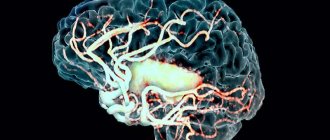
Background retinopathy is a set of ophthalmological diseases that occur when the blood supply to the retina is impaired. The cause of the pathology is the course of certain types of dangerous diseases. Despite its mild course, retinopathy can lead to complete or partial loss of vision.
Retinopathy is a series of retinal pathologies that occur due to physiological or mechanical damage to the vascular channels and insufficient blood supply to the retina. This disease can occur against the background of inflammatory and non-inflammatory processes. In 99% of cases, background retinopathy (also called secondary) - a condition that develops as a result of the course of another dangerous disease.
Despite the fact that the pathology often occurs without pronounced symptoms, background retinopathy can be accompanied by serious consequences. That is why it is necessary to diagnose and treat a dangerous disease in time.
Etiology of the process
Retinopathy and pre-retinopathy of the eyes are a complex nosology . A similar term refers to lesions of various origins that are not associated with inflammation of the retina itself. The disease progresses rapidly, which provokes serious disruptions in blood flow in the mesh structures. This is a dangerous condition, which subsequently leads to hypoxia, ischemia, and degenerative processes.
The causes of the pathology are directly related to the type of lesion. It has not been proven what exactly provokes the occurrence of primary retinopathy. Secondary ailments occur in a number of diseases:
- injury;
- systemic form of atherosclerosis;
- hematological lesions;
- toxicosis.
Retinal disease of newborns has a different etiology. The main reason for this condition is the problematic, defective development of retinal elements during the period of intrauterine development. Often, pathology develops in premature babies. The main aggressive factor is intensive oxygen supply .
Causes of the disease
The main mechanism for the appearance of retinopathy is a persistent disruption of the blood supply to the retina over a long period of time.
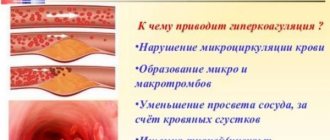
In accordance with the etiological classification, microcirculation disorders can lead to:
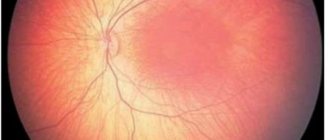
- Hypertonic disease. The vessels of the fundus are in a state of prolonged spasm due to a persistent increase in blood pressure. The small vascular network begins to hyalinize against the background of protein dystrophy. Because of this, the blood walls become “vitreous” (become fragile and brittle). The next stage is angiosclerosis. The lumen of blood vessels is significantly reduced due to the formation of connective tissue, and their walls lose the ability to contract and relax normally. Severe congestion occurs, so the optic disc becomes swollen. Further progression of the changes is fraught with vision loss.
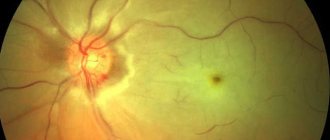
- Systemic atherosclerosis. The initial stages of retinal changes are similar to those in arterial hypertension. Fundamental differences appear only at the last stage: due to the appearance of capillary microhemorrhages, the deposition of insoluble crystals formed from frozen inflammatory fluid (exudate) occurs along the vascular network. The optic disc (optic disc), which is in a state of lack of blood supply, becomes pale.
- Diabetes. This retinopathy is similar in morphofunctional changes observed in hypertension and atherosclerosis in the first two stages. The differences begin from the third stage: diabetic retinopathy with a tendency to proliferation is formed. In conditions of constant insufficiency of blood supply, compensatory neovascularization of the retina occurs. The resulting vessels are defective due to fragile walls that are easily destroyed. Continuation of neovascularization leads to the fact that the vessels are damaged when growing into the vitreous body and cause the formation of multiple areas of small hemorrhages. If the pathological process is not stopped in time, retinal detachment will occur due to excessive tension of the vitreous fibers.
- Blood diseases. The course of background retinopathy will directly depend on the type of hematological pathology. Changes in the retinal microvasculature can result from:
- Polycythemia (thrombosis of small vessels, followed by hyalinization and sclerosis of their walls, as well as severe swelling of the optic nerve head);
- Anemia (pathological expansion of the lumen of blood vessels and frequent hemorrhages lead to retinal detachment);
- Leukemia (tortuosity of the vascular bed, accompanied by frequent hemorrhages and the release of exudate under the retinal tissue);
- Multiple myeloma (the formation of a pathological protein causes blood thickening and, as a result, persistent dilation of the retinal vessels with a tendency to hemorrhage).
- Traumatic injury. Retinopathy is often observed in people who have suffered severe and prolonged chest compression. Such a traumatic factor leads to the arterioles of the fundus going into a state of persistent contraction. Vasospasm causes retinal hypoxia. Under conditions of lack of oxygen, transudate (non-inflammatory fluid) begins to sweat through the vascular wall, leading to retinal edema.
A number of specialists include additional points in the considered etiological classification:
- Vascular changes in the retina due to autoimmune damage;
- Retinopathy due to radiation exposure;
- Pathology of retinal vessels due to thrombosis of the central retinal vein.
Principles of classification
To prescribe adequate therapy, it is important to know the characteristics of the disease. The disease comes in different subtypes. Each of them has its own symptoms of retinopathy, pathogenesis, and etiology of the process. In medicine, there are 2 main groups of retinopathy: primary and secondary processes.
