What it is
EF is considered a common indicator that an ultrasound machine can provide. These data indicate the quality of the heart during contraction. During the entire process, the volume of blood that has left the left ventricle into the vascular bed is measured and removed as a percentage.
The measurement is taken in the left ventricle, from here the blood goes into the systemic circulation. When the indicator decreases, this indicates that the heart cannot contract at full strength and there is a lack of blood volume in the body. For minor violations, this situation can be corrected with medication .
Typically, studies are prescribed when the patient complains of shortness of breath, tachycardia, dizziness, fainting, fatigue, pain in the heart or behind the sternum, swelling of the extremities. A biochemical blood test and an electrocardiogram are initially indicated.
Sometimes, for a complete picture, Holter monitoring, bicycle ergometry or ultrasound are performed.
Cardiac ultrasound results: interpretation and analysis of the obtained indicators
Among modern research methods in cardiology, cardiac ultrasound occupies a special place. This highly informative diagnostic procedure can detect many diseases at the earliest stages. Interpretation of the results of ultrasound of the heart reflects its anatomical structure and functional state, and the obtained parameters are the basis for diagnosis.
The method is used without restrictions in any age groups, including newborns, because it does not have a negative effect on the body, is not invasive, and does not cause discomfort. The analysis of the results is carried out taking into account the age and gender of the patient, and the study is carried out using various methods.
What is cardiac ultrasound and what is its purpose?
Ultrasound examination is based on the property of different tissues to reflect ultra-high frequency sound waves differently. The waves come from the generator and the reflected ones are captured by a sensor, which transmits them to the converter, and an image of the heart and all its structures appears on the screen of the device.
The technique is constantly being improved. More accurate information is provided by the transesophageal scanning method , when the sensor is inserted as close as possible to the heart - into the esophagus. The screen reflects its anatomy in a 2-dimensional image with the exact parameters of individual structures.
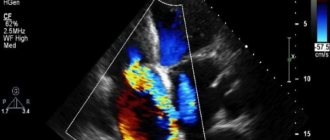
A new method that combines ultrasound with Doppler examination is Doppler echocardiography , which allows you to determine the condition of the coronary arteries, their filling with blood, identify circulatory disorders, and determine the most appropriate treatment method.
What pathology can be detected?
What can a heart ultrasound show in a child and an adult? The method includes the study of structural and functional parameters of the heart, changes in which can reveal the following pathology:
- hypertrophy (increase in size);
- change in organ configuration, which is typical for defects;
- various congenital defects (septal defects, hypertrophy, vascular anomalies and others);
- pathology of the heart valves (sclerosis, narrowing of the valve openings);
- tumors;
- dystrophic changes (myocardial dystrophy);
- inflammatory process (myocarditis, endocarditis, pericarditis);
- myocardial infarction - fresh and suffered in the past;
- cicatricial changes in the myocardium;
- pathology of large vessels (sclerosis of the aorta, pulmonary artery);
- the presence of blood clots in the atria;
- functional cardiac output failure;
- violation of coronary circulation (coronary heart disease).
In essence, an ultrasound examination provides an answer to the question of why a patient experiences this or that symptom, that is, it reveals its causes.
Indications for ultrasound diagnostics of the heart
Ultrasound scanning of the heart is prescribed in the following cases:
- with angina pectoris - pain in the heart during stress, physical activity;
- when there is pain behind the sternum;
- with repeated attacks of dizziness, fainting, loss of consciousness;
- if there is frequent tachycardia - palpitations;
- with interruptions in the heart area;
- when the ECG reveals extrasystoles and other rhythm disturbances, blockades;
- hypertensive patients with high blood pressure;
- when noises are heard on auscultation;
- newborns with suspected congenital heart disease;
- to monitor the dynamics of treatment after a heart attack, cardiac surgery;
- during a medical examination in persons over 40 years of age.
The procedure can be done not only in paid clinics, but also in government clinics for free if you have a compulsory medical insurance policy and a referral from a cardiologist, because it is included in the list of medical services paid from the federal budget.
Normal sizes of heart structures
There are single generally accepted averages for various cardiac parameters, approved by the World Health Organization, and they are developed taking into account age and gender. These are normal indicators, which are a guideline when deciphering an ultrasound of the heart, and are included in the program of the ultrasound scanner analyzer.
Indicators and their parameters in adults and children
Ultrasound parameters of a healthy heart and its individual structures in an adult, used in interpretation, are presented in the table:
| Name of heart parameter | Norm for men | Norm for women |
| LVMM—left ventricular myocardial mass | 135-180 g | 95-142 g |
| LVMI—left ventricular mass index | 71-92 g/m2 | 71-88 g/m2 |
| ESD – LV end-systolic size | 31-42 mm | 31-42 mm |
| EDV - end diastolic size | 46-58 mm | 45-58 mm |
| LV wall thickness in diastole | up to 11 mm | up to 10 mm |
| Blood ejection volume during LV systole | 60-100 ml | 60-100 ml |
| Wall thickness of the RV - right ventricle | 5 mm | 4.8-5 mm |
| LA size - left atrium | 18.5-33 mm | 17.5-33 mm |
| LA end-diastolic volume | 50-82 ml | 38-57 ml |
| RA end-diastolic volume - right atrium | 20-100 ml | 20-100 ml |
| Thickness of the IVS - interventricular septum in systole | 5-9.5 mm | 5-9.0 mm |
| IVS thickness in diastole | 7.5-11 mm | 7.5-11 mm |
| Aortic opening area | 20-35 mm2 | 20-35 mm2 |
| Thickness of the outer membrane of the pericardium | 1.2-1.7 mm | 1.2-1.7 mm |
| Volume of fluid in the pericardial cavity | 10-30 ml | 10-30 ml |
These are just the main indicators of ultrasound scanning; there are many other parameters of structure and function, the state of valves, blood vessels, depending on the characteristics of the research technique (in 2-dimensional or 3-dimensional format, Doppler ultrasound).
