Not for self-medication. Consult your doctor.
ABRAMOV-FIDLER MYOCARDITIS
It is characterized by a severe course, often in the absence of indications of an infectious or toxic cause of the disease. In the clinical picture of the advanced stage of myocarditis, the leading place is occupied by severe heart failure, refractory to the therapy. The picture of the disease is complicated by rhythm disturbances (often a combination of intraventricular or atrioventricular block with paroxysmal or persistent disturbances of excitability), episodes of cardiac asthma, cardiogenic shock, thromboembolism in the systemic and pulmonary circulation.
Some patients have myocarditis
accompanied by severe pain resembling angina. In addition to rhythm disturbances, the ECG reveals severe changes in the repolarization phase (deep negative T wave), and sometimes a deep Q wave, reflecting necrotic focal changes in the myocardium. This often gives rise to an erroneous diagnosis of coronary artery disease and myocardial infarction, especially in people over 40 years of age.
The enlargement of the heart can be significant (on echocardiography, the diameter of the left ventricle can exceed 6-6.5 cm, the left atrium - 4-4.5 cm), which causes the appearance of auscultatory changes - a three-term rhythm, systolic, and sometimes diastolic murmurs. In young patients in such cases, there is a need for differential diagnosis with heart disease, which is often resolved only with echocardiography. The multivariate clinical picture of Abramov-Fiedler myocarditis is reflected in the classification proposed by M. I. Teodori (1956, 1972), which includes asystolic, thromboembolic, arrhythmic, pseudocoronary and mixed forms of idiopathic myocarditis
. According to the course of this classification, there are options: 1) acute - with a fatal outcome in 2-8 weeks, 2) subacute - 3-18 months, 3) chronic recurrent - can last several years, 4) latent - without clear clinical manifestations, which sometimes ends in sudden death.
Forecast
Abramov-Fiedler
myocarditis is unfavorable, the cause of death is most often progressive heart failure and ventricular fibrillation, less often - thromboembolic complications.
Treatment
myocarditis. Etiological treatment is aimed at eliminating the source of infection, and in this case treatment is carried out with antibiotics, interferon, and isolation of the patient from other possible causes of myocarditis (drugs, allergens, toxic substances).
Anti-inflammatory treatment includes NSAIDs, primarily indomethacin (75-100 mg/day) in combination with delagil (0.25-0.5 g/day) for at least 4-5 weeks. The duration of treatment is determined by clinical signs of improvement, ECG and EchoCG dynamics, and a decrease in laboratory activity tests. If the use of indomethacin is contraindicated, it can be replaced with acetylsalicylic acid (3-4 g/day), voltaren or diclofenac (75-100 mg/day), pyrazolone derivatives (butadione - 600 mg/day).
In the treatment of severe forms of myocarditis of the Abramov-Fiedler type and myocarditis with signs of high activity of immune reactions (in combination with pericarditis, vasculitis, arthritis, dermatosis, hyperuglobulinemia, altered lymphocyte blast transformation reaction, high titer of anticardiac antibodies), the administration of GCS in a dose of 30-40 mg is indicated /day up to 2 months with a gradual reduction in dose; in these cases, heparin is prescribed up to 40 thousand units per day for 7-10 days. As additional agents, metabolic drugs are used (anabolic steroids, ATP, cocarboxylase, riboxin, potassium orotate and vitamins), as well as anti-bradykinin substances (parmidin, prodectin, trasylol).
Symptomatic therapy is prescribed for heart failure, rhythm disturbances and thromboembolic complications.
Myocarditis can occur with any infectious disease, but currently myocarditis is most often observed with viral infections. Non-infectious factors that cause myocarditis include some drugs (antibiotics, sulfonamides, etc.), serums and vaccines. Myocarditis also occurs with systemic connective tissue diseases, for example, with systemic lupus erythematosus and other systemic vasculitis.
Among the causes of myocardial inflammation, a special place is given to rheumatism, in which myocarditis is one of the main manifestations of the disease, along with a combination with pericarditis.
Depending on the cause of myocarditis, there are:
Rheumatic;
Infectious (viral, bacterial, rickettsial, etc., including measles, rubella, chickenpox, diphtheria, scarlet fever, severe pneumonia, sepsis; the most common is the Coxsackie B virus, which causes myocarditis in half of the diseases);
Allergic (medicinal, serum, post-vaccination);
For diffuse (systemic) connective tissue diseases, injuries, exposure to ionizing radiation;
Idiopathic (that is, unknown nature) Abramov-Fiedler myocarditis.
The leading role in the development of the inflammatory process belongs to allergies and impaired immunity.
