etiology is quite difficult.
Diagnosis of heart valve diseases
After listening to the symptoms you describe and examining your medical record, the doctor will measure your pulse and blood pressure and listen to your heart using a stethoscope.
If your doctor suspects that you have a heart disease, he may ask you to undergo a series of special diagnostic tests that will help make an accurate diagnosis and prescribe the necessary treatment.
One of these research methods is a non-invasive method. i.e., in which no internal intervention is required.
Another type of research is invasive. with the help of instruments inserted into the body, which, as a rule, causes only minor inconvenience to the patient.
Chest X-ray
This test allows the doctor to obtain valuable information about the size of the heart, heart chambers and the condition of the lungs.
Electrocardiogram (ECG)
An electrocardiogram monitors the electrical current passing through the heart and stimulates the chambers to contract. An ECG is especially useful in diagnosing abnormal heart rhythms and rates.
These studies also show muscle enlargement or damage, and the presence of congestion on one side or another of the heart.
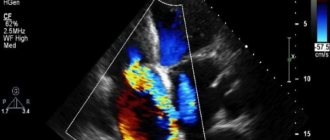
Echocardiogram (EchoCG)
This test is carried out using a “small” microphone placed on the surface of the chest, which emits high-frequency sound waves.
Sound waves are reflected back (hence the term "echo") from each layer of the heart wall and valves and then displayed on a monitor screen. The “echo” image from different points allows you to see a cross-section of the heart at the moment of its operation.
During the echo, the speed of blood flow is also recorded, the direction of blood movement is monitored: is the blood moving in the normal forward direction or is there a reverse movement (as in the case of valve insufficiency).
A narrowed (or stenotic) valve causes increased blood flow. The degree of valve stenosis is in many cases accurately determined by the increased blood flow velocity.
This test will not only show how the heart valves work, it will also provide useful and comprehensive information about the size of the heart chambers, as well as the thickness and function of the heart muscle.
Cardiac catheterization and angiogram
These tests are done by inserting a thin, hollow tube (catheter) through a vein or artery in the arm or groin area and into the chambers of the heart, using X-rays.
During catheterization, the pressure in the chambers of the heart is measured and the volume of blood in the bloodstream is determined.
Angiography consists of the injection of a radiopaque contrast agent, which is visible using X-rays and allows you to evaluate the work of the heart in pumping blood, the function of the valve and the patency of the arteries (coronary) that supply blood to the heart muscle.
Despite the fact that similar studies have been routinely carried out before, it is not at all necessary that they are needed in your case if the information obtained by echocardiography is complete and accurate.
In many cases, the only invasive test required before surgery is a coronary angiogram if it is determined that the patency of one or more arteries is impaired.
If there are blockages in the coronary arteries, the doctor will usually perform bypass surgery at the same time as heart valve surgery.
Aortic stenosis in newborns
Aortic stenosis in newborns
Causes of congenital aortic stenosis
- hereditary tendency;
- bad habits of the mother, poor ecology;
- some genetic diseases of the child: Williams syndrome.
- a membrane above the valve with a narrow hole in the center or side;
- valve development abnormalities (single or bicuspid valve);
- tricuspid valve with fused petals and asymmetrical leaflets;
- narrowed aortic ring;
- a cushion of connective and muscle tissue located under the aortic valve in the left ventricle.
Symptoms and external signs of aortic stenosis in newborns
Well-being
- pale skin, sometimes blue discoloration on the wrists and areas around the mouth;
- frequent regurgitation;
- weight loss;
- rapid breathing more than 20 times per minute;
- the child sucks weakly at the breast and has shortness of breath.
