Phlebectasia is a complex pathological disorder that affects the veins of the esophagus. Phlebectasia or varicose veins of the esophagus is a consequence of impaired blood flow into the vena cava. This in turn provokes an increase in the lumen of the vessels and their further protrusion in the form of sacs.
With this pathology, the membrane in the area of protrusion is often significantly thinned, inflamed and susceptible to erosion. The appearance of varicose hemorrhages is also possible. They, in turn, significantly complicate the diagnosis of the disease, since after heavy blood loss the veins collapse and become invisible.
Most often, varicose veins of the esophagus are observed in the distal or proximal part of the stomach. The pathology is caused by an increase in pressure in the portal-type venous system. This deviation is also characteristic of liver cirrhosis.
Important: Most often, grade 1 and grade 2 esophageal varicose veins occur in men whose age has crossed the line of 50 years. Before treatment, the patient must undergo a series of studies to make an accurate diagnosis and select the most rational treatment.
What can cause
Varicose veins are a rather complex phenomenon that is characterized by spontaneity. So, the disease can appear at the most unexpected moment. Congestion in the portal vein of the liver leads to the fact that internal hemorrhage can occur for a variety of reasons - during heavy lifting, with simple gastrointestinal diseases, with unstable febrile conditions.
Important: Internal varicose bleeding is manifested by a slight tickling in the throat and a metallic taste in the mouth. This is usually followed by nausea and vomiting. Vomiting blood is characterized by a bright scarlet color and the consistency resembles coffee grounds. With excessive blood loss, the patient experiences dizziness, weakness, malaise, and possible loss of consciousness.
The reasons for increased pressure in the portal vein of the liver may be associated with the following factors:
- cirrhosis of the liver;
- chronic hepatitis;
- various neoplasms;
- tuberculosis;
- thrombosis;
- cyst;
- adhesions;
- the presence of stones in the bile ducts;
- echinococcosis;
- peritonitis;
- adenopathy;
- portal vein thrombosis;
- angiomas;
- splenomegaly;
- Bunty syndrome;
- atrophic cirrhosis of Laennec;
- chronic lymphocytic leukemia.
The above problems can also cause dilation of the esophagus. Also, enlargement of the esophagus and its veins can be directly related to certain diseases of the stomach and pancreas. They can have a direct impact on hemodynamics in the superior vena cava.
Enlargement of the esophagus can appear regardless of a person’s age and gender. In this case, a problem that interferes with normal blood flow plays a role.
Symptoms
Dilatation of the esophagus, as well as dilated veins of the esophagus, are most often an advanced disease of the gastrointestinal tract. The initial period of development of the pathology is not characterized by an increased degree of activity. Thus, the disease most often develops asymptomatically, it does not cause any specific inconvenience, allowing a person to coexist normally.
The development of pathology occurs until bleeding begins. In this case, the disease manages to expand to large-scale forms. In this case, it makes sense to talk about grade 3 varicose veins.
Symptoms of VRP can sometimes appear as follows:
- heaviness in the chest;
- belching;
- esophagia and dysphagia;
- heartburn;
- malaise;
- weakness.
In some cases, a feeling of tightness may indicate the presence of a pre-mortem hemorrhage. So, according to statistics, 3 out of 5 deaths are observed with varicose veins. Most often, it turns out that all three cases of death were not subjected to sufficient research or sought help too late.
Diagnostics
Diagnostic tests are carried out to identify the cause of the disease and determine its extent. So, most often, with varicose veins of the esophagus, the following measures are suggested:
- fibroesophagoscopy - helps to identify the causes of bleeding, determines the degree of dilatation of the veins, the condition of the walls, and the presence of ruptures.
- X-ray of the esophagus - determines the nature of the dilation of the veins;
- laboratory tests - biochemistry, APTT, liver test;
- esophagoscopy.
Stage 1 and 2 illnesses are sometimes somewhat difficult to diagnose. This may well require additional research and analysis.
Important: The first trip to the doctor should take place immediately after the first suspicious symptoms are detected. If the doctor did not hospitalize you and prescribed a second appointment, then you cannot ignore it.