Infectious myocarditis
Myocarditis begins against the background of infection or shortly after it with malaise, sometimes persistent pain in the heart, palpitations and interruptions in its work and shortness of breath, and occasionally pain in the joints. Body temperature is normal or slightly elevated. The onset of the disease may be unnoticeable or hidden. The severity of symptoms is largely determined by the prevalence and severity of the progression of the process. The size of the heart increases early. Important, but not constant signs are rhythm disturbances (tachycardia, its acceleration, bradycardia, its decrease, atrial fibrillation, extrasystole) and conduction (various blockades): palpitations, interruptions in the work of the heart, a feeling of “fading”, “stopping”. Myocarditis can be complicated by the development of heart failure. Infectious myocarditis can occur in two forms: infectious-toxic, in which signs of heart damage appear during a period of severe intoxication; infectious-allergic, in which signs of heart damage usually occur 23 weeks after the onset of an acute or exacerbation of a chronic infectious disease.
Symptoms of Abramov-Fiedler myocarditis
The disease occurs without elevated body temperature, but in the later stages of the disease febrile attacks are observed.
Symptoms of idiopathic myocarditis are the following:
- frequent shortness of breath;
- tachycardia;
- cardiac asthma;
- arterial hypotension;
- formation of blood clots in blood vessels;
- circulatory disorders;
- prostration;
- heart, kidney failure;
- swelling.
Myocarditis in children
Myocarditis in a child, as well as in an adult, occurs as a result of the action of viruses and bacteria. Children are characterized by the presence of two types of myocarditis:
Congenital - in this case, the child suffers from lethargy, pallor, and shortness of breath from the day he is born. Gets tired quickly when feeding and does not gain weight. This type of disease is characterized by a significant expansion of the boundaries of the heart, tachycardia.
Acquired. This type of myocarditis is divided into acute, subacute and chronic. Acute myocarditis is a consequence of acute respiratory viral infection. Initial signs: lack of normal appetite, restlessness and night moans of the child, attacks of cyanosis (blue discoloration) and shortness of breath, nausea and vomiting. In the case of subacute and chronic myocarditis, both significant and minor symptoms are noted. Minor ones include hepatomegaly (enlarged liver), tendency to faint, and vomiting. Significant - cyanosis, cardiac hump (change in the shape of the chest above the heart area in the form of a hump), tachypnea (increased breathing).
Etiology
Damage to the heart muscle during myocarditis can be caused by direct exposure to infection, parasitic infections, chemical and physical effects, and allergic damage to the myocardium. The leading role in the occurrence of myocarditis belongs to infectious diseases. The most common cause of myocarditis in recent times is viruses, which is associated with the spread of epidemics of viral respiratory tract infections in large populated areas, a decrease in natural immunity, and improved diagnostics to identify pathogens. Most often, myocarditis is caused by enteroviruses Coxsackie A and B, ECHO. In 20% of cases, the course of myocarditis caused by the Coxsackie B virus becomes chronic.
Myocarditis of bacterial origin takes 4th place, inferior not only to viral, but even parasitic lesions of the heart muscle in some regions. Streptococcal myocarditis accounts for no more than 5%. In this case, heart damage is caused either by the direct effect of bacteria on the myocardium, or by an infectious-allergic mechanism. Carditis can be caused by toxoplasma infection (especially congenital forms). Fungal myocarditis develops in patients with chronic diseases during massive antibacterial therapy. Allergic myocarditis (drug-induced, serum-related, post-vaccination) and myocarditis due to collagenosis are recorded. One should not lose sight of a possible hereditary predisposition to this disease.
Forecast
The prognosis depends on the form of the disease and its severity. With Abramov-Fiedler myocarditis, septic and diphtheria myocarditis, the prognosis for life is unfavorable. In most cases, myocarditis is asymptomatic and ends with complete recovery. Other forms of myocarditis with acute and subacute course in at least 1/3 of cases result in complete recovery. In other patients, the outcome is cardiosclerosis, the location and extent of which determines the state of heart function, or dilated cardiomyopathy develops. Extremely severe variants of the course of myocarditis with rapid progression of refractory heart failure and death are known. Heart rhythm disturbances can lead to sudden death.
Symptoms
Abramov-Fiedler myocarditis has a severe, often malignant course. In the acute form, symptoms of right ventricular or progressive total heart failure quickly increase. Shortness of breath, orthopnea, cyanosis, tachycardia, arterial hypotension, edema, ascites, hepatomegaly and splenomegaly appear.
Cardiac asthma and pulmonary edema may develop. Cardiac pain resembling angina pectoris often occurs. In the acute stage, there is an increase in body temperature to 38-39°C. Sometimes the leading cause in the clinic is thromboembolic syndrome; in this case, the disease can manifest with pulmonary embolism, thromboembolism of the cerebral, renal, and splenic vessels. The fulminant course of Abramov-Fiedler myocarditis always ends in death.
Abramov-Fiedler myocarditis is characterized by a severe, often malignant course. In the acute form of the pathology, there is a rapid increase in symptoms of right ventricular or progressive total heart failure. The patient develops shortness of breath, orthopnea, cyanosis of the skin, tachycardia, decreased blood pressure, edema, ascites, hepatomegaly and splenomegaly.
