Atrial septal defect - description, causes, symptoms (signs), diagnosis, treatment.
Atrial septal defect (ASD) is a congenital heart defect with communication between the atria. Statistical data: 7.8% of all congenital heart disease detected in infancy, and 30% in adults;
VSD of the ostium secundum type - 70%, ostium primum - 15%, sinus venosus - 15%; Lutembashe syndrome accounts for 0.4% of all cases of ASD, the combination of ASD with mitral valve prolapse - 10–20%; the predominant gender is female (2:1–3:1). Code according to the international classification of diseases ICD-10:
- Q21.1 Atrial septal defect
Etiology: factors that form congenital heart disease (see Tetralogy of Fallot).
Pathogenesis • The magnitude and direction of shunt depend on the size of the defect and the relative compliance of the ventricles • In adults, the right ventricle is more compliant than the left, as a result of which shunt occurs from the left atrium to the right • A small shunt leads to a moderate volume overload of the right heart, and pressure in the pulmonary artery remains normal • The severity of pulmonary hypertension may be insignificant even with a large shunt • Only in rare cases does severe pulmonary hypertension develop, leading to right ventricular failure and right-to-left shunt • Unlike VSD, with ASD the shunt is smaller and affects only the right side of the heart.
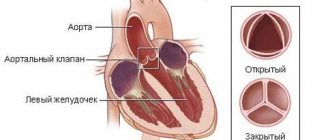
Variants of ASD • Ostium secundum (secondary defects) are localized in the area of the oval fossa, are often multiple, accompany many syndromes: Holt-Oram syndrome (ASD of the ostium secundum type in combination with digital hypoplasia), Lutembashe syndrome (combination of ASD with mitral valve stenosis), combination of ASD with mitral valve prolapse, etc. • Ostium primum (primary defects) are usually large in size, localized in the lower part of the septum, at the attachment point of the mitral and tricuspid valves, interatrial and interventricular septa. They are part of an open AV canal and are often combined with abnormal drainage of the pulmonary veins, splitting of the anterior mitral valve leaflet, mitral regurgitation and Down syndrome • Defects of the sinus venosus type are localized near the mouth of the superior vena cava and the sinus node, often combined with sick sinus syndrome, AV - nodal rhythm and abnormal drainage of the pulmonary veins.
Clinical picture
Complaints: shortness of breath, palpitations, fatigue during physical activity, retarded physical development, frequent infections, paradoxical embolisms.
Objectively • Pallor of the skin • Harrison's furrows - displacement of areas of the chest as a result of chronic shortness of breath • Splitting of the first tone with a pronounced component of the tricuspid valve • Pronounced fixed splitting of the second tone (pronounced - due to - due to prolongation of the time of blood ejection from the right ventricle; fixed - due to - due to the fact that the dependence of venous return on the phases of breathing is leveled by discharge from the left atrium) • An ejection click and a soft systolic murmur of relative stenosis of the pulmonary artery in the second intercostal space to the left of the sternum • Due to an increase in blood flow through the tricuspid valve, a low-frequency diastolic murmur sometimes occurs above the xiphoid process of the sternum.
Instrumental diagnostics
• ECG. Signs of hypertrophy and overload of the left sections, and with pulmonary hypertension - also of the right. With ostium primum, there is a sharp deviation of the EOS to the left due to the displacement of the hypoplastic branch of the left leg of the His bundle forward. Various variants of sick sinus syndrome, AV block. With a defect such as sinus venosus - lower atrial rhythm or AV rhythm - junction.
• Jugular venography: equal amplitude of A and V waves.
• X-ray examination of the chest organs. Strengthening the pulmonary pattern. Expansion and lack of structure of the roots of the lungs, bulging of the right atrium arch and upward displacement of the right cardiovasal angle. Fluoroscopy reveals increased pulsation of the roots of the lungs (a rather specific sign). The “Turkish saber” symptom with concomitant anomalous drainage of the right pulmonary veins into the superior vena cava.