Objective symptoms
- pale skin;
- tachycardia over 170 beats per minute;
- the pulse on the wrists is almost not palpable due to poor filling of the arteries;
- Using a stethoscope, the doctor listens to the heart murmur;
- if a newborn has developed sepsis, then the noise is practically absent due to weak heart contractions;
- peculiarity of the disease - noise is heard in the vessels of the neck;
- The doctor feels a trembling of the chest under the palm of his hand. This is the result of turbulent flows and eddies in the blood flow in the aorta;
- The smaller the opening of the aortic valve, the lower the blood pressure. It may be different on the right and left hand;
- A characteristic sign of the disease is that symptoms intensify over time.
Data from instrumental examination of aortic stenosis in newborns
Electrocardiography
- left ventricular overload;
- failure in the transmission of biocurrents to the heart;
- disturbances in the rhythm of ventricular contraction.
Chest X-ray
- signs of congestion in the lungs with severe stenosis - pulmonary blood vessels are dilated;
- the heart is slightly enlarged in the area of the ventricles, and narrowed in the middle - the waist of the heart is pronounced.
Echocardiography
- a mass (membrane or cushion) above or below the aortic valve;
- narrowed opening of the aortic valve;
- disturbances in the operation of the valve: it consists of 1 or 2 leaflets, they bend into the cavity of the left ventricle when closing;
- thickening of the muscular wall of the left ventricle due to the proliferation of muscle or connective tissue;
- decreasing the size of the internal space during contraction and relaxation.
Dopplerography
- allows you to assess the severity of stenosis - the size of the aortic inlet;
- helps to calculate the pressure gradient - features of the pressure difference in the left ventricle and in the aorta.
Cardiac catheterization and angiocardiography
Diagnostics
Listening to the heart - auscultation
- a rough noise in the heart and in the arteries in the neck that occurs when blood passes through a narrowed hole;
- fast and irregular heartbeats.
Electrocardiography
- signs of left ventricular overload;
- tachycardia (fast heartbeat) in a newborn, more than 170 beats per minute;
- heart rhythm disturbances – arrhythmia;
- Occasionally, signs of thickening of the heart in the left ventricle are noticeable.
Chest X-ray
- enlarged left side of the heart;
- sometimes there are signs of blood stagnation in the lungs, which appear as darkening on the image.
Echocardiography Echocardiography or ultrasound examination of the heart
- deformed aortic valve cusps;
- reduced opening of the aortic mouth;
- the appearance of turbulent blood flow in the aorta. Swirls and waves occur when blood passes under pressure through a narrowed area;
- reduction of the cavity of the left ventricle due to the proliferation of its walls;
- changes in the level of blood pressure in the left ventricle and aorta during heart contraction.
Cardiac catheterization
- narrowing of the aorta;
- an increase in pressure in the left ventricle and a decrease in it in the aorta.
Types of operations for aortic stenosis in newborns
Contraindications to the operation are:
- Sepsis is blood poisoning.
- Severe left ventricular failure (underdevelopment or proliferation of connective tissue in its walls).
- Concomitant severe diseases of the lungs, liver and kidneys.
Heart valve surgery
Often heart defects do not manifest themselves for a long time, because the heart adapts to working under overload. In the case where the heart defect is “moderate” and does not lead to serious overload of the heart, in some cases they are limited to observation or drug therapy. But when the defect is severe, it must be treated surgically.
The following operations are performed on heart valves: reconstruction or complete replacement of a damaged valve.
Heart valve reconstruction
Sometimes during surgery it is possible to preserve the valve flaps and only correct their shape. This procedure is called valve repair.
.
Sometimes the shape of the valve can be restored by strengthening its base with threads, or by sewing a special ring to the base, while the valve’s own flaps are preserved. This procedure is called annuloplasty.
. it is possible only for the mitral and tricuspid valves.
Valve reconstruction can largely restore its function. For severe heart valve damage, valve replacement surgery may be the only treatment option. The results of these operations exceed the effect of drug therapy. Today, heart valve surgery can be performed on patients of any age group.
