Age characteristics
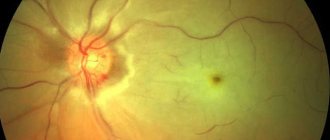
The fundus of the eye in newborns is normally light yellow in color, and the optic disc is pale pink with a grayish tint. This slight pigmentation usually disappears by the age of two. If a similar pattern of depigmentation is observed in adults, this indicates optic nerve atrophy.
The afferent blood vessels in a newborn are of normal caliber, while the efferent blood vessels are slightly wider. If childbirth was accompanied by asphyxia, then the fundus of the children will be dotted with small pinpoint hemorrhages along the arterioles. Over time (within a week) they resolve.
With hydrocephalus or another cause of increased intracranial pressure in the fundus, the veins are dilated, the arteries are narrowed, and the boundaries of the optic disc are blurred due to its swelling. If the pressure continues to increase, the optic nerve nipple swells more and more and begins to push through the vitreous body.
Narrowing of the arteries of the fundus accompanies congenital atrophy of the optic nerve. His nipple looks very pale (more so in the temporal areas), but the boundaries remain clear.
Changes in the fundus of the eye in children and adolescents can be:
- with the possibility of reverse development (no organic changes);
- transient (they can only be assessed at the moment of their appearance);
- nonspecific (no direct dependence on the general pathological process);
- predominantly arterial (without changes in the retina characteristic of hypertension).
With age, the walls of blood vessels thicken, causing small arteries to become less visible and, in general, the arterial network to appear paler.
The norm in adults should be assessed taking into account concomitant clinical conditions.
Methods for treating vasoconstriction in the fundus
Due to the fact that retinopathy is most often of the nature of a systemic disease, their treatment consists of etiotropic therapy of the underlying disease. Vitamin preparations, angioprotectors, tissue preparations (vitreous body, aloe) are prescribed.
In degenerative processes, vasodilators (No-Shpa, Papaverine), which are administered endonasally using electrophoresis, have some effect. Recently, laser coagulation has been used to treat retinodystrophies, which, unfortunately, also gives a temporary effect.
Research methods
There are several methods for checking the fundus. An ophthalmological examination aimed at studying the fundus of the eye is called ophthalmoscopy.
An examination by an ophthalmologist is performed by magnifying the illuminated areas of the fundus with a Goldmann lens. Ophthalmoscopy can be performed in forward and reverse view (the image will be inverted), which is due to the optical design of the ophthalmoscope device. Reverse ophthalmoscopy is suitable for general examination; the devices for its implementation are quite simple - a concave mirror with a hole in the center and a magnifying glass. Direct is used when a more accurate examination is needed, which is carried out with an electric ophthalmoscope. To identify structures invisible in normal lighting, illumination of the fundus with red, yellow, blue, yellow-green rays is used.
Fluorescein angiography is used to obtain an accurate picture of the retinal vascular pattern.
Why does the fundus of the eye hurt?
The reasons for changes in the fundus picture may relate to the position and shape of the optic disc, vascular pathology, and inflammatory diseases of the retina.
Vascular diseases
The fundus of the eye most often suffers from hypertension or eclampsia during pregnancy. Retinopathy in this case is a consequence of arterial hypertension and systemic changes in arterioles. The pathological process occurs in the form of myeloelastofibrosis, less commonly hyalinosis. The degree of their severity depends on the severity and duration of the disease.
The result of an intraocular examination can establish the stage of hypertensive retinopathy.
First: slight stenosis of arterioles, the beginning of sclerotic changes. There is no hypertension yet.
Second: the severity of stenosis increases, arteriovenous crossovers appear (the thickened artery puts pressure on the underlying vein). Hypertension is noted, but the condition of the body as a whole is normal, the heart and kidneys are not yet affected.
Third: constant vasospasm. In the retina there is effusion in the form of “lumps of cotton wool”, small hemorrhages, swelling; pale arterioles have a “silver wire” appearance. Hypertension levels are high, the functionality of the heart and kidneys is impaired.
The fourth stage is characterized by the fact that the optic nerve swells and the blood vessels undergo critical spasm.
Arterial hypertension can be an indirect cause of thrombosis or spasm of the retinal veins and central retinal artery, ischemia and tissue hypoxia.
