Maps and diagrams of Vienna
The page shows a map of Vienna in Russian.
Use the menu on the left to mark the necessary points of interest on the map, for example, attractions in Vienna. Zoom out on the map to see where Vienna is located on the map of Austria. This page has added a Vienna metro map, street map and hotels. Also on the interactive maps in the list below you can find the Vienna train station and airport, and see the center of Vienna on the map. Mobile applications with offline maps are available for download.
Popular cards
Interactive map of Vienna in Russian from Google
Panoramas, attractions, stops
Interactive map of Vienna hotels from Wikimapia Search for objects, restaurants, hotels, view areas and streets
Detailed map of Vienna by district from Bing Transport stops, hotels, shops, attractions
Attractions of Vienna on a map from Sygic Maps Tourist map of the city
Map of the city of Vienna from Austria.info Transport, shops, cafes and restaurants, attractions
Schemes and road maps
Vienna road map from ViaMichelin
Map of roads and stops in Vienna from Here
Vienna railway map from OpenRailwayMap
Map of Vienna cycling routes from Bikemap
Vienna parking map from Parkopedia
Schemes and maps of public transport
Interactive Vienna metro map from Yandex Stations and metro lines and much more
All Vienna transport on the map Bicycle routes, parking, traffic and more
Map of Vienna public transport routes from Wikiroutes Metro, buses, minibuses, trams
Map of Vienna public transport routes from Moovit Metro, buses, trams
download in PNG format
download in PNG format
Vienna Tourist Bus Route
Maps for smartphones (iOS, Android)
CityMaps2Go for Android Offline maps
CityMaps2Go for iOS Offline maps
Google Maps for Android Navigation and public transport
Google Maps for iOS Navigation and public transport
Map of Vienna offline for Android City map offline
Vienna Offline City Map Lite for Android City map offline
Locus Map Free for Android Outdoor GPS Navigation and Maps
Other maps and diagrams
Vienna tourist map from Lonely Planet Architecture, entertainment, shopping
Weather map in Vienna from Windy Air temperature, precipitation, wind
Map of Vienna Airport Interactive diagram on the official website
Wi-Fi coverage areas in Vienna Interactive map
Map of Vienna with attractions
Vienna city center walking map
Vascular diseases
Anatomy as a branch of biology is studied at school, and then they become acquainted with diseases of the circulatory system. The most dangerous are those that pose a threat to life:
- stroke;
- hypertension;
- aneurysm of the thoracic artery and abdominal cavity;
- ischemic disease;
- atherosclerosis of the carotid artery;
- renal vascular problems.
Diseases of the lower extremities lead to poor circulation, valve pathologies and slower fluid clotting. Atherosclerosis affects large and medium-sized vessels - the aorta, femoral, iliac and popliteal arteries. This leads to severe pain and impaired movement. Varicose veins most often affect women after 40 years of age; men are almost unaffected by this disease. The expansion and contraction of veins, which ensures the movement of blood through the vessels, becomes difficult. Nodes form and the walls become thinner.
Diseases are treated by angiosurgeons and phlebologists. They examine the patient, make a diagnosis, and apply surgery or preventive measures. Medicines help improve lipid metabolism and blood rheology, and reduce cholesterol levels. The doctor will also prescribe vitamin and mineral complexes and draw up a table for their intake.
As a preventive measure, you need to do warming massages and exercise. Healthy blood vessels will keep your limbs and internal organs healthy.
In case of formation of seals in the veins, severe pain or discomfort, you should be examined by a doctor.
Previous
AnatomyCerebral cortex structure and functions, what controls, the surface of the cerebral hemispheres is formed by gray matter, what advantage does folding give
Next
Anatomy: Autonomic nervous system definition, structural features, divisions, classification, functions, importance of the organ in human life, diseases
Venous system structure
The topographic anatomy of the human venous system, depending on its location, is conventionally divided into superficial and deep. The deep veins bear the heaviest load, since up to 90% of the total blood volume passes through them. Superficial veins account for only up to 10% of the blood. Superficial vessels are located directly under the skin. Topographic anatomy distinguishes the greater and lesser saphenous veins, the veins of the plantar zone and the back of the ankle, as well as branches.
