Considering the nature and intensity of expression, lymphangitis, the treatment of which is a long process, is divided into serous (or simple) and purulent. Considering the depth of location, superficial and deep lymphangitis are distinguished.
Varieties
Lymphangitis has two forms - reticular (mesh) and truncular lymphangitis. With reticular lymphangitis, a large number of superficial lymphatic capillaries are involved in the inflammatory process. Inflammation of the lymphatic vessels (one or more) is observed with truncular lymphangitis.
According to the clinical course of the disease, acute and chronic lymphangitis are distinguished.
Cause or effect?
Lymphangitis, like other diseases associated with infectious lesions of the lymphatic system, can hardly be classified as independent diagnoses.
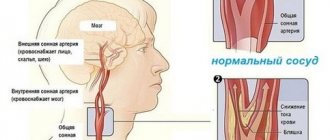
The fact is that the lymphatic system itself is an auxiliary vascular structure, the main purpose of which is to protect the body during attacks of all kinds of infections.
This protection involves the supply of lymph into the venous bed, blood purification, the production of lymphoid elements involved in immune reactions, and the creation of barriers to infections.
Normally, lymphatic vessels independently cope with pathogens. However, severe infection and decreased immunity sometimes cause the lymphatic system to lose its barrier function. As a result, its vessels, tissues and nodes themselves become inflamed: this is how lymphangitis develops, affecting the vascular bed, as well as acute and chronic lymphadenitis, affecting regional lymph nodes.
Thus, the above pathologies always develop against the background of some other inflammatory processes and are secondary in nature: complete cure of the underlying disease automatically returns the condition of the lymphatic system to normal.
Why does lymphangitis develop?
Lymphangitis is an infectious lesion of the walls of deep and superficial lymphatic vessels, the cause of which is most often the intervention of Staphylococcus aureus - a formidable bacterium that constantly mutates and causes many serious diseases of the skin, lungs, heart, and joints.
Colonies of Staphylococcus aureus live on the skin without causing harm to humans, but if the integrity of its integument is damaged through cuts or abrasions, they penetrate into the blood and are carried by current throughout all organs and systems.
However, in some cases, the activity of the infection is not sufficiently suppressed by the body due to the amazing ability of staphylococcus to adapt to the most unfavorable conditions for it and a temporary weakening of the immune system.
The entry points for infection are wounds, abrasions, ingrown nails, boils - in general, any foci in which suppuration develops.
Why is lymphangitis dangerous?
Long-term lymphangitis can lead to:
- lymph circulation disorder (the qualitative composition of lymph changes, its quantity increases significantly);
- obliteration of lymphatic vessels (the lumen of the vessel becomes overgrown);
- development of elephantiasis (skin and subcutaneous tissue thicken due to chronic inflammation of the lymphatic vessels), lymphostasis (tissue swelling resulting from impaired lymph outflow);
- abscess (purulent inflammation of tissues with their melting, which leads to the formation of a purulent cavity);
- sepsis (a systemic inflammatory reaction diagnosed as a result of infectious agents entering the blood);
- cellulite (changes in the structure of the subcutaneous fat layer, which lead to disturbances in lymphatic outflow and lymph circulation).
How does it manifest itself?
The mesh (superficial) form resembles ordinary inflammation: around the wound there is redness and swelling of the skin without clear boundaries, but the vascular mesh in the infected area suggests to the doctor that lymphangitis has begun.
Deep lymphangitis is characterized by red, painful streaks running from the infected wound to nearby lymph nodes. In addition to these symptoms, patients complain of pain when pressing along the vessels, and the specialist pays attention to seals.
The deeper the lymphatic vessels are affected, the less likely the appearance of red streaks: the clinical picture here is pain and swelling of the extremities.
If lymphangitis develops in the legs, then elephantiasis (elephantiasis) may appear.
Perilymphangitis has rather sparse symptoms: they are limited only to subcutaneous compactions along the vessels.
The rapidly developing inflammatory process during lymphangitis can be accompanied by a significant increase in temperature (sometimes even up to 39 degrees), profuse sweating and weakness.
Lymphangitis (inflammation of the lymphatic vessels): how it develops, symptoms, how to treat
© Andrey Alekseevich Illarionov, therapist, bacteriologist, especially for SosudInfo.ru (about the authors)
Lymphangitis is a disease of the lymphatic system, caused by inflammation of vessels of various sizes and complicating the course of a number of pathologies. Lymphangitis is usually accompanied by regional lymphadenitis.
Most often, the vessels of the upper and lower extremities are affected, which is associated with their trauma and the presence of a large number of microbes on the skin. Bacterial toxins and cell breakdown products are absorbed into the blood and penetrate the lymphatic vessels, which leads to their inflammation.
Clinical signs of the disease are skin hyperemia, pain and swelling along the inflamed vessels, regional lymphadenitis, fever, chills and weakness.
To cure lymphangitis, specialists carry out sanitation of existing foci of infection in the patient’s body, antibiotic therapy, and open abscesses and phlegmons.
To get rid of lymphangitis, it is necessary to cure the underlying disease.
The severity of clinical symptoms is determined by the caliber of the inflamed vessels: when large, deep-lying vessels are affected, stem lymphangitis develops, and when small capillaries are inflamed, mesh lymphangitis develops.
In the first case, hyperemia without clear boundaries appears around the boil or purulent wound, and in the second, narrow red stripes appear that go from the source of infection to the regional lymph nodes and along which a painful compaction in the form of a cord can be felt.
Symptoms
Acute lymphangitis is characterized by severe intoxication and local manifestations.
General symptoms of pathology:
- Fever,
- Chilling,
- Deterioration in general health,
- Increased sweating
- brokenness,
- Tongue coated
- Leukocytosis in the blood.
Manifestations of lymphangitis
Local signs of the disease:
- Hyperemia and swelling around the lesion without clear boundaries,
- The skin in the affected area is hot to the touch,
- Vascular network in the infected area,
- "Marbled" erythema,
- Linear redness of an uneven shape,
- Inflammation of surrounding tissues
- Dryness and roughness of the skin,
- Enlarged, hardened and painful lymph nodes,
- Bursting pain in the affected area,
- Painful palpation along the vessels,
- Swelling and throbbing pain in the limb,
- Limitation of movement in a limb due to pain.
Chronic lymphangitis is a continuation of the acute form of the disease and is characterized by pronounced proliferation, proliferation of connective tissue fibers, vascular spasm, slowing of lymph flow and its stagnation, swelling of the limb, development of elephantiasis and organ dysfunction.
The purulent form of the disease is the most severe. Lymphangitis develops quickly after injuries or septic operations. The following conditions aggravate the course of the pathology: diabetes mellitus, alcoholism, chronic starvation, cachexia.
Carcinomatous or cancerous lymphangitis is a type of chronic lymphangitis that develops in people with lung or breast cancer.