Examination of the fundus for vascular changes is also required in case of systemic disturbances in glucose metabolism, which leads to the development of diabetic retinopathy. Excess sugar in the blood is detected, osmotic pressure increases, intracellular edema develops, the walls of the capillaries thicken and their lumen decreases, which causes retinal ischemia. In addition, microthrombi form in the capillaries around the foveola, and this leads to the development of exudative maculopathy.
During ophthalmoscopy, the fundus picture has characteristic features:
- microaneurysms of retinal vessels in the area of stenosis;
- an increase in the diameter of the veins and the development of phlebopathy;
- expansion of the avascular zone around the macula due to capillary closure;
- the appearance of a hard lipid effusion and soft cotton-like exudate;
- microangiopathy develops with the appearance of couplings on the vessels, telangiectasias;
- multiple small hemorrhages at the hemorrhagic stage;
- the appearance of an area of neovascularization with further gliosis - the proliferation of fibrous tissue. The spread of this process can gradually lead to tractional retinal detachment.
Pathology of the optic nerve disc can be expressed in the following:
- megalopapilla - measurement shows an increase and pallor of the optic disc (with myopia);
- hypoplasia – a decrease in the relative size of the optic disc in comparison with the retinal vessels (with hypermetropia);
- oblique ascension – the optic disc has an unusual shape (myopic astigmatism), the accumulation of retinal vessels is shifted to the nasal region;
- coloboma – a defect of the optic disc in the form of a notch, causing visual impairment;
- symptom of “morning glow” – mushroom-shaped protrusion of the optic disc into the vitreous body. Ophthalmoscopy descriptions also indicate chorioretinal pigmented rings around an elevated optic disc;
- congestive nipple and edema - enlargement of the optic nerve nipple, its pallor and atrophy with increased intraocular pressure.
Pathologies of the fundus of the eye also include a complex of disorders that occur in multiple sclerosis. This disease has multiple etiologies, often hereditary. In this case, the myelin sheath of the nerve is destroyed against the background of immunopathological reactions, and a disease called optic neuritis develops. An acute decrease in vision occurs, central scotomas appear, and color perception changes.
In the fundus one can detect sharp hyperemia and swelling of the optic disc, its boundaries are erased. There is a sign of optic nerve atrophy - blanching of its temporal region, the edge of the optic disc is dotted with slit-like defects, indicating the onset of atrophy of the retinal nerve fibers. Narrowing of the arteries, formation of couplings around the vessels, and macular degeneration are also noticeable.
Treatment for multiple sclerosis is carried out with glucocorticoid drugs, since they inhibit the immune cause of the disease, and also have an anti-inflammatory and stabilizing effect on the vascular walls. Injections of methylprednisolone, prednisolone, and dexamethasone are used for this purpose. In mild cases, corticosteroid eye drops such as Lotoprednol can be used.
Retinal inflammation
Chorioretinitis can be caused by infectious-allergic diseases, allergic non-infectious, post-traumatic conditions. In the fundus, they appear as many rounded formations of light yellow color, which are located below the level of the retinal vessels. The retina has a cloudy appearance and a grayish color due to the accumulation of exudate. As the disease progresses, the color of inflammatory foci in the fundus may approach whitish, as fibrous deposits form there and the retina itself becomes thinner. The retinal vessels remain virtually unchanged. The outcome of retinal inflammation is cataract, endophthalmitis, exudative, and in extreme cases, atrophy of the eyeball.
Diseases affecting the retinal vessels are called angiitis. Their causes can be very diverse (tuberculosis, brucellosis, viral infections, mycoses, protozoa). The ophthalmoscopy picture shows vessels surrounded by white exudative couplings and stripes, areas of occlusion and cystic edema of the macula area are noted.
Despite the severity of the diseases causing fundus pathologies, many patients initially begin treatment with folk remedies. You can find recipes for decoctions, drops, lotions, compresses from beets, carrots, nettles, hawthorn, black currants, rowan berries, onion peels, cornflowers, celandine, immortelle, yarrow and pine needles.
I would like to draw your attention to the fact that by taking home treatment and delaying a visit to the doctor, you may miss the period of development of the disease at which it is easiest to stop it. Therefore, you should regularly undergo ophthalmoscopy with an ophthalmologist, and if pathology is detected, carefully follow his instructions, which you can supplement with folk recipes.
Vasoconstriction is an important mechanism in the development of many diseases. The normal state of the vascular bed presupposes a sufficient supply of organs and tissues with blood, and due to the blood supply - with nutrients, components for energy production, and oxygen. Both arteries and veins are important.
