Description and concept
The disease is quite rare - about 20 cases per 100,000 newborns are registered annually. Vascular malformation of the brain is a pathology with an incompletely understood cause, which most often affects men aged 20 to 40 years. Basically it is congenital. Can occur in both the brain and spinal cord.
The classification of the disease consists of the following types of pathology:
- Arterial;
- Arteriovenous fistulous;
- Arteriovenous micromalformation;
- Arteriovenous cavernous;
- Telangiectasia;
- Venous malformation of cerebral vessels;
- Dural fistula located in the dura mater;
- Hemangiomas.
Mechanism of action of the disease
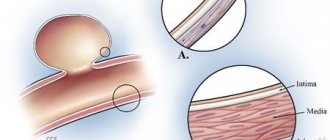
The abnormal structure of vascular tangles leads to their failure. Numerous weaves and different diameters make the walls fragile and brittle. Due to the fact that most of the malformations are arterial-venous (AVM), blood circulation is also impaired. In angiomas, mixing of venous and arterial blood occurs. This leads to oxygen deficiency in the brain tissue.
Nerve cells are exposed to ischemia and hypoxia. Compensatory mechanisms maintain them in this state. But over time, brain cells die. The glomeruli of the malformation are prone to destruction due to their fragile structure. Mixed arteriovenous blood flows into the intracranial cavity - hemorrhage occurs.
In addition, malphromation of cerebral vessels can cause compression of intracranial structures. And, consequently, the appearance of neurological symptoms. Depending on where the abnormal focus is located, the severity of clinical manifestations will depend.
Possible complications
Even before the malformation manifests itself clinically, the person will latently develop irreversible pathomorphological phenomena. This occurs due to hypoxia of a section of brain tissue, its degeneration and death. Depending on the location of the affected area, characteristic focal symptoms are observed (impaired speech, gait, voluntary movements, intelligence, etc.), and there may be epileptic seizures.
Severe complications begin already in adulthood. Abnormal vessels have thin walls and are more susceptible to rupture, so ischemic strokes are more common in patients with malformations.
Large conglomerates of arteries and veins compress the tissue around them, causing hydrocephalus. The most dangerous is hemorrhage resulting from the rupture of several vessels at once.
This can either have fatal consequences or end with virtually no consequences. It all depends on the amount of blood shed.
Hemorrhagic stroke has a much poorer prognosis and may recur over time.
Ignoring the symptoms of vascular malformation increases the likelihood of developing complications of the disease. Abnormal vessels can lead to insufficient blood supply to certain areas of the brain, causing hypoxia.
Hypoxia, in turn, leads to degeneration and death of brain tissue. As a result, the clinical picture of ischemic stroke develops.
Compression of surrounding tissues can lead to the development of hydrocephalus of the brain, persistent movement disorders, and severe neurological disorders.
A very serious consequence of malformations is cerebral hemorrhage. Depending on the volume of hemorrhage and its location, the result can vary from headache to death.
Even before the rupture, when a vascular malformation exists, a person experiences insufficient blood supply to a certain area of the brain, that is, its hypoxia. As a result, dystrophy and gradual death of brain tissue occurs.
This phenomenon can provoke ischemic stroke, which is accompanied by loss of vision, memory, paresis and paralysis, speech impairment and other various and severe disorders. Large AVMs put pressure on surrounding tissues so that they cause dropsy (hydrocephalus).
Causes
A small group of factors can trigger the process of malformation. These include:
- Congenital structural abnormalities of vascular walls;
- Changes in the intima under the influence of atherosclerotic and hyperplastic processes;
- Traumatization of the angiotic network.
These reasons lead to changes in the configuration of arteries and veins. In some cases, communicating vessels are formed. This dramatically increases the speed of linear cerebral blood flow. Vascular glomeruli can reach impressive sizes and have a bizarre shape. They are located in almost any part of the angiotic bed of the brain.
Signs of arterial rupture
Common symptomatic manifestations of a ruptured vessel are:
- Headache of varying intensity;
- Feeling of ringing and noise in the ears;
- Loss of consciousness;
- Nausea and vomiting that does not bring relief;
- Increased intracranial pressure;
- Decreased function of vision, smell, speech and hearing;
- The appearance of hallucinations in the form of red flashes before the eyes.
The body will signal the patient that a hemorrhage has occurred. With malformation of cerebral vessels, the signs worry the patient. You shouldn't ignore them. Timely contact with a specialist can save lives. After all, the skull is a closed space. And uncontrolled bleeding often causes adverse consequences for the patient.
Symptoms
In approximately 50% of cases, symptoms of malformation manifest as a sudden cerebral hemorrhage, that is, a stroke. Other potential complications include seizures, headaches, and disturbances in movement, speech, and vision. These complications may accompany cerebral hemorrhage or occur independently.