Regional lymphadenitis is a local complication of lymphangitis. Microbes from the lesion penetrate through the vessels into the lymph nodes. Inflammation of the lymph nodes is manifested by their enlargement and pain against the background of intoxication syndrome. The purulent-inflammatory process spreads to one or more adjacent lymph nodes.
The largest lymph nodes affected by regional lymphadenitis
In men, the lymphatic vessels of the penis often become inflamed. Non-venereal lymphangitis develops as a result of regular masturbation or after traumatic injury to the penis.
Abrasions and cracks appear on the skin, which are entry points for infection. In this case, the lymphatic vessels located along the shaft of the penis become inflamed. This area becomes swollen, hard and painful.
Lymphangitis of the penis lasts several days or hours and goes away on its own.
Complications of lymphangitis are: lymphodema - a pathology characterized by swelling of soft tissues and impaired lymph flow, early lymphadenitis, perilymphangitis, pachydermia, thrombophlebitis, elephantiasis, multiple abscesses, subcutaneous phlegmon, sepsis.
Epizootic lymphangitis is classified into a special group. This is an infectious disease of horses, characterized by granulomatous inflammation of the lymphatic vessels. Infection occurs through microtraumas of the skin when sick and healthy animals are kept together.
When inflammation affects the lymph nodes
Since the inflammatory process is always localized near the lymph nodes, there is a possibility of their infection. In such cases, signs of lymphadenitis appear - inflammation in the neck and in other places - in the armpits, in the groin.
This is regional lymphadenitis - a complication that is local in nature.
Its symptoms are characterized by enlarged and painful lymph nodes, very high fever, weakness and sweating.
For example, inflammation of the nodes in the groin is observed during attacks of sexually transmitted infections (syphilis, chlamydia, trichomoniasis, gonorrhea and others), as well as during tuberculosis and tularemia.
A boil on the leg can also cause infection of the inguinal lymph nodes and the development of inguinal lymphadenitis - a very painful and severe complication.
A purely male problem
Despite the fact that inflammation of small and large lymphatic vessels most often manifests itself on the extremities, sometimes men who have a very active sex life face this problem.
They develop non-venereal lymphangitis - a consequence of stagnation of lymph in the penis, which occurs with frequent masturbation or prolonged sexual intercourse.
Scuffs and abrasions form on the skin and mucous membranes of the penis, through which the infection easily penetrates into the lymphatic vessels located next to the coronary sulcus or along the entire length of the organ.
The inflamed area looks like a painful swelling, which disappears quite quickly and does not require special treatment.
However, the supposed non-venereal lymphangitis may ultimately turn out to be a completely venereal disease: the clinical picture of some STDs has a certain similarity with the course of inflammation of the lymphatic vessels of a non-venereal nature.
For this reason, patients are usually referred for consultation to a venereologist to rule out:
- Primary syphilis;
- Genital herpes;
- Chlamydial and gonococcal urethritis.
There is one more pathology that should also be excluded during the examination: Mondor's disease (thrombophlebitis of the superficial veins of the penis).
The examination is absolutely necessary, since all of the above diseases require treatment - conservative or surgical.
How to recover?
It has already been mentioned that lymphangitis is not an independent disease, but a complication of inflammatory purulent processes on the skin or mucous membranes.
Treatment of lymphangitis should be carried out only by a specialist, ideally in a hospital department. The fact is that suppuration on the skin most often represents a bag with purulent contents, inaccessible to antibiotics.
Therefore, they are opened to remove the pus, and the opening site is treated. Only a qualified surgeon can do this, which is why you should always go to the hospital with such problems.
What you should absolutely not do if you have an abscess at the site of inflammation:
- Apply ointments;
- Warm up the sore spot using home methods.
Typically, the course of treatment includes therapy with antibiotics and anti-inflammatory drugs, selected in accordance with the identified pathogen, as well as physiotherapeutic procedures - for example, UHF hardware heating, laser procedures.
Antibiotics used to treat lymphangitis usually belong to the class of penicillins, first-generation cephalosporins. Drugs from aminoglycosides or lincosamides can also be prescribed, but the choice is made only by a specialist: self-treatment with antibiotics is unacceptable.
Chronic inflammatory processes in the lymphatic vessels are treated with physiotherapy using ultraviolet irradiation, mud therapy, and applying ointment and semi-alcohol dressings to the affected area.
What can happen without treatment
If you rely only on home methods or do not pay attention to the problem at all, untreated or improperly treated lymphangitis quickly becomes chronic, leading to persistent impairment of lymph circulation, narrowing of lymphatic vessels, and early development of severe diseases of the lymphatic system - lymphostasis and elephantism.
Causes of lymphangitis
Lymphangitis develops secondarily, against the background of an existing superficial or deep purulent-inflammatory focus - an infected abrasion or wound, boil, abscess, carbuncle, phlegmon. The main pathogens in lymphangitis are Staphylococcus aureus, beta-hemolytic streptococcus, less often Escherichia coli and Proteus, as well as other aerobic flora in the form of a monoculture or in associations. Specific lymphangitis is more often associated with the presence of tuberculosis in the patient.
The likelihood of developing lymphangitis depends on the location, size of the primary infectious focus, virulence of the microflora, and characteristics of lymph circulation in a given anatomical zone.
Microbial agents and their toxins enter from the source of inflammation into the interstitial space, then into the lymphatic capillaries, moving along them in the direction of the lymph flow to larger vessels and lymph nodes. Reactive inflammation of the vascular wall is expressed in swelling of the endothelium, increased permeability, development of exudation, loss of fibrin clots, and intravascular thrombus formation. These changes lead to disorders of local lymph circulation - lymphostasis. With further progression of inflammation, purulent lymphangitis and purulent melting of blood clots may develop.
If inflammation spreads to surrounding tissues, perilymphangitis develops, which can affect blood vessels, joints, muscles, etc. Ascending inflammation can spread to the thoracic lymphatic duct. In clinical practice, lymphangitis of the lower extremities is more often diagnosed, which occurs as a result of abrasions, microtraumas, scratching, trophic ulcers, felons.
In andrology, there is sometimes a condition regarded as non-venereal lymphangitis of the penis: its causes may be injury to the tissues of the penis during frequent masturbation and prolonged sexual intercourse. Specific venereal lymphangitis can develop with primary syphilis, genital herpes, and urethritis caused by sexually transmitted infections.
Causes of occurrence and mechanism of development
Lymphangitis can be a complication of an infected wound.
Almost always, lymphangitis is a secondary disease that does not develop independently, but against the background of some source of inflammation. This focus can be located on the surface of the skin or deep in the tissue and can be an infected wound, abrasion, abscess, boil or carbuncle, or phlegmon. This disease is a sign of progression of the primary pathological process, which complicates its course.
