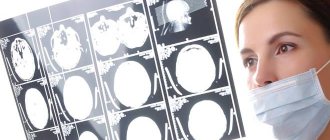
MRI signs of dyscirculatory encephalopathy
If the above symptoms occur, you should immediately contact a neurologist, who will refer you for additional instrumental studies. During an MRI, the doctor may suspect the presence of dyscirculatory changes based on specific MRI signs:
- vascular hypotensive inclusions;
- signs of hydrocephalus;
- the presence of calcifications (atherosclerotic plaques);
- narrowing or blockage of vertebral, basilar, carotid vessels.
CT signs
Computed tomography helps determine the extent of brain damage. Pathological changes in the organ on a CT image appear as areas of low density. These may be the consequences of a cerebral infarction (incomplete type), foci of ischemic damage, or cysts of post-stroke origin. A CT scan is performed to refute or confirm the diagnosis of DEP. Criteria that confirm the presence of pathology:
- expansion of the ventricles of the brain and subarachnoid space;
- the phenomenon of “leukoaraiosis” in the subcortical and periventricular layer;
- lesions in the gray and white medulla, which are represented by post-ischemic cysts and lacunar strokes.
Diagnostics
Only a neurologist can diagnose the disease. To make a diagnosis, an examination of the neurological status requires the presence of revived reflexes, the presence of oral automatism reflexes, pathological reflexes, changes when performing coordination tests, and signs of disturbance of the vestibular apparatus. You should also pay attention to the presence of nystagmus, deviation of the tongue away from the midline and some other specific signs that indicate the suffering of the cerebral cortex and a decrease in its inhibitory effect on the spinal cord and reflex sphere.
Types of disease
Depending on the cause of the disease, there are several types of vascular insufficiency of the brain:
- venous encephalopathy (impaired venous outflow of blood);
- hypertensive angioencephalopathy (damage to subcortical structures and white matter);
- discirculatory leukoencephalopathy of the brain (diffuse vascular damage against the background of persistent arterial hypertension);
- atherosclerotic encephalopathy (impaired arterial patency due to atherosclerosis);
- encephalopathy of mixed origin.
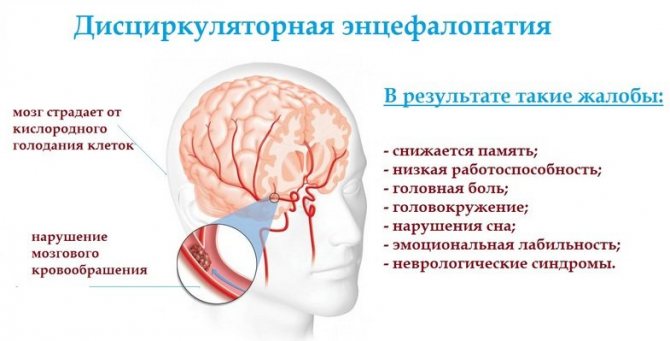
As a result of a decrease in blood supply to the brain for the above reasons, hypoxia occurs - a chronic lack of oxygen in brain cells.
Under conditions of oxygen starvation, especially sensitive nerve cells of the brain die, and in their place there remain pockets of rarefaction - essentially voids, they are called silent infarctions.
The cells of the white matter and subcortex die first.
Connections between different parts of the brain are disrupted and gradually disappear, which is why disorders of thinking, memory, and emotional stability begin.
Then the structures responsible for coordinating movements change.
As a result, a persistent neurological disorder develops – dyscirculatory encephalopathy.
Causes
Neuropathologists and vascular surgeons distinguish two groups of provoking factors:
- congenital abnormalities of cerebral vessels. Aneurysms, anastomoses, fusion of walls, dissection of arteries and veins of the head may well occur even in a child. There is no way to prevent this;
- acquired defects of the circulatory system. This includes diseases of the cardiovascular and endocrine systems, as well as injuries, such as concussion or concussion.
Among the acquired causes, atherosclerosis leads. High levels of cholesterol in the blood provoke the formation of fatty plaques. They attach to the endothelium (the inner layer of the blood vessel), narrowing its lumen, increasing the pressure in a separate part of the system. Over time, these abnormalities and atherosclerotic plaque lead to inflammatory processes in the artery. Inflammation develops at the site of attachment of the fatty deposit, and the normal elastic tissue of the artery is replaced by scar.
( Video : “Dyscirculatory encephalopathy: “Pro” and “Contra”. Approaches to diagnosis and therapy.”)
In second place among the causes is inflammation of blood vessels. The disease is rare and appears due to bacterial, infectious infection, severe allergic reaction, after poisoning with heavy metals or chemicals.