In children, due to the rapid growth and development of the body, the range of cardiac parameters is very variable. The standards for heart ultrasound criteria take into account the following age categories: newborns up to 1 month, every trimester of a baby’s life up to one year, children 1-3 years old, 3-6 years old, 6-10 years old, 10-14 years old. After 14 years, all parameters are assessed as in adults, with differences by gender.
The doctor explains in this video what are the benefits of undergoing an ultrasound.
Deviations from the norm
A change in certain ultrasound parameters in a patient, their deviation from the age norm indicates the presence of a certain type of cardiovascular pathology in the patient:
- thickening of the atria and an echo-negative area in the interatrial septum indicate the presence of a congenital defect in it;
- hypertrophy of the atria or ventricles, narrowing of the outgoing vessels and their abnormal location are signs of congenital combined heart disease;
- an increase in the size of the heart cavities and a decrease in systolic blood output indicates a dystrophic or inflammatory process in the myocardium;
- weak contraction of the myocardial area, the presence of scar tissue is a sign of a previous heart attack;
- thickening of the outer membrane and an increase in fluid content in its cavity indicates the presence of pericarditis;
- changes in the valves - surface unevenness, tears - signs of inflammation of the inner lining of the heart (endocarditis);
- the appearance of pain in the heart area during functional stress ultrasound indicates coronary heart disease;
- decreased blood flow and thickening of the walls of the arteries of the heart are a sign of coronary artery disease (CHD).
How are acquired defects determined by ultrasound?
Unlike congenital defects, these defects develop in the area of the heart valves and their openings after endocarditis. After healing of the inflamed endocardium, scar changes are formed, as a result of which the valve leaflets are deformed, shortened and do not completely close the opening during diastole.
The so-called regurgitation syndrome occurs - the return of blood through the gap between the affected valve and the walls of the hole.
The result is overfilling of the cavities of the heart, hypertrophy, gradual development of decompensation and heart failure.
If the valve is not replaced, the scar process progresses - the hole narrows, and a complex defect develops: valve insufficiency with stenosis of the hole.
This process can occur between the atria and ventricles on the right and left, at the point where the aorta originates from the left ventricle, at the point where the pulmonary artery exits from the right ventricle. All these phenomena are visualized on ultrasound: shortening of the valves, a decrease in the area of the holes, blood regurgitation, enlargement of the heart cavities, and a decrease in cardiac output.
Source: https://uzi.guru/grud-klet/serd/rezultaty-uzi-serdtsa-rasshifrovka.html
How is the emission rate calculated?
There is a calculation formula. To do this, stroke volume is multiplied by heart rate. This is how you get the desired value. The result will tell you how much volume is pushed out in one minute. In general, the normal figure should be approximately 5.5 liters.
Formulas for calculating ejection fraction
In medicine, they also use special programs that automatically calculate the fraction. For this, the Teicholz formula and Simpson method are used. Moreover, the data for these two calculations may differ by an average of 10%.
EF should be within 50-60%; the Simpson norm suggests that the lower limit should not be less than 45%, and Teicholz 55%.
The Teicholz formula uses systolic and diastolic volume and left ventricular size. A small part of the latter is involved in the study.
The overall length does not matter.
Typically, the study is carried out on old equipment and in the presence of areas with impaired local contractility (for example, in the case of ischemia), the Teicholz formula may fail and give an unclear result.
To obtain the EF indicator, the volume of shortening is multiplied by a factor of 1.7. The op-amp is obtained from the formula ((KDD – KSD)/KDD)*100%. Where EDD is the end diastolic diameter, ESD is the end systolic diameter.
Simpson's formula is more modern; it accurately shows all significant zones of the myocardium, taking into account the geometry of the ventricle and the presence of zones with impaired local contractility through the apical 4- and 2-chamber section.
The Simpson method involves dividing the left ventricular cavity into thin disks and determining their boundaries. The outlined systole and diastole are visible along the contour of the cardinal surface of the ventricle; from these data, an estimate of the ejection volume can be made.
Preparation for the procedure
No special preparation is required for cardiac echocardiography.
It is recommended to follow some important rules:
- On the eve of the procedure, limit the consumption of coffee and black tea.
- Avoid all types of alcoholic beverages several days before the test.
- Do not overwork, do not engage in physical exercise immediately before the ECHO ECG.
The procedure is carried out as follows:
- The patient needs to undress to the waist, freeing the chest;
- Lie down on a medical couch;
- A contact gel is applied to the chest for the procedure;
- Special sensors are located on the chest.