Brain hemorrhage
The risk of hemorrhage is about 2–4% per year. In the year following the first hemorrhage, the risk of recurrence is highest. After the first hemorrhage, if left untreated, the risk of repeated hemorrhage increases threefold. However, then, for unknown reasons, the risk of recurrent hemorrhages gradually decreases year after year.
Symptoms of hemorrhage depend on the location of the malformation, as well as the amount of bleeding. These symptoms may include:
- sudden severe headache, nausea and vomiting;
- epileptic seizures;
- loss of consciousness;
- speech impairment, numbness, tingling, weakness in the muscles of the limbs, visual impairment.
Hemorrhage occurs as a result of weakening of blood vessels due to shunting of arterial blood directly into the veins through the AVM. The short- and long-term neurological consequences of hemorrhage depend on the volume of blood leaked and the location of the hemorrhage. Some factors responsible for spontaneous bleeding in the absence of or before drug treatment include:
- history before cerebral hemorrhage;
- presence of previous hemorrhages;
- aneurysms of the feeding arteries.
Epileptic seizures
Epileptic seizures not caused by hemorrhage are present as an early symptom in 16–53% of patients. The following types of seizures are noted:
- A generalized seizure involving the entire body and accompanied by loss of consciousness. This type is most typical for frontal AVMs.
- Focal epileptic seizures and involuntary muscle contractions depending on the location of the AVM in the brain. In this case, loss of consciousness usually does not occur. These types of epileptic seizures are most common in parietal malformations.
An epileptic seizure occurs when there is a short burst of electrical activity in a specific part of the brain or throughout the brain. Scar tissue present within or surrounding abnormal blood vessels is thought to disrupt normal electrical activity in the brain.
Headache
Headache is a symptom that allows diagnosing AVM in 7–48% of patients. These headaches usually have no distinguishing characteristics such as frequency, duration, or severity. The role of AVM in the occurrence of these headaches is also unclear.
Symptoms resembling cerebral hemorrhage
Focal neurological disorders without signs of hemorrhage are observed in 1–40% of patients. Typically, these signs have been attributed to redirection of blood flow through the AVM and resulting insufficient blood supply to the brain. However, there is no compelling reason to consider this phenomenon to be a clinically important mechanism.
Another hypothesis is that the abnormal blood vessels that form the core of the malformation pulsate and press on adjacent parts of the brain. One study showed that 66% of patients with malformation had difficulty learning information, leading to thoughts of a brain malfunction even before the development of clinical signs of this pathological condition.
Classification and types of vascular malformation
There are several divisions of this pathology into types. The most common classifications are the following:
- Hamburg;
- International Society for the Study of Vascular Anomalies (ISSVA);
- Schobinger.
According to Hamburg malformation, it can be:
- Arterial;
- Venous;
- Shunt arteriovenous;
- Lymphatic;
- Microvascular or capillary;
- Combined.
The same classification suggests dividing abnormal glomeruli into:
- Stem and non-stem;
- Limited and diffuse;
- Deep and superficially located.
The International Society for the Study of Vascular Anomalies (ISSVA) proposes to evaluate blood flow velocity in malformations. She may be:
- Fast;
- Slow.
The first is divided into:
- Arterial;
- Arteriovenous;
- Arteriovenous fistula - fistula.
Slow ones are:
- Capillary;
- Venous;
- Lymphatic;
- Combined.
Schobinger's classification is based on the stages of development of the pathological process:
- The first characterizes peace. In this case, there may be hot and reddened skin over the malformation;
- The second means expansion or increased growth. The signs of the previous stage include the growth of vessels in diameter, their expansion, and the development of a convoluted structure. Externally, increased pulsation of the arteries appears;
- The third signifies the beginning of destruction. The existing disorders are accompanied by a decrease in tissue nutrition, as well as ulceration and bleeding;
- The fourth leads to decompensation. The body cannot cope with existing disorders. This is fraught with cardiovascular failure with left ventricular hypertrophy.
Diagnosis of the disease
Often the malformation does not manifest itself in any way until the moment the vessel bursts. Pathology can develop in a patient as a child, and be detected by chance during an examination for other diseases. To do this, use instrumental methods:
- CT;
- MRI;
- Contrast or superselective angiography.
These diagnostic manipulations make it possible to identify the smallest changes in the structure of the brain. A tomography image, both computed tomography and magnetic resonance imaging, helps determine the structure of the organ under study layer by layer. Thanks to these methods, it is possible to identify the shape of the pathological lesion, its size and relationship to other tissues.
Angiography is the most accurate research method for identifying malformations. It is based on x-ray action. The patient is injected with a contrast agent into the vasculature. The connection reaches the head and then it becomes possible to examine the existing arteriovenous malformation in the brain.