Quite often, the leading symptom of the pathology is thromboembolic syndrome; in this case, the disease can manifest with pulmonary embolism, thromboembolism of the cerebral, renal, and splenic vessels. The fulminant course of Abramov-Fiedler myocarditis in almost all cases ends in the death of the patient.
In the chronic course of idiopathic Abramov-Fiedler myocarditis, the disease is caused by a recurrent course. Experts note that in this case, after each exacerbation, the patient experiences progression of myocardial fibrosis, cardiomegaly and irreversible circulatory disorders. Cases of latent Abramov-Fiedler myocarditis have been recorded, which lead to sudden death.
What can you do?
If a young patient or a child who has not previously had heart problems experiences pain and discomfort in the heart area during or after an infection, or interruptions in heart function, it is necessary to immediately contact a cardiologist to receive the necessary treatment.
Elderly people suffering from any heart disease, who suddenly experience interruptions in the functioning of the heart, pain in the heart area that does not decrease while taking usually effective medications, also need to consult a cardiologist.
Diagnostics and differential diagnostics
Diagnosis of myocarditis is based on a combination of a number of data: the presence of a previous infection (proven by clinical and laboratory tests), the results of examining the patient (weakening of heart sounds, expansion of its boundaries, rapid heartbeat, symptoms of congestive heart failure), data from additional methods of examining the patient (electrocardiographic, x-ray , echocardiographic studies, laboratory examination results, methods for studying the central circulation, radionuclide methods, endomyocardial biopsy).
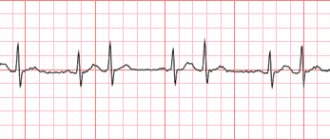
Electrocardiographic examination for suspected myocarditis is mandatory. Detection of nonspecific changes in the final part of the ventricular complex in combination with rhythm and conduction disturbances makes it possible to suspect myocarditis. Drug tests for myocarditis are always negative. In the chronic course, changes in the ECG are persistent and are caused by the development of myocardial cardiosclerosis (impaired atrioventricular and intraventricular conduction and rhythm disturbances).
X-ray examination of patients with myocarditis allows us to clarify the degree of enlargement of the heart as a whole and its individual chambers. In severe myocarditis, all parts of the heart are enlarged, and there are signs of circulatory disorders in the pulmonary circle. Mild myocarditis is accompanied by enlargement of only the left ventricle. The X-ray method allows exudative pericarditis to be excluded as the cause of expansion of the borders of the heart.
An echocardiographic examination helps to exclude other causes of heart enlargement and to accurately determine the severity of the expansion of various chambers of the heart.
The results of laboratory research methods are not conclusive for the diagnosis of myocarditis, but they make it possible to accurately determine the presence of a previous infection. In some cases, to confirm the diagnosis, they resort to a study of the central circulation, with the help of which the degree of impairment of the pumping function of the heart is determined, and changes in blood circulation parameters make it possible to evaluate the effectiveness of the treatment. Radionuclide methods prove the presence of foci of cardiosclerosis in patients with severe myocarditis. Finally, the endocardial biopsy method makes it possible to accurately determine the quality and extent of myocardial damage.
Myocarditis should be distinguished from each other, from endocardial damage with the formation of valvular disease, myocardial dystrophy (see), coronary heart disease (see), pulmonary heart disease, cardiomyopathy (see), endocardial fibroelastosis, alcoholic myocardial damage, heart defects (see. ), pericardial diseases, functional disorders of the cardiovascular system.
What can a doctor do?
There are no strictly specific signs of myocarditis. The diagnosis is made on the basis of clinical signs, changes in the electrocardiogram, echocardiography, the presence of laboratory signs of inflammation, and changes in radiographs.
Hospitalization is usually indicated for myocarditis. General measures include bed rest, restriction of physical activity, oxygen inhalation if necessary, and drug therapy.
Drug therapy depends on the underlying disease and the nature of cardiac dysfunction. For infectious non-viral myocarditis, antibiotics are prescribed, the choice of which depends on the isolated pathogen and its sensitivity to antibiotics.
Other areas include the treatment of heart failure, cardiac arrhythmias and conduction disorders, and thromboembolic complications. In the first months after discharge from the hospital, patients who have had myocarditis should be monitored; it is necessary to limit physical activity.
The book “Diseases of the cardiovascular system (R.B. Minkin).”
Idiopathic myocarditis Abramov-Fiedler
Idiopathic myocarditis was described in 1897 by S. S. Abramov and in 1899 identified as an independent disease by Fiedler, so the disease is named after the names of these authors. The etiology and pathogenesis of the disease have not been precisely established.
It is believed that allergic mechanisms play a role in the development of the disease (the disease can develop after the administration of therapeutic vaccines and serums, taking medications, etc.), and the role of a viral infection that contributes to autoimmune damage to the heart cannot be ruled out.
