An article about bilirubin; the norm for men by age is presented, a summary table for convenience. Bilirubin is a yellow-green bile pigment that functions as an antioxidant in the human body and is part of bile. A blood test to determine the norm of total (direct + indirect) bilirubin in men is the first stage in diagnosing pathologies of the liver and bile ducts.
The study is of particular importance for elderly patients over 60 years of age and those who abuse alcohol, since their liver’s detoxifying ability is reduced. Deviation of the criterion from the norm always indicates pathology.
Types of bilirubin: direct, total and indirect
The indirect fraction is toxic to the human body and can penetrate the blood-brain barrier. It is formed during the breakdown of hemoglobin. Due to the high degree of lipophilicity (affinity for organic fats), it easily penetrates the cytoplasmic membrane of the cell and then into the mitochondria. The result is a disruption of metabolic and energy processes in the cell.
Transport of the indirect fraction to the liver is carried out by binding to simple proteins albumin. Its detoxification (neutralization) occurs in the liver by adding a sugar-containing component - glucuronic acid. The resulting stable complex of the direct fraction, together with bile, is transported to the small intestine.
Further metabolism leads to the restoration of the direct fraction to urobilinogen. One part goes into the enterohepatic circulation of bile acids and returns back to the liver, and the other goes into the enterohepatic urobilinogen cycle with conversion to the yellow pigment urobilin.
Bilirubin is excreted in the form of stercobilin in feces (a small part in the form of stercobilinogen is excreted in the urine).
The total fraction is the total amount of direct and indirect bilirubin. During laboratory analysis, the direct and total fractions are determined, and the indirect fraction is determined by the calculation criterion, calculated as the difference between the total and direct fractions.
What are the indications for bilirubin testing in men?
The normal level of total bilirubin in the blood of men must be determined during a routine preventive annual examination, as well as if the patient exhibits signs of increased bilirubin levels (hyperbilirubinemia). Among them:
- accumulation of bile pigment in the connective tissue, eyeball, mucous membranes or skin, leading to their yellowing (sometimes a greenish tint to the skin may be observed);
- discoloration of stool;
- change in urine color (dark beer color);
- pain in the liver and pancreas;
- constant bloating;
- itching of the skin;
- constant nausea;
- taste of bile (bitterness) in the mouth;
- constant heartburn;
- constipation;
- bad breath.
In addition, the study is relevant for blood diseases (hemolytic anemia), stones in the bile ducts, hereditary bilirubinemia, hepatitis, treatment with hepatotoxic drugs, gastrointestinal diseases, infectious pathologies, alcohol poisoning or other toxic substances.
Diet for high bilirubin (treatment at home)
The following foods reduce the level of bile pigment in the body and help improve liver function:
- Tomato juice: One glass of tomato juice mixed with a pinch of salt and pepper should be taken on an empty stomach in the morning.
- Juice from radish leaves: Take radish leaves and squeeze the juice out of them using a grater, meat grinder or blender. Drink about half a liter of this concentrated juice daily, after about ten days you can go for a retest and observe a decrease in the substance in the body.
- Papaya leaf tea and honey: Add one tablespoon of honey to a cup of papaya leaf tea (available at the pharmacy). Drink this tea regularly for one to two weeks. Helps effectively, especially if the elevated level is caused by jaundice.
- Basil Leaves : Take about 10-15 basil leaves and make a paste. Add half a glass of fresh radish juice to the pasta. Drink this daily for two to three weeks.
- Lemon: The anti-inflammatory property in lemon helps in treating jaundice. Squeeze the juice from 2 whole lemons and add to a glass of water. Prepare and drink this infusion three times a day, as it protects liver cells from damage.
- Turmeric: Add a pinch of turmeric to a glass of warm water. Mix well and drink 3-4 times a day.
- Beetroot and Lemon: Take one cup of beetroot juice and mix equal amounts of lemon juice. The drink should be drunk regularly for several 2-3 days.
- Chamomile: Douching with chamomile in folk medicine is very effective; a glass of brewed chamomile tea should be drunk at least once a day for several weeks.
Products you should avoid
- Anything spicy and fried.
- Carbohydrate-rich foods.
- Stop drinking alcohol, caffeine and large quantities of red (black) tea.
- Avoid unpasteurized milk.
Other Dietary Recommendations
- Increase your intake of foods rich in calcium and minerals (iron and magnesium).