Next comes arterial hypertension. Chronic high blood pressure puts a strain on the blood vessels of the whole body. Due to overstrain, they become inflamed, stratified, forming circulatory pathologies.
Neuropathologists have established a connection between osteochondrosis of the cervical spine and DEG. Disruption of the transmission of nerve impulses and inflammation in the cervical-collar area negatively affect the outflow of venous blood from the head and increase intracranial and intraocular pressure.
Encephalopathy is often caused by blood diseases, blood clotting disorders, and thrombosis. The quality of blood circulation is directly affected by hormonal levels. Taking medications or contraceptives in violation of doctor's recommendations or for a longer period of time causes blood thickening and increases the risk of blood clots.
Prevalence
Sad statistics provide disappointing data - approximately 6% of the world population is diagnosed with DEP.
Among population groups, persons suffering from stage 2 DEP were identified among 35-55 year old citizens. The likelihood of developing DEP increases many times in older people over 60 years of age.
A correlation between the disease and profession was discovered - a larger number of cases were among people engaged in mental work. This is also due to the forced position of the body, lack of physical activity during the day - and, as a consequence, the development of cervical osteochondrosis, which provokes DEP.
For the most part, the disease affects older people.
The absolute absence of any treatment contributes to its slow progression, and ultimately leads to such deadly complications as stroke.
In grade 2, in contrast to grade 1, motor dysfunction and deterioration in adaptation to society are more clearly manifested.
Stages
There are three stages of vascular encephalopathy:
- Stage 1 DEP involves minor brain damage that can easily be confused with symptoms of other diseases. When diagnosed at this stage, stable remission can be achieved. The first degree is expressed by the following symptoms: noises in the head, dizziness, sleep disturbance, and the appearance of instability when walking.
- Degree 2 DEP is characterized by the patient’s attempts to blame other people for his failures, but this condition is often preceded by a time of strict self-control. The second stage of dyscirculatory changes in the brain is represented by the following symptoms: severe memory loss, impaired control of actions, depression, seizures, increased irritability. Although this degree of dyscyclic state suggests the presence of disability, the patient still retains the ability to care for himself.
- DEP grade 3 (decompensation) is the transition of pathology to the form of vascular dementia, when the patient has severe dementia. The third stage assumes that the patient has urinary incontinence, parkinsonism, disinhibition, and coordination disorders. A person is completely dependent on others and needs constant care and supervision.
Stage II-III dyscirculatory encephalopathy is characterized by an increase in cognitive and motor impairment. There is a significant deterioration in memory, lack of attentiveness, intellectual decline, and severe difficulties when it is necessary to perform previously feasible mental work. At the same time, patients with DEP themselves are not able to adequately assess their condition and overestimate their performance and intellectual capabilities. Over time, patients with discirculatory encephalopathy lose the ability to generalize and develop a program of action, and begin to have poor orientation in time and place. In the third stage of discirculatory encephalopathy, pronounced disturbances in thinking and praxis, personality disorders and behavior are noted. Dementia develops. Patients lose the ability to work, and with deeper impairments, they also lose self-care skills.
Of the disorders of the emotional sphere, discirculatory encephalopathy of later stages is most often accompanied by apathy. There is a loss of interest in previous hobbies, a lack of motivation for any activity. With stage III dyscirculatory encephalopathy, patients may be engaged in some unproductive activity, and more often they do nothing at all. They are indifferent to themselves and the events happening around them.
Movement disorders that are barely noticeable in stage I of dyscirculatory encephalopathy later become obvious to others. Typical of DEP are slow walking with small steps, accompanied by shuffling due to the fact that the patient is unable to lift the foot off the floor. This shuffling gait in dyscirculatory encephalopathy is called the “skier’s gait.” It is typical that when walking, a patient with DEP finds it difficult to start moving forward and also difficult to stop. These manifestations, as well as the gait of a patient with DEP, have significant similarities with the clinical picture of Parkinson’s disease, but unlike it, they are not accompanied by motor disorders in the hands. In this regard, clinical manifestations of dyscirculatory encephalopathy similar to parkinsonism are called by clinicians “parkinsonism of the lower body” or “vascular parkinsonism”.
In stage III DEP, symptoms of oral automatism, severe speech impairment, tremors, paresis, pseudobulbar syndrome, and urinary incontinence are observed. Epileptic seizures may occur. Often discirculatory encephalopathy of stage II-III is accompanied by falls when walking, especially when stopping or turning. Such falls can result in limb fractures, especially when DEP is combined with osteoporosis.
Classification
According to etiology, dyscirculatory encephalopathy is divided into hypertensive, atherosclerotic, venous and mixed. According to the nature of the course, there are slowly progressive (classical), remitting and rapidly progressing (galloping) discirculatory encephalopathy.