Children's cardiac ultrasound does not require special preparation for the study. For a cardiac ECHO, the only thing you need to do is make an appointment with the doctor and come at the appointed time. You need to have a diaper or a small towel with you to lay on the couch and wipe your chest from the contact gel used during the study to improve gliding and eliminate additional waves that create interference.
Standards for adults
The indicators do not depend on the gender of the patient, so the norms are identical for women and men. However, they may differ depending on age. The older a person is, the lower his standard.
An EF of less than 45% is considered reduced. At rates around 40%, heart failure can be suspected.
If in adults the level is less than 35%, then this indicates that violations are occurring and the person is in danger . With hypertension, the indicator may increase, at the same time, in some people it may be extremely low, which is determined by physiological predisposition, but not less than 45%.
PV can be calculated using the formula: ((KDO – KSO)/KDO)*100.
General characteristics
Echocardiography (EchoCG) is a method for studying morphological and functional changes in the heart and its valvular apparatus using ultrasound.
The echocardiographic research method allows:
- Quantitatively and qualitatively assess the functional state of the LV and RV.
- Assess regional LV contractility (for example, in patients with coronary artery disease).
- Assess LVMM and identify ultrasound signs of symmetric and asymmetric hypertrophy and dilatation of the ventricles and atria.
- Assess the condition of the valve apparatus (stenosis, insufficiency, valve prolapse, presence of vegetations on the valve leaflets, etc.).
- Assess the level of pressure in the PA and identify signs of pulmonary hypertension.
- Identify morphological changes in the pericardium and the presence of fluid in the pericardial cavity.
- Identify intracardiac formations (thrombi, tumors, additional chords, etc.).
- Assess morphological and functional changes in main and peripheral arteries and veins.
Indications for echocardiography:
- suspicion of acquired or congenital heart defects;
- auscultation of heart murmurs;
- febrile states of unknown cause;
- ECG changes;
- previous myocardial infarction;
- increased blood pressure;
- regular sports training;
- suspicion of a heart tumor;
- suspected thoracic aortic aneurysm.
Left ventricle
The main causes of local disturbances in LV myocardial contractility:
- Acute myocardial infarction (MI).
- Post-infarction cardiosclerosis.
- Transient painful and silent myocardial ischemia, including ischemia induced by functional stress tests.
- Constant ischemia of the myocardium, which has still retained its viability (the so-called “hibernating myocardium”).
- Dilated and hypertrophic cardiomyopathies, which are often also accompanied by uneven damage to the LV myocardium.
- Local disturbances of intraventricular conduction (blockade, WPW syndrome, etc.).
- Paradoxical movements of the IVS, for example, with volume overload of the RV or bundle branch blocks.
Right ventricle
The most common causes of impaired RV systolic function:
- Tricuspid valve insufficiency.
- Pulmonary heart.
- Stenosis of the left atrioventricular orifice (mitral stenosis).
- Atrial septal defects.
- Congenital heart defects accompanied by severe pulmonary arterial hydrangea (for example, VSD).
- PA valve insufficiency.
- Primary pulmonary hypertension.
- Acute right ventricular myocardial infarction.
- Arrhythmogenic pancreatic dysplasia, etc.
An increase in normal values is observed, for example, with some heart defects.
Right atrium
Only the value of the volumetric volume at rest is determined. A value of less than 20 ml indicates a decrease in EDV, a value of more than 100 ml indicates its increase, and an EDV of more than 300 ml occurs with a very significant increase in the right atrium.
Heart valves
Echocardiographic examination of the valve apparatus reveals:
- fusion of valve leaflets;
- insufficiency of one or another valve (including signs of regurgitation);
- dysfunction of the valve apparatus, in particular the papillary muscles, leading to the development of prolapse of the valves;
- the presence of vegetation on the valve flaps and other signs of damage.
The presence of 100 ml of fluid in the pericardial cavity indicates a small accumulation, and over 500 - a significant accumulation of fluid, which can lead to compression of the heart.
The concept of echocardiography literally translated from Greek means “echo” - echo, “cardio” - heart and “graphia” - to record or depict. Scientists from Sweden were the first to create and test a device for this study in the second half of the 20th century.
Echocardiography, like all other techniques based on the capabilities of ultrasound, is carried out by passing and reflecting wave oscillations with their subsequent recording. The principle of this diagnosis lies in the differences in density and ability to reflect ultrasound by different tissue structures, both healthy and pathologically altered.
There are several Echo-CG methods, and the appropriateness of prescribing one or another is determined by the doctor, based on the present symptoms and anatomical features of the patient. Thus, the main ones are transthoracic echocardiography (TTE) and transesophageal (TE) or transesophageal.
The first is the most preferable because it does not require preparation and is not accompanied by unpleasant sensations for the patient, and the second is most often prescribed if it is impossible to perform TTE.
In addition, recently, after the introduction of the Doppler effect into medical diagnostics, during Echo-CG it has been possible to study the quality and main characteristics of blood flow in the vessels of the heart and the surrounding area.
Doppler echocardiography involves changing the frequency of oscillations depending on the movement of the source propagating the waves. As the latter approaches, the frequency increases and the length decreases, and this is displayed in red on the screen. When deleted, accordingly, the changes are opposite and are marked in blue.
Considering the information content, simplicity and, in addition, low cost of echocardiography, anyone who has noted the above symptoms should think about visiting a doctor and undergoing an examination.