- Vegetables and fruits should be taken raw or steamed.
- Drink more vegetable juices (carrot, tomato).
If your bilirubin level is elevated, you should immediately talk to your doctor and ask for additional tests to rule out any serious illnesses.
Until additional diagnostics are carried out, you cannot rely on treatment at home; you must first rule out a number of serious diseases.
How can a man prepare for a bilirubin test?
It is extremely important to follow the rules of preparation for collecting biomaterial (venous or capillary blood), since the criterion is highly sensitive to many external factors. Blood is donated on an empty stomach, at least 12-14 hours after the last meal.
The following causes false results: smoking (excluded 2-3 hours before the test), fasting, excessive physical or emotional stress, administration of an intravenous contrast agent and exposure to UV radiation.
You must stop taking the following medications for 3 days:
- antibacterial;
- antiviral;
- antihistamines;
- antimalarial;
- vitamin A and C;
- anticonvulsants.
Norm of bilirubin in blood in men and summary table
The information presented is not sufficient to make a diagnosis and cannot serve as a guide for self-diagnosis. The interpretation of the results obtained is carried out by the attending physician, taking into account the clinical picture and data from additional diagnostic methods.
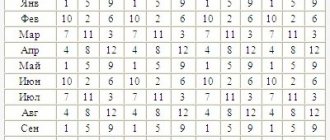
It is necessary to select reference (acceptable) values taking into account age. The table shows the norm of total and direct bilirubin in men by age.
| Age | Reference values, µmol/l | |
| Total bilirubin fraction | Direct fraction of bilirubin | |
| 0 – 1 day for full-term babies | 25 – 150 | Ratio of direct to indirect fractions = 90 to 10% |
| 12 o'Clock in the noon | 55 – 256 | |
| up to 1 week | 28 – 210 | |
| 1 week – 1 month | 60 – 100 | |
| Over 30 days and up to 50 years of life | 8,5 – 20,5 | up to 5 |
| In men after 50 years | 3,7 – 18 | |
The normal level of direct bilirubin does not differ between men and women.
Reduced levels in men
If the result of laboratory tests shows a discrepancy to a lesser extent, this may be a sign of coronary heart disease or a violation in preparation for the analysis, and more specifically, the man may have drank strong coffee or tea before taking the test.
So, if a man suspects liver or gallbladder disease, he should immediately consult a doctor. After conducting laboratory tests of a blood test and identifying abnormalities, the doctor will take action. Most diseases require hospital treatment, since deviations are almost always evidence of dangerous diseases that require constant medical supervision.
Problems indicated by deviations in bilirubin levels can lead to very serious consequences, so both men and women should not delay visiting a doctor and, of course, should not self-medicate.
How to return the bilirubin level to normal?
First, it is necessary to establish the root cause of the deviation of bile pigment from normal values. Further treatment tactics depend on this, which must be determined by the attending physician.
If viral hepatitis is detected, antiviral and immunostimulating drugs are prescribed. Treatment of liver cirrhosis consists of the use of hepatoprotectors, and in case of chronicity of the process, organ transplantation is indicated.
For systemic infectious pathologies, the prescription of antimicrobial agents, hepatoprotectors, vitamin preparations, sorbents, etc. is indicated.
In case of bile stagnation, ursodeoxycholic acid, antispasmodics and choleretic agents are prescribed.
For Gilbert's syndrome, Barboval is prescribed (due to the phenobarbital content it reduces the level of bilirubin), ursodeoxycholic acid, vitamins (B, A, E), antispasmodics and choleretic agents, as well as probiotics and sorbents.
Medicines to reduce bilirubin, for example:
- Milk thistle tablets ® (RUB 110) – exhibit pronounced antitoxic properties due to direct interaction with free radicals, as a result of which their toxicity is significantly reduced. Activates the enzyme RNA polymerase necessary for the biosynthesis of phospholipids and proteins;
- Liv 52 ® (360 rubles) is a combination medicine that exhibits hepatoprotective and choleretic effects, and also improves digestion. Helps stabilize liver cell membranes and enhance antioxidant processes. The drug can be used to prevent cholelithiasis and treat cirrhosis, hepatitis and hepatosis;
- Karsil ® (400 rubles) - the mechanism of action of the hepatoprotector is the competitive displacement of toxins onto the sensitive receptors of the liver cell membrane. Due to this, the neutralizing function of the liver is activated and the cell membrane is stabilized;
- Essentiale Forte N ® (RUB 1,260) is a hepatoprotector whose action is based on strengthening the cell wall of hepatocytes and activating their detoxification function.