Undoubtedly, the influence on vascular tone of impulses from the brain and hormonal balance. Many factors can lead to vasoconstriction.
Clinical signs of pathology
Clinically, there are three degrees of retinal angiopathy - first, second (moderate) and third.
The degree of narrowing of the vessels of the fundus can only be determined during ophthalmoscopy.
In the initial stages of retinal vascular narrowing, the patient usually does not have complaints or has complaints that are general.
With slight narrowing of the retinal vessels (first degree angiopathy), patients may complain of:
- headache;
- discomfort in the eyeballs;
- visual disturbances (floaters, fog or spots before the eyes, slight decrease in visual acuity).
Changes in the fundus vessels in the first degree of angiopathy are reversible, as they are functional. Provided that effective treatment of the disease that caused angiopathy is prescribed in a timely manner, these changes can be easily regressed.
As angiopathy progresses, more specific signs appear, by which the clinician may suspect pathology of the fundus vessels:
- throbbing pain in the eyes;
- marked decrease in visual acuity, often myopia;
- narrowing or loss of visual fields;
- impaired light sensitivity.
But given the fact that the narrowing of retinal vessels is not an isolated pathology, the symptoms characteristic of the underlying disease, which caused the onset of angiopathy, come to the fore in the symptoms.
Ophthalmoscopy in the second degree of angiopathy reveals organic vascular lesions that are difficult to regress:
To clean VESSELS, prevent blood clots and get rid of CHOLESTEROL, our readers use a new natural drug recommended by Elena Malysheva. The preparation contains blueberry juice, clover flowers, native garlic concentrate, rock oil, and wild garlic juice.
- significant narrowing of the arteries;
- dilatation and tortuosity of veins;
- retinal hemorrhages;
- retinal vascular thrombosis;
- pallor of the fundus;
- newly formed vessels in the area of the optic nerve.
With adequate treatment of the underlying disease, it is possible to stabilize angiopathy and prevent its further progression.
The most severe (third) degree of angiopathy, which threatens the patient with loss of vision, is clinically manifested by the following symptoms:
- a sharp decrease in visual acuity;
- straightening the arteries;
- uneven caliber of arteries;
- cotton wool-like lesions;
- massive hemorrhages in the retina;
- swelling of the retina and optic nerve.
Depending on the causes of narrowing of the fundus vessels, the following types of retinal angiopathy are distinguished:
Hypertensive, which is based on an increase in blood pressure that occurs as a result of persistent spasm of the muscular component of the arterial walls;
Traumatic, which occurs with injuries to the cervical spine, neck or head. As a result of increased intracranial pressure, a reflex narrowing of the arterioles occurs, resulting in retinal hypoxia.
Conditions for the occurrence of narrowing of veins and arteries
The causes of vasoconstriction are very diverse. They depend on the type of vessel, external and internal factors, and the duration of their exposure.
External reasons
Arteries have a pronounced muscular layer, so they more often react with spasm to unfavorable factors. During spasm, small arteries narrow temporarily, but frequent repetition can lead to loss of the ability to relax and become stable.
Contributing factors are:
- smoking,
- stressful situations,
- alcohol consumption,
- hypothermia.
A similar external effect on the arteries is observed:
- with the development of vegetative-vascular dystonia;
- in the initial stages of hypertension and ischemic disease;
- with frostbite of the extremities;
- with Raynaud's syndrome.
Longer-term narrowing of arterial vessels from external factors is observed with mechanical compression:
- during severe injuries (long-term compartment syndrome);
- tumor growth near blood vessels;
- the pressing action of the bone tissue of the spinous processes of the spine;
- prolonged incorrect use of a tourniquet to stop bleeding (this is why first aid requires placing a note indicating the time of application).
Internal reasons
Internal causes of vasoconstriction include:
- atherosclerotic damage to the wall - between the middle and inner membranes of arteries of the muscular-elastic type, a low-density fraction of lipoproteins is deposited with the formation of plaques, over time they are supplemented with calcium salts, the lumen of the vessel loses its diameter;
- inflammatory changes (vasculitis, arteritis) - swelling of the walls reduces blood permeability;
- endarteritis - an unclear allergic reaction from the intima of the arteries of the legs and arms, leading to complete obliteration of the vessel;
- congenital pathology (aortic stenosis);
- thrombosis and embolism - play an important role in the development of pathology of the brain and heart;
- metabolic disorders in diabetes mellitus, thyrotoxicosis, obesity.