Patient examination plan
If you have symptoms of varicose veins of the esophagus or stomach, consultation with a phlebologist and gastroenterologist is required. The following studies need to be carried out:
- magnetic resonance imaging;
- Ultrasound of the esophagus;
- radiography;
- FGDS;
- blood tests.
An ultrasound can determine the condition of the liver and determine the cause of varicose veins. Using X-ray examination, the shape, relief and diameter of the esophagus are assessed. With varicose veins, narrowing and deformation are observed. The image reveals the convoluted folds of the organ and changes in contours. FGDS has the greatest diagnostic value.
This is an endoscopic examination in which a thin probe with a camera at the end is inserted into the esophagus and stomach through the mouth. The procedure is performed slowly so as not to injure the veins. During the examination, tuberosity of the esophageal mucosa and the presence of nodes are revealed. Laboratory tests are of little value. A blood test can reveal signs of inflammation and anemia.
Treatment
The patient should understand that treatment can only weaken some symptoms of the disease, but, alas, it is not yet possible to get rid of varicose veins completely; complete recovery of patients from varicose esophagus has not been observed in world medical practice.
The main emphasis in therapy is on preventive measures that can save the patient from the possible onset of bleeding. The main 3 principles of treatment are:
- Therapy aimed at eliminating the disease that led to varicose veins. This could be hepatitis, angina pectoris, cirrhosis of the liver, etc.);
- Adjusting the patient's lifestyle. Physical activity and fatigue (including emotional fatigue) are completely excluded from the patient’s daily routine; emphasis is placed on observing strict rules of personal hygiene;
- The patient must follow a diet. When prescribing therapeutic nutrition, the doctor focuses his attention on the disease that led to varicose veins. Based on this diagnosis, a specific table is assigned.
Medical therapy includes a number of medications that can be prescribed to the patient. Among them are 3 main types of drugs:
- Antacids are substances that help reduce the acidity of gastric juice;
- Vitamin substances;
- Astringents.
If the patient has suffered from blood loss, the doctor prescribes the following methods of maintaining the body:
- Transfusion of blood, red blood cells, plasma;
- Vasoconstrictor drugs;
- Drugs aimed at stopping bleeding;
- Inserting a probe into the esophageal tube to stop bleeding;
Application of thrombin or adhesive film to the affected areas.
The most optimal treatment method is surgery. It usually involves ligating the splenic artery, lining the veins, removing some vessels from the esophageal tube, and other procedures. Doctors also often use ligation of esophageal varices. Surgical treatment is more acceptable, since the mortality rate with this method of therapy is three times lower than in the case of conservative treatment.
Diagnosis of the disease
Diagnostic measures for patients with varicose veins are aimed at determining the cause of the pathology and its severity. The patient is examined as follows:
- First, the doctor collects the patient’s medical history—identifies his current condition, as well as the presence of chronic and hereditary diseases. Then he examines the patient, palpates and percusses.
- Next, the patient is prescribed a general blood test to determine the level of hemoglobin, red blood cells, platelets and leukocytes, and blood type. And a biochemical analysis to determine urea and creatinine, which characterize the functioning of the kidneys, as well as aminotransferases, which are responsible for the condition of the liver.
- In addition, a coagulogram is prescribed to determine blood clotting.
- Ascitic fluid is taken for analysis.
In addition to laboratory research methods, instrumental ones are also prescribed. Among them:
- X-ray of the sternum. It will show the contours of the esophagus, the quality of the mucous membrane and the accumulation of venous nodes.
- EFGDS. For examination, a thin tube with an endoscope is inserted into the patient through the mouth and the condition of the upper gastrointestinal tract is examined.
- Capsule endoscopy. A rare but very effective method. To carry it out, the patient swallows a capsule containing a small video camera inside. This allows the doctor to carefully examine the condition of the gastrointestinal tract.
- Computed tomography of the abdominal cavity.
- Dopplerography of the portal and splenic veins.