The great saphenous vein of the leg is the longest in the human body and can have up to ten valves. The great saphenous vein of the leg begins with the internal vein of the foot and then connects with the femoral vein, which is located in the groin area. Its topographical scheme is such that along its entire length it includes the venous branches of the thigh and leg, as well as eight large trunks. The small saphenous vein of the leg begins on the outer area of the foot. Curving around the back of the lower leg, under the knee it connects with the veins of the deep system.
Two venous networks are formed in the foot and ankle: the venous subsystem of the plantar part and the subsystem of the dorsum of the foot. The superficial veins in the human legs are located in the fat layer and do not have the same muscular support that the deeper vessels have. It is because of this that superficial veins are more likely to suffer from diseases. But the deep veins of a person’s legs are completely surrounded by muscles that provide them with support and promote blood movement. The topographic scheme of the dorsal arches forms the anterior tibial veins, and the plantar arch forms the posterior tibial and receiving peroneal venous vessels.
The superficial and deep veins are connected to each other: through the perforating veins there is a constant release of blood from the superficial veins to the deep ones. This is necessary in order to remove excess pressure on the superficial veins. These vessels also have valves, which, due to various diseases, can stop closing, collapse and lead to various trophic changes.
The topographic scheme of the location of the veins determines the following zones: perforators of the medial, lateral and posterior zones. The veins of the medial and lateral group are called straight because they unite the superficial veins with the posterior tibial and peroneal veins. The posterior group of veins does not enter into large vessels - and therefore they are called indirect venous vessels.
Two venous systems - deep and superficial - are connected and pass into each other. These connecting vessels are called perforating vessels.
Women's magazine - Secrets of health and beauty
Structure and functions of the venous system
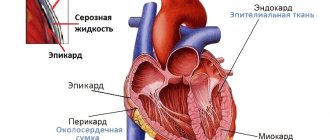
Arterial blood from the left ventricle in the heart enters the aorta, then through the arteries extending from it, which are divided into smaller ones (down to capillaries), it is sent to organs and tissues. In the process of circulation through the capillaries, this blood takes metabolic products from the tissues, is saturated with carbon dioxide and is collected through the venous capillaries into veins, gradually increasing in size, and directed to the heart. The venous system of the systemic circulation consists of a number of morphologically distinct systems. These primarily include the portal and inferior vena cava systems, as well as the portal vein system, which collects blood from all organs and tissues. The superior and inferior vena cava empty into the right atrium. The superior vena cava system consists of veins of the trunk, head and upper extremities. The inferior vena cava system consists of the vessels of the lower extremities, partly the veins of the torso located below the diaphragm, the renal and portal veins. The portal vein collects blood from the unpaired abdominal organs (spleen, stomach, pancreas and intestines), divides into right and left branches and drains into the liver. Here the branches gradually divide into capillaries, the blood from which collects in the hepatic veins. The latter flow into the inferior vena cava.
The structure of the veins of the upper and lower extremities
has its own characteristics. The first is the presence of a superficial and deep vein system; the second is the presence of valves on the inner surface of the veins, which play a large role in the outflow of blood.
The valves are located from the fingers to the shoulder and from the toes to the thigh. The number of valves in the arms and legs decreases from the fingers to the shoulder and the toes to the thigh. There are up to 20 veins in the arms and up to 25 valves in the legs. A feature of superficial veins is the presence of large trunks running independently of the artery. Deep veins always follow strictly along the arteries of the same name. They usually come in pairs. Superficial veins flow into deep veins. In addition, they are connected to each other by connecting vessels through which blood flows from the superficial veins to the deep ones.