When do veins narrow?
The venous system is more prone to lose tone, but there is a pathology that leads to a persistent gradual loss of the diameter of the venous capillaries, and then the cessation of blood supply. We are talking about cirrhosis of the liver. All blood flowing from the tissues necessarily passes through this organ. With chronic inflammation of the lobules of liver cells (hepatocytes) and replacement of the interlobular space with scar tissue, the venules narrow. Then the blood flow through them completely stops. Problems arise in the area of the portal vein. Due to its sharp narrowing, hypertension and stagnation occur in the underlying sections, and overload of “excess” into the veins of the esophagus.
Thrombophlebitis (inflammation + thrombosis) cannot be excluded as a cause. In diseases that cause a decrease in blood flow velocity (stagnation), the process of parietal thrombus formation is activated. The spread of infection from chronic foci increases the narrowing of the affected area of the vein.
Symptoms of circulatory disorders due to altered vascular lumen depend on the specific location of the affected area. Let's look at the manifestations of the most significant diseases.
Clinical manifestations of impaired blood supply to the brain
Signs of cerebral insufficiency are caused by narrowing of the carotid and vertebral arteries, which carry blood to the brain.
For adults, the main importance is given to:
- atherosclerosis;
- cervical osteochondrosis;
- congenital pathology of vertebral vessels;
- hypertension;
- thromboembolic complications.
The disease can take a long-term chronic course or occur suddenly in the form of a stroke.
For the child, the most important are:
- mother's condition during pregnancy;
- birth injuries;
- previous vasculitis due to childhood infections;
- congenital pathology of the heart and blood vessels.
In acute cases, concern:
- severe headaches;
- dizziness to the point of loss of consciousness;
- noise in ears;
- impaired vision;
- decrease or disappearance of sensitivity and movements in the limbs;
- impaired speech.
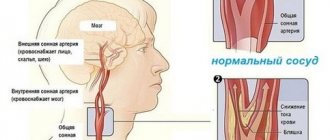
Clinical features for narrowing of arteries in the neck
Atherosclerosis of the carotid artery is considered the first manifestation of the disease. It is detected during Doppler sonography in individuals who do not yet have symptoms. Osteochondrosis affects the processes of the vertebrae in the cervicothoracic region, which compress the vertebral artery. The patient is concerned about:
- headaches in the temples, back of the head, forehead;
- feeling of "pressure";
- connection of well-being with turning and tilting the head to the side;
- dizziness, darkening of the eyes;
- possible loss of consciousness;
- nausea, vomiting.
Less often they complain of numbness of the tongue and hands.
What manifestations suggest a narrowing of the blood vessels of the heart?
The vessels of the heart or coronary arteries are very sensitive to factors contributing to spasm. And the local location of atherosclerotic plaques in them seriously changes the blood supply to the myocardium. “Oxygen starvation” manifests itself:
The pain is pressing or squeezing in nature, located behind the sternum or on the left, radiating to the left jaw, shoulder blade, arm, lasting up to 30 minutes.
With more intense and prolonged pain, severe weakness of the patient, and a feeling of arrhythmia, one should think about acute myocardial infarction. In this case, the narrowing of the vessel leads to an area of tissue necrosis.
What does narrowing of the fundus arteries indicate?
The fundus arteries undergo the same changes as others. They are considered a “mirror” of the state of cerebral circulation. The degree of narrowing is influenced by the following external and internal reasons:
- bad light;
- eye strain when working at a computer;
- watching TV for a long time;
- increased blood pressure.
The patient complains of:
- blurred vision;
- headache;
- throbbing pain in the eyeballs.
The ophthalmoscopy procedure allows the ophthalmologist to examine the arteries and veins of the fundus of the eye.
What causes vasoconstriction in the fundus?
Retinal angiopathy, as one of the ophthalmological symptoms, occurs in various diseases and pathological conditions of the human body:
- arterial hypertension;
- neurocirculatory dystonia;
- atherosclerosis;
- hemorrhagic stroke;
- diabetes mellitus;
- kidney diseases (chronic glomerulonephritis, nephropathy of pregnancy);
- traumatic injuries of the cervical spine, neck, head, eyes;
- cervical osteochondrosis;
- hydrocephalic syndrome;
- tumors inside the skull;
- thrombosis of the venous sinuses and cerebral veins;
- infectious diseases of the central nervous system;
- leukemia;
- congenital anomalies in the structure of vascular walls;
- autoimmune systemic diseases (periarteritis nodosa, multiple sclerosis, systemic lupus erythematosus);
- exposure to harmful production factors;
- long-term intoxication of the body (alcohol, drugs, salts of heavy metals, smoking).