Yulia Martynovich (Peshkova)
Certified specialist, in 2014 she graduated with honors from the Orenburg State University with a degree in microbiologist. Graduate of the graduate school of the Federal State Budgetary Educational Institution of Higher Education Orenburg State Agrarian University.
In 2020 At the Institute of Cellular and Intracellular Symbiosis of the Ural Branch of the Russian Academy of Sciences, she completed advanced training in the additional professional program “Bacteriology”.
Laureate of the All-Russian competition for the best scientific work in the “Biological Sciences” category 2020.
Bilirubin in the blood of men, women and children is a bile component (pigment) of a greenish-yellow hue. It is formed as a result of protein breakdown. Decomposition products with bile are removed through the intestines. When accumulated, the pigment becomes a source of yellowing of the skin and mucous membranes.
How is bilirubin formed?
Hemoglobin, which delivers oxygen to all organs and systems, is located in erythrocytes or red blood cells. Having aged, they are destroyed with its release.
Through chemical reactions, it is transformed into indirect bilirubin, which is toxic (poisonous). By binding to other substances in the liver, it is converted into direct (bound), less dangerous. This pigment is removed through the intestines with bile secreted by the liver. This is the substance that colors stool.
The conversion of hemoglobin to bilirubin can be observed visually during the formation of bruises . A change in color from bluish to purple occurs when blood escapes from damaged vessels into the tissue.
The appearance of a greenish tint is observed when pigments of the corresponding color leave hemoglobin. Finally, as bilirubin forms, the bruise turns yellowish.
Bile pigment is found in small quantities in blood plasma. Exceeding the norm signals problems with the liver and impaired bile flow. In men, Gilbert's syndrome, in which bilirubin increases, is diagnosed many times more often (about 10 times) than in women.
Types of bilirubin
Total bilirubin consists of two fractions:
- direct (related, conjugated);
- indirect (unbound, free).
Their main difference is their ability to dissolve in water.
Indirect bilirubin
It is formed in the spleen, which is responsible for the disposal of aged red blood cells. Here the blood cells are destroyed and a toxic enzyme appears. It does not dissolve in water, so the kidneys are not able to eliminate it from the body.
Indirect bilirubin combines with the blood component albumin, is sent through the vessels to the liver, where it is transformed into direct bilirubin.
It is able to dissolve in the fats of healthy cells, causing them harm through toxicity. Therefore, it is important to monitor the normal level of its content in the blood. Indirect pigment is dangerous, having the ability to disrupt cellular respiration and protein formation.
Straight
It is low toxic and practically harmless. Formed in the liver. Easily dissolves in aqueous media.
Direct bilirubin is excreted from the body through urine and feces.
Forms
One of the important indicators of the human body is bilirubin. With his help
it is possible to determine the condition or processes occurring in the liver. Sometimes the disease can be diagnosed only by the high level of bilirubin in the blood.
There are three forms of bilirubin in blood serum. These are direct, indirect and total bilirubin. The last two forms together form total blood bilirubin.
Indirect
The indirect form is formed in the human body during the breakdown of red blood cells, and more specifically from hemoglobin, which is part of their composition before it is processed by the liver. Indirect insoluble in water. But it perfectly penetrates healthy cell membranes, disrupting their functioning, and easily dissolves in fats. It is very toxic to the human body. The indirect form represents the difference between general and direct. The normal level of indirect bilirubin in male blood is 19 µmol per liter.
Straight
Direct bilirubin is the indirect form processed by the liver. Direct enters the human small intestine and is converted into urobilinogen there. But first it combines with glucoronic acid in the liver, and because of this it is also called bound bilirubin. Direct bilirubin is excreted from the body using bile. Not as toxic as indirect and soluble in water. The normal blood level for direct bilirubin is 0-7.9 µmol per liter.
Symptoms of increase:
- pain in the right hypochondrium;
- decreased appetite;
- darkening of urine;
- belching;
- skin itching;
- liver colic.
General
Total bilirubin in the human body should normally be 3.4-17.1 µmol per liter.
The level of bilirubin in the blood is determined by conducting laboratory tests for which it is necessary to take a blood test from a man from a vein.