Functions of the venous system
The venous system carries out the outflow of blood saturated with carbon dioxide and metabolic products. In addition, hormones from the endocrine glands, as well as various nutrients absorbed in the gastrointestinal tract, enter the bloodstream thanks to the veins. Veins play a role in the regulation of general and local blood circulation, as well as in the spread of various disease processes: inflammatory (thrombophlebitis), tumor (metastasis), embolism (fat, air, etc.).
Blood circulation through veins is significantly different from circulation through arteries. Arterial blood is normally expelled by heart contraction under a pressure of 120 mmHg. Art., in the capillary network the force of the cardiac impulse fades, and the pressure drops to 10 mm Hg. Art.
In this regard, the pressure and speed of blood flow in the veins are much lower, the total capacity of the venous system is 2 times higher than the capacity of the artery. That is why the same volume of blood thrown into the aorta by contraction of the left ventricle must be distributed in a much larger container with a slower flow of venous blood. This is the main difference between the venous system and the arterial system. The exception is blood circulation in the small circle, where the vessel capacities are the same.
The second distinctive feature of the venous system is the movement of blood predominantly against the force of gravity, and therefore the venous blood experiences the full force of hydrostatic pressure.
Structure of the venous system
The venous wall consists of three layers without sharp demarcation with a predominance of collagen tissue in all of them, which provides special strength to the vein wall. Muscle tissue is located in the form of separate bundles in the longitudinal and spiral-circular directions. Passive resistance to hydrostatic pressure is carried out in the vein due to the collagen layer of elastic fibers, active - due to muscles. However, the muscles do not provide complete compensation for hydrostatic pressure, therefore, under unfavorable conditions, stretching of the veins occurs and obstruction of blood outflow.
The most important factors determining normal venous outflow of blood include contraction of the muscles of the limb, respiratory movements of the diaphragm, tension and relaxation of the abdominal press and the suction force of the chest with changes in negative pressure during inhalation and exhalation. The suction force of the chest most affects the venous outflow of the upper extremities and other vessels flowing into the superior vena cava.
Valves play a primary role in venous blood flow. The presence of a valve apparatus in the veins determines the central movement of venous blood and regulates collateral circulation. The speed of venous blood flow and pressure largely depends on the tone of the venous wall, which is constantly under the influence of motor and sensory innervation, as well as under the influence of substances in the blood. The thickness of the venous walls, along with other factors, promotes the movement of blood to the heart and regulates the filling of blood in the right ventricle.
Veins have one more ability: when venous outflow is difficult, through connecting connections, an additional path of blood is carried out from one system to another (for example, from deep to superficial).
The structure of the veins of the lower extremities
The veins of the lower extremities are located in the soft tissues at different depths and form a venous network, which is divided into two sections - superficial and deep.
Superficial veins are located directly under the skin. These are the large and small saphenous veins and their smaller tributaries. The tributaries of the great saphenous vein collect blood from the front surface of the foot, from the front and inner surfaces of the leg. Next, the trunk of the vein passes along the inner surface of the thigh and flows into the femoral vein in the groin area. Through the system of the great saphenous vein, blood flows from 2/3 of the surfaces of the lower limb. The small saphenous vein is located on the back of the leg and flows into the popliteal vein at the border of the knee joint. The superficial saphenous veins of the thigh and leg are accessory and assist the veins located deep in the muscles. The small saphenous vein provides the outflow of venous blood from the outer surface of the leg. It anastomoses with the deep vein system of the leg through direct and indirect connecting veins.
The deep veins (posterior and anterior tibial, popliteal, femoral, deep vein of the thigh) are located along the muscles and provide the outflow of 80–90% of venous blood from the legs. There is a communication between the deep and superficial veins - communicating veins (connecting). Under normal conditions, the communicating veins of the leg and thigh carry out the outflow of blood from the superficial veins to the deep ones.