Pathological anatomy. At the autopsy of patients with Abramov-Fiedler myocarditis, a significant increase in the size of the heart, dilatation and hypertrophy of its parts are determined; the weight of the heart can reach 700-800 g (with a norm of 250-300 g).
The cavities of the heart chambers contain parietal thrombi, which during the patient’s lifetime were a source of embolism in various organs. Microscopic examination reveals inflammatory changes in the interstitial tissue, its plethora and swelling, accumulation of cellular elements; phenomena of dystrophy and necrosis are observed in muscle fibers; Characterized by massive scar fields in the myocardium, in which muscle elements seem to be immured.
Clinical picture. Abramov-Fiedler myocarditis can occur acutely, subacutely and chronically. Acute and subacute course are characterized by rapidly progressing heart failure and poor prognosis.
The patient complains of shortness of breath, discomfort in the heart area, weakness, and fever. An objective examination reveals cyanosis; pulse is rapid, low filling.
The size of the heart is enlarged, the sounds are muffled, a gallop rhythm, systolic and sometimes diastolic functional murmur can be heard. Failure of the left heart is accompanied by symptoms of stagnation in the pulmonary circulation, and of the right - in the large circle (congested veins of the neck, enlarged liver, swelling of the legs, etc.). Signs of pericarditis may be detected.
Embolisms are often observed in various organs: kidneys, lungs, spleen, etc. The ECG shows signs of pronounced diffuse muscle changes, coronary insufficiency, disturbances of atrioventricular and intraventricular conduction, various arrhythmias, up to atrial fibrillation and others, which, along with heart failure, can cause sudden death.
X-ray and EchoCG studies reveal a significant and progressive increase in the size of the heart, dilatation of its cavities, and weakening of pulsation. Blood tests show neutrophilic leukocytosis with a shift to the left and increased ESR.
A history of previous infection, various allergenic factors (hypothermia, insolation, taking medications, etc.), clinical and laboratory signs of inflammation help in making a correct diagnosis. According to the clinical picture, Abramov-Fiedler myocarditis is similar to dilated cardiomyopathy, but, unlike the latter, myocarditis is characterized by acute onset of heart failure or its relapse due to infection, vaccination, or medication.
Abramov-Fiedler myocarditis in most cases is severe and has a poor prognosis. The causes of death are severe heart failure, rhythm and conduction disorders, embolism in various organs. Death can occur suddenly; usually the disease lasts from several months to 1-2 years.
Treatment consists of prescribing bed rest, digitalis and diuretics, and anticoagulants to prevent thromboembolism. In case of damage to other organs and systems, along with the myocardium, cytostatic therapy is indicated.
Idiopathic myocarditis...
Idiopathic malignant myocarditis, Abramov-Fiedler myocarditis
Version: MedElement Disease Directory
Isolated myocarditis (I40.1)
Cardiology
Myocarditis in childhood
If a child has heart failure, but does not have a congenital heart defect, then doctors immediately begin to suspect myocarditis. Most often, viruses, bacteria and other infections can provoke the development of the disease in question in childhood. But there are other reasons:
- allergic diseases;
- leukemia;
- connective tissue diseases;
- Kawasaki syndrome;
- metastases of malignant tumors;
- chemical or physical influences.
It is very difficult to diagnose myocarditis in children, because its clinical picture is asymptomatic.
Treatment of myocarditis in children should be carried out in compliance with the following rules:
strict bed rest for at least 12 hours a day;
- strictly dosed physical activity;
- prescription of non-hormonal anti-inflammatory drugs;
- prescription of therapy with antibacterial drugs (penicillin series);
- identification and elimination of the underlying disease;
- treatment of heart failure.
Modern medicine, in most cases, successfully treats myocardial inflammation, and no morphological or physiological consequences for the body are noted. Due to the fact that doctors use modern methods of laboratory and instrumental research as part of diagnosis, severe forms of the disease that end in death for the patient are extremely rare. But timely detection of the inflammatory process in the myocardium remains a very important point, therefore preventive examinations must be performed at least once a year.
Tsygankova Yana Aleksandrovna, medical observer, therapist of the highest qualification category
8, total, today
( 186 votes, average: 4.69 out of 5)
Tachycardia - signs, types of tachycardia, treatment
Pulmonary hypertension: signs, treatment, possible risks
Related Posts
general information
Short description
Acute idiopathic myocarditis is a rare form of heart disease first described in 1889 by Fiedler.
Idiopathic isolated Fiedler's myocarditis
- this is a severe myocarditis Myocarditis - inflammation of the myocardium (the middle layer of the heart wall, formed by contractile muscle fibers and atypical fibers that make up the conduction system of the heart.); manifested by signs of impairment of its contractility, excitability and conductivity with an unfavorable outcome and unknown etiology, having an autoimmune genesis and not accompanied by damage to the endocardium and pericardium. Typical for idiopathic myocarditis are isolated cardiac lesions, a combination of extensive dystrophic changes in the myocardium with infiltrative-inflammatory changes and thrombus formation against the background of widespread cardiosclerosis. Cardiosclerosis is the excessive development of connective tissue in the myocardium.