The leading cause of lymphangitis is opportunistic and pathogenic bacteria, in particular beta-hemolytic streptococcus, aureus and other types of staphylococcus, Proteus, Escherichia coli, and aerobic bacteria. Sometimes lymphangitis occurs against the background of tuberculosis - mycobacteria become the etiological factor in this case. In many cases, the pathological process is caused not by one, but by several bacteria at once.
Bacteria from the infectious focus enter the interstitial space, and from there into the lymphocapillaries. In the vessels they move along with the lymph, spreading into larger vessels and lymph nodes. In lymphatic vessels, bacteria and their toxins provoke inflammation of the cells lining them from the inside - the endothelium: the wall swells, the permeability of the cells increases, they produce a large amount of inflammatory fluid - exudate, microthrombi form inside the blood vessels. The consequence of all these processes is stagnation of lymph in the vessels - lymphostasis and purulent lymphangitis.
In the absence of timely treatment, the tissues surrounding the inflamed lymphatic vessel are involved in the pathological process - inflammatory changes develop in them, which are called “perilymphangitis”. The process also spreads along the course of the lymphatic vessel itself up to the thoracic lymphatic duct, affecting the lymph nodes encountered along the way (lymphadenitis develops).
In most cases, lymphangitis affects the vessels of the extremities, which is associated with frequent injuries and microtraumas of these parts of the body, a wide variety of microorganisms in this area, as well as the characteristics of the lymphatic system.
Sometimes urologists or andrologists encounter lymphangitis in their patients. The disease in this case affects the lymphatic vessels of the penis and may be non-venereal (develop as a result of microtraumatization of tissue during masturbation or sexual intercourse) and venereal (with genital herpes, syphilis, and other sexually transmitted diseases) nature.
Classification of lymphangitis
Taking into account the nature and severity of inflammation, lymphangitis can be serous (simple) and purulent; according to the clinical course - acute or chronic; according to the depth of location of the affected vessels - superficial or deep.
Depending on the caliber of the inflamed lymphatic vessels, lymphangitis is divided into capillary (reticular or reticular) and stem (truncular). With reticular lymphangitis, many superficial lymphatic capillaries are involved in inflammation; with the stem - one or more large vessels become inflamed.
Forms of lymphangitis
Modern medicine uses several etiological classifications of the disease. Based on which vessels are involved in the inflammation process, the following forms are distinguished:
- Reticular lymphangitis (or reticular). This form is characterized by damage to a large number of small vessels located in the near-surface zone of the skin. Therefore, during inflammation, the patient observes a peculiar pattern on the skin in the form of a red mesh.
- Stem (or truncular). In this case, the disease spreads to one or more large vessels, which are also called stem vessels.
It is also classified according to the severity of the pathological inflammatory reaction:
- Acute lymphangitis. It is characterized by pronounced and painful symptoms. It appears suddenly.
- Chronic lymphangitis. In most cases, it is asymptomatic and causes inconvenience to a person only during periodic exacerbations.
The disease is also divided into the following types:
- Venereal lymphangitis. The causes of venereal lymphangitis are infections transmitted from a sick partner to a healthy one during intimate contact. Symptoms affect exclusively the organs of the genitourinary system.
- Non-venereal form of the disease. Develops as a result of stagnant processes in the tissues of the male genital organ. It has a second name – lymphostasis of the penis. Also associated with mechanical injuries to tissues and skin.
- Carcinomatous lymphangitis. Occurs against the background of breast cancer in women or lung cancer in patients of both sexes.
- Lymphangitis of cancer etiology is a complication of malignant neoplasms in lung tissue.
Depending on the complexity and nature of the inflammation, it varies:
- Serous lymphangitis. Manifested by the presence of blood clots that do not develop over time.
- Purulent inflammatory process. It has a pronounced clinical picture. It is always preceded by the appearance of purulent foci in the body.
There is a classification depending on the depth of spread of the inflammatory process. If a capillary adjacent to the surface of the dermis is inflamed, this indicates the presence of superficial lymphangitis. Deep lymphangitis affects only internal vessels.
Symptoms of lymphangitis
With lymphangitis, general intoxication is always significantly pronounced, accompanying a severe purulent-inflammatory process. There is a high temperature (up to 39-40°C), chills, sweating, weakness, and headache. Reticular lymphangitis begins with the appearance of pronounced superficial hyperemia around the source of infection (wound, abscess, etc.) with an enhanced mesh (marble) pattern against the background of intense erythema. According to the clinical picture, reticular lymphangitis resembles erysipelas, however, the hyperemia has vague boundaries, uncharacteristic of erysipelas.
A local manifestation of stem lymphangitis is the presence of narrow red stripes on the skin along the inflamed lymphatic vessels, reaching to the regional lymph nodes. Swelling, thickening and soreness of the cords, swelling and tension of the surrounding tissues, and regional lymphadenitis quickly develop. Palpation along the vessels reveals painful seals like a cord or rosary.
With deep lymphangitis, local hyperemia is not observed, but swelling and pain in the limb quickly increases; with deep palpation, sharp pain is noted, lymphedema develops early. In the case of perilymphangitis, areas of inflamed surrounding tissue can transform into an abscess or subfascial phlegmon, untimely opening of which can lead to the development of sepsis.
The symptoms of chronic lymphangitis are erased and are usually characterized by persistent swelling due to blockage of deep lymphatic trunks and lymphostasis. With non-venereal lymphangitis, a painless, compacted cord appears along the shaft or coronary sulcus of the penis, which can persist for several hours or days, after which it disappears spontaneously.
Lymphangitis - causes, symptoms, prevention in Nizhny Novgorod
Lymphangitis is an inflammation of the capillaries and lymphatic trunks, which develops against the background of purulent-inflammatory processes. The disease is accompanied by swelling, pain and hyperemia along the inflamed lymphatic vessels, weakness, and increased body temperature.
Pathology can affect vessels of different locations and sizes. Most often in their practice, phlebologists and lymphologists encounter lymphangitis of the lower extremities. This is explained by the nature of local lymph circulation, frequent microtrauma and the presence of a fairly large number of microbial pathogens.
Slightly less frequently diagnosed:
- lymphangitis of the lungs;
- non-venereal lymphangitis of the penis;
- specific venereal lymphangitis;
- lymphangitis of the mammary gland, etc.
The disease is characterized by symptoms of secondary lymphadenitis.
Forms of lymphangitis
Based on the nature and severity of the developed inflammatory process, the following are distinguished:
- serous, or simple, lymphangitis;
- purulent lymphangitis.
According to the depth of the vessels:
According to the clinical course, it happens:
- acute lymphangitis;
- chronic lymphangitis.
Taking into account the caliber of inflamed lymphatic vessels, the disease is classified into:
- capillary (mesh, reticular) – the surfaces of a large number of lymphatic capillaries are involved in the inflammatory process,
- stem (truncular) – one or more large lymphatic vessels are inflamed.