Access for operations on the aortic valve or on several valves simultaneously is made through an incision in the center of the sternum. When performing operations on the mitral valve, it is possible to use the “keyhole technique,” when surgical access is made through a small incision in the projection of the mitral valve: on the side and below the chest.
When it is impossible to save the leaflets of the native valve, or if they are preserved, there is a high probability of the defect returning and repeated surgery, the native valve is excised and implanted in its place
artificial
valve prosthesis
.
The most commonly performed surgeries are mitral valve reconstruction. In this case, the own valve is preserved - this is very important.
, Ross surgery is performed to treat aortic disease.
. The damaged aortic valve is replaced with the patient's own pulmonary valve, which is similar in structure, and an artificial prosthesis is implanted instead of the excised pulmonary valve.
When the aortic valve and aortic wall are damaged, it may be necessary to replace the ascending aorta with a valve-containing aortic graft
(sometimes called a conduit). In this case, not only the aortic valve is replaced, but also the adjacent ascending aorta.
Your attending physician will inform you about the possibility of reconstructive surgery on the heart valve in your case. In some cases, the question of the possibility of valve reconstruction is decided during the operation: if reconstruction is not possible, then an operation is performed to replace the damaged valve.
Heart valve replacement
To replace human heart valves, two types of valve prostheses are used: the first type is artificial prostheses: made from artificial composite material (see Fig. 1), the second type is biological prostheses: made from chemically treated lobes of the heart of pigs and cows, applied to a supporting frame. (see Fig. 2) and without a frame (see Fig. 3).
The advantage of a mechanical heart valve prosthesis is its significant strength, but the disadvantage is the need for lifelong therapy with drugs that inhibit blood clotting (anticoagulants, for example, warfarin, Marcumar, etc.).
The advantage of a biological prosthesis is the absence of any additional drug therapy after surgery, the disadvantage is the limited survival time of the prosthesis: currently it is approximately 12-15 years, and then a repeat operation.
The choice of type depends on age, concomitant diseases, lifestyle and other factors. You must make this choice together with your doctor.
Heart valve surgery
(plasty or replacement of the mitral valve)
One of the important areas of activity of the department is heart valve surgery. If the functioning of the heart valves is disrupted - they are narrowed (so-called stenosis) or insufficiency, there is the possibility of their replacement or plastic surgery (reconstruction).
When replacing valves, modern mechanical and biological models are used. Mechanical valves are very reliable, last a lifetime and do not need to be replaced, but they require constant use of special medications to reduce blood clotting. Biological valves (porcine or made from equine pericardium) can deteriorate over time, and the lifespan of these valves is highly dependent on the age of the patient and his concomitant diseases. With age, the process of destruction of biological valves slows down greatly. The decision about which valve is the best option in a particular situation is made individually before surgery in a mandatory conversation between the surgeon and the patient. Our clinic pays special attention to operations that allow you to preserve your own valve. For these purposes, our center has developed improved techniques for plastic surgery (reconstruction) of the mitral and aortic valves.
One of the new techniques is the use of special threads to fix the torn mitral valve leaflets, the so-called neo-chordae (Fig. 6a). The use of neochords makes it possible in many cases to avoid mitral valve replacement and preserve your own valve for a long time. Similar operations are performed through a small incision under the armpit (Fig. 6)
Such operations avoid the constant anticoagulation required when implanting mechanical valves or the risk of destruction over time of biological valves.
Currently, in our Center, in most cases, patients with diseases of the mitral, tricuspid or aortic valves undergo sparing surgery without incision of the sternum. The operation through a minimally invasive approach between the ribs is performed using a heart-lung machine, which is connected through a small incision in the groin.
Frameless valves are a variant of biological valves and are used to replace the aortic valve. You can also use the patient’s own pulmonary artery to replace the aortic valve using the Ross technique. This type of surgery is the standard treatment method in our clinic.