In addition, people with a hereditary predisposition, that is, whose close relatives have been diagnosed with heart disease, fall into the risk category. According to the recommendations of the Ministry of Health, men after 40 years of age and women after 45 years should undergo echocardiography at least once every 5 years, provided there are no pathological symptoms.
What studies are used to establish the indicator?
If the doctor suspects a heart disorder, he directs the patient to do a cardiogram and a biochemical blood test. Holter monitoring, electrocardiogram, bicycle ergometry and ultrasound examination of the organ can also be performed.
The indicator can be calculated using radiopaque or isotropic ventriculography, as well as using ultrasound of the heart. Most often, the latter method is chosen, as it is safe, informative and the cheapest.
Doctors study all indicators at once and judge the presence of pathology based on their total value. The main ones are the following:
- Cardiac output should be between 55 and 60%.
- The size of the right chamber atrium is 2.7-4.6 cm.
- The diameter of the aorta is 2.1-4.2 cm.
- The size of the left atrium is 1.8-4 cm.
- The normal stroke volume is 60-100 cm.
When is diagnosis necessary?
Echo-CG is widely used in cardiological diagnostics, as it allows to identify many heart pathologies, including congenital and acquired defects. The procedure will be prescribed if the patient has the following symptoms:
- pain of various types, localized in the chest area (especially on the left);
- general weakness, fatigue, shortness of breath even with minor physical exertion;
- dizziness, fainting or loss of consciousness (either a single episode or frequent);
- long-term dry cough not accompanied by colds;
- poor circulation, expressed in cold extremities, swelling (in the evening or throughout the day);
- rapid heartbeat or, conversely, freezing of the heart, irregular rhythm of its work;
- the presence of a heart murmur, as well as pathological changes in electrocardiogram parameters.
Ultrasound of the heart is mandatory and at certain intervals for patients with rheumatism, collagen diseases (for example, lupus erythematosus), etc. In most cases, the procedure makes it possible to establish the causes leading to attacks of tachycardia (increased heart rate).
In addition, echocardiography is used to monitor cardiac activity during the treatment of many diseases. There is a procedure for Echo-CG with Doppler, more about which you can read in this article.
Reasons for lowering the value
The indicator may be reduced in the following pathologies:
- Myocardial infarction. When scars appear on the muscles and they cannot contract properly. Moreover, after a heart attack, it is not possible to increase the fraction by medication.
- Ischemic disease. This reduces blood flow.
- Failure of rhythmic contractions. Leads to conduction disturbances and wear and tear of the heart.
- Cardiomyopathies. Causes an increase in muscle size.
Identifying pathology in the early stages and eliminating it through drug therapy can save the situation. If nothing has been done, then gradually the EF decreases even more.
This occurs due to the fact that the heart muscle begins to change, its layer grows, the structure of small blood vessels deteriorates, the fibers weaken and blood absorption decreases.
In addition, the causes of pathology may be hidden in:
- Angina pectoris.
- Hypertension.
- Pericarditis, endocarditis, myocarditis.
- Aneurysm of the ventricular walls.
- Congenital defects of an organ or blood vessels.
- Vasculitis.
There are predisposing factors that can also disrupt the functioning of the organ. These include obesity, tumors, severe intoxication, hormonal imbalance and diabetes.
Symptoms of a low rate
The main symptom when the fraction is reduced is the appearance of shortness of breath, regardless of the load. It can appear even due to minor stress when doing homework. Sometimes shortness of breath may occur at night or when lying down .
Among other signs, patients note:
- Increased weakness, fatigue and dizziness, up to loss of consciousness. This is due to a lack of blood supply and, as a result, oxygen starvation.
- The appearance of edema. This occurs due to fluid stagnation.
- Severe pain in the right side of the abdomen. This is noted due to congestion in the liver vessels, which can further provoke cirrhosis.
- Visual impairment.
- Pain in the heart area with increased contraction rhythm.
- Decreased sensitivity of the limbs.
- Loss of coordination.
- Nausea, vomiting.
How to increase the value of the indicator
First, the patient is diagnosed to identify the pathology that caused the decrease. Next, medications appropriate to the diagnosis are prescribed. For ischemia, the use of nitroglycerin is indicated; for hypertension, antihypertensive drugs and surgical correction of defects are prescribed.
In addition to treating the underlying disease, contractile function is stabilized with glycosides. These include Digoxin, Korglykon, Strophanthin.
To prevent the cardiovascular system from being overloaded with fluid, it is recommended to follow a diet, reduce salt and the volume of daily fluid.
At the same time, diuretics are indicated to help remove excess fluid: Veroshpiron, Diacarb, Diuver, Indapamide, Torasemide.
ATP inhibitors help strengthen blood vessels and thus protect the heart. When taken, tissue nutrition improves, the performance of the heart muscle and the resistance of the myocardium to stress increase. This group includes: Enalapril, Perindopril, Captopril.
Beta blockers help reduce the organ's need for oxygen and nutrients, increase the volume of areas of myocardial contraction, reduce cell death and heart rate. Their list includes: Nebivolol, Metoprolol, Bisoprolol.
Aldosterone receptor antagonists stabilize blood electrolyte levels, remove excess fluid, and reduce the load on the myocardium.
Representatives of the group are Spironolactone, Eplerenone. Angiotensin 2 receptor antagonists have a similar effect, but they are somewhat stronger. Valsartan, Candesartan, Olmesartan are prescribed.