Surgical removal of cerebral vascular malformation - stages of surgery
Open surgery to remove malformations of the veins and arteries of the brain is a serious neurosurgical intervention.
It is carried out in the presence of the following indications:
- superficial location of vascular pathology;
- if the malformation is small.
To perform surgery on arteriovenous malformations, craniotomy is necessary. Malformations are often accompanied by hemorrhages. Then, simultaneously with the abnormal choroid plexus, the surgeon also removes the intracranial hematoma.
This type of surgery requires the highest level of general anesthesia.
To carry out the operation you need:
- microsurgical equipment;
- special intraoperative microscope;
- apparatus for ultrasound intraoperative examination.
The steps of the operation include:
- Excision of tissue from the area of the brain where the malformation is located.
- Disconnection from the bloodstream using special clamps of the main source of nerve impulses.
- Complete removal of anomalies of the vascular structure.
- Coagulation of nerve endings.
https://youtube.com/watch?v=3d3UFFY-N1w
During open surgery, it is possible to remove the vascular malformation while minimizing the surrounding tissue. Abnormal vascular plexuses are removed along with large hematomas. Sometimes intracranial hematomas can be a threat to the patient’s life, then an emergency operation is performed to remove them.
If vascular pathology is detected in deep areas of the brain or in areas responsible for many body functions, a neuronavigation unit is used for its precise localization. This equipment allows you to clarify the localization of a vascular formation with an accuracy of 1-2 millimeters.
The use of neuronavigation when operating on functionally significant areas of the brain allows:
- using a stereotactic pointer, identify the exact location of the anomaly;
- coordinate the surgeon’s actions by directing the surgical instrument along the ideal path of access to the malformation;
- perform precise removal of vessels susceptible to anomalies.
One of these operations is clearly shown in the video:
Treatment
For cerebral vascular malformation, treatment can be divided into 2 groups:
- Surgical;
- Medication.
At the current level of development of medicine, preference is often given to the surgical method of therapy. For this purpose, not only open surgical interventions are used, but also minimally invasive ones such as endovascular embolization. However, all surgical treatment methods involve excluding the abnormal glomerulus from the general bloodstream.
The method of endovascular embolization has become widespread. Due to its minimal invasiveness, the operation carries the least likelihood of complications. The access point does not require opening the skull. Through X-ray surgical angiography, it becomes possible to see the entire vascular network, find an abnormal glomerulus and introduce an artificial embolus - a particle that will clog the malformation, turning it off from the general blood flow.
Instead of directly opening the skull, a special catheter is inserted into the patient's femoral artery. And through it they reach the desired brain vessel and inject an embolus. Due to the lack of open access, the likelihood of developing complications is reduced. Patients recover faster. Their rehabilitation is simpler and easier than that of patients operated on with open access. This method has received good reviews from patients.
Another progressive method of treating cerebral vascular malformation is the use of a gamma knife. It is used for deep location of the abnormal glomerulus. The action of this method is based on radioactive radiation collected in a fixed beam. Gamma knife allows you to exclude malformation from the bloodstream. The cost of these procedures is higher than with open access.
The use of medications is a less effective treatment for this disease. Vascular drugs can only improve the rheological properties of blood and oxygen delivery. But medications cannot turn off a pathological focus from the general blood supply. Traditional medicine in this case cannot be considered as the main source of therapy.
Algorithm of actions for diagnosis
To quickly diagnose the disease, a standard algorithm of actions has been developed to help doctors.
At the clinic or outpatient level, the patient’s condition is assessed by:
We also recommend reading: Rupture of a brain aneurysm
- medical history;
- general symptoms;
- measuring temperature, pulse, blood pressure;
- identification of neurological symptoms (if possible, examination by a neurologist);
- consultation with an ophthalmologist.
Mandatory studies:
- general blood and urine tests;
- biochemical tests;
- coagulogram;
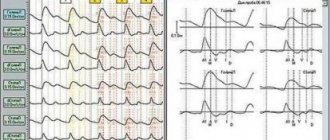
- echoencephalography;
- rheoencephalography of cerebral vessels;
- Dopplerography of the vessels of the head and neck.
If vascular pathology is suspected, the patient should be referred for consultation to the nearest vascular center or to a neurosurgeon.
In specialized departments (centers), examinations are carried out by specialists of related specialties (neurologist, neurosurgeon, vascular surgeon, ophthalmologist). Specific symptoms are identified and differentiated with different pathologies.
Methods used:
- magnetic resonance imaging;
- selective angiography;
- echoencephalography.
Only such consistent actions make it possible to correctly assess the patient’s condition and make a diagnosis of malformation.