Valve implantation in a minimally invasive way
Transcatheter reconstruction of the mitral valve using Mitraclip
Elderly patients or patients with serious concomitant diseases (severe chronic obstructive heart disease, dialysis, severe cerebral atherosclerosis, and others) have an increased risk of complications when undergoing conventional or minimally invasive mitral valve reconstruction using a heart-lung machine. In such cases, we use transcatheter implantation of a mitral clip (Mitralclip) without the use of a heart-lung machine. In a patient under light anesthesia, the catheter is inserted under local anesthesia through the femoral vein into the right atrium, and then through the interatrial septum into the left atrium. After this, the mitral valve leaflets are connected to each other with a clothespin - a clip (Fig. 9 and 10).
The advantage of this operation is a quick recovery: the patient can be discharged home the next day. This technique is a good alternative to open heart surgery in patients with an increased risk of postoperative complications.
Our website presents highly qualified specialists in diagnostics, medicinal and surgical treatment, as well as rehabilitation therapy in the field of cardiology and cardiac surgery in Germany. All specialists mentioned on our website are professionals in this medical field and have been selected in accordance with strict criteria.
Currently, mitral regurgitation remains one of the most common pathologies of the cardiovascular system, negatively affecting the functioning of the heart, which is why in Germany the issues of mitral valve reconstruction are given an important role.
Aortic stenosis and comorbidity in the elderly and senile age
When evaluating older patients for aortic stenosis, clinicians often focus only on the valve as the main cause of the patient's complaints. However, the presence of concomitant, often severe, diseases should be taken into account
Concomitant diseases can affect the outcome of surgical treatment, which makes a comprehensive examination of the patient necessary.
In older patients with severe pulmonary diseases, such as pulmonary hypertension or chronic obstructive pulmonary disease, it may be difficult to recognize whether symptoms are signs of cardiovascular or pulmonary disease. Aortic valve replacement may not improve clinical symptoms or outcome.
In patients who underwent TKA, significant impairment of pulmonary function was observed in 60% of cases, and more than 30% of patients required oxygen therapy. Increased morbidity and mortality have been observed in patients with serious pulmonary disease who undergo aortic valve replacement.
Another small cohort study found that 77% of cases had significant sleep-disordered breathing. Chronic kidney disease, liver disease, and anemia were independently associated with increased mortality after aortic valve replacement.
Mitral valve insufficiency
The cardiac mitral valve is a valve located in the left heart, consisting of connective tissues whose role is to suppress reverse blood flow from the left atrium. With a completely healthy heart, the valve is able to regulate the amount of blood entering by opening and closing. However, if there are any disturbances in the smooth operation of the valve, the human “motor” begins to stretch and hypertrophy, which affects its operation.
The diagnosis of “mitral valve insufficiency” is made when the mitral septum is unable to close completely, leaving an opening through which blood from the left atrium begins to flow back. As a result of this defect, the heart muscle works in an increased mode, which leads to its overload.
Most often, in people whose medical history includes such a diagnosis, mitral valve insufficiency is mild, which, as a rule, does not require its reconstruction and does not cause complications. However, with more severe forms of pathology, the imprint of increased cardiac activity falls on almost all systems and organs. Often, such patients experience an enlargement of the left atrium, which ultimately, in the absence of effective therapy, results in heart failure and arrhythmia.
Mitral valve insufficiency is a very serious disease, which is why such patients must be observed by a cardiologist, who, after a thorough examination, will decide on the need for surgical intervention and select the most optimal method of performing the operation.
Typically in Germany, in such cases, doctors resort to radical replacement or reconstruction of the damaged mitral valve. But in situations where the patient has concomitant illnesses in severe forms, such as heart pathologies or renal failure, the operation is associated with a huge risk to the patient’s life.
Today, the German medical cardiology industry has found an excellent innovative solution to this problem. The catheter-friendly, minimally invasive technique for installing special MitraClip clamps is a real breakthrough.