These reasons often lead to irreversible changes in the blood vessels of the human body, including the vessels of the fundus.
Narrowing of the retinal arteries can also be reversible. The causes of reversible (reflex) constriction of the fundus vessels include:
- long-term stay in rooms with poor lighting;
- long hours of work at the computer;
- watching TV for a long time, especially with the lights off.
The narrowing of retinal vessels is based on different mechanisms:
- spasms - prolonged contraction of the muscle layer of the vascular walls;
- stenosis - a decrease in the lumen of blood vessels due to plaques present on their inner surface;
- sclerosis – thickening of vascular walls due to the replacement of their muscular elements with connective tissue;
- formation of granulomas or deposition of autoimmune complexes on vascular walls;
- mechanical compression of the arteries supplying the eye from the outside.
How to treat narrowed blood vessels
Treatment for vasoconstriction depends on the underlying causes. If there is a connection with external factors, their complete exclusion is necessary. Any temporary spasm carries the possibility of turning into permanent obstruction. Therefore, you should take the recommendations for regimen and diet seriously:
- stop sitting at night in front of the computer and TV;
- normalize sleep;
- pay more attention to active recreation, walks;
- learn to relieve stress;
- establish nutrition according to the requirements of an anti-atherosclerotic diet (do not indulge in coffee, spicy foods, fatty meat dishes, add enough fruits, vegetables, and dairy products to the diet);
- choose feasible exercises and do morning physical exercises.
You should treat your illness with medications only as prescribed by your doctor.
If necessary, the following are prescribed:
- cholesterol-lowering agents;
- antispasmodics;
- medications that stimulate collateral (auxiliary) blood circulation;
- drugs that strengthen the vascular wall;
- means to reduce tissue oxygen demand;
- vitamin complexes;
- physiotherapeutic supportive treatment.
Disturbed metabolic processes in tissues are treated with antioxidants and nootropics.
Depending on the severity of the patient’s condition and after determining the degree of narrowing of the afferent vessels, angiosurgeons choose surgical treatment. Methods include:
- replacement of a damaged vessel with an artificial analogue;
- bypass installation operation;
- removal of a blood clot from a large artery;
- installation of stents to expand the spasmodic area.
Folk remedies against angiopathy
In most cases, folk remedies are not only possible, but also should be used in the treatment of angiopathy. After all, if you look at it, even eye drops prescribed by doctors for illness are, to a certain extent, a nourishing solution. Folk remedies are a complete set of vitamins that help restore the normal functioning of the blood vessels of the eye.
There are quite a lot of different recipes offered by traditional healers. For our region, the most relevant of them are those that do not contain any exotic plants, although today you can probably buy everything you need in pharmacies. For example, we can cite a herbal tincture that includes chamomile, St. John's wort, birch buds, immortelle and yarrow. All ingredients are taken one hundred grams each and mixed. After this, the herbs are placed in a jar, from which one tablespoon is taken every morning and poured with boiling water (0.5 liters). After infusion for twenty minutes, the infusion is filtered and drunk one glass in the morning and after dinner.
Using traditional medicine, eye drops and other drugs prescribed by a doctor, it is often possible to bring the vessels of the fundus to a normal state, but you should be aware that treatment can last quite a long time.
Is it possible to be treated with traditional methods?
You cannot straighten a narrowed vessel with folk remedies. You should not collect and test on yourself numerous “tips” for cleaning and getting rid of atherosclerosis.
Using a combination of garlic, lemon and honey is more of a dietary recommendation. It has a good effect on the immune system, so it is always useful. The product will help in the recovery period after stress, injury or infection. But it is impossible to “dissolve plaques” at the current level.
Medicines will help delay further narrowing. People's advice can be tried against the background of their application.
Treatment methods
To treat patients with narrowed vessels in the eyes, the following methods of conservative therapy are used:
- Use of medications. Microcirculation correctors (Solcoseryl, Cavinton) help restore blood supply to the retina. The permeability of vascular walls is reduced by drugs based on extracts of ginkgo biloba, diosmin and hesperidin (Detralex, Phlebodia, Ginkor forte). In case of increased blood clotting, antiplatelet agents (Lospirin) are prescribed. To eliminate the underlying disease, hypoglycemic and antihypertensive drugs are used. The use of drops that normalize blood circulation (Taufon, Emoksipina) helps improve vision.