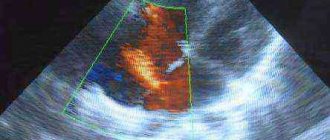
• EchoCG. Hypertrophy and dilatation of the left sections, and with pulmonary hypertension - also of the right. Visualization of ASD in Doppler and B-mode. Differentiation from an open foramen ovale (the anatomical closure of the latter occurs no later than 2 years of life) is the inconsistency of visualization of the discharge in color Doppler mapping and the presence of a leaflet in the cavity of the left atrium. Diagnosis of associated anomalies (abnormal drainage of the pulmonary veins, valvular defects, etc.). The degree of discharge and the ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) are determined. Adults undergo transesophageal echocardiography. With intravenous contrasting of the right parts of the heart, there is a negative contrast effect (displacement of the contrast agent by a stream of blood from the left atrium).
• Radionuclide angiocardiography (first pass method or equilibrium): registration of pathological discharge and its quantitative assessment, diagnosis of concomitant abnormal drainage of the pulmonary veins and ventricular dysfunction.
• Probing of the cardiac cavities •• Indicated for suspected pulmonary hypertension, before open-heart surgery and with conflicting clinical data •• If the catheter can be passed from the right atrium to the left, then this in itself cannot be a sign of an atrial septal defect: sometimes the catheter it is possible to carry out through the open foramen ovale •• Tests are carried out with aminophylline and oxygen inhalation to determine the prognosis regarding the reversibility of pulmonary hypertension •• The ratio of pulmonary minute blood flow to systemic blood flow (Qp/Qs) is calculated - a reference indicator of the amount of discharge.
• Right atriography, angiopulmonography: flow of contrast from the right atrium to the left; identification of concomitant abnormal pulmonary venous drainage.
Drug therapy. In uncomplicated ASDs of the ostium secundum type, infective endocarditis prophylaxis is usually not carried out. For ASDs of the ostium primum type, large defects of the sinus venosus type, and a combination of ASDs with mitral valve defects, antibiotics are prescribed before and for 6 months after uncomplicated surgical correction. For right ventricular failure, diuretics are prescribed.
Surgery
Indications: Qp/Qs ratio is 1.5 or more, defects of the ostium primum type, large defects of the ostium secundum type, concomitant hemodynamically significant anomalies (abnormal drainage of the pulmonary veins, mitral stenosis, etc.).
Contraindications: severe concomitant pathology that threatens the patient’s life; end-stage circulatory failure, irreversible pulmonary hypertension, the ratio of total pulmonary vascular resistance to peripheral vascular resistance is 0.9 or more.
Methods of surgical treatment. Endovascular correction with a button or two-patch Sideris device or an Amplatz device is feasible for central defects no larger than 2 cm in size. In the absence of experience in endovascular treatment, small defects are sutured under artificial circulation. In other cases, ASD repair with a synthetic or autopericardial patch under artificial circulation is recommended.
Specific postoperative complications • Sick sinus syndrome (after correction of sinus venosus type defects) • AV block (after correction of ostium primum type defects) • With mitral regurgitation that existed before surgery, symptoms may worsen after correction of ASD • Atrial fibrillation that occurred before surgery , as a rule, persists after it.
Forecast. In early childhood the course is benign. In rare cases, severe circulatory disorders can lead to death in the first months of life. Spontaneous closure of the defect is possible before the age of 5. The average life expectancy without treatment is 40 years. 5–15% of patients die before age 30. 10 - year survival rate - 90%, 20 - year - 88%, 30 - year - 67%; 40 years old - 44%, 50 years old - 25%, 60 years old - 13%, 70 years old - 7%. More than 75% of patients with large defects die from other causes. For uncomplicated defects of the ostium secundum type, perioperative mortality is less than 1%, it is slightly higher for defects of the ostium primum type, the latter also require mitral valve replacement or repair.
Abbreviations. Qp/Qs is the ratio of the pulmonary minute volume of blood flow to the systemic one.
ICD-10 • Q21.1 Atrial septal defect
Source: gipocrat.ru
Q24.9 Congenital heart defect, unspecified
Other diagnoses in the ICD 10 section
- Q24.0 Dextrocardia
- Q24.1 Levocardia
- Q24.2 Triatrial heart
- Q24.3 Infundibular stenosis of the pulmonary valve
- Q24.4 Congenital subaortic stenosis
The information posted on the site is for informational purposes only and is not official.