Primary lesions are severe ophthalmic lesions, the cause of which is not fully understood. Secondary processes develop against the background of other ailments that occur in the body. They are considered a complication of other diseases. Background retinopathy in newborns is highlighted separately.
Primary lesions include:
- central serous retinopathy;
- rear multifocal;
- exudative form.
Treatment of the disease
Background retinopathy and retinal vascular changes, the causes of which are concomitant diseases, require a separate approach. First, it is necessary to eliminate this cause, that is, try to cure or prevent the development of diseases that provoke disorders in the retina. Only after this can you resort to ophthalmological treatment methods.
In newborns and children under one year of age, the process of retinal destruction can be reversible. The child must be under constant medical supervision and undergo preventive treatment every year in the ophthalmology department. In more serious cases, laser coagulation may be offered as a method of vision correction. If the condition is very advanced and treatment does not bring results, removal of the vitreous may be indicated.
In adults, retinopathy is treated depending on concomitant conditions:
- If a person suffers from hypertension, the disease is treated with antihypertensive drugs, antispasmodics, and vitamins. Laser cauterization may be used.
- Atherosclerotic changes in blood vessels are treated with drugs that dilate blood vessels, lower cholesterol, angioprotectors, diuretics and antioxidants.
- Blood diseases also lead to serious circulatory problems in the retina. Therefore, success in the treatment of retinopathy in this case directly depends on the success of treating the patient’s blood disease.
It should be remembered that if treatment is not started in time, the disease can have very serious consequences. Among them: hemorrhages, optic nerve atrophy, cataracts, scarring or retinal detachment, and even blindness.
ICD-10 category: H35.0
Pathology in newborns
The reasons for the development of retinopathy in infants are the incompletely formed elements of the eye. The main etiology of the rapid progression of the disease is nursing babies in oxygen incubators. It has been proven that it is high concentrations of oxygen that destroy delicate eye structures. The body compensates by stimulating the growth of new capillaries. This aggravates the course of the disease. The risk of retinopathy is especially high in babies under 31 weeks.
For retinopathy, treatment is carried out after a complete examination of the child. Therapy starts a few weeks after the baby is born. It has been proven that only timely and complete therapy can provide healing and complete restoration of vision. If the condition does not improve with therapy, specialists resort to surgery. Cryoretinopexy or laser coagulation is more often used. Infantile retinopathy should not be left unattended. Otherwise, it will develop into myopia, glaucoma, strabismus, or even end in retinal detachment.
How is it diagnosed?
Undesirable changes in the organs of vision can be detected using ultrasound.
Background retinopathy and other changes in the eyes can be detected using ophthalmoscopy. In addition, an ultrasound examination of the organ is performed, which helps to detect foci of hyaline and scar changes. Angiography is also performed to determine the condition of the vascular network. Magnetic resonance imaging, electroretinography and biomicroscopy are indicated. It is important to take a general and biochemical blood test, as well as determine the main cause of retinopathy.
Diagnostics and treatment methods
The success of therapy depends entirely on the timeliness and correctness of the diagnosis. Patients with suspected retinopathy are examined comprehensively. The list of standard methods includes:
- ophthalmoscopic examination;
- tonometric examination;
- perimetry;
- Ultrasound.
Treatment of the disease depends on the severity, extent and extent of damage. Ophthalmologists use both conservative and surgical treatment methods. It is recommended to treat the patient taking into account the results of the examination, his general state of health and the individual characteristics of the body.
Conservative therapy includes the use of ophthalmic drops. For surgical intervention, coagulation and vitrectomy are chosen. The patient may be prescribed oxygen barotherapy or vitreoretinal surgery .
Navoyan Maranush Meruzhanovna
Pediatric ophthalmologist.
Graduated from Moscow State Medical and Dental University.
A.I. Evdakimova, 2014 Specializes in examination and assessment of visual functions at the initial appointment (skiascopy, direct and indirect ophthalmoscopy, biomicroscopy, tonometry, refractometry, determination of the angle of strabismus, study of binocular vision), performing p/b and s/c injections, examination with a Goldmann lens, selection of spectacle correction.
This might be interesting
- Myopia in children
- Strabismus in children
- Pediatric ophthalmologist
- Farsightedness in children
- Dacryocystitis of newborns
Preventive measures
Ophthalmologists have developed special measures that make it possible to most likely prevent the appearance of the slightest signs of damage. To prevent the disease, constant clinical monitoring of patients at risk is recommended. First of all, the ophthalmologist should monitor hypertensive patients suffering from atherosclerotic disease.
It is important to prevent retinopathy in children. This requires careful management of pregnancy and improved conditions for the survival of children. After suffering from retinopathy, all young patients should be registered with an ophthalmologist until they are 18 years old.
Retinopathic eye disease is a serious and insidious disease. It does not manifest itself for a long time, but at the same time it greatly worsens the condition of the visual analyzer. Such a pathology cannot be ignored. In advanced forms, retinopathy leads to blindness.
What are the main symptoms of background retinopathy?
Regardless of the form, background retinopathy has the same clinical picture. The first symptoms are detected during the transition from the second to the third stage of the disease:
If at the stage of development of the disease a person has diabetes mellitus, then background retinopathy makes itself felt with the following symptoms:
- photopsia - sparks or flashes of light may appear in the eyes;
- inability to perceive colors correctly;
- decreased contrast of visible objects.