Causes of lymphangitis
Lymphangitis is a secondary infection. It always occurs due to the patient’s existing superficial or deep purulent-inflammatory foci. This refers to boils, carbuncles, abscesses, wounds, phlegmon.
Among the main pathogens:
- beta-hemolytic streptococcus;
- Staphylococcus aureus;
- Proteus;
- coli;
- other aerobic flora in associations or as a monoculture.
Specific lymphangitis is caused by tuberculosis.
The causes of lymphangitis of the lower extremities are:
- microtraumas;
- abrasions;
- trophic ulcers;
- scratching;
- panaritiums.
Non-venereal lymphangitis of the penis is a consequence of trauma to the tissues of the organ during prolonged sexual intercourse and frequent masturbation.
Specific venereal lymphangitis develops as a result of diseases caused by sexually transmitted infections:
- genital herpes;
- primary syphilis;
- urethritis.
Pathogenesis
The risk of developing an inflammatory process depends on:
- location and size of the primary infectious focus;
- features of lymph circulation in the anatomical zone;
- virulence of microflora.
Microbial agents, together with toxins, enter the interstitial space from the source of inflammation. Afterwards they penetrate the lymphatic capillaries and, together with the lymph flow, move to large lymph nodes and vessels.
Signs of reactive inflammation of the vascular wall are:
- endothelial swelling;
- increased permeability;
- loss of fibrin clots;
- development of exudation;
- formation of blood clots inside blood vessels.
These processes cause a disorder of local lymph circulation (lymphostasis). In the absence of proper treatment, the disease may progress to a purulent form.
If inflammation spreads to surrounding tissues, the doctor diagnoses perilymphangitis, which leads to damage to joints, blood vessels, and muscles. Together with the blood flow, the pathological process can spread all the way to the thoracic lymphatic duct.
Symptoms of lymphangitis
Common symptoms of lymphangitis include:
- intoxication accompanying the inflammatory (purulent) process;
- high body temperature (39-40°C);
- chills;
- hyperhidrosis;
- headache;
- weakness.
Reticular ( capillary ) lymphangitis always begins with superficial hyperemia around the infectious focus (wound), an increase in the mesh pattern against the background of erythema. According to clinical signs, this form of the disease resembles erysipelas. The main difference is that hyperemia has vague boundaries, which is not observed with erysipelas.
Stem lymphangitis is characterized by red stripes on the skin along the inflamed lymphatic vessels leading to the regional lymph nodes. At the same time, swelling develops, edema forms, and dense and painful to the touch cords appear.
In the case of a deep form, hyperemia does not occur, but edema increases very quickly, and lymphedema develops almost immediately. With perilymphangitis, the tissue surrounding the inflamed area can transform into an abscess or subfascial phlegmon. Untimely opening of the lesion is fraught with sepsis.
Chronic lymphangitis does not have acute symptoms and is characterized only by the presence of persistent edema, the formation of which is caused by blockage of deep lymphatic trunks. Non-venereal lymphangitis of the penis is manifested by the appearance of a compacted cord along the coronary groove or shaft (it goes away on its own within a few days).
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Diagnosis of lymphangitis
A lymphologist can diagnose regional lymphangitis during a routine visual examination. In this case, the disease must be differentiated from superficial phlebitis and erysipelas, which can only be done through laboratory and instrumental studies.
Diagnostic signs of lymphangitis:
- pronounced leukocytosis in peripheral blood;
- duplex scanning and ultrasound doppler scanning reveal changes in the lymphatic vessels according to the type of heterogeneity of structure, narrowing of the lumen, reticular changes in the lymph nodes;
- during computed tomography, it is possible to determine the depth and extent of lymphangitis, to distinguish the disease from other pathologies that have similar symptoms;
- Bacteriological culture of a detachable purulent wound makes it possible to identify the pathogen.
In case of a complicated form of the disease, a blood test for sterility is required.
Treatment of lymphangitis
Treatment of lymphangitis is aimed at eliminating the primary focus that provoked the occurrence of the inflammatory process in the lymphatic vessels.
To do this:
You cannot massage, heat inflamed tissues or rub ointments into them. It is important to provide the patient with complete motor rest.
Medications indicated:
- Antibacterial drugs (first and second generation cephalosporins, semisynthetic penicillins, lincosamides, aminoglycosides can achieve the best effect).
- Antihistamines.
- Anti-inflammatory complexes.
Physiotherapeutic procedures can include:
- laser blood irradiation (ILBI);
- ultraviolet blood irradiation (UFOI).
Surgical treatment is performed only if it is necessary to drain the abscess.
Treatment of chronic lymphangitis
In case of a sluggish chronic course of the disease, the patient is prescribed:
- semi-alcohol compresses;
- local ointment dressings;
- X-ray therapy;
- mud therapy;
- compresses with dimethyl sulfoxide;
- Ural Federal District.
Specific treatment for non-venereal lymphangitis of the penis is usually not carried out. If the pathology is caused by a sexually transmitted infection, the underlying disease is treated.
Why is lymphangitis dangerous?
Long-term lymphangitis can lead to:
- lymph circulation disorder (the qualitative composition of lymph changes, its quantity increases significantly);
- obliteration of lymphatic vessels (the lumen of the vessel becomes overgrown);
- development of elephantiasis (skin and subcutaneous tissue thicken due to chronic inflammation of the lymphatic vessels), lymphostasis (tissue swelling resulting from impaired lymph outflow);
- abscess (purulent inflammation of tissues with their melting, which leads to the formation of a purulent cavity);
- sepsis (a systemic inflammatory reaction diagnosed as a result of infectious agents entering the blood);
- cellulite (changes in the structure of the subcutaneous fat layer, which lead to disturbances in lymphatic outflow and lymph circulation).
Prevention
Prevention of acute lymphangitis consists of:
- high-quality and timely treatment of wounds;
- rehabilitation of pustular diseases;
- taking vitamin and mineral complexes;
- observing the rules of personal hygiene.
Secondary prevention of lymphangitis consists of opening the resulting purulent foci and taking antibacterial drugs prescribed by a doctor.
Source: https://nn.MedCentr.online/library/letter/l/illness/limfangit
Diagnosis of lymphangitis
Reticular lymphangitis can be easily diagnosed by a lymphologist during a visual examination, but it should be differentiated from erysipelas and superficial phlebitis. Identification of the primary inflammatory focus helps in establishing the diagnosis.
Recognizing deep lymphangitis can be difficult. In this case, clinical and anamnestic data, the results of instrumental and laboratory studies are taken into account. With lymphangitis, pronounced leukocytosis is observed in the peripheral blood. Doppler ultrasound and duplex scanning visualize changes in lymphatic vessels such as heterogeneity of structure, narrowing of the lumen, the presence of a hyperechoic rim around the vessel, and reactive changes in the corresponding lymph nodes.