— Privat-docent, dr. med. Science Luciano Pizzuli -
MitraClip, as opposed to established methods of surgical treatment of mitral insufficiency, is characterized by the absence of risks to the patient’s life and is considered safer and more effective. The operation itself is performed under general anesthesia, does not require a thoracotomy, and all manipulations are performed through installed catheters.
Nitroglycerin relieves pain
This treatment is prescribed if surgery can be avoided. It is aimed at eliminating symptoms and treating diseases that caused the development of stenosis. Drug therapy is also used in the preoperative and postoperative period.
Prevention can last for several years, but can also be prescribed for life. But it is only necessary if surgery has eliminated valve damage caused by acute rheumatic fever.
After implantation of an artificial valve, lifelong use of blood thinning medications. This prophylaxis prevents the formation of blood clots. For more than a year now, warfavin has been the standard as the best anticoagulant.
Medical recommendations for this disease are not much different from the prescriptions that are intended for patients with other cardiovascular diseases. Among these recommendations:
- Elimination of physical activity;
- Limiting fluid and salt intake;
- Quitting alcohol and smoking;
- Exclusion from the diet of fatty and fried foods.
It is necessary to regularly take medications prescribed by a doctor and undergo the necessary diagnostic measures.
Doctor's instructions regarding actions during pregnancy may vary and depend on the degree of the disease. Severe aortic stenosis may be a reason for termination of pregnancy. This is explained by the fact that during the period of gestation, all organs begin to work in an enhanced mode and the cardiovascular system is no exception. In safer forms, pregnancy proceeds normally, but preventive measures are taken to prevent the development of valve pathology.
The essence of the mitral valve reconstruction method in Germany Mitra-Clip
The Mitraclip is based on state-of-the-art technology developed by Abbot's international cardiac division. This method is aimed at successfully eliminating pathological changes in the mitral valve, and is suitable for both young and older patients.
The mitral valve reconstruction itself in Germany using the Mitra-Clip method is a surgical procedure with minimal blood loss, penetration and damage to healthy tissue. During the operation, a catheter is inserted through the groin area at the site of the femoral artery, at the end of which a clip is installed - a kind of clamp. The catheter is advanced towards the heart and upon reaching the valve apparatus, the clamp is installed between the mitral leaflets, thus creating a connection. Installation of the clip creates free flow of blood on the sides of it, preventing its reverse outflow, thus compensating for mitral insufficiency.
The entire process of intervention and implantation of the clip is carried out by the cardiac surgeon under the strict control of radiographic equipment through runesophageal echocardiography, thanks to which all the specialist’s actions are as accurate as possible, and if necessary, there is the possibility of adjustment. The procedure is completely atraumatic. After ensuring that the mitral clamp is installed correctly and securely, the catheter is removed from the body, leaving only small punctures in the skin.
To date, mitral valve reconstruction in Germany using the MitraClip method has been successfully performed on several thousand patients from all over the world.
Types of artificial valves, their features
They can be divided into two groups:
- Mechanical.
- Biological.
The latter are produced from animal tissues: pig endocardium or calf pericardium.
For aortic valve defects, the Ross operation is popular, when a pulmonary valve is installed in place of the aortic valve (it is replaced with a biological prosthesis).
Advantages and disadvantages of biological prostheses:
| pros | Minuses |
| No risk of blood clots | Low durability (8–15 years) |
| No need to take anticoagulants | If worn out, need to be replaced again |
| Better tolerated by older people | High risk of recurrent infective endocarditis |
Advantages and disadvantages of mechanical prostheses:
| pros | Minuses |
| High wear resistance: service life - more than 20 years | High risk of blood clots, so constant use of anticoagulants is necessary |
The feasibility of using various valves:
| Who gets biological valves? | Who gets mechanical ones? |
| Patients with an increased risk of blood clots | For infective endocarditis |
| To old people | At a young age (since the biological prosthesis lasts up to 15 years, and then will need to be replaced again) |
Recovery period after mitral valve reconstruction in Germany
The postoperative period is surprisingly easy. Almost immediately after the surgical procedures for installing the Mitraclip, the patient comes to his senses and within a day can move freely. The recovery period takes only 2-3 days, depending on the nominal condition of the patient. An improvement in the general condition is noted immediately after the end of the surgical intervention.