Compliance of bilirubin concentration with standards
The level of bile pigment is compared with the corresponding norms. In 100% of the total amount, approximately one fifth is bound pigment, the rest belongs to free pigment.
Table 1 - normal indicator of bile pigment in men.
Bilirubin is a bile pigment consisting of obsolete red blood cells. It enters the blood in a strictly defined amount. The level of bilirubin in the blood of men depends largely on age and diet. Serious changes in concentration often indicate the presence of a disease that requires treatment. Typically, the causes of increased bilirubin concentrations are liver and gallbladder diseases. Therefore, doctors advise periodically donating blood for analysis and, in case of deviations from the norm, conducting a detailed examination.
Normal for men
After collecting material for research, a laboratory technician can receive results within two hours . Normal enzyme levels in the male body are as follows:
- the total pigment indicator should not exceed the norm of 5.0-17.1 mmol/l;
- the indirect pigment indicator cannot go beyond the indicator of 3.3-12.1 mmol/l;
- the number of direct bilirubin should be within the range of 1.6-5.0 mmol/l.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
Additionally, the doctor will check the ratio of direct to indirect bilirubin. The total amount of soluble fraction should not fall below 70%, and the ideal range is 70-75 %.
In rare cases, taking certain medications may cause your bilirubin level to increase or decrease. But such a deviation will be insignificant and will disappear in a week or two. But a deviation from normal limits by even one percent means it is necessary to check the functioning of the liver. That is why, if there is a violation in the amount of bilirubin, the analysis can be carried out again to control the fractions over time.
How is bilirubin formed and what is its role in the body?
Bilirubin is a product of the breakdown of hemoglobin in the liver, bone marrow and spleen. A popular theory is that bile pigment is the main cellular antioxidant that binds free radicals.
The following types are distinguished:
- Indirect, or free. Produced by the tissues of the spleen during the destruction of old red blood cells. Insoluble, binds to albumin, penetrates the liver, where it is converted directly.
- Straight. It has low toxicity and is highly soluble in water.
Indirect bilirubin is highly toxic. Exceeding its norm negatively affects the condition of the liver and brain.
What is bilirubin?
Bilirubin is a unique bile pigment with a rather bright red-brown color. It is an important product of hemoglobin catabolism. It is known that the main part of bilirubin itself is always formed in the liver. Its excessive accumulation in the blood or significant appearance in the urine in humans is of great diagnostic importance. These conditions are called hyperbilirubinemia and bilirubinuria.
The small molecule of bilirubin contains four pyrrole simple rings that are connected linearly to each other. The determined molecular weight of bilirubin is 548.68. Ordinary pure bilirubin can be characterized as a crystalline substance. It is always sparingly soluble in water, glycerin, ether, and also slightly soluble in alcohol, while it is slightly better in chlorobenzene, chloroform and various diluted alkali solutions.
Since bilirubin is a special breakdown product of red blood cells, it is continuously produced in the body. In tissues and blood, only an indirect type of bilirubin is initially formed, in other words, a toxic substance. It is practically insoluble in water, and therefore is not excreted from the human body at all. It is believed that normally this indirect bilirubin always goes directly to the liver along with the blood, where its direct form is formed.
This resulting substance is subsequently soluble in water, due to which it is easily excreted from the human body along with feces or urine. It is worth mentioning that it is the substance bilirubin that gives human feces such a characteristic brown color.
| Type of bilirubin | Children 1-3 days of life | Children 3-6 days of life | Children after a month | Adults |
| General | From 24 to 190 µmol/l | From 28 to 210 µmol/l | From 3.5 to 20.4 µmol/l | From 8 to 20.5 µmol/l |
| Straight | 0,5-10,2 | 1-12,4 | 0-5,1 | 0-5,1 |
| Indirect | 23,5-179,8 | 27-197,6 | Up to 16.5 | Up to 16.5 |
Find out more: Norm of bilirubin in blood
How to prepare for the test: diagnostic features
Bilirubin in men is determined by a biochemical blood test. For planned biochemical studies it is necessary to prepare:
- A few days before blood sampling, avoid alcohol, fried foods, and spicy foods.
- In the morning before the test, do not eat, drink juices, carbonated drinks, coffee or tea.
- Do not smoke before blood collection.
On the day of the analysis, it is forbidden to have breakfast. Donate blood on an empty stomach.