Depending on the severity of clinical manifestations, dyscirculatory encephalopathy is classified into stages. Stage I dyscirculatory encephalopathy is characterized by the subjectivity of most manifestations, mild cognitive impairment and the absence of changes in neurological status. Stage II discirculatory encephalopathy is characterized by obvious cognitive and motor disorders, aggravated disturbances in the emotional sphere. Stage III dyscirculatory encephalopathy is essentially vascular dementia of varying severity, accompanied by various motor and mental disorders.
There are several key types of dyscirculatory encephalopathy of the 2nd degree, differing in the specific course and symptoms:
- The most common type of stage 2 DEP is atherosclerotic.
The reason is banal and scary in the scale of its occurrence - blockage of cerebral vessels with atherosclerotic plaques, impeding blood flow and normal processes of brain activity.
- The second most common type is hypertensive
It appears in both young and elderly patients. It often develops to a severe form in a short period of time. The main symptom is an abrupt, acute increase in blood pressure to high numbers. Characteristic changes in psycho-emotional state such as apathy and lethargy.
- The third type is venous encephalopathy.
The reason lies in the obstructed outflow of blood from the brain through the veins, this leads to effusion of the liquid phase of blood into the tissue surrounding the vessels of the brain and its swelling. Chronic stagnation of venous blood provokes worsening of DEP.
- Mixed type.
This form combines the features of all three forms described above. Symptoms are changeable, which is why the attending physician may have some difficulties in making a diagnosis.
Common symptoms include vomiting, incoordination, decreased attention, poor and sluggish thinking, mood instability, fundus changes, and memory loss.
A disease such as DEP implies the presence of a number of syndromes:
- Vestibular coordination syndrome - this syndrome is characterized by a disruption in the functioning of the vestibular apparatus, which is responsible for the normal coordination of movements and spatial sensation.
- Dissomnia syndrome – sleep disturbances in all manifestations.
- Cephalgic syndrome literally means a severe headache, as well as the presence of ringing, noise in the ears, and sometimes vomiting.
- Cognitive syndrome - implies a disorder of thinking, especially pronounced after active mental work, more often in the evening.
Diagnostics
Only a neurologist can diagnose the disease. To make a diagnosis, an examination of the neurological status requires the presence of revived reflexes, the presence of oral automatism reflexes, pathological reflexes, changes when performing coordination tests, and signs of disturbance of the vestibular apparatus. You should also pay attention to the presence of nystagmus, deviation of the tongue away from the midline and some other specific signs that indicate the suffering of the cerebral cortex and a decrease in its inhibitory effect on the spinal cord and reflex sphere.
Treatment of dyscirculatory encephalopathy of the brain
Therapy for patients with DEP includes measures aimed at correcting vascular pathology of the brain, preventing relapses, improving blood circulation and normalizing impaired brain function. Basic principles of complex treatment:
- reduction of excess body weight;
- avoiding consumption of saturated fats;
- limiting the consumption of table salt to 4 g/day;
- prescription of regular physical activity;
- giving up alcohol and smoking.
Standards of treatment
If lifestyle correction is ineffective, the standard of treatment in neurology involves prescribing medications that lower blood pressure, suppress the manifestations of atherosclerosis, and drugs that act on brain neurons. When drug therapy does not help eliminate or slow down the development of encephalopathy, surgical intervention is performed on the walls of the main cerebral vessels.
Due to the difficulty of diagnosis, treatment of vascular encephalopathy often begins from the second stage, when cognitive impairment is no longer in doubt. For the purpose of pathogenetic therapy of dyscirculatory changes in the brain, medications belonging to different groups are prescribed:
- Angiotensin-converting enzyme inhibitors. Indicated for patients with hypertension, diabetes mellitus, atherosclerosis of the renal arteries, and heart failure.
- Beta blockers. These drugs lower blood pressure and help restore cardiac function.
- Calcium antagonists. They cause a hypotensive effect and help normalize heart rate. In elderly patients, cognitive impairment and movement disorders are eliminated.
- Diuretics. Designed to reduce blood pressure by reducing the volume of circulating blood and removing excess fluid.
Lifestyle
Correcting the lifestyle of a patient with DEP involves:
- Bringing body weight to optimal values;
- Proper nutrition;
- Elimination of alcohol and smoking;
- Moderate physical activity.
Excess body weight causes hypertension and contributes to the formation of atherosclerotic plaques, which is why it needs to be dealt with. Therefore, patients should eat a healthy diet and be physically active whenever possible. In addition, they need to quit smoking, because nicotine has a bad effect on the walls of blood vessels.