- Physiotherapeutic procedures. Vascular spasm is relieved through laser exposure, acupuncture, magnetic therapy and massage of the cervical region.
- Folk remedies. It is recommended to treat mild retinopathy with infusions of hawthorn, chamomile or lemon balm. 20 g of raw material is poured into a glass of water and left for 3 hours. Take 50 ml infusion 3 times a day.
If conservative therapy is ineffective and the disease develops rapidly, surgical interventions are used - laser coagulation of the retina, photocoagulation, removal of the vitreous.
Forecast
It is always necessary to remember that any narrowing of blood vessels activates the blood coagulation system and slows down the speed of blood flow. The clinical course of the disease worsens, which leads to extreme consequences (stroke, heart attack with acute heart failure, blindness, gangrene of the legs).
Treatment and prevention must be carried out constantly. This is especially true for people suffering from chronic diseases with initial symptoms in the form of spasms.
Diseases of the circulatory system are displayed on the vessels of the fundus.
Diagnostic methods allow for visual examination of veins and arteries and a detailed assessment of the patient’s condition.
Constriction of the fundus vessels does not occur independently. The disorder always occurs with the development of general somatic pathologies.
Non-surgical eye treatment in 1 month.
Symptoms of retinal angiopathy
Vascular angiopathy is divided into types depending on the underlying disease:
Diabetic angiopathy. The most common. In patients with type 1 diabetes, it is observed in 40% of cases, in patients with type 2 – in 20%. Typically, angiopathy begins to develop 7-10 years from the onset of the disease. There are two possible development options: microangiopathy and macroangiopathy. With microangiopathy, capillaries are affected and thinned, which leads to impaired microcirculation and hemorrhages. With macroangiopathy, larger vessels are affected, occlusions (blockage) occur, which leads to retinal hypoxia;
Hypertensive angiopathy. Against the background of chronically high blood pressure, the retinal arteries narrow and the veins dilate. Vascular sclerosis gradually forms, the venous bed becomes branched, exudates are formed due to blood leakage through the walls of the capillaries;
Hypotonic angiopathy. Against the background of arterial hypotension, on the contrary, the arteries dilate, the blood flow slows down, the veins pulsate, the vessels become tortuous, which increases the likelihood of blood clots. Characteristic symptoms in this case are a feeling of pulsation in the eyes and dizziness;
Traumatic angiopathy. With injuries to the head or chest, compression of the abdomen, or osteochondrosis, intraocular pressure can sharply increase. If the vessels cannot withstand the load, then they rupture with subsequent hemorrhages;
Angiopathy during pregnancy. In this case, angiopathy is functional in nature and goes away on its own 2-3 months after birth. This is explained by the fact that an increase in the volume of circulating blood causes passive dilation of the retinal vessels. Another question is if diabetic or hypertensive angiopathy was present before pregnancy. In this case, it is likely to begin to progress quickly.
The danger of angiopathy is that in the early stages and for quite a long time it is asymptomatic. At the stage of noticeable deterioration of vision, the process is usually irreversible.
General symptoms of angiopathy:
Decreased visual acuity;
The appearance of fog and spots before the eyes;
Narrowing of the field of view;
Feeling of pulsation in the eyeball;
The presence of burst vessels and yellow spots on the conjunctiva.
Diseases of the circulatory system are displayed on the vessels of the fundus.
Diagnostic methods allow for visual examination of veins and arteries and a detailed assessment of the patient’s condition.
Causes
Factors influencing vasoconstriction:
- hypertension;
- diabetes;
- genetic structural abnormalities;
- lowering blood pressure;
- toxins in the body;
- elderly age;
- smoking, alcohol abuse;
- poor quality of sleep, fatigue;
- increased intracranial pressure;
- insufficiently active lifestyle.
Vasoconstriction occurs as a result of the development of the disease. The blood stagnates, many blood clots appear, and retinal tissue ischemia develops. At the same time, the veins dilate, the tissues of the eye swell due to the large accumulation of blood. The tone of blood vessels deteriorates due to frequent changes in pressure, they burst, hemorrhage occurs, and the quality of vision deteriorates.