When the ejection fraction is low, statins may be used as adjunctive therapy to lower cholesterol and protect blood vessels. Pravastatin, Fluvastatin, Simvastatin are used.
Anticoagulants are also effective, they thin the blood and prevent atherosclerotic changes. This is Warfarin, Xarelto.
Ventricular extrasystole
Ventricular extrasystole is a type of cardiac arrhythmia characterized by extraordinary, premature contractions of the ventricles.
Ventricular extrasystole is manifested by sensations of interruptions in the work of the heart, weakness, dizziness, anginal pain, and lack of air. The diagnosis of ventricular extrasystole is established on the basis of data from cardiac auscultation, ECG, and Holter monitoring.
In the treatment of ventricular extrasystole, sedatives, ß-blockers, and antiarrhythmic drugs are used.
Extrasystolic arrhythmias (extrasystoles) are the most common type of rhythm disturbances, occurring in different age groups. Taking into account the place of formation of the ectopic focus of excitation in cardiology, ventricular, atrioventricular and atrial extrasystoles are distinguished; Of these, ventricular ones are the most common (about 62%).
Ventricular extrasystole is caused by premature excitation of the myocardium in relation to the leading rhythm, emanating from the conduction system of the ventricles, mainly the branches of the His bundle and Purkinje fibers.
When recording an ECG, ventricular extrasystoles in the form of single extrasystoles are detected in approximately 5% of healthy young people, and with 24-hour ECG monitoring - in 50% of subjects.
The prevalence of ventricular extrasystole increases with age.
Ventricular extrasystole
Ventricular extrasystole can develop in connection with organic heart diseases or be idiopathic in nature.
Most often, the organic basis of ventricular extrasystole is ischemic heart disease; in patients with myocardial infarction it is recorded in 90-95% of cases.
The development of ventricular extrasystole may be accompanied by post-infarction cardiosclerosis, myocarditis, pericarditis, arterial hypertension, dilated or hypertrophic cardiomyopathy, chronic heart failure (CHF), cor pulmonale, and mitral valve prolapse.
Idiopathic (functional) ventricular extrasystole can be associated with smoking, stress, consumption of caffeine-containing drinks and alcohol, leading to increased activity of the sympathetic-adrenal system.
Ventricular extrasystole occurs in persons suffering from cervical osteochondrosis, neurocirculatory dystonia, and vagotonia. With increased activity of the parasympathetic nervous system, ventricular extrasystole can be observed at rest and disappear during physical activity.
Quite often, single ventricular extrasystoles occur in healthy individuals for no apparent reason.
Possible causes of ventricular extrasystole include iatrogenic factors: overdose of cardiac glycosides, use of ß-adrenergic stimulants, antiarrhythmic drugs, antidepressants, diuretics, etc.
Based on the results of daily ECG monitoring according to Holter, 6 classes of ventricular extrasystole were identified:
- class 0 – no ventricular extrasystoles;
- Class 1 – during any hour of monitoring, less than 30 single monomorphic (monotopic) ventricular extrasystoles are recorded;
- Class 2 – during any hour of monitoring, more than 30 frequent single monomorphic (monotopic) ventricular extrasystoles are recorded;
- Class 3 – polymorphic (polyfocal) ventricular extrasystoles are recorded;
- class 4a – monomorphic paired (2 at a time) ventricular extrasystoles are recorded;
- Class 4b – polymorphic paired ventricular extrasystoles are recorded.
- Class 5 – volley (group) polymorphic ventricular extrasystoles are recorded (3-5 in a row for 30 seconds), as well as episodes of paroxysmal ventricular tachycardia.
Class 1 ventricular extrasystoles do not manifest themselves clinically and are not accompanied by hemodynamic disturbances, therefore they are classified as functional. Ventricular extrasystoles of classes 2-5 are associated with an increased risk of developing ventricular fibrillation and sudden coronary death.
According to the prognostic classification of ventricular arrhythmias, there are:
- Benign ventricular arrhythmias – characterized by the absence of signs of organic heart damage and objective signs of left ventricular myocardial dysfunction; the risk of sudden cardiac death is minimal;
- ventricular arrhythmias of a potentially malignant course - characterized by the presence of ventricular extrasystoles against the background of organic heart lesions, a decrease in ejection fraction up to 30%; are accompanied by an increased risk of sudden cardiac death;
- ventricular arrhythmias of a malignant course - characterized by the presence of ventricular extrasystoles against the background of severe organic lesions of the heart; are accompanied by the highest risk of sudden cardiac death.
Subjective complaints with ventricular extrasystole may be absent or consist of sensations of “fading” of the heart, “interruptions” or “push” caused by increased post-extrasystolic contraction.
Ventricular extrasystole in the structure of vegetative-vascular dystonia occurs against the background of increased fatigue, irritability, dizziness, and periodic headaches.
Frequent extrasystoles that occur due to organic heart diseases can cause weakness, anginal pain, a feeling of lack of air, and fainting.
An objective examination reveals pronounced presystolic pulsation of the jugular veins, which occurs when the ventricles contract prematurely (venous Corrigan waves).
An arrhythmic arterial pulse with a long compensatory pause after an extraordinary pulse wave is determined. Auscultatory features of ventricular extrasystole are a change in the sonority of the first tone and splitting of the second tone.