Symptoms and treatment of stage 2 DEP
The described disease gradually progresses over time. Stage 2 DEP is characterized by an increase in the severity of symptoms.
Patients and their loved ones notice a deterioration in memory and intelligence, and cease to fully cope with work activities.
Even at the everyday level, problems arise. For long hours, such patients can sit or lie idle, not showing interest in anything. The mood becomes apathetic.
The difficulty of diagnosis is that grade 2 DEP is difficult to differentiate from grade 3 DEP.
Treatment
Medicinal component
Therapeutic and preventive diet, which involves reducing the consumption of foods with high fat content and low salt content:
- Reducing the amount of meat consumption, all fried and smoked;
- Regular use of low-fat fish and other seafood in the diet;
- Daily consumption of fresh vegetables and fruits;
- Nuts and dried fruits;
- Dairy products;
- Cereals;
- And also, stopping smoking and alcohol abuse;
- Physiotherapy.
Physiotherapeutic treatment:
- Baths that promote vasodilation - for example, radon or carbon dioxide;
- Therapeutic massage of the collar zone helps relieve tension in the cervical spine and vascular spasm;
- Galvanotherapy of the collar zone - the procedure helps normalize blood circulation;
- Ultra-high frequency therapy (UHF) – is aimed at increasing the speed of blood flow, accelerating the delivery of oxygen and nutrients to tissues, and has an anti-inflammatory effect;
- Electrosleep - the essence of the technique is to stimulate the white and gray matter of the brain with low-frequency currents, the therapy promotes relaxation and improves the formation of new neural connections;
- Treatment with infrared laser radiation - the principle of therapeutic action is similar to UHF therapy.
All physiotherapy techniques require a course of use lasting 8-20 procedures.
Treatment methods of alternative medicine can be used - acupuncture, hirudotherapy, herbal medicine.
Also, in addition to the syndromic classification, there is a gradation according to the degree of encephalopathy. So, there are three degrees. Discirculatory encephalopathy of the 1st degree means the most initial, transient changes in brain function. Discirculatory encephalopathy of the 2nd degree indicates persistent disorders, which, however, only affect the quality of life, usually not leading to a severe decrease in ability to work and self-care. Discirculatory encephalopathy of the 3rd degree means persistent gross disorders, often leading to disability of a person.
Folk remedies
At the initial stage of development of dyscirculatory changes in the brain, the following folk recipes can be effective:
- Rosehip infusion. Reduces capillary permeability, improves cerebral circulation. Dry fruits (2 tablespoons) should be crushed, pour boiling water (500 ml), and leave for 20-30 minutes. Next, you need to drink instead of tea 2-3 times a day throughout the entire course of treatment.
- Infusion of clover flowers. Get rid of noise in your head. For cooking you need 2 tbsp. l. pour 300 ml of boiling water over the raw materials, leave for 1 hour. Take 3-4 times throughout the day, half an hour before meals. The infusion should be drunk during an exacerbation of symptoms.
Complications
Without proper treatment and follow-up of patients, progression of the disease and the following complications are possible:
- Brain hemorrhage and stroke;
- Brain swelling;
- Heart attack;
- Dementia.
Disability
Today, disability is assigned when a patient becomes unable to perform work duties due to a diagnosis of dyscirculatory encephalopathy.
The possibility of disability with DEP of the 1st degree is low.
In case of DEP of the 2nd degree of the disease, patients are awarded the 3rd group of disability if they are able to partially fulfill their work obligations.
The second group is awarded for both 2 and 3 degrees of DEP - in this option, patients have periodic memory lapses. They cannot perform professional duties to any extent.
The first disability group can be assigned only for DEP of the 3rd degree, which indicates the enormous danger of this form.
The above points are reflected in the Federal Law of the Russian Federation “On Social Protection of Disabled Persons”. Assignment to a specific group is carried out after passing a medical examination.
How long do they live?
How long can you live with the problem? The diagnosis of DEP is far from a death sentence for patients. Timely and competent treatment can slow down the progression of the pathology of brain disorders for decades.
If you ignore the symptoms of the disease, the transition to the next stage occurs in approximately 18-24 months.
Prevention
There are not many methods for preventing the disease, but standard treatment cannot do without prevention. To prevent the development of dyscirculatory encephalopathy, as well as to reduce its manifestations, you should constantly monitor the level of blood pressure, the content of cholesterol and its fractions. Psycho-emotional overload should also be avoided.
If you have dyscirculatory encephalopathy, you should also regularly (1-2 times a year) undergo a full course of vasoactive, neuroprotective, nootropic therapy in a day or round-the-clock hospital to prevent progression of the disease. Be healthy!