Vein valves
In ensuring the direction of both arterial and venous blood flow, the valves of the heart, pulmonary artery, aorta, and also the venous system play a decisive role. There are a lot of valves in the lymphatic vessels. The valves are composed of collagen, elastic and smooth muscle fibers. On both sides they are covered with endothelium. A feature of the veins of the lower extremities is that in their branches, at the point of confluence with a more fragile vein or at the confluence of equal veins, there is a valve, and where the vein flows into a more fragile one, a valve is always found in the latter below the confluence of the collateral. There are significantly more valves in the venous collaterals than in the main veins. There are especially many valves in the muscle veins. The valves are specific to the veins of the lower extremities. They are not found in the portal vein system, in the veins of the lungs, brain, or neck. There are no valves in the vena cava, the common iliac vein, and there are few or none in the external iliac vein.
The venous valves regulate the maintenance and direction of blood flow in the inferior vena cava system. They ensure the movement of blood in a strictly defined direction. Valves in the main saphenous veins ensure that blood flows only towards the center. Meanwhile, the movement of blood through connecting (communication) veins is possible only towards the deep veins. In the system of deep veins of the lower extremities, with full valves, blood flows only to the center.
Despite the presence of valves in the inferior vena cava system, the movement of blood through it largely depends on the position of the person. In the supine position, blood flow occurs at a venous pressure equal to the pressure in the veins of the upper extremities. In a standing position, 85–90% of the blood from the saphenous veins enters the deep veins through the connecting veins, where hemodynamic conditions are much better than in the superficial veins. Thus, if the structure of the valves is normal, the horizontal discharge of venous blood from the saphenous vein system is directed only towards the deep veins. While walking, hemodynamic conditions improve dramatically as a result of the active function of the musculofascial pumps of the foot and lower leg.
Vein valves are subject to various kinds of pathological changes. During intrauterine development and in childhood, when the formation of venous valves is largely completed, anomalies in their structure are already observed. Congenital inferiority of the valves creates the preconditions for disturbances of venous outflow and accelerates the development of varicose veins.
Observations of complete congenital absence of valves in the veins of the lower extremities, manifested by severe forms of varicose veins, are described. In turn, factors contributing to the development of varicose veins lead to the occurrence of relative insufficiency of previously complete valves. With the development of varicose veins, the relative insufficiency of the valves increases and is accompanied by deformation and then destruction of the valve leaflets in the process of phlebosclerosis. To the greatest extent, phlebosclerosis develops in the superficial veins, therefore severe pathological changes in the valves are also observed in the superficial veins. Due to fibrosis, thickening, shortening and deformation of the valve leaflets occur; they no longer close, which is the cause of valve failure. In deep veins, the process of phlebosclerosis is, as a rule, less pronounced, and valve incompetence is often caused by uniform dilation of the veins. Naturally, the anatomical inferiority of individual valves can be combined with the acquired relative inferiority of other venous valves. In addition, with increasing age, atrophy of individual valves may develop, which also creates the preconditions for disturbances in venous outflow and the occurrence of local hypertension in the veins. As a result, the function of the underlying valves may also be impaired.
The second most common cause of morphological changes in valves, up to their complete destruction, is thrombosis. Venous valves are sometimes damaged during injury. A person falling from a height of several meters onto their feet can be accompanied by rupture of the valve flaps. Thus, with varicose veins, valve dysfunction develops under the influence of various factors and is observed in all parts of the venous system of the lower extremities: in the deep, superficial, connecting and smallest veins. Valve dysfunction underlies the development of varicose veins.