The final diagnosis of ventricular extrasystole can be carried out only with the help of instrumental studies.
The main methods for detecting ventricular extrasystole are ECG and Holter ECG monitoring.
The electrocardiogram records the extraordinary premature appearance of an altered ventricular QRS complex, deformation and expansion of the extrasystolic complex (more than 0.12 sec.
); absence of P wave before extrasystole; complete compensatory pause after ventricular extrasystole, etc.
Carrying out a bicycle ergometry or treadmill test allows us to identify the relationship between the occurrence of rhythm disturbances and exercise: idiopathic ventricular extrasystole is usually suppressed by physical activity; the occurrence of ventricular extrasystoles in response to stress makes us think about the organic basis of rhythm disturbances.
If necessary, TEE, echocardiography, rhythmocardiography, sphygmography, and polycardiography are additionally performed.
Special treatment is not indicated for persons with asymptomatic ventricular extrasystole without signs of organic heart pathology. Patients are recommended to follow a diet enriched with potassium salts, eliminate provoking factors (smoking, drinking alcohol and strong coffee), and increase physical activity during physical inactivity.
In other cases, the goal of therapy is to eliminate symptoms associated with ventricular extrasystole and prevent life-threatening arrhythmias. Treatment begins with the prescription of sedatives (herbal medicines or small doses of tranquilizers) and ß-blockers (anaprilin, obzidan).
In most cases, these measures manage to achieve a good symptomatic effect, expressed in a decrease in the number of ventricular extrasystoles and the strength of post-extrasystolic contractions.
In case of existing bradycardia, relief of ventricular extrasystole can be achieved by prescribing anticholinergic drugs (belladonna alkaloids + phenobarbital, ergotoxin + belladonna extract, etc.).
In case of severe health problems and in cases of ineffectiveness of therapy with beta-blockers and sedatives, it is possible to use antiarrhythmic drugs (procainamide mexiletine, flecainide, amiodarone, sotalol). The selection of antiarrhythmic drugs is made by a cardiologist under the control of ECG and Holter monitoring.
With frequent ventricular extrasystole with an established arrhythmogenic focus and lack of effect from antiarrhythmic therapy, radiofrequency catheter ablation is indicated.
The course of ventricular extrasystole depends on its form, the presence of organic heart pathology and hemodynamic disorders. Functional ventricular extrasystoles do not pose a threat to life.
Meanwhile, ventricular extrasystole, developing against the background of organic heart damage, significantly increases the risk of sudden cardiac death due to the development of ventricular tachycardia and ventricular fibrillation.
Source: //www.KrasotaiMedicina.ru/diseases/zabolevanija_cardiology/ventricular-extrasystole
When is a high fraction value diagnosed?
An increase in the indicator is rare, since it is physiologically impossible. The heart cannot expel more blood than it should. Therefore, a level of 80% can occur in children at an early age, athletes and patients leading an active lifestyle.
Sometimes an increase indicates myocardial hypertrophy, when the left ventricle strives to compensate for the onset of CHF and pushes out blood with considerable force.
If the indicators are not normal, it is imperative to consult a cardiologist and undergo echocardioscopy to prevent the development of pathologies.
Consequences
If you do not pay attention to the problem, severe chronic heart failure develops. Moreover, the body experiences a lack of oxygen, since the blood is pushed out in insufficient quantities and does not carry all the necessary nutrients.
Oxygen starvation can lead to serious pathologies of both the heart and brain.
Health forecast
The prognosis depends on how low the indicator is diagnosed in the patient. When the value decreases to 40-45%, the risk of cardiac arrest is small, about 10-15%. When EF decreases to 34-39%, the possibility of death is within 20-25%.
If this indicator becomes even lower, the threat to life for the patient increases as the EF decreases.
It is not possible to completely get rid of the pathology, so patients with this diagnosis must constantly undergo corrective therapy, which will allow them to maintain their vital functions for many years.
Ejection fraction provides information about the performance of the left ventricle. In men and women, the norm is the same (55-70%), but in children the figure can reach 70-80%, which is not considered a pathology.
The most common is the low fraction. To raise the rate, it is necessary to find the cause of the pathology and organize adequate treatment. If this is not done, the patient is at risk of developing heart failure and death.
In physiology of the cardiovascular system, end-diastolic volume (EDV)
, this is the volume of blood in the right and/or left ventricle at the final moment of filling (diastole).
Since EDV is associated with stretching of the ventricle(s), EDV is often used as a synonym for preload, that is, the length of the cardiac muscle sarcomeres before contraction (systole). Increasing EDV increases preload on the heart and, through the Frank-Starling mechanism of the heart, increases the volume of blood pushed out of the ventricle(s) during systole (stroke volume). End-diastolic volume of the left ventricle (EDV)
- the volume of the cavities of the left ventricle at the end of diastole - 110-145 ml
Left ventricular end-systolic volume (LVES)
– the volume of the LV cavity at the end of systole is 40-65 ml. Stroke volume is the volume of blood expelled into systole in one contraction. UO=KDO-KSO (70-100 ml)
LV ejection fraction is the ratio of SV to EDV. Norm 50 -70%
Interpretation of ultrasound of the heart
A modern method of hardware diagnostics - echocardiography or ultrasound of the heart, is based on the use of oscillations of high-frequency sound waves.