Assessment of the severity, prevalence and depth of lymphangitis is carried out using computer thermography. A set of studies makes it possible to distinguish deep lymphangitis from soft tissue phlegmon, deep vein thrombophlebitis, and osteomyelitis. Determination of the causative agent of lymphangitis is carried out by bacteriological culture of discharge from a purulent wound. In case of complicated lymphangitis, a blood test is performed to determine sterility.
Treatment of lymphangitis
First of all, in case of acute lymphangitis, it is necessary to eliminate the primary focus that supports inflammation in the lymphatic vessels.
Treatment of infected wounds, opening of abscesses, phlegmons, panaritiums, their drainage and sanitation are carried out. The affected limb is fixed in an elevated position; the patient is advised to rest. For lymphangitis, massage and self-warming of the area of inflammation, or rubbing in ointments, are unacceptable. Drug treatment includes antibiotics (semi-synthetic penicillins, 1-2nd generation cephalosporins, aminoglycosides, lincosamides), anti-inflammatory and antihistamines, infusion therapy, laser (ILBI) or ultraviolet blood irradiation (UFO).
In the case of chronic sluggish lymphangitis, local ointment dressings, semi-alcohol or dimethyl sulfoxide compresses, mud therapy, and ultraviolet radiation are prescribed; in case of persistent inflammation, radiotherapy is indicated. Treatment for non-venereal lymphangitis of the penis is not required. For lymphangitis caused by an STD, the underlying infection is treated.
Lymphangitis: what it is, symptoms and treatment of inflammation
Endocrinologist of the highest category Anna Valerievna
46259
Update date: April 2020
The inflammatory process of lymphatic trunks and capillaries, which occurs acutely or has a chronic form, is called lymphangitis.
Its distinctive characteristic is the fact that the processes are secondary, that is, they arise against the background of other purulent-inflammatory pathologies.
There is redness of the skin and swelling during inflammation, the presence of pathological processes in regional lymph nodes, general weakness, chills against the background of an increase in body temperature to 40°C. Let's take a closer look at what lymphangitis is.
What is the essence of the disease, its classification
Lymphangitis is accompanied by painful swelling along the inflamed lymphatic vessels, edema, regional lymphadenitis, high body temperature (39-40°C), chills, weakness
Lymphangitis is an inflammation, a secondary pathology that spreads to the vessels of the lymphatic system. The disease develops, as a rule, when the skin is wounded: along the edges of the wound, the skin becomes inflamed, and red stripes radiate from it, which indicates a pathological process in the lymph vessels.
The depth and size of the violation of the integrity of the skin does not play a role in inflammation of the vessels of the lymphatic system - any microtrauma can be the cause.
In most cases, lymphangitis progresses with injuries to the extremities, since it is on the arms and legs that the largest number of microbes are found. But it can also be observed on other parts of the body. After infectious agents penetrate into the interstitial cavities, they first affect the capillaries, and then the vessels and lymph nodes.
In medical practice, lymphangitis is classified according to several parameters:
| According to the flow form | · acute – symptoms are clearly manifested; · chronic – symptoms are not manifested, but swelling is pronounced; |
| According to the nature of the inflammatory process | · simple; · purulent; |
| By depth of location | · superficial; · deeply located; |
| By pathogen | · viral lymphangitis; · bacterial lymphangitis; |
| For affected vessels | · reticular or reticular, when the lesion spreads to small superficial capillaries; · stem (truncular), when lymphangitis affects one or more vessels. |
The following forms of lymphangitis can also be distinguished:
- venereal – develops against the background of some sexually transmitted diseases;
- non-venereal lymphangitis or lymphangitis of the penis - affects the male genital organ as a result of infectious and inflammatory processes against the background of microtraumas that occur during unprotected sexual intercourse or during masturbation;
- cancerous lymphangitis - occurs against the background of malignant neoplasms;
- perilymphangitis is an inflammatory process localized around the lymphatic trunk.
Symptoms and signs
Most often, lymphangitis progresses with injuries to the extremities, since it is on the arms and legs that the largest number of microbes are found
The clinical picture directly depends on the size of the vessels that were affected. When the pathological process affects small capillaries, it appears on the skin in the form of small red stripes that go from the site of inflammation to the local lymph nodes. When palpating the affected area, a thickening is clearly felt, as if there is a cord running under the red stripe.
When the cause of inflammation of the lymphatic vessels is a boil or a festering wound, redness without clear boundaries is observed around it. Acute lymphangitis is accompanied by pronounced local manifestations and intoxication.
The following general symptoms are identified:
- feverish conditions, chills;
- weakness, the patient complains of poor general health;
- increased body temperature;
- headache;
- increased sweating;
- limited limb movements;
- numbness of the tongue.
A blood test in the acute form indicates an excess of leukocytes.
There are also a number of local symptoms that more clearly indicate lymphangitis:
- the skin around the wound site turns red and swells, the redness does not have clearly defined boundaries;
- the site of swelling becomes hot to the touch;
- characteristic red lines spread across the skin of the limb;
- a vascular network appears at the site of the lesion;
- when pressing on the red lines or during friction, a pressing pain is felt along the entire length of the inflamed vessel;
- the patient feels throbbing pain in the affected limb;
- the skin becomes rough and dries;
- Local lymph nodes enlarge.
If we talk about the chronic form of lymphangitis, then, in addition to the above symptoms, the following manifestations are also observed:
- vasospasm;
- expansion of infected areas;
- stagnant blood processes and slow blood flow;
- swelling of the infected limb.
In some cases, the functioning of the organ near which the inflamed vessel passes is also disrupted. This is how lymphangitis of the lungs occurs, for example.
If the lymphadenitis is deep, then there may be no redness on the skin. Only painful sensations appear when pressing on the areas where the pathological process occurs.
Diagnostics
Vascular ultrasound will help more accurately diagnose and identify the pathology of the disease.
A lymphologist diagnoses the disease. First, the doctor interviews the patient, examines all complaints, and conducts an initial examination to determine the expressed symptoms. To confirm the diagnosis, the patient is referred for hardware and laboratory tests.
Laboratory tests are also necessary to exclude erysipelas and phlebitis (inflammatory process of the venous walls). Their symptoms are similar.
The main diagnostic methods include the following:
- General and biochemical blood test. Indicates deviations from the norm, allows you to determine inflammatory processes in blood vessels;
- immunological tests to determine antibodies in the blood that are responsible for inflammation;
- biopsy. Examination of a skin fragment under a microscope is usually used to exclude erysipelas;
- Vascular ultrasound. This method allows you to assess the condition of the vessels visually: see the width of the lumen, foci of inflammation, deformation, etc.;
- Dopplerography is an additional ultrasound examination that allows you to determine the speed of blood flow. In difficult cases, the doctor prescribes duplex scanning - this is Dopplerography and ultrasound examination in combination;
- MRI. Prescribed for acute lymphangitis to determine the general condition of the body and identify concomitant diseases.