Sometimes, if the condition worsens, urgent analysis is necessary. During an emergency examination, small errors in readings are acceptable and no special preparation is required.
Diagnostics
Doctors diagnose elevated bilirubin in combination with other laboratory tests (alkaline phosphatase, aspartate aminotransferase (AST), alanine aminotransferase (ALT)) associated with liver problems.
Laboratory diagnosis of bilirubin is carried out when:
- Jaundice (Gospel's disease);
- When the patient suffers from alcoholism or often abuses alcohol;
- If you suspect that you are taking narcotic or toxic drugs;
- When a person has been exposed to viruses that cause hepatitis.
A blood chemistry test may also be done if hemolytic anemia is suspected as the cause of anemia (a condition characterized by low levels of hemoglobin or red blood cells in the blood).
In this case, additional tests are often prescribed to evaluate hemolysis (complete blood count, reticulocyte test, haptoglobin and lactate dehydrogenase (LDH)).
Types and norms of bilirubin in men by age: table
The concentration of pigment in the blood of both sexes differs slightly. But men tend to have a slightly higher level compared to women. This is due to the high content of red blood cells in the blood of men. The minimum amount is observed in young people under the age of 21. The concentration gradually increases and reaches a peak by the age of 30. Then there is a gradual decline, and by the age of 60 the lowest rate is noted.
Bile pigment is found in small quantities in blood plasma. Exceeding the norm signals problems with the liver and impaired bile flow. In men, Gilbert's syndrome, in which bilirubin increases, is diagnosed many times more often (about 10 times) than in women.
The norm of bilirubin in men is determined according to the table:
Signs of changes in bilirubin in the blood
The disease is indicated not only by the result of a blood test, but also by external signs. With an increase in the amount of bilirubin in plasma, the following is noted:
- Yellow skin tone. A similar symptom is sometimes provoked by an increased concentration of vitamin A, pathologies of the pancreas or thyroid gland. With hyperbilirubinemia, the sclera of the eyes necessarily turn yellow - this sign allows you to more accurately determine the disease.
- Bitter taste in the mouth.
- Periodic nausea and vomiting.
- Feeling of heaviness in the area of the right hypochondrium.
- The stool is discolored.
- The pigment accumulates in the urine, so its color resembles dark beer.
Reasons for deviation from the norm
Changes in this indicator indicate problems in the body. Increased or decreased concentrations indicate specific pathologies.
Promotion
This means that the liver simply does not have time to process the indirect pigment. Hemolysis (breakdown of red blood cells) occurs rapidly. If liver cell decomposition (necrosis) occurs, hepatocytes are unable to perform direct functions, and toxic bilirubin accumulates.
Excess of indicators is observed in the following diseases and conditions:
- Gilbert's syndrome. A hereditary disease that most often affects representatives of the stronger sex. According to statistics, out of every 100 patients, 90 are men.
- Dubin-Johnson syndrome and Rotor syndrome. Genetically caused jaundice.
- Liver diseases, for example, cirrhosis, hepatitis.
- Vitamin B12 deficiency. A lack of vitamins disrupts hematopoietic processes - red blood cells quickly disintegrate, and the concentration of bilirubin increases.
- Cholelithiasis. As a result of the blockage, the bile ducts swell and bile does not exit the bladder. Indirect bilirubin easily penetrates into the blood, causing jaundice.
- Worm infestation.
- Congenital anemia, in which red blood cells are rapidly destroyed.
- Acquired anemia caused by lupus erythematosus, rheumatoid arthritis, lymphorganulomatosis. Also accompanied by rapid destruction of blood cells.
- Syphilis stages 2–3.
- Sepsis.
- Internal bleeding.
- Typhoid fever.
Often, a man’s pigment level is elevated due to taking medications. Typically, the provocateurs are Levomycetin, Aspirin, and Insulin. Men who work at chemical plants and do not follow safety precautions are also at risk of exceeding concentrations. Therefore, employees of such enterprises are recommended to undergo preventive examinations 1–2 times a year with mandatory blood donation for bilirubin.
Often an overestimated concentration is detected in a child. Approximately 80% of newborns have physiological jaundice. Usually the problem indicates that the baby is premature. The concentration of bilirubin in newborns sometimes reaches 140–240 µmol/liter. If there are no problems with the liver, the indicator returns to normal during the first 2 weeks of life. When the concentration remains elevated, there are risks of genetic disease.