The surgical procedure itself takes place in 1 hour, in a standard situation. However, the operation time may vary within a certain range depending on the physiological characteristics of the patient.
Typically, the hospital stay after catheter clipping is about 3 days, however, based on individual indications and needs, the attending physician can extend the time spent in the hospital until the condition improves.
Symptoms of the pathological condition
The symptomatic picture of aortic insufficiency appears depending on the form of the pathology. There are chronic and acute forms of the course. Determination of the form depends on the root cause of the pathology. For example, with traumatic influences, the pathology takes on an acute form and rapid development, and with lupus erythematosus suffered in childhood, aortic insufficiency appears as a complication and is chronic.
In the chronic form of the course, the following symptoms are observed:
- frequent and severe headaches, which are accompanied by tinnitus and a feeling of pulsation in the head;
- increasing muscle weakness;
- dizziness;
- increased sweating;
- angina pectoris;
- arrhythmia;
- sinus tachycardia;
- fainting;
- short-term loss of consciousness (often occurs during a sharp rise);
- heart pain that does not have an etiological origin in physical activity or stress;
- arterial pulsation.
When moving to the stage of decompensation, the patient experiences increased shortness of breath. This condition occurs due to disturbances in blood circulation in the lungs. Under these conditions, the first symptoms of asthma appear.
The acute form has distinctive features:
- pulmonary edema;
- arterial hypotension.
Both chronic and acute forms can be treated with medications. In case of severe symptoms and increased severity of the disease, surgical treatment of the disease is performed. In case of inoperability, treatment is considered on an individual basis.
Drug therapy after mitralbic reconstruction
After standard surgery on the mitral valve, the patient may be prescribed drug therapy for a period of up to 3 months. Antithrombotic drugs are usually prescribed to thin the blood.
However, for patients who have undergone mitral valve reconstruction in Germany using MitraClip technology, the prescription of medications is much reduced, due to the significant improvement in the general condition after the intervention. All recommendations after mitral clipping are limited to monitoring your condition, reducing physical activity and protecting yourself from psycho-emotional stress for one month.
Despite the fact that the MitraClip technique is relatively new, in just a few years of its active use this technique has gained an excellent reputation and has established itself as an effective, safe and non-traumatic type of heart surgery. All patients who have undergone such mitral valve reconstruction in Germany note a significant improvement in their condition, with virtually no rehabilitation period.
Cardiac surgery. Clinics and doctors
Life after surgery
In the first year after valve replacement, you should go to the doctor for examination every month. In the second year - once every six months. Then – once a year.
During the examination, an ECG and EchoCG must be done.
Throughout your life you must follow these rules:
- Give up bad habits and drinking coffee.
- Take anticoagulants prescribed by your doctor.
- Follow a diet: give up fatty, fried, salty foods, eat more fruits, vegetables and dairy products.
- Work no more than 8 hours a day.
- Sleep at least 8 hours a day.
- Do not lead a sedentary lifestyle, walk more, spend at least 1-2 hours a day in the fresh air.
Physical exercise
Competitive sports and hard work are contraindicated.
You can and should perform therapeutic exercises, agreed upon with your doctor.
Precautions for future surgeries
Any surgical intervention, even dental, can provoke endocarditis. Therefore, be sure to tell your surgeon that you have undergone heart valve replacement surgery.
To prevent inflammation in the heart, you need to take an antibiotic 30–60 minutes before the surgical procedure. This may be Amoxicillin, Azithromycin, Ampicillin or Cephalexin to choose from. Please discuss this with your doctor in advance.