To determine the type of bacteria that caused the pathological process, a bacteriological examination of the contents of the wound is prescribed. In case of pulmonary lymphangitis, additional radiography is required.
Treatment
Therapy of acute lymphangitis involves the elimination of the primary focus that provoked the development of the inflammatory process in the lymphatic vessels. The patient is treated with infected wounds, phlegmons and abscesses are opened, they are drained and sanitized. After these measures, the patient is recommended to have motor rest with the limb fixed in an elevated state.
Any independent treatment of lymphangitis can lead to the development of all kinds of complications of this disease. In particular, heating damaged areas, rubbing ointments and massage are prohibited.
Drug treatment
Conservative therapy is the basis for treating the disease in the first stages of its development. In order to effectively combat the source of infection, an integrated approach is required. It can be achieved using medications from the following groups:
- antibiotics;
- antihistamines (antiallergic) drugs;
- anti-inflammatory drugs.
The dosage and duration of taking these drugs are determined by the doctor individually for each patient. Therapy is carried out under medical supervision and adjusted if necessary.
Physiotherapy
Physiotherapeutic procedures enhance the effect of drug treatment
Physiotherapeutic procedures are an addition to drug treatment. They enhance the effect of drugs and help stabilize the patient’s condition. Typically, the following procedures are used for lymphangitis:
- Ural Federal District;
- blood irradiation using laser (ILBI) and ultraviolet radiation (UFO);
- mud therapy;
- dressings with medicinal ointments;
- semi-alcohol compresses.
Lymphangitis of a non-venereal nature most often does not require specialized treatment. In this case, all that is required is to eliminate the source of infection. The disease goes away on its own within a few days after the inflammatory process subsides.
If the pathology is characterized by a protracted course, then X-ray therapy is used to eliminate the primary focus. The essence of this procedure is to have a destructive effect on the affected cells. As a result, vital processes in the affected cellular structures gradually slow down. This leads to a gradual decrease in the inflammatory focus.
Forecast
Modern medicine makes it possible to effectively treat lymphangitis at almost any stage of the disease. It should be understood that the long course of the chronic form of the disease can cause a number of complications. The most severe of them are:
- obliteration of lymphatic vessels;
- lymphostasis;
- various lymph circulation disorders.
Therefore, the sooner professional therapy is started, the better.
Measures to prevent lymphangitis include timely sanitation of purulent foci, primary treatment of wounds and adequate antibiotic therapy.
Source: https://limfouzel.ru/zabolevaniya/limfangit/
Causes
The cause of lymphangitis is the entry of pathological microorganisms into the vessels. In most cases, the disease is provoked by streptococcus, Proteus, Escherichia coli and Staphylococcus aureus. Specific lymphangitis is triggered by Koch's bacillus (the causative agent of tuberculosis).
Infectious agents penetrate the lymph flow from purulent or inflamed foci - boils, abscesses, abrasions. First, microbes enter the interstitial fluid, then into the lymphatic capillaries, from them into large vessels and nodes.
The inflammatory process is characterized by swelling and increased permeability of the inner layer of blood vessels, release of fluid, loss of fibrin fibers and the formation of blood clots. As a result, local lymph flow deteriorates. Without treatment, purulent lymphangitis may develop, blood clots may melt, and perilymphangitis may occur - inflammation of the tissues surrounding the lymphatic vessels (blood capillaries, muscles, joints).
The likelihood that a violation of the integrity of the skin will lead to lymphangitis is determined by the size of the wound, the activity of the microflora, the state of general immunity and the characteristics of lymph circulation in the affected area.
Since most organs and tissues of the human body are penetrated by lymphatic vessels, the pathological process can affect any part of the body. There is lymphangitis of the breast, penis, lungs, arms, legs, and so on.
The disease is classified according to other criteria:
- according to the nature of the course - chronic and acute lymphangitis.
- according to the size of the vessels - reticular (affects many superficial capillaries) and stem lymphangitis (affects large vessels).
In addition, a distinction is made between non-venereal lymphangitis of the penis and venereal lymphangitis. In the first case, the pathology is associated with mechanical trauma to tissues, and in the second - with urogenital infections.
Forecast
Modern medicine makes it possible to effectively treat lymphangitis at almost any stage of the disease. It should be understood that the long course of the chronic form of the disease can cause a number of complications. The most severe of them are:
- obliteration of lymphatic vessels;
- lymphostasis;
- various lymph circulation disorders.
Therefore, the sooner professional therapy is started, the better.
Measures to prevent lymphangitis include timely sanitation of purulent foci, primary treatment of wounds and adequate antibiotic therapy.
Treatment of inflammation of lymphatic capillaries and blood vessels gives a favorable prognosis for life. How long do people live with lymphangitis? People don’t die, but complications are possible if you neglect your own health:
- Infection of lymphatic vessels;
- Elephantiasis (lymphedema);
- Circulatory disorder.
Prevention of lymphangitis:
- Treatment of infectious diseases as the basis for prevention;
- Treatment of wounds;
- Seek medical help at the first symptoms.
Symptoms
Symptoms of lymphangitis vary depending on where and how deeply the vessels are inflamed. In any case, general intoxication occurs:
- temperature increase up to 40 °C;
- sweating;
- chills;
- headache;
- weakness;
- fast fatiguability.
Reticular (reticular) regional lymphangitis is accompanied by pain and burning in the area of inflammation of the capillaries around the wound or abscess, as well as such local skin changes as:
- redness;
- edema;
- the appearance of a dense red network of blood vessels.
Symptoms of stem lymphangitis are red stripes on the skin (inflamed large vessels), pain, stiffness of movement when the limbs are affected, swelling that grows in case of thrombosis, enlargement of regional lymph nodes.
When deep vessels become inflamed, the skin turns pale. Severe swelling, sharp pain when moving, and lymphodema (impaired lymph flow) occur.
The addition of perilymphangitis to acute lymphangitis can provoke the appearance of subfascial phlegmon - suppuration in the connective tissue membrane covering the muscles. Its untimely opening can lead to sepsis.
Cancerous or carcinomatous lymphangitis of the lungs occurs when malignant cells metastasize into the lymphatic vessels from the lungs, breast or other organs. Symptoms of the cancerous form are shortness of breath and pain in the lungs. Carcinomatous pulmonary limited lymphangitis does not manifest itself in any way. Its diffuse version is accompanied by shortness of breath, cough with blood in the sputum, fever, and so on.
Lymphangitis of the mammary gland (erysipelas-like cancer) is characterized by such signs as redness of the skin in the form of spots with jagged edges, as well as hyperthermia.