Pathogenesis and pathological anatomy
The mechanisms of myocarditis development are due to the direct impact of the occurrence factor on the heart muscle, as well as their combination with immune disorders. With a decrease in the immunological reactivity of the body, the infection from the primary focus enters the bloodstream and spreads to various organs and tissues, where foci of secondary reproduction of the infectious agent are formed. The myocardium is most often affected. In this case, the pathogen has a direct damaging effect on the heart muscle, being a trigger for the development of the inflammatory process. In response to damage, special substances are released with the subsequent development of a hypersensitivity reaction. This increases the permeability of the vascular wall and damages the vascular walls.
Autoallergy in this process is one of the stages of the pathological process. In the chronic course of myocarditis, the pathogen does not play a significant role, and the disease is based on disorders of the immune system. All of these mechanisms lead to systemic myocardial damage, a malignant and relapsing course of the disease, resistant to traditional treatment.
Changes in myocarditis are characterized by an increase in the mass and size of the heart, the thickness of the ventricles, the presence of focal or widespread replacement with connective tissue in the form of scars in the myocardium, and parietal thrombi.
Classification
Teodori M.I. proposed to distinguish the following clinical forms of Fiedler's idiopathic myocarditis
: — asystolic (with clinical signs of severe heart failure); - thromboembolic; - arrhythmic (with atrial fibrillation, paroxysmal tachycardia, complete atrioventricular block), - pseudocoronary with pain in the heart, infarction-like changes ECG-ECG - Electrocardiography (method of recording and studying the electric fields generated during the work of the heart); - mixed.
Professor Gurevich M.A. first described the pseudovalvular variant
Fiedler's myocarditis.
Treatment of idiopathic myocarditis
No etiotropic therapy has been developed for this disease. Treatment of idiopathic Abramov-Fiedler myocarditis consists only of symptomatic treatment of arrhythmias, heart failure, and prevention of thromboembolic complications.
Appointed:
- diet therapy;
- bed rest;
- taking medications (cardiac glycosides, nitrates, ACE inhibitors, diuretics, anticoagulants, aldosterone receptor antagonists, beta blockers).
Anti-inflammatory therapy consists of prescribing NSAIDs (Voltaren, indomethacin, diclofenac).
Severe forms of idiopathic myocarditis with high activity of immune reactions require the use of glucocorticoids, and in an allergic background - desensitizing drugs.
Additionally, metabolic drugs are indicated (riboxin, cocarboxylase, potassium orotate, vitamins).
Giant cell myocarditis suggests heart transplantation.
Etiology and pathogenesis
There are 3 ideas about the etiology of this disease: 1. Idiopathic myocarditis (Abramov-Fiedler myocarditis) is a variant of severe myocarditis of different etiologies with an autoallergic mechanism of development. Often the initiator of the process is medication. 2. Idiopathic myocarditis is caused by a viral infection that triggers autoimmune mechanisms. 3. Some researchers suggest that Abramov described dilated cardiomyopathy Dilated cardiomyopathy (DCM) is a condition in which the heart's ability to pump blood decreases due to the enlargement and weakening of the left ventricle (the main pumping chamber of the heart), which reduces the ejection fraction (the amount of blood , which the heart ejects with each beat), and Fiedler - severe diffuse myocarditis Diffuse myocarditis - inflammation of the myocardium, in which the entire myocardium is affected; usually manifests itself as severe heart failure (this opinion is based on a review of Abramov and Fiedler’s preparations and patient autopsy reports).
Histological examination of cardiac muscle tissue reveals large granulomatous foci containing lymphocytes, macrophages and multinucleated giant cells.
Three histological types of myocarditis have been described:
— inflammatory-infiltrative type; - dystrophic; - mixed type.
Causes of idiopathic myocarditis
If we look at the causes of idiopathic Abramov-Fiedler myocarditis, then the term “idiopathic” indicates the unclear origin of this disease. Some researchers (Ya.L. Rapoport, A.I. Abrikosov) saw the allergic nature of the disease and the autoallergic mechanism of its development. Its appearance is often preceded by eczema, serum sickness, and drug allergies.
Recently, the possibility of trigger factors that initiate the process of idiopathic myocarditis, such as autoimmune reactions or viral infections, has been suggested.
Statistical data confirm the hypothesis of a viral effect on Abramov-Fiedler myocarditis: if in the general population chronic idiopathic myocarditis occurs in 0.005% of cases, then in those who have had viral acute myocarditis it develops in 4-9% of cases. There is even an opinion that this disease is the worst course of infectious-allergic myocarditis.