Causes of angiopathy
Common causes of angiopathy include:
- Hypertension. This pathology leaves its mark on the vessels of the entire body, including the fundus. They narrow, so blood cannot circulate smoothly. Subsequently, part of the vessel is destroyed, this is clearly visible during examination. The sooner you contact an ophthalmologist, the better. In some cases, the unpleasant consequences of this disease can be avoided.
- Diabetes. An increased concentration of glucose in the blood provokes vascular obstruction. In the absence of treatment measures, the patient may lose his vision.
- Severe injuries to the spine or head. With such injuries, the pressure inside the skull increases greatly, so specialists carefully check the fundus.
Doctors include smoking, uncontrolled alcohol consumption, and age as secondary reasons. There are a number of other reasons that do not depend on the influence of extraneous factors.
These include:
- Eales disease or angiopathy in adolescence. Until now, scientists have not come to a consensus about the causes of this type of disease. But the symptoms and consequences are known. Multiple hemorrhages occur on the retina, which can lead to its detachment. Subsequently, glaucoma, cataracts, or complete loss of vision develop.
- Retinal vasoconstriction in infants. This disease is very rare. It can be triggered by difficult childbirth or injuries received during it. Also, angiopathy was often detected in premature infants.
- Retinal angiopathy during pregnancy occurs if the expectant mother has hypertension. Since doctors monitor every change in a woman’s body, there is no need to be afraid. Early detection of pathology will allow you to get rid of the problem as soon as possible.
Taking into account all of these factors, we can judge that angiopathy occurs due to some effect on the blood vessels. To prevent the occurrence of such a retinal disease, you should attend routine examinations on time.
Risk group
The category of people most prone to disorders:
- pregnant women;
- diabetics;
- patients with moderate and complex myopia.
The disorder occurs more often in hypertensive patients. Retinal angiopathy develops as a result of circulatory disorders.
- hypertensive;
- diabetic;
- youthful;
- traumatic.
The hypertensive form is accompanied by dilation of blood vessels and an increase in branches. Often people have a feeling of pulsation, the fundus of the eye is covered with dilated vessels. Cloudiness occurs in several places if the pathology becomes more complex.
Macroangiopathy or microangiopathy develops in diabetics. The walls of small or large vessels are affected.
Juvenile angiopathy is expressed by inflammation of the veins, hemorrhage occurs in the retina or vitreous body. Sometimes detachment occurs or glaucoma develops.
Traumatic angiopathy appears after severe compression of the chest. The pressure in the blood vessels increases, and hemorrhages appear in the area of the retina and nerve tissue.
Methods for treating vasoconstriction in the fundus
Due to the fact that retinopathy is most often of the nature of a systemic disease, their treatment consists of etiotropic therapy of the underlying disease. Vitamin preparations, angioprotectors, tissue preparations (vitreous body, aloe) are prescribed.
In degenerative processes, vasodilators (No-Shpa, Papaverine), which are administered endonasally using electrophoresis, have some effect. Recently, laser coagulation has been used to treat retinodystrophies, which, unfortunately, also gives a temporary effect.
The basis of effective therapy is the timely detection of initial changes in the retina, therefore it is recommended to undergo ophthalmoscopy at least once a year.
It is advisable for people suffering from existing pathologies to be examined at least once every six months.
Symptoms
- scotomas form in the field of view;
- a veil appears before the eyes;
- visual acuity decreases;
- horizons narrow;
- throbbing pain occurs;
- hemorrhage occurs;
- migraine;
- dizzy;
- blood clots form more often.
The disease, which is inherited, manifests itself in early childhood. Narrowed and excessively tortuous vessels are detected after ophthalmoscopy. The doctor identifies areas of expansion and areas of the macula that are filled with blood.
We offer a discount to readers of our site!
Diagnostics
Places of development of ischemia and hemorrhage are identified during examination.
- blood analysis;
- MRI;
- angiography.
Ultrasound diagnostics reveals blood clots and areas of vascular blockage.
Letters from our readers
I have had vision problems since childhood; I wore glasses at school, but at university I switched to contact lenses.
I accidentally came across a doctor’s answer about vision treatment without surgery. I decided to try it, left a request, they gave me a free consultation over the phone, answered all my questions, and told me how to completely restore my vision in my case.
I was skeptical about this treatment, but after a while I began to notice that I could see worse with lenses than without them. I even began to perceive the pattern on the wallpaper in the room differently. Vision was restored, if not 100%, then definitely at least 90%. I'm sending a link to the site
- Indirect is carried out using a magnifying glass and a mirror device. The fundus is examined through magnified reflection.