Who to contact
If bleeding occurs, you should never wait until you go to the doctor on your own. The patient should call an ambulance as soon as possible. Ambulance doctors will urgently transport the patient to a surgical hospital. After bleeding stops in the hospital, the patient will need long-term treatment and observation by a gastroenterologist or hepatologist. Sometimes the patient may be sent to a cardiologist. This is possible if the patient suffers from cardiac cirrhosis resulting from a severe form of heart failure.
Clinical picture
Phlebectasia develops individually, and the course directly depends on the presence of concomitant disorders and the cause. In certain cases, the pathology can be characterized by rapid development and pronounced symptoms. The main manifestations of the disease include:
- heartburn;
- belching;
- difficulty swallowing food;
- discomfort in the chest area;
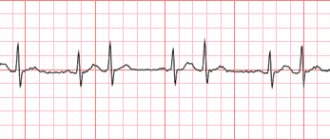
- increased heart rate;
- bleeding, which manifests itself as the presence of blood in the stool.
At stage 1 of the development of esophageal varicose veins, signs may not appear, and the disease may proceed secretly. Moreover, the earlier the symptoms were detected and treatment started, the greater the patient’s chances of improving the condition.
Forecast
The prognosis for curing varicose veins cannot be positive. Medicine still does not know how it is possible to rid a patient of this disease forever. However, in most cases it is possible to make the patient’s life easier. To do this, you just need to seek medical help immediately after detecting alarming symptoms. Adequate treatment in such a situation can alleviate the symptoms of the disease and prevent blood loss.
Medical practice and observations of people around the world indicate rather unpleasant statistics. So, for more than 50% of patients with already existing bleeding from the veins of the esophagus, this disease ends in death. Most patients who survive blood loss experience a relapse. Usually the interval before relapse of the disease is 1-2 years.
Due to the particular severity of varicose veins, long-term life for the patient is almost impossible. Frequent relapses of hemorrhages and weakening of the patient’s entire body also make their mark. A favorable prognosis is only possible if the patient goes to the clinic on time and avoids possible bleeding.
Diet
Patients with phlebectasis should follow a special diet. Experts recommend eating 4-6 times a day. It is important that the last meal is taken no later than 3-4 hours before bedtime. The temperature of all dishes should not be too low or too high.
In order to prevent acidic fluid from the stomach from entering the esophagus, the head of the bed should be raised by at least 10 centimeters.
You can also help your body by eating right.
. While eating, there is no need to be distracted by talking or watching TV.
Experts recommend drinking about two liters of liquid per day. Patients need to give up strong black tea, confectionery, sweets, alcohol, coffee and baked goods.
Dietary nutrition must be combined with physical therapy. Daily exercise will help restore blood circulation and prevent blood clots.
Complications
Bleeding from esophageal varices is the most common complication of the disease. Bleeding can occur due to severe physical exertion, including bending forward, as well as due to overeating. Bleeding that occurs during sleep is also often considered.
Blood can come out almost imperceptibly, but there are also cases when the blood loss is so great that it poses a threat to the patient’s life and requires immediate hospitalization.
Even in situations where blood loss is insignificant, such a symptom can pose a health threat. With frequent but mild blood loss, anemia and iron deficiency may appear. This leads to weight loss, weakness and fatigue. A characteristic sign indicating bleeding is the symptom of vomiting mixed with scarlet clots.
Thus, varicose veins of the esophagus have complications that are quite dangerous for human health. If alarming signs are detected, you must immediately contact the clinic and undergo all necessary diagnostic measures.
Treatment options
The therapeutic effect to eliminate the risk of bleeding in case of damage to the veins of the esophagus and stomach should take into account the stage of the pathological process, the general health of the patient, and the susceptibility of his body to the therapeutic effect. Modern medicine is constantly improving methods of influencing the veins of the esophagus, which makes it possible to quickly eliminate the most obvious manifestations of the pathology in question.
Today, an integrated approach is used in the treatment of the considered pathology of the veins of the esophagus and stomach, which consists of traditional, surgical and medicinal methods of influence. Each method has its own characteristics, can be used for certain indications and is prescribed by a doctor. The progress of treatment should be monitored at all stages by the attending physician, who, if necessary, will promptly make the necessary adjustments and prevent possible risks of complications.