Heart defects.congenital (classification)
Classification of congenital heart disease by severity classes (J. Kirklin et al. 1981) • Class I. It is possible to perform a planned operation later than 6 months: VSD, ASD, radical correction for tetralogy of Fallot • Class II. Elective surgery can be performed within 3–6 months: radical correction for VSD, open atrioventricular canal (PAVC), palliative correction for TF • Class III. A planned operation can be performed within a period of up to several weeks: radical correction for transposition of the great vessels (TMS) • Class IV. Emergency surgery with a maximum preparation time of several days: radical correction for total anomalous pulmonary vein drainage (TAPD), palliative correction for TMS, VSD, OAVC • Class V. The operation is performed urgently due to cardiogenic shock: various types of defects in the decompensation stage.
Classification of congenital heart disease by prognostic groups (Fyler D. 1980) • 1 group. Relatively favorable prognosis (mortality during the first year of life does not exceed 8–11%): patent ductus arteriosus, VSD, ASD, pulmonary stenosis, etc. • Group 2. Relatively unfavorable prognosis (mortality during the first year of life is 24–36%): tetralogy of Fallot, myocardial diseases, etc. • Group 3. Poor prognosis (mortality during the first year of life is 36–52%): TMS, coarctation and stenosis of the aorta, tricuspid valve atresia, TADLV, single ventricle of the heart, OAVC, origin of the aorta and pulmonary artery from the right ventricle, etc. • Group 4. Extremely unfavorable prognosis (mortality during the first year of life is 73–97%): hypoplasia of the left ventricle, pulmonary atresia with an intact interventricular septum, common truncus arteriosus, etc.
Classification of congenital heart disease according to the possibility of radical correction (Turley K. et al. 1980) • 1 group. Defects for which only radical correction is possible: aortic stenosis, pulmonary artery stenosis, TADLV, triatrial heart, coarctation of the aorta, patent ductus arteriosus, aortopulmonary septal defect, ASD, mitral valve stenosis or insufficiency • Group 2. Defects in which the advisability of radical or palliative surgery depends on the anatomy of the defect, the age of the child and the experience of the cardiology center: various variants of TMS, pulmonary atresia, common truncus arteriosus, tetralogy of Fallot, OAVC, VSD • group 3. Defects for which only palliative operations are possible in infancy: a single ventricle of the heart, some variants of the origin of the great vessels from the right or left ventricle with pulmonary stenosis, atresia of the tricuspid valve, atresia of the mitral valve, hypoplasia of the ventricles of the heart.
Abbreviations • PAVK - patent atrioventricular canal • TMS - transposition of the great vessels • TADPV - total anomalous drainage of the pulmonary veins.
ICD-10 • Q20 Congenital anomalies [malformations] of the heart chambers and connections • Q21 Congenital anomalies [malformations] of the cardiac septum • Q22 Congenital anomalies [malformations] of the pulmonary and tricuspid valves • Q23 Congenital anomalies [malformations] of the aortic and mitral valves • Q24 Other congenital anomalies [malformations] of the heart.
Mechanisms of development of anomalies and causes
Aneurysm of the interatrial septum in newborns
The etiology of this anomaly is not fully understood today, despite the fact that aneurysm of the interatrial septum (as the term “interatrial septum” is abbreviated) has been known for a long time.
Studying the mechanism of development and causes of the anomalous phenomenon, doctors have identified several theories. Aneurysm of the interatrial septum in a newborn causes disagreement among scientists. One group argues that it is associated with a genetic factor, that is, it is a hereditary pathology, and the other - that abnormal disorders occurred during intrauterine development and could be caused by infectious diseases of the expectant mother.
Regarding the mechanism of development of atrial septal aneurysm in children, doctors describe another quite probable process. During fetal development, this septum contains the oval window, which closes soon after the baby is born. Presumably, under the influence of various factors destabilizing the process, a weak spot (thinned, insufficiently dense) remains at the site of this window, which, under the pressure of the blood flow, begins to stretch and forms an abnormal protrusion, i.e., an aneurysm. Closing the window too late can also cause an abnormal structure of the septum, which contributes to the formation of an aneurysm.
In adults, abnormal protrusion develops as a result of a previous myocardial infarction. The dangerous influence of the development of atherosclerosis, arterial hypertension, and smoking cannot be ruled out.
Based on what caused the formation of the anomalous phenomenon, the appropriate code for the aneurysm of the interatrial septum is selected according to ICD 10. For example, congenital anomalies are in group Q21, and the consequence of a heart attack is I23.1.
Q24.9 Congenital heart defect, unspecified
Other diagnoses in the ICD 10 section
Q24.0 Dextrocardia Q24.1 Levocardia Q24.2 Triatrial heart Q24.3 Infundibular stenosis of the pulmonary valve Q24.4 Congenital subaortic stenosis
The information posted on the site is for informational purposes only and is not official.
Heart defects.congenital (classification)
Classification of congenital heart disease by severity classes (J. Kirklin et al. 1981) • Class I. It is possible to perform a planned operation later than 6 months: VSD, ASD, radical correction for tetralogy of Fallot • Class II. Elective surgery can be performed within 3–6 months: radical correction for VSD, open atrioventricular canal (PAVC), palliative correction for TF • Class III. A planned operation can be performed within a period of up to several weeks: radical correction for transposition of the great vessels (TMS) • Class IV. Emergency surgery with a maximum preparation time of several days: radical correction for total anomalous pulmonary vein drainage (TAPD), palliative correction for TMS, VSD, OAVC • Class V. The operation is performed urgently due to cardiogenic shock: various types of defects in the decompensation stage.
Classification of congenital heart disease by prognostic groups (Fyler D. 1980) • 1 group. Relatively favorable prognosis (mortality during the first year of life does not exceed 8–11%): patent ductus arteriosus, VSD, ASD, pulmonary stenosis, etc. • Group 2. Relatively unfavorable prognosis (mortality during the first year of life is 24–36%): tetralogy of Fallot, myocardial diseases, etc. • Group 3. Poor prognosis (mortality during the first year of life is 36–52%): TMS, coarctation and stenosis of the aorta, tricuspid valve atresia, TADLV, single ventricle of the heart, OAVC, origin of the aorta and pulmonary artery from the right ventricle, etc. • Group 4. Extremely unfavorable prognosis (mortality during the first year of life is 73–97%): hypoplasia of the left ventricle, pulmonary atresia with an intact interventricular septum, common truncus arteriosus, etc.
Classification of congenital heart disease according to the possibility of radical correction (Turley K. et al. 1980) • 1 group. Defects for which only radical correction is possible: aortic stenosis, pulmonary artery stenosis, TADLV, triatrial heart, coarctation of the aorta, patent ductus arteriosus, aortopulmonary septal defect, ASD, mitral valve stenosis or insufficiency • Group 2. Defects in which the advisability of radical or palliative surgery depends on the anatomy of the defect, the age of the child and the experience of the cardiology center: various variants of TMS, pulmonary atresia, common truncus arteriosus, tetralogy of Fallot, OAVC, VSD • group 3. Defects for which only palliative operations are possible in infancy: a single ventricle of the heart, some variants of the origin of the great vessels from the right or left ventricle with pulmonary stenosis, atresia of the tricuspid valve, atresia of the mitral valve, hypoplasia of the ventricles of the heart.
Abbreviations • PAVK - patent atrioventricular canal • TMS - transposition of the great vessels • TADPV - total anomalous drainage of the pulmonary veins.
ICD-10 • Q20 Congenital anomalies of the cardiac chambers and connections • Q21 Congenital anomalies of the cardiac septum • Q22 Congenital anomalies of the pulmonary and tricuspid valves • Q23 Congenital anomalies of the aortic and mitral valves • Q24 Other congenital anomalies of the heart.
How dangerous is the anomalous phenomenon?
Aneurysm of the interatrial septum
Knowing that over time, the weakened part of the interatrial septum will thin out even more, and the abnormal protrusion will increase in size, those patients who have been diagnosed with this disease begin to fear its rupture. Other types of aneurysms really threaten human life if their integrity is violated. In the case of an aneurysm of the interatrial septum, doctors say that everything is not so dangerous. The rupture will not seriously affect the work of the myocardium, much less lead to its stop. The fact is that the pressure of the blood flow in this particular segment of the organ is not so strong as to lead to fatal consequences. The only thing that forms at the site of the rupture is a defect, but patients live happily with it for many years.
With all this, the anomaly cannot be called harmless. The main problem is that an aneurysm located in the interatrial septum can lead to such a dangerous phenomenon as an embolic stroke. This is due to the fact that blood clots form in the bulging “bag”. If it ruptures, the particle can travel through the bloodstream to the brain, blocking a blood vessel and causing a stroke. Also, when an aneurysm ruptures, the blood clot threatens to enter not only the brain, but also other organs, provoking, for example, a renal infarction.
Classification
According to this international classification, ICD 10 code lists all existing heart defects.
There are quite a few of them. Conventionally, all defects can be divided into two groups, each of which has its own subgroups:
- White. Heart diseases in which mixing of venous and arterial blood does not occur.
- defect of the interatrial and interventricular septum;
- pathologies caused by depletion of the pulmonary circulation;
- defects associated with depletion of the systemic circulation;
- pathologies not associated with hemodynamic disorders.
- Blue. Venous and arterial blood mix.
- defects caused by enrichment of the small circle;
- pathologies caused by depletion of the small circle.
Each of the above groups and subgroups has its own specific code, which helps to determine the type of disease as accurately as possible.
Clinical picture of a dangerous condition
At the very beginning of its development, the anomaly is not accompanied by any signs and does not manifest itself. Further, its symptoms are most often associated with age:
- from 1 year to 3 years: attention should be paid to the appearance of some delay in the physical development of the baby; he may not have time to gain the required weight, or be too susceptible to viral infections;
- from 4 to 7 years: the child cannot withstand physical activity, complains of weakness, chest pain, and is stunted. Pallor of the skin and arrhythmias are observed;
- after 7 years: children of this age are also lagging behind in physical development; there may be a delay in the development of the reproductive system, chest pain. When listening, the doctor hears characteristic abnormalities: soft systolic murmurs.
- sudden chest pain;
- feeling of discomfort;
- increased weakness;
- inability to cope with any physical activity.
Hemodynamic disturbance
When these factors-causes are exposed and manifested in the fetus during development, characteristic disturbances occur in the form of incomplete or untimely closure of the membranes, underdevelopment of the ventricles and other anomalies.
Intrauterine development of the fetus is distinguished by the functioning of the ductus arteriosus and the oval window, which is in an open state. The defect is diagnosed when they still remain open.
The presented pathology is characterized by the absence of manifestations in intrauterine development. But after birth, characteristic disorders begin to appear.
Such phenomena are explained by the time of closure of the communication between the systemic and pulmonary circulation, individual characteristics and other defects. As a result, the pathology can make itself felt some time after birth.
Often, hemodynamic disorders are accompanied by respiratory infections and other concomitant diseases. For example, the presence of a pale type pathology, where arteriovenous discharge is noted, provokes the development of pulmonary hypertension, while a blue type pathology with a venoarterial shunt promotes hypoxemia.
The danger of the disease in question lies in the high mortality rate. Thus, a large discharge of blood from the pulmonary circulation, provoking heart failure, in half of the cases ends in the death of the baby before the age of one, which is preceded by the lack of timely surgical care.
The condition of a child over 1 year of age improves noticeably due to a decrease in the amount of blood entering the pulmonary circulation. But at this stage, sclerotic changes often develop in the vessels of the lungs, which gradually provokes pulmonary hypertension.
Symptoms appear depending on the type of anomaly, the nature and time of development of circulatory disorders. When the cyanotic form of the pathology develops in a sick child, a characteristic blueness of the skin and mucous membranes is noted, which increases its manifestation with each strain. The white defect is characterized by pallor, constantly cold hands and feet of the baby.
The baby himself with the presented disease differs from others in hyperexcitability. The baby refuses to breastfeed, and if he starts sucking, he quickly gets tired. Often, children with this pathology are diagnosed with tachycardia or arrhythmia; external manifestations include sweating, shortness of breath and pulsation of neck vessels.
In the case of a chronic disorder, the child lags behind his peers in weight, height, and there is a physical delay in development. As a rule, at the initial stage of diagnosis, a congenital heart defect is listened to, where heart rhythms are determined. In the further development of the pathology, edema, hepatomegaly and other characteristic symptoms are noted.
Complications include bacterial endocarditis, venous thrombosis, including cerebral thromboembolism, congestive pneumonia, angina syndrome and myocardial infarction.
Diagnostic procedures and treatment of abnormalities
Diagnosis of atrial septal aneurysm
To identify an anomaly, an ultrasound of the heart and an electrocardiogram are sufficient; a CT scan may also be needed. Simple diagnostics make it possible to identify an abnormal phenomenon immediately after the birth of a baby, and many women only learn about such an abnormality in their body during pregnancy through an ultrasound scan.
Only the attending physician can make a conclusion about whether it is necessary to treat an aneurysm of the interatrial septum and what kind of treatment, based on the diagnostic results. If a protrusion is detected that does not exceed 10 mm, then the patient can only be shown dynamic observation. If the anomaly exceeds the permissible norm, then maintenance drug therapy can be carried out (these can be drugs that lower blood pressure, thin the blood, improve metabolism).
If there is a threat of rupture of the aneurysm of the bladder or the development of pulmonary hypertension, a decision may be made to perform surgical intervention.
Source: medsosud.ru
Tests for diagnosis. Their essence
Diagnosis of a patent window can be made through ultrasound examination during routine examinations of the newborn. Sometimes pathology can be detected in the first year of life, but more often this is only possible with a thorough examination. In especially difficult cases, it is practiced in cardiology to use stress tests for patent oval window. They are carried out using a special technique, and the results obtained make it possible to more qualitatively and accurately assess the degree of disturbance of coronary blood flow, as well as determine the body’s ability to adapt.
The essence of stress tests is to take ECG readings not at rest, but at high load on the heart. An electrocardiogram in a calm state of the patient will show a normal result, but during physical activity ischemic changes may appear. To obtain an accurate picture of the state of the heart, readings are taken after intense walking or jogging on a treadmill with changes in the angle of inclination and speed of movement. Today in cardiology, tests on a bicycle ergometer are widely used - treadmill tests, which allow one to obtain information about the patient’s condition even during exercise. If no abnormalities in the functioning of the heart are detected, the test is considered negative. If there are signs of ischemic disease, the test is positive.
Aneurysm of the interatrial septum
Aneurysm of the interatrial septum is a fairly common pathology that occurs among children and adults. We are talking about the curvature of that same septum (protrusion) to one side. It is classified as a minor anomaly of the heart and is not considered too dangerous. In most cases, patients diagnosed with such a pathology are simply registered with a cardiologist, without responding to any treatment. But sometimes therapy is still required.
What is the essence of the disease
If we talk about aneurysm of the interatrial septum in children, then in this case it is congenital. At the time when the fetus is at the stage of intrauterine development, there is a small hole (window) in the interatrial septum. After the baby is born it closes. These are the normal indicators. But sometimes it happens that after closing the window, the thinnest part of the partition is formed in this area. Under the influence of blood flow, the latter begins to stretch and undergo curvature.
As for the reasons that could provoke the development of atrial aneurysm in a newborn, they have not been precisely studied. Factors that increase the likelihood of pathology include a hereditary predisposition to heart disease, insufficient supply of vitamins to the fetus during its development, exposure to negative external factors on the fetus, and infectious diseases that developed in a woman during pregnancy.
Considering the fact that in the case under consideration the anomaly does not manifest itself in any way and does not affect the functioning of the heart and its pumping function, then specific treatment is also often not required. The child will simply be registered with a cardiologist, systematically undergoing examination and examination. The doctor, assessing the patient’s condition, will be able to give recommendations that will need to be followed in the future.
Important! The decision on the advisability of treatment is made in each case separately. Everything will depend on the results of the ultrasound, which can be used to judge the size of the aneurysm. If they do not exceed 10 mm, then such a pathology is considered practically safe. If the indicators of septal bulge are greater, then the doctor will give separate recommendations for such a patient.
At-risk groups
A woman's poor nutritional status during pregnancy is a risk factor for a patent foramen ovale in the baby's heart.
A window remains open for many reasons. In addition to genetic inheritance, there are factors that contribute to the opening of the gap:
- Physical activity with a high load, this applies to weightlifters, divers or strength athletes
- Thromboembolism of the pulmonary artery, more often in patients with vascular occlusion of the lower extremities
- Dependence on bad habits during pregnancy
- Poor nutritional status of a woman while expecting a baby
- Severe toxin poisoning during pregnancy
- Premature birth
- Low immunity of women
- Harmful environmental conditions
Disease prevention
To prevent acquired heart disease, diseases that can cause damage to the heart valves are treated.
Most often, the acquired defect occurs due to rheumatism, so it is important to promptly identify and eliminate streptococcal infection.
Often, with rheumatism, patients are additionally prescribed prophylaxis with bicillin (a long-acting antibiotic): the drug is administered monthly for a year. Moreover, if there is a suspicion of a heart defect, such a patient is advised to undergo constant monitoring by a cardiologist.