For normal blood circulation, it is necessary for blood to move through the veins from the periphery to the center, i.e., to the heart, and not move back under the influence of gravity. This is ensured by the valves located on the inner wall of the vein. When blood flows in the normal direction towards the heart, the valve flaps open and allow blood to flow through. If the blood flow rate is high, the valve leaflets are pressed against the walls of the vein. If the blood slows down, the valve gradually closes its doors. When the blood tends in the opposite direction, the valves close completely and thus prevent the reverse flow of blood. Blood circulation is ensured due to the pressure difference. From places of high pressure, blood flows to places where the pressure is lower, and the greater this difference, the stronger the blood circulation, the more intense the metabolic processes. The pressure in arterioles should be greater than in venules. This forces blood from the capillaries to flow into the venules, and then into larger veins and move further to the heart, where the pressure in the vein is lowest. If the pressure in the venules increases, then the rate of metabolic processes decreases accordingly. If the pressure in the venules was equal to the pressure in the arterioles, then the blood would stop altogether and metabolic processes would cease. There is one more important circumstance. The walls of veins and arteries are structured differently. Both vessels must be elastic, i.e., have the ability to expand and contract depending on need. But arteries have a thick wall due to a large number of collagen, elastic and muscle fibers. This allows the arteries to pulsate, helping blood flow. But the walls of the vein contain fewer such fibers and therefore are not as elastic as the walls of the arteries. However, the elasticity of the veins of the extremities is maintained externally. After all, they are surrounded by muscles, which, when in contact, put pressure on the veins and promote blood flow.
The diameter of each specific vessel and the structure of its wall are determined by the direct function of this particular vessel. For example, the smallest veins, venules, do not have a muscular layer, but have only an endothelial and fibrous membrane. The walls of the venules are thin. Therefore, in the event of an excessive increase in internal pressure due to obstacles that arise in the veins during the outflow of blood, these smallest vessels will be the first to fail. The largest veins, the hollow ones, have a large diameter and, accordingly, the thickest wall. They do not participate in metabolism and play only the role of a transfer capacitance. The question arises: what causes blood to rise through the veins back to the heart? To do this, there is not only one mechanism in the body that promotes constant and uniform circulation of blood flow through the veins.
Firstly, this also happens due to the fact that when you inhale, a partial vacuum is formed in the lungs due to their expansion, due to which a kind of blood suction occurs. Secondly, this is facilitated by the work of muscles, which, when tense, squeezing the veins, help push blood further. Human muscles are therefore sometimes called the second heart. Finally, the venous valves come into play, preventing blood from flowing in the opposite direction. And since it is the malfunction of the venous valves that causes varicose veins, the leg veins are primarily susceptible to varicose veins. Not only because they are the longest, but also because they are the most distant, and the effort required for the blood from the wall to reach the heart is much greater. The large and small saphenous veins are most susceptible to varicose veins.
The great saphenous vein is the longest vein in the human body; it merges with the femoral vein and flows with it into the saphenous vein located in the pelvis. The iliac vein, in turn, flows into the inferior vena cava, which carries blood to the heart. Both veins are located in the fat layer directly under the skin.
To get blood from the lower extremities to the heart, it is necessary to overcome a much greater distance and a much greater force of gravity than from all other parts of the body.
This may be one of the reasons for vein deformation, especially if you inherited weaker veins. If the veins in the lower extremities begin to dilate, this can lead to insufficient closure of the valves, which in turn leads to backflow of blood.
Sections of the veins begin to fill with blood, stretch even more, wriggle, and form peculiar nodes and sacs in the weakest places. Thus, one disturbance causes another. And this process, if you do not intervene in time and stop it, can lead to the most tragic consequences. The process of stretching of the superficial saphenous veins, i.e. the actual development of varicose veins, occurs in cases where the blood does not encounter any obstacles in covering the distance from the foot to the heart.
In these cases, there is a kind of discharge of blood from the deep veins into the superficial ones, which have more degrees of freedom due to the elasticity of the skin. If such a “reset” is a short-term phenomenon, then no special violations occur. If the “obstacle” is not removed for a long time, then eventually distortion and overstretching of the superficial veins occur, especially if they are hereditarily weak.
The speed of venous blood flow and pressure largely depend on the tone of the venous wall, which is constantly under the influence of motor and sensory innervation, as well as under the influence of substances in the blood.
The tone of the venous walls, along with other factors, promotes the movement of blood to the heart and regulates the filling of the right heart with blood. Veins have one more ability: when venous outflow is difficult, a collateral (additional) blood path is carried out through communication connections from one system to another (for example, from deep to superficial).