Traditional method
First of all, when using the traditional treatment option for varicose veins of the esophagus, bleeding is stopped, which can cause death. This will also allow for additional therapeutic methods that will ensure faster regeneration of damaged tissue and create the necessary scar at the site of damage to the esophageal vein.
In order to compensate for hypovolemia and prevent the occurrence of hemorrhagic shock, a significant (calculated by the doctor) dose of vitamin K is introduced into the patient’s body, as well as an infusion of frozen plasma (1-2 doses, intravenous transfusion is performed).
In parallel with endoscopic hemostasis, ocreotide is administered, which is a synthetic analogue of the drug somatostatin. With its help, therapy is carried out to increase visceral pressure and resistance, which causes an active release of visceral vasidilator hormones. This drug is more preferable in comparison with the proposed analogues, since it has fewer possible side complications for the patient’s health.
Conservative method
In case of severe bleeding, which becomes a real danger to the patient’s life, a rubber inflating probe can be used to quickly stop the bleeding. Using a probe, pressure is applied to the bleeding vessel, which stops the movement of blood. For example, a probe of such a device, the Sengstaken-Blackmore probe, is popular in eliminating bleeding during the development of varicose veins in the digestive organs, in particular the esophagus. Corrugated varieties of such probes are also used, which are widely used in the treatment of esophageal varices during bleeding and bleeding gastric ulcers.
When a probe is inserted below the site of a vein breakthrough, the esophagus can be washed with hot water at a temperature of 40°C - this measure often helps stop active bleeding and stabilize the patient’s condition. However, in case of repeated bleeding and with its high intensity, in parallel with the use of probes, it is recommended to carry out intravenous and intramuscular administration of substances that also help stop the bleeding. Calcium chloride 10-20 ml is administered intravenously, Vicasol is administered intramuscularly. Do not administer drugs that act to increase blood pressure.
Treatment with an endoscope
Since this disease of the esophageal veins is most often diagnosed during endoscopic examination, endoscopic hemostasis can be prescribed to eliminate the most characteristic manifestations of the lesion (eliminate bleeding). This method involves suturing the affected areas of the veins in the esophagus, and it is this therapeutic option that is preferable in comparison with injection sclerotherapy due to the more pronounced positive dynamics of the treatment.
Endoscopic treatment results in rapid stopping of bleeding and prevention of possible relapses of the disease. Octreotide, used in the endoscopic treatment of bleeding from varicose veins of the esophagus and stomach, is administered intravenously at a dose of 50 mcg; its action is aimed at increasing visceral vascular resistance, which allows stabilizing the patient’s condition and preventing excessive blood loss. This drug is preferable to other drugs that may be prescribed to stop venous bleeding from the esophagus, since it has fewer possible side effects, even with long-term use.
The use of an endoscope involves the use of a special endoscopic examination of the esophagus, which is most often prescribed for bleeding, the cause of which is unclear. This technique is very popular due to the high efficiency of this diagnostic method and the good positive dynamics of treatment (ligation is performed) carried out using an endoscope. Endoscopic examination of the veins of the esophagus and stomach has shown itself well at any stage of development of the pathological process; This method also makes it possible to identify even the initial manifestations of diseases of the digestive system in relation to blood circulation in the veins and to identify varicose veins of the esophagus.
Use of balloon tamponade
The endoscopic technique also involves the use of an option to stop bleeding from the veins of the esophagus, such as balloon tamponade. It consists of applying special tamponing agents to the site of damage to the vein. However, in case of severe bleeding, balloon tamponade may not be very effective; additional medications should be used to stimulate regenerative processes in the tissues of the vein walls.
The classification, which is currently proposed for the division of varicose veins of the esophagus, allows us to determine the most effective treatment regimen. Taking into account the characteristics of the stage of the current pathological process, the body’s perception of the medications used and control of the treatment provided allows the attending physician to make timely adjustments and achieve the best results in stopping bleeding and stabilizing the patient’s condition.
Surgical intervention
Heavy bleeding, which poses a danger to the patient's life due to significant blood loss, may require surgery.