Idiopathic myocarditis in approximately 1/5 of patients is accompanied by autoimmune diseases. The fact of detection of cellular toxicity and antibodies to the myocardium also speaks in favor of the immunopathological mechanism of inflammation.
Clinical picture
Symptoms, course
Fiedler's myocarditis has a clinical picture consistent with the most severe form of myocarditis. The course of the disease is acute (sometimes fulminant).
Main clinical manifestations:
- severe shortness of breath; - weakness; - pain in the heart area; - heartbeat; - clinic of severe congestive heart failure (orthopnea Orthopnea - a forced sitting position taken by the patient to facilitate breathing with severe shortness of breath, acrocyanosis Acrocyanosis - bluish coloration of the distal parts of the body (fingers, ears, tip of the nose) due to venous stagnation, more often with right heart failure, peripheral edema , swelling of the neck veins, enlarged painful liver, possible development of ascites Ascites - accumulation of transudate in the abdominal cavity, hydrothoraxHydrothorax - accumulation of transudate (edematous fluid) in the pleural cavity); - a sharp expansion of the boundaries of relative dullness of the heart, mainly to the left, dullness of heart sounds, pathological three-part rhythm (usually proto-diastolic gallop rhythm), systolic murmur of relative mitral or tricuspid insufficiency, often - cardiac arrhythmias.
Suspicion of idiopathic myocarditis should arise in the following cases: - predominance of complaints of shortness of breath with little physical activity, severe fatigue, interruptions in cardiac function; - the size of the heart increases very early with the rapid (within several days) formation of cardiomegaly. Cardiomegaly is a significant increase in the size of the heart due to its hypertrophy and dilatation, which is detected by percussion and x-ray; - thromboembolic syndrome is observed. Thromboembolic syndrome is the re-occurrence of embolisms (blockage) of various arteries with thrombotic masses, due to the presence of a focus of thrombus formation or a significant increase in blood clotting (a fairly common occurrence in idiopathic myocarditis); - hepato- and splenomegaly are observed.
Causes and symptoms
Abramov-Fiedler myocarditis is a severe myocardial pathology
It is impossible to identify the main reasons for the development of pathology. Provoking factors are allergic or autoallergic pathologies. Eczema, serum sickness or an allergic reaction to medications contribute to the development of idiopathic myocarditis.
Abramov-Fiedler myocarditis is often observed in individuals suffering from acute viral myocarditis. The disease is quite common in people with autoimmune diseases. Antibodies to the myocardium are produced, and myocarditis develops against this background.
The pathology has an acute course and gradually progresses. The patient complains of shortness of breath, swelling, cyanosis, and rapid heartbeat. Signs of cardiac asthma and pulmonary edema may also be observed. In the acute stage, body temperature often rises and headaches appear. Sometimes there may be thromboembolic syndrome. In most cases, Abramov-Fiedler myocarditis is malignant in nature with the subsequent development of cardiac or right ventricular failure.
In the chronic form, the focus of inflammation renews, and as a result, myocardial fibrosis, circulatory disorders, and cardiomegaly develop.
Clinical features of idiopathic myocarditis are similar to dilated cardiomyopathy. This pathology can lead to serious complications in the form of massive thromboembolism, severe cardiac arrhythmias, and heart failure. All this ends in death.
Classification
The disease is very dangerous and can cause serious complications
Taking into account histological signs, Abramov-Fiedler myocarditis can be of several types:
- Dystrophic myocarditis. It is characterized by destructive changes in muscle fibers. As they progress, they die.
- Inflammatory-infiltrative myocarditis. With this form, infiltration of the interstitial tissue develops and its swelling is observed.
- Vascular myocarditis. It is diagnosed when small branches of the coronary arteries are affected.
- Mixed myocarditis. This type is characterized by a combination of signs of dystrophic and infiltrative myocarditis.
Giant cell myocarditis with the formation of non-caseating granulomas is also distinguished.
According to the course of the pathology, acute, subacute and chronic are distinguished. The acute form lasts from 2 to 8 weeks, the subacute form lasts 3-18 months, and the recurrent or chronic form lasts for several years. In rare cases, latent Abramov-Fiedler myocarditis without accompanying symptoms may occur.
The main reason for the development of myocarditis in patients is infectious diseases, but most often the disease is detected against the background of viral pathologies - about 50% of all cases.
Often the cause of inflammation is two or more infections, in which case one of the diseases creates the conditions for the disease, the second directly affects the heart muscle.
The reasons influencing the development of myocarditis are usually combined into several groups:
- Infectious (various bacteria, fungi, influenza viruses, herpes and hepatitis, as well as parasites).
- Allergic (the body’s reaction to the administration of serums and other protein preparations, exposure to external allergens).
- Toxic (alcohol, drug overdose, drugs, radiation, work in chemical production, etc.).
- Endocrine (hormonal disorders).