In older children, both male and female, increased concentrations occur as a result of infectious diseases, as well as treatment with antibiotic drugs, sulfonamides, and hormonal agents.
Decline
A reduced level of bilirubin in a man’s blood is not accompanied by a significant health hazard. Often the pigment concentration drops if a man:
- often drinks coffee and strong tea;
- systematically experiences stress;
- is in a depressed state.
However, recently a theory linking low pigment concentrations with diseases of the cardiovascular system, in particular ischemia, has been confirmed. Therefore, if there is insufficient amount of pigment in the blood, a man needs to consult a cardiologist and undergo a detailed examination.
Causes of elevated bilirubin
A significant increase in the content of bilirubin in human blood is due to such reasons as an increase in the intensity of hemolysis of erythrocytes, serious damage to the liver parenchyma with the inevitable disruption of its important bilirubin-excretory function, a significant disruption of the outflow of bile from all bile ducts into the human intestine, severe loss of an enzyme link that is always provides the necessary biosynthesis of bilirubin glucuronides.
In addition, an increase in bilirubin can provoke a serious disturbance in the hepatic secretion of direct conjugated bilirubin into bile, a significant increase in the intensity of hemolysis, which is observed in various hemolytic anemias. You should know that hemolysis can often be increased in case of malaria, B12-deficiency anemia, massive hemorrhages in various tissues of the body, with crush syndrome, otherwise called unconjugated hyperbilirubinemia, and with dangerous pulmonary infarctions.
With a fairly strong increase in a certain concentration of bilirubin in the blood, a person first of all often develops a slightly yellowish characteristic tint of the skin and sclera of the eyes, while the urine takes on a darker color. Because at a greatly increased concentration, bilirubin always leaks into the tissues of the human body, which leads to the coloring of the tissues in a yellowish-gray tint.
In most cases, the accumulation of bilirubin is often accompanied by severe discomfort after various physical activities in the right hypochondrium. Fatigue, fever, and weakness may also occur. If these specific symptoms occur, it is advisable to go to the hospital to have your bilirubin level tested.
Moreover, if the level of this substance is greatly increased, then the next step is to immediately find out the causes of this condition, followed by the appointment of the necessary treatment.
In tiny newborns, blood for testing is always taken from the heel, while in adults it is taken from a vein. It is recommended to do this analysis in the morning and on an empty stomach. To get correct objective results, you should not drink for 4 hours before donating blood.
A significant increase in bilirubin in the blood is caused by such conditions and diseases of the liver and blood as anemia, problems with the gallbladder, disorders of the formation of bilirubin in the liver, helminthic infestation and vitamin B12 deficiency.
Congenital or acquired anemia often leads to a significant acceleration of the process of direct destruction of red blood cells in humans, due to which the level of bilirubin rises. At the same time, all other links of the chain in this case are completely intact. This anemia is characterized by an increase in indirect bilirubin. Due to autoimmune and many other diseases such as malaria, acquired hemolytic anemia can develop.
A significant impairment in the formation of direct bilirubin in the liver is considered the second most important possible cause of the disease. These include all types of cancer, hepatitis and cirrhosis. Along with this, increased bilirubin levels are also characterized by hereditary diseases, Gilbert's syndrome, when the correct production of liver enzymes is severely impaired. To find out the cause, specific additional tests must be done.
Problems with the gallbladder can also trigger this condition. If there is a serious violation of the outflow of bile from the gallbladder itself, an increased level of direct bilirubin is often observed. Among other things, in quite rare cases it can be said that taking certain medications due to their side effects can change the level of this bile pigment in the blood.
You should also not underestimate the prevalence of dangerous worm infestations. Numerous types of parasites in the human body can often produce, in addition to the main symptoms of infection, an increase in bilirubin levels. A significant deficiency of vitamin B12 can also trigger the disease.
How to normalize bilirubin metabolism
It is important to keep the level of the substance normal, but traditional methods are useless here. It is necessary to identify the cause of the pathology and undergo treatment with drugs, strictly following the doctor’s instructions. In case of liver disease, a man will have to go to hospital and adhere to a strict diet. If the concentration disorder is caused by blockage of the bile ducts with stones, they resort to surgery.
Although hereditary pathologies are not amenable to drug therapy, the man’s condition is maintained with periodic red blood cell transfusions. In case of severe genetic diseases, excision of the spleen is recommended.