- Direct examination is performed using an electric ophthalmoscope. This analysis provides more useful information.
- Ophthalmochromoscopy is carried out using equipment with replaceable filters. Colored lenses in different combinations reveal changes in the arteries at an early stage, which are difficult to detect with natural color.
- Polarization allows you to diagnose retinal edema at the first stage.
The results of ophthalmoscopy are clarified by additional examinations:
- Biomicroscopy is performed using a slit lamp and a fundus lens. A device with 3 mirrors is installed on the cornea for a detailed examination of the retina.
- An ultrasound machine is applied to the closed eyelid if the patient has no contraindications to such a procedure. The condition of the retinal vessels is studied and the speed of blood flow is measured. Ultrasound allows you to determine minimal vasoconstriction.
- Laser ophthalmoscopy, in which the retina is illuminated with optical rays, the refractive characteristics of which are displayed on the monitor. The technique allows you to study the condition of the fundus of the eye when the lens is clouded.
- Rheoophthalmography is a contact method for examining the blood supply system, in which pulse waves of the arteries are detected. A lens with electrodes is placed on the cornea to sense impulses.
- Fluorescein angiography is based on photographing blood vessels after administration of a contrast agent. Diagnosis is carried out using a slit lamp with fundus lenses.
- Densitometry is photography performed after the administration of a contrast agent.
These diagnostic methods complement information about the patient’s condition, but do not replace each other. The ophthalmologist independently chooses examination methods, taking into account the possibilities of the examination.
How to detect pathology?
It is impossible to detect retinal angiopathy with the naked eye. This requires special equipment - ophthalmoscopes, slit lamps, ultrasound machines.
Ophthalmoscopy
An ophthalmoscopy allows the ophthalmologist to examine the arteries and veins of the fundus through the pupil. The most common methods of examining the retina include:
- Indirect ophthalmoscopy (mirror). This procedure is performed using a mirror ophthalmoscope and a magnifying glass. The fundus image is presented as a mirror image and provides only an overview.
- Direct ophthalmoscopy. Examination of the fundus is carried out using an electric ophthalmoscope. This procedure is more informative compared to the mirror procedure.
- Ophthalmochromoscopy. Examination of the fundus with an ophthalmoscope with replaceable filters. The use of colored glasses (red, green and blue) in different combinations during the procedure makes it possible to identify initial changes in the retinal vessels that remain invisible in white.
- Polarizing ophthalmoscopy. Examination of the fundus in polarized light makes it possible to detect retinal edema in the initial stage.
Clarifying research methods
In modern medicine, many other methods of studying retinal vessels are used to clarify the results of ophthalmoscopy:
- Biomicroscopy of the fundus using a slit lamp with fundus lenses. This is a contact method for examining the fundus, in which a three-mirror lens is placed on the cornea, allowing a detailed examination of the entire surface of the retina.
- Doppler ultrasound examination of the eyes. It is carried out through a closed eyelid and has no contraindications. Allows you to study the vessels of the retina and evaluate the speed of blood flow through them. Determines the narrowing of the fundus vessels in the initial stages.
- Laser ophthalmoscopy. With this research method, the retina is illuminated with a laser, and an image of the retina is displayed on a monitor. The advantage of this method is the ability to examine the fundus of the eye while reducing the transparency of the lens and vitreous body.
- Rheoophthalmography. This is a contact method for studying the blood supply to the retina, based on recording pulse waves from the vessels of the fundus. To capture impulses from them, electrode lenses are applied to the cornea.
- Fluorescein angiography of the fundus. This is a highly informative method based on photographing contrasted vessels of the fundus. The contrast agent is administered intravenously. The procedure is performed using a slit lamp with fundus lenses.
- Densitometry. The procedure is performed similarly to fluorescein angiography, but photographs of the retina are taken, which allows one to evaluate the blood flow in it over time.
These methods do not replace each other, but complement each other perfectly. The choice of diagnostic procedure in most cases depends on the doctor’s preferences, territorial and financial accessibility of the diagnostic method, and the transparency of the eye structures.
Narrowing of the fundus vessels can lead to blindness of the patient, so it is very important to identify the pathology in time, establish the causes of its occurrence and prescribe appropriate treatment.
The preservation of the functions of such an important human sensory organ as the eye depends on this.