- Autoimmune (rheumatism and rheumatoid arthritis, systemic lupus erythematosus, vasculitis, etc.).
The main causes of cardiac myocarditis
Most often, patients develop secondary myocarditis as a complication of severe infection, connective tissue damage, burn disease, transplant rejection after surgery, etc.
In some cases, primary, or isolated, myocardial damage that is not associated with a specific disease is diagnosed. This is usually allergic or viral myocarditis, in which the virus multiplies directly in the heart cells, and the classic manifestations of infection (runny nose, cough, lacrimation, temperature fluctuations) are absent.
There are also additional factors that can serve as a kind of trigger for the development of myocarditis: chronic infection (cholecystitis, pulpitis, adnexitis), hypothermia, poor nutrition, constant stress.
- Viral infections (most often enteroviral infections, such as coxsackievirus).
- Other infections: bacterial, fungal, rickettsia and spirochetes (rickettsiosis, borelliosis).
- Cocaine intoxication.
- Cardiomyopathy of pregnancy.
- Giant cell myocarditis.
- Idiopathic myocarditis.
The cause of myocarditis is most often infectious: viral (influenza, adenoviruses, Coxsackie), bacterial (diphtheria, coccal infection), fungal.
Non-infectious myocarditis is associated with chemical and pharmacological (vaccines, serums) agents. There are also allergic and idiopathic myocarditis, the etiology of the latter has been little studied.
Patients complain of prolonged pain in the heart region, such as cardialgia, localized in the apex of the heart, or angina pectoris. Often concerned about palpitations, interruptions in heart function, shortness of breath, low-grade fever. Asthenovegetative syndrome is expressed.
Auscultation of the heart reveals a muffled first tone, a blowing systolic murmur, and often rhythm disturbances. There is an increase in the borders of the heart to the left, and in severe forms there is a total increase in the size of the heart.
Rg-logically determines the increase in heart size.
ECG: nonspecific ST and T changes, rhythm disturbances.
EchoCG: cardiomegaly, dilatation of the heart chambers, decreased ejection fraction, myocardial hypokinesia.
Laboratory data:
- general blood analysis;
- biochemical changes in the form of dysproteinemia, increased levels of fibrinogen, transaminases, the appearance of C-reactive protein.
Diagnostic criteria
- A history of previous infection, proven by clinical and laboratory data, plus signs of myocardial damage.
- Clinical manifestations of myocardial damage.
- Laboratory and instrumental data.
Diagnostics
ECG:
- smoothed or negative T waves; — depression of the ST interval; - pathological Q waves may appear in many, mainly left chest leads; - various heart rhythm disturbances.
EchoCG:
- expansion of the cavities of the heart; - often detection of wall thrombi; - a sharp violation of the contractile function of the left ventricular myocardium; - relative mitral and tricuspid insufficiency.
X-ray data
: - cardiomegaly; - signs of venous congestion in the lungs; - episodes of thromboembolism in the vessels of the systemic and pulmonary circulation.
Myocardial biopsy
in recent years has gained some importance in the diagnosis of idiopathic myocarditis. During the study: - in 48% of cases, changes similar to cardiomyopathy are revealed: fibrosisFibrosis is the proliferation of fibrous connective tissue, occurring, for example, as a result of inflammation. , myolysisMyolysis - melting (dissolution) of necrotic muscle fibers (muscle cells), stromal edema; — in 25% of cases, myocardial changes are not detected; — in 4.4% of cases, round cell infiltration is detected;
In 1% - giant cell myocarditis. Giant cell myocarditis is an inflammation of the myocardium, characterized by the progressive breakdown of muscle fibers and the presence of multinucleated giant cells in the myocardial stroma.
Symptoms and signs of cardiac myocarditis
Diagnosis of myocarditis often causes difficulties due to the fact that patients generally have the same set of clinical manifestations as with idiopathic DCM.
However, there are a number of symptoms that in some cases can confirm the presence of myocarditis:
- general signs of inflammation;
- the presence of extracardiac signs of inflammation (in joints, muscles, kidneys, etc.) associated with autoimmune mechanisms;
- positive effect from the use of glucocorticoids (which is not typical for DCM).
In many cases, myocarditis is asymptomatic. Forecast.
With a mild asymptomatic course, the disease most often ends in complete recovery. In the presence of clinical manifestations, a favorable outcome occurs in approximately 50% of patients, and in the other 50%, myocarditis is complicated by the development of DCM.
The giant cell form of idiopathic Abramov-Filler myocarditis has an unfavorable prognosis.
Clinical signs
- Fatigue, shortness of breath and chest discomfort.
- Fever with tachycardia disproportionate to the height of the fever may occur.
- With severe LV dysfunction, heart failure may develop (not common).
- Atrial and ventricular arrhythmias are common.