Acute lymphadenitis of the face and neck can appear if there is a focus of infection in the oral cavity. Most often, the pathological process affects the lymphatic vessels near the ears, under the jaw, and on the neck. The disease manifests itself as redness and pain.
Non-venereal lymphangitis of the penis lasts several days and goes away on its own. Its symptom is a painless compaction (“swollen vein”) in the area of the coronary sulcus.
The chronic form of lymphangitis, unlike the acute form, does not have clear symptoms. As a rule, it is accompanied by blockage of lymph vessels and persistent swelling.
Lymphangitis - what is it, causes of the disease, symptoms and treatment
What is lymphangitis? This is an inflammation of the lymphatic vessels, which can occur for various reasons. Its appearance is accompanied by a number of characteristic symptoms.
No one is immune from this disease, and therefore we will now talk about why it can arise, what signs can actually be used to identify it, as well as how diagnosis is carried out and treatment is carried out.
Manifestation of the disease
To begin with, it’s worth talking in a little more detail about what lymphangitis is. This is a chronic or acute inflammation of the lymphatic capillaries or trunks, which occurs secondary. It is always preceded by a purulent-inflammatory process.
This phenomenon is accompanied by swelling along the inflamed vessels, which is noticeable to the naked eye. Swelling is also possible. Lymphadenitis, an inflammation of the lymph nodes of a purulent nature, often develops.
It is important to note that with this disease, completely different vessels located at any depth can be affected. As a rule, inflammation is concentrated on the extremities, and this is logical - after all, they are injured most often.
You should consult a doctor as soon as you notice mild manifestations of lymphangitis, the photo of which shows a truly unpleasant sight. If a person begins to progress with this disease, it means that the primary pathology is progressing.
Etiology
Many people know that the lymphatic system is a complex vascular structure. When pathogenic bacteria and viruses enter the body, immune cells are produced in the lymph, which become a barrier to them and also cleanse the blood.
If this protection does not exist (the reason is severe infection and weakened immunity), then this “barrier” does not arise.
As a result, bacteria from the purulent focus enter the interstitial space. And from there - into the lymphatic system. As a result, the endothelium of small vessels is affected and inflammation occurs. First, reticular lymphangitis forms, and then stem lymphangitis.
Causes
As mentioned earlier, lymphangitis (ICD-10 - I89.1) develops secondarily. The prerequisite is a deep or superficial purulent-inflammatory focus. In general, the reasons can be identified as follows:
- Infected wound or abrasion.
- Phlegmon.
- Carbuncle.
- Abscess.
- Furuncle.
If we talk about pathogens, they are the following pathogens:
- Staphylococcus aureus.
- Proteus.
- Beta-hemolytic streptococcus.
- Escherichia coli.
It is important to note that specific lymphangitis usually occurs in patients who have had tuberculosis.
Symptoms
There are several signs by which you can determine the presence of lymphangitis. The symptoms are as follows:
- High temperature, reaching 39-40 °C.
- Severe superficial hyperemia observed around the infectious focus.
- The presence of narrow red stripes on the skin that stretch to the regional lymph nodes.
- Pain, induration, swelling of the cords.
- Tension and swelling of surrounding tissues.
- Painful lumps along the vessels, resembling rosaries or cords.
- Chills.
- Strong headache.
- Weakness.
- Sweating.
Over time, symptoms worsen. Sharp pain is observed, lymphedema begins to develop, some areas transform into an abscess or phlegmon. If they are not opened, sepsis may develop.
Lymphangitis of the lower extremities or any other parts of the body can be determined by a specialist during a visual examination. The difficulty lies in only one thing - the disease must be differentiated from superficial phlebitis and erysipelas. And here identifying the inflammatory focus helps.
It will be difficult to detect deep lymphangitis. What it is? This is the name of a disease in which pronounced leukocytosis can be detected in the peripheral blood. That is why it is necessary to submit this biological fluid for analysis.
In addition, the lymphologist must take into account the results of laboratory and instrumental studies and clinical and anamnestic data.
The patient is also referred to undergo the following diagnostic procedures:
- Duplex scanning.
- Ultrasound Doppler.
- Computer thermography.
- Bacterial culture.
All this helps to determine changes in the lymphatic vessels, narrowing of the lumen, the depth and severity of lymphangitis, as well as determine which microorganism was the causative agent.
Principles of treatment
So, based on all of the above, you can understand what lymphangitis is. This is a serious disease, and it is better not to delay its treatment.
The first step is to eliminate the primary focus, which maintains inflammation in the lymphatic vessels. To do this, the doctor treats infected wounds, opens phlegmons, panaritiums, abscesses, after which he drains and sanitizes them.
The affected limb is then fixed in a slightly elevated position. The person will have to maintain motor rest.
Many people do not immediately consult a doctor and prefer to treat themselves. So, you can’t do this! The following actions are also strictly prohibited before opening (and after):
- Rubbing in ointments.
- Warming the affected area.
- Massage.
Drug treatment is indicated, but it is prescribed only by a lymphologist, and only after examining the patient.
Drug therapy
Now we can talk about the treatment of lymphangitis. After the actions described above have been completed, a rehabilitation period begins, during which the person must take a course of medications. He may be assigned:
- Cephalosporins: Cefazolin or Cefotaxime. They have a bactericidal effect.
- Macrolides: Erythromycin or Azithromycin. They have a bacteriostatic effect.
- Aminoglycosides: Gentamicin or Netilmicin. Effective in treating infections.
- Antihistamines: Suprastin or Tavegil. Suppresses the effects of free histamine.
- Anti-inflammatory non-steroidal drugs: Nimesil or Ibuprofen. Well relieves skin redness, swelling, pain and inflammation.
The patient may also be recommended to undergo ultraviolet or laser irradiation. These procedures significantly speed up the healing process and also improve the overall condition.
Chronic and persistent course
These are special cases. To cure a patient facing chronic or persistent lymphangitis of the extremities (or other part of the body), the following is prescribed:
- Local ointment dressings.
- Treatment with mud.
- Compresses with dimethyl sulfoxide or the addition of alcohol.
- Ural Federal District.
- X-ray therapy.
Also a special case is venereal infectious lymphangitis. This is a serious case, but the treatment here is simple - it is aimed at eliminating STDs.
What medications the venereologist will prescribe depends on the pathogen. Some medications help in the fight against gonorrhea, but other medications will be needed to treat syphilis - everything is very individual.
Non-venereal lymphangitis of the penis
This disease deserves separate consideration. It usually affects the vessels around the coronary sulcus or along the trunk of the organ. Most men who encountered this problem had:
- Frequent and prolonged intimate acts.
- Unusual positions that caused the penis to bend.
- Increased masturbation.
Specific symptoms include the following:
- Sharp pain in the groin area.
- Purulent discharge.
- Swelling and hardening of the penis.
- The appearance of painful and purulent infiltrates.
- General intoxication.