Surgical intervention may be prescribed for large blood losses, in which intravenous administration of plasma, blood and blood substitute fluids does not bring a significant positive result. There are several types of surgery for significant blood loss. Each of them is prescribed according to its own indications, determined by the doctor.
Today, the following types of surgical intervention are recognized as the most effective:
- application of a special bandage made of medical rubber. This ligation of damaged veins allows you to quickly stop blood circulation and stop blood loss, which can cause a significant deterioration in the patient’s condition;
- Carrying out an operation such as bypass surgery leads to a decrease in blood pressure in the veins and, as a result, stops bleeding. When performing bypass surgery, the liver tissue is affected; a special stent is inserted into the middle of this organ, which creates a kind of bridge between the liver tissues and the tissues of the esophagus, which lowers blood pressure. The hepatic and portal veins, having such a “bridge,” receive reduced pressure, which leads to stopping bleeding;
- Splenorenal shunting is a type of shunting operation that helps prevent possible bleeding when varicose veins are detected in the tissues of the esophagus and stomach.
The listed surgical options can eliminate high blood pressure in the veins of the esophagus damaged by varicose veins. All of them are carried out under the control of x-rays and provide the greatest positive effect from manipulations to stop bleeding.
Drug treatment of varicose veins
There is also the option of medicinal effects on the body in order to treat the initial stage of varicose veins of the esophagus. The choice of the type of medication is determined by the doctor after conducting an examination of the patient’s body and determining the stage of the current pathological process. When carrying out this type of therapy, indicators such as the patient’s body’s susceptibility to the drug used and the likelihood of developing allergic reactions must be taken into account.
The following medications with a pronounced effect on the veins are most often used in the treatment of this disease:
- "Vasopressin", which ensures rapid restoration of the normal lumen of narrowed veins. And this ensures better blood circulation in the tissues of the organ, preventing bleeding;
- a drug with nitrate, which contains the drug “Nitroglycerin”. It is prescribed to reduce high pressure in the veins of the esophagus;
- "Octreotide" - with its help you can quickly reduce pressure in the veins and restore the normal state of dilated blood vessels.
The listed medications have a number of possible side effects that should be taken into account when prescribing them.
Treatment with folk remedies
The reliability of drugs and methods of traditional medicine has been tested for centuries, but its effectiveness is not high enough to independently cope with the manifestations of varicose veins of the esophagus. Traditional medicine can be used as a maintenance drug to increase the speed of restoration processes in the tissues of the veins. For example, if there is a high probability of bleeding, it is recommended to take orally decoctions and infusions of herbs that have a hemostatic effect. These can be collections of stinging nettle, thyme, and knotweed.
Treatment with folk remedies is also possible at home, which is especially important during maintenance therapy of the disease, at the stage of remission. Since esophageal varicose veins are a serious lesion that poses a serious threat to the health and life of the patient, it is necessary to take into account the degree of exposure of the chosen traditional medicine. Treatment at home is carried out under constant medical supervision.
Do I need a diet?
When diagnosing varicose veins in the digestive organs, the question of choosing a diet should be considered one of the most important, since both his well-being and the performance of the therapeutic effect largely depend on the food entering the patient’s body. The diet, which is recommended for varicose veins of the esophagus, involves the observance of several feasible rules, which involve the exclusion of certain foods and the inclusion in the daily menu of certain products that heal the body in general and the esophagus in particular.
A diet for varicose veins of the esophagus should exclude the following foods and substances from the patient’s diet:
- seasonings;
- a large amount of table salt;
- excessive amounts of oils, especially of animal origin;
- fried, canned, smoked food, which will irritate the tissue of the esophagus and can cause bleeding.
Nutrition for varicose veins of the esophageal tissue, as well as for cirrhosis of the liver, should include more boiled and stewed foods; fermented milk products will perfectly support the necessary microflora in the intestines, without creating an excessive load on the digestive system as a whole. Fractional nutrition in small portions, controlling the number of calories to prevent excessive impact on the digestive system will prevent the worsening of existing pathology and maintain the health of the esophagus.