The clinical picture of acute myocarditis can vary significantly between diffuse and focal lesions. The former are usually more severe and lead more likely to signs of heart failure and disruption of the contractile function of the working muscle.
The latter often turn out to be milder and are clinically manifested mainly by signs from the conduction system—arrhythmias of various types; they are recognized only when special attention is paid to the state of the heart during infections, when individual extrasystoles or other arrhythmias are found and an electrocardiographic study allows one to confidently make a diagnosis of myocarditis.
Laboratory diagnostics
In the diagnosis of myocarditis, routine laboratory research methods are considered uninformative and do not differ in specificity.
Laboratory indicators
(in order of decreasing frequency of information content): - increase in the content of a2- and g-globulins in the blood serum; — detection of antibodies to the myocardium; — positive reaction of inhibition of lymphocyte migration (RTML); - increase in sialic acids; - appearance of C-reactive protein; - increased activity of cardiac-specific enzymes and isoenzymes in the blood serum.
When analyzing troponin T levels above 0.1 ngm/ml, the sensitivity of the method for detecting myocarditis is 53%, and the specificity is 94%. For troponin 9, sensitivity is 34% and specificity is 89%.
Of the virological and immunological research methods, the following are of diagnostic importance: - determination of anticardiac autoantibodies of the IgM class (specific and partially specific for heart tissue); - detection of the viral genome using PCR-PCR - polymerase chain reaction.
Myocarditis
Myocarditis is inflammation of the heart muscle. The disease is usually caused by a viral infection, but can be caused by a bacterial or fungal infection, alcohol abuse, certain autoimmune disorders, and medications. Weakening of the body's defenses and autoimmune disorders are important predisposing factors to the disease.
Myocarditis occurs at any age, with equal frequency in men and women. Most often it occurs under the guise of the infection that caused it and may go unnoticed. In severe forms, cardiac failure develops, which reduces blood delivery to organs and tissues. Blood clots may also form, leading to a stroke or heart attack.
For mild forms of myocarditis, no special treatment is required; the underlying disease is treated. In complicated forms, treatment is aimed at restoring normal heart function and correcting immune disorders. In severe forms of heart failure and blockage of blood vessels by blood clots, surgical intervention may be required.
Synonyms Russian
Inflammation of the heart muscle.
English synonyms
Myocarditis.
Symptoms
Symptoms of myocarditis are varied and may vary depending on the cause and severity of the disease. Mild forms may be asymptomatic or disguised as a viral infection. In severe cases, signs of heart failure come to the fore.
Heart symptoms include:
- chest pain, often radiating to the left arm;
- palpitations;
- rapid pulse;
- shortness of breath during exercise, and then at rest;
- swelling in the ankles and feet;
- fatigue.
General manifestations of infection:
- weakness;
- sweating;
- headache;
- pain in joints and muscles;
- fever;
- a sore throat;
- diarrhea.
General information about the disease
Inflammation of the heart muscle can occur against the background of any infection, most often viral. Cases of non-infectious myocarditis are also quite common and can be caused by certain medications, harmful chemicals or radiation. In many cases, the exact cause cannot be determined.
The most common causes of infectious myocarditis include:
- viral infections, among which the most important are Coxsackie enterovirus, influenza A and B, measles, rubella, infectious mononucleosis and hepatitis B;
- bacterial infections, primarily staphylococcal, streptococcal and diphtheritic;
- some parasites, primarily trypanosomes and toxoplasma;
- fungi (candida, pathogens of aspergillosis and histoplasmosis).
Non-infectious factors causing myocarditis:
- medications (antibiotics, sulfonamides);
- narcotic substances (cocaine);
- excess thyroid hormones;
- renal dysfunction;
- serums and vaccines;
- connective tissue diseases (nonspecific ulcerative colitis, scleroderma, rheumatoid arthritis, rheumatism, systemic vasculitis, Wegener's granulomatosis, systemic lupus erythematosus);
- injuries and burns;
- factors of unknown origin (idiopathic myocarditis Abramov-Fiedler).
Regardless of the cause of the disease, the changes that occur in the heart muscle are of a similar nature. As a result of inflammation, myocardial edema develops and its blood supply deteriorates. Individual cells can be destroyed with the release of substances into the blood, including protein fragments, which are perceived by the body's defense system as foreign due to their similarity to the proteins of some bacteria and viruses. This leads to activation of the immune system and the development of a reaction to its own tissues. The severity of these reactions largely determines the severity of the disease.
According to the course, acute and chronic myocarditis are distinguished. The course of the disease largely depends on its cause. Infectious myocarditis is most often acute or subacute, sometimes recurrent, and rarely becomes chronic. Non-infectious myocarditis usually turns into a chronic progressive form with the development of complications such as increasing heart failure, heart rhythm disturbances, blood clots, and heart attack.
Who is at risk?
- Suffering from systemic and autoimmune diseases.
- Patients with rheumatism.
- Having undergone heart surgery.
- Pregnant women