Non-venereal lymphangitis of the penis is treated in the same ways as inflammation that occurs in another part of the body. However, in this case there are specific recommendations.
To prevent inflammation from occurring in such an intimate place, you need to avoid any injuries to the penis and prolonged masturbation. You need to adhere to a measured sex life, as well as maintain hygiene.
Lymphangitis of the lungs
This is a specific, special inflammation that can become cancerous. With this disease, metastases spread through the lymphatic vessels of the lungs. In these cases, the primary cancer occurs in the pancreas, breast, colon, or stomach.
The following symptoms are observed:
- Persistent dry cough.
- Weakness.
- Dyspnea.
- Low-grade body temperature.
- Respiratory failure.
- Hyperchromic anemia.
Often a person is treated unsuccessfully for sore throat and bronchitis, since the symptoms are similar. But here an X-ray examination is necessary. It is this that allows you to notice the transformation of the pulmonary pattern, as well as other changes.
You must make an appointment for an x-ray immediately. It is better to make mistakes in assumptions than to allow the lymph nodes to enlarge to such a size that they begin to appear on the tomogram.
Folk remedies
They can be used during the rehabilitation period only after permission from a doctor. The following tools are popular:
- Freshly squeezed beet juice mixed with carrot juice in a ratio of 1:4. This drink is a natural “supplier” of chlorine to the body, which is necessary for the functioning of the lymph nodes.
- Baths made from dried nut leaves. You need to take 1 kg of them, add water (2-3 l) and boil for 45 minutes. For a foot or sitz bath, ¼ of this volume is sufficient. You will have to pour the entire broth into a regular one.
- Nettle decoction. This plant has an excellent anti-inflammatory effect. You need to take 1 tbsp. l. nettle leaves and brew with 1 cup of boiling water. Let it brew for 30 minutes. Strain and drink half a glass twice a day before meals.
- Dandelion decoction. This plant is a storehouse of vitamin C and the antioxidant luteolin. You need to take 1 tsp. dandelion leaves, pour a glass of boiling water and leave for 20 minutes. Then strain. Drink ¼ half an hour before meals three times a day.
- Aloe tincture. This plant is used to treat various serious ailments, even pneumonia and radiation sickness. You need to wash a few aloe leaves and squeeze out the juice - you should get 150 ml. Then mix with 1 glass of honey, dilute with Cahors (350 ml). Leave the mixture for 5 days in a dark place. Then take 1 tbsp. l. three times a day half an hour before meals.
These are good remedies, and with their help you can strengthen your immune system, but they are not a replacement for drug treatment. We must remember this.
Complications
If a person does not ignore the symptoms and begins treatment on time, the disease can be eliminated without consequences. Otherwise, he will suffer from complications, including:
- Circulatory disorder.
- Lymphedema.
- Infection of lymphatic vessels.
And these complications, in turn, are fraught with serious consequences. Lyphedema, for example, is almost always eliminated surgically - the vessels are crossed, followed by coagulation of the central ends and the creation of anastomoses.
And a circulatory disorder is even fraught with blood leaving the vessels and changing its volume.
This is why it is important to immediately seek help from a doctor. Once neglected, an untreated infection can lead to very serious consequences that are dangerous to health and life.
Diagnostics
Features of the diagnosis of lymphangitis depend on the form of the disease and the primary pathology. The reticular variant is identified based on a history and visual examination of the affected area. It is differentiated from phlebitis and erysipelas. The defining moment is the detection of a purulent-inflammatory focus.
Brainstem lymphangitis is more difficult to detect. To diagnose it, an ultrasound duplex scan is performed, which shows:
- heterogeneous structure of blood vessels;
- the presence of a light (hyperechoic) rim around them;
- narrowing of the lumen;
- changes in nearby lymph nodes.
To assess the degree and extent of inflammation in the vessels and surrounding tissues, computer thermography is performed - registration and analysis of infrared radiation from the body surface. The use of these methods makes it possible to distinguish deep lymphangitis from phlegmon, thrombophlebitis and osteomyelitis.
Regardless of the type of disease, laboratory tests are carried out:
- general blood test - demonstrates an increase in ESR, an increased level of leukocytes and a shift in the leukocyte formula to the left (the appearance of immature forms of white blood cells);
- bacteriological culture of discharge from a purulent focus - allows you to identify the causative agent of inflammation;
- blood test for sterility - carried out in case of complicated course.
Inflammation of the lymph vessels of the lungs is diagnosed using x-rays. In the carcinomatous form, the image shows diffuse darkening in the pathological area and enlarged lymph nodes. With cancer - a linear shadow reaching the roots of the lungs, without changes in the lymph nodes.
Non-venereal lymphangitis of the penis is detected by examination and palpation. It is differentiated from thrombophlebitis, syphilis, genital herpes and chlamydial or gonococcal urethritis. For this purpose, PCR, serological testing and bacteriological culture are additionally carried out.
Treatment
The first stage of treatment for lymphangitis is the elimination of the primary source of infection. For this purpose, wounds are treated, phlegmons, abscesses, boils and other purulent elements are opened, with their subsequent drainage.
If the inflammatory process develops in the vessels of the extremities, then they are immobilized and lifted upward to improve the outflow of lymph. The patient is prescribed bed rest.
To stop the spread of infection during lymphangitis, antibiotics are used - semisynthetic penicillins, aminoglycosides, lincosamides, first and second generation cephalosporins. The choice of drug is made on the basis of bacteriological culture. The dosage regimen depends on the characteristics of the clinical picture.
In addition, drug therapy includes drugs that help reduce inflammation and pain:
- non-steroidal anti-inflammatory drugs - nimesulide, ibuprofen, but only if the patient does not have erosive gastrointestinal diseases;
- antihistamines – loratadine, cetirizine, chloropyramine.
Additional methods of treating lymphangitis with severe intoxication:
- infusions of detoxifying substances;
- laser irradiation of blood - improves the properties of red blood cells and blood circulation, stimulates metabolism, relieves inflammation;
- irradiation of blood with ultraviolet light - ensures the activation of antioxidants, increasing the level of hemoglobin, as well as suppressing the activity of viruses and bacteria.
In case of acute lymphangitis, massage, heating the affected area and rubbing ointments into it are contraindicated.
Therapy for the chronic form includes:
- dressings with ointments;
- compresses with alcohol and dimethyl sulfoxide;
- mud applications;
- ultraviolet treatment.
If it is not possible to achieve an improvement in the patient's condition, radiography is used - low-dose irradiation of foci of inflammation in order to destroy pathogenic microorganisms and activate regeneration processes.
Non-venereal lymphangitis of the penis does not require treatment. Once the venereal nature of the disease is established, the underlying pathology is treated with antibiotics. For cancerous and carcinomatous inflammation of the lymph vessels of the lungs or mammary gland, chemotherapy and radiation therapy are indicated.