Through ultrasound examination, a medical specialist determines the cause of functional failures in the organ, identifies changes in the anatomical structure and histological structure of tissues, and determines abnormalities in the vessels and valves of the heart. The prerogative aspects of ultrasound diagnostics are:
- absence of damage to the skin and penetration into the patient’s body (non-invasive);
- harmlessness. Ultrasonic waves are safe for health;
- information content. Clear visualization of the heart allows you to accurately determine the pathology;
- no contraindications to the use of the method;
- the ability to observe dynamic processes;
- relatively low cost of research;
- insignificant time costs for the procedure.
Ultrasound of the heart is performed by a doctor from the radiology department based on the direction and recommendation of a cardiologist. If you wish, you can go through the procedure yourself.
Purpose of the study
Indications for the procedure are patient complaints about certain symptoms:
- systematic pain in the chest area;
- difficulty breathing during physical activity;
- heart rhythm disturbances (usually rapid);
- swelling of the extremities not associated with kidney disease;
- persistently elevated blood pressure.
In addition, patients who have had a heart attack, suffer from hypertension, and chronic cardiac diseases need regular heart examinations.
Newborns are examined if developmental anomalies are suspected and if pathology is diagnosed during the perinatal period. The following cases may be a reason to check the heart function of a child: loss of consciousness for a short time, reluctance to suck milk from the breast for no apparent reason (cold, abdominal cramps), difficulty breathing with shortness of breath without signs of acute respiratory viral infection.
The list continues with systematically freezing hands and feet under normal temperature conditions, bluish discoloration (cyanosis) in the mouth, chin and nasolabial part of the face, rapid fatigue, pulsating veins in the right hypochondrium and neck, developmental abnormalities. A pediatrician may also recommend an examination if, when listening with a medical phonendoscope, an extraneous sound is detected during myocardial contractile activity.
The procedure for ultrasound examination of the heart in an infant requires the mandatory presence of parents
Children during puberty should undergo the procedure because the body experiences a sharp growth spurt and the heart muscle may lag. In this case, ultrasound is focused on assessing the adequate development of internal organs to the external data of a teenager.
Study parameters and possible diagnoses
Using ultrasound, the following are installed:
- sizes of the heart, ventricles and atria;
- thickness of the heart walls, tissue structure;
- the rhythm of the beats.
In the image, the doctor can record the presence of scars, tumors, and blood clots.
Echocardiography informs about the condition of the heart muscle (myocardium) and the outer connective tissue membrane of the heart (pericardium), examines the valve located between the left atrium and the ventricle (mitral).
Ultrasound with Dopplerography gives the doctor a complete picture of the condition of the vessels, the degree of their blockage, the intensity and volume of blood flow.
Information about the health of the heart and vascular system obtained from the study allows you to most accurately diagnose the following diseases:
How is coronary angiography done?
- impaired blood supply due to blockage of blood vessels (ischemia);
- necrosis of part of the heart muscle (myocardial infarction, and pre-infarction stage);
- stage of hypertension, hypotension;
- defect in the structure of the heart (congenital or acquired defect);
- clinical syndrome of chronic organ dysfunction (cardiac decompensation);
- valve dysfunction;
- heart rhythm failure (extrasystole, arrhythmia, angina pectoris, bradycardia);
- inflammatory tissue damage in the membranes of the heart (rheumatism);
- damage to the heart muscle (myocarditis) of inflammatory etiology;
- inflammation of the heart membrane (pericarditis);
- narrowing of the aortic lumen (stenosis);
- complex of symptoms of organ dysfunction (vegetative-vascular dystonia).
In order to determine the listed diseases, the doctor decodes the image of the cardiovascular system obtained on the monitor.
Through the ultrasound procedure of the heart, it is possible to analyze in detail the entire cardiac cycle - a period that consists of one contraction (systole) and one relaxation (diastole). Assuming that the normal heart rate is about 75 beats per minute, the duration of the cardiac cycle should be 0.8 seconds.
Decoding of echocardiography indicators is carried out sequentially. Each unit of the cardiac structure is described by the diagnostician in the study protocol.
This protocol is not a document with a final conclusion. The diagnosis is made by a cardiologist after a detailed analysis and comparison of protocol data.
Therefore, when comparing your ultrasound results and standards, you should not engage in self-diagnosis.
Normal ultrasound readings are an average value. The results are influenced by the gender and age category of the patient. Men and women have different indicators of the mass of the myocardium (muscle tissue of the heart) of the left ventricle, the index coefficient of this mass, and the volume of the ventricle.
For children, there are separate standards for the size, weight, volume, and functionality of the heart parts. However, they are different for boys and girls, for newborns and infants. For adolescents from the age of 14, indicators are compared against adult male and female standards.
Designation of the parts of the heart on an ultrasound image, the condition and size of which are assessed by an ophthalmologist
In the final protocol, the evaluation parameters are conventionally designated by the initial letters of their full names.
Parameters and standards for pediatric echocardiography
Interpretation of ultrasound of the heart and functions of the circulatory system of the newborn is carried out as follows:
- left atrium (LA) or interatrial septum diameter in girls/boys: 11–16 mm/12–17 mm, respectively;
- right ventricle (RV) in diameter: girls/boys – 5–23 mm/6–14 mm;
- final size of the left ventricle at relaxation (diastole): dev./small. – 16–21 mm/17–22 mm. Abbreviation in the LV CDR protocol;
- the final size of the left ventricle during contraction (systole) is the same for both sexes – 11–15 mm. In the protocol - LV DCS;
- posterior wall of the left ventricle in thickness: girl/small. – 2–4 mm/3–4 mm. Abbreviation – TZSLZH;
- intergastric septum thickness: girl/small. – 2–5 mm/3–6 mm. (MZhP);
- free wall of the pancreas – 0.2 cm–0.3 cm (in boys and girls);
- ejection fraction, that is, part of the blood that is ejected from the ventricle into the vessels at the time of cardiac contraction - 65–75%. Abbreviation FB;
- blood flow in the pulmonary artery valve at its speed is from 1.42 to 1.6 m/s.
Indicators of heart size and function for an infant correspond to the following standards:
| Study parameters | Girls | Boys |
| LDV (left ventricle) | 18–24 mm | 19–25 mm |
| LP in diameter | 12–17 mm | 13–18 mm |
| LV diameter | 5–13 mm | 6–14 mm |
| CSR (left ventricle) | from 12 to 17 mm | |
| posterior wall of the left ventricle in thickness | from 3 to 5 mm | |
| MZhP by thickness | from 3 to 6 mm | |
| Pancreatic wall thickness | from 2 to 3 mm | |
| blood flow in the pulmonary valve by speed | approximately 1.3 m/s |
Routine ultrasound of the heart for babies is performed for infants aged one month and one-year-old babies.
Standards for adults
Normal ultrasound readings in an adult should correspond to the following digital ranges:
- LV myocardial mass (left ventricle): men/women – 135–182 g/95–141 g, respectively;
- LV myocardial mass index: male – from 71 to 94 g/m2, female – from 71 to 89 g/m2;
- end diastolic size (EDS)/ESR (end systolic size): 46–57.1 mm/ 31–43 mm, respectively;
- LV wall thickness in relaxation (diastole) – up to 1.1 cm;
- blood ejection during contraction (FB) – 55–60%;
- the amount of blood pushed into the vessels - from 60 ml to 1/10 liter;
- Pancreas size index – from 0.75 to 1.25 cm/m2;
- pancreatic wall thickness – up to ½ cm;
- ECD of the pancreas: 0.95 cm–2.05 cm.
Normal ultrasound indicators for the IVS (intergastric septum) and atria:
- wall thickness in the diastolic phase – 7.5 mm–1.1 cm;
- maximum deviation at systolic moment is 5 mm–9.5 mm.
- final diastolic volume of the RA (right atrium) – from 20 ml to 1/10 liter;
- LA dimensions (left atrium) – 18.5–33 mm;
- LA size index – 1.45–2.9 cm/m2.
The aortic opening normally ranges from 25 to 35 mm2. A decrease in the indicator indicates stenosis. The heart valves should be free of tumors and deposits.
Valve performance is assessed by comparing normal sizes and possible deviations in four degrees: I – 2–3 mm; II – 3–6 mm; III – 6–9 mm; IV – over 9 mm.
These indicators determine how many millimeters the valve sags when the valves are closed.
Description of the operation of the heart valves in the ultrasound examination protocol - information that is deciphered by the treating cardiologist
The outer lining of the heart (pericardium) in a healthy state has no adhesions and does not contain fluid. The intensity of blood flow is determined during an additional examination to ultrasound - Dopplerography.
An ECG reads the electrostatic activity of heart rhythms and heart tissue. An ultrasound examination evaluates the speed of blood circulation, the structure and size of the organ. Ultrasound diagnostics, according to cardiologists, is a more reliable procedure for making the correct diagnosis.
Source: https://apkhleb.ru/uzi/rasshifrovka-serdca
Physiological properties of the heart (automaticity, conductivity, contractility, excitability)
Excitability –
this is the ability of the myocardium to be excited under the action of a stimulus,
conductivity
to conduct excitation,
contractility
to shorten when excited.
A special property is automation
. This is the ability of the heart to undergo spontaneous rerhythmic contractions that occur in the organ itself. Aristotle also wrote that the nature of the heart has the ability to beat from the very beginning of life to its end, without stopping. In the last century, there were 3 main theories of cardiac automaticity. Prohaska and Müller put forward a neurogenic theory, considering nerve impulses to be the cause of its rhythmic contractions. Gaskell and Engelman proposed the myogenic theory, according to which excitation impulses originate in the heart muscle itself. There was a theory of a heart hormone that is produced in it and initiates its contractions. Automaticity of the heart can be observed on an isolated heart according to Straub. In 1902, using this technique, Tomsk professor A.A. Kulyabko for the first time revived the human heart.
Automaticity of the heart
- this is the ability of the heart to contract rhythmically under the influence of impulses originating in itself.
Cardiac excitability
is the ability of the heart muscle to be excited by various stimuli of a physical or chemical nature, accompanied by changes in the physical and chemical properties of the tissue.
Cardiac conductivity
– carried out in the heart electrically due to the formation of an action potential in pacemaker cells. The place where excitation transfers from one cell to another is the nexus.
Cardiac contractility
– The force of contraction of the heart muscle is directly proportional to the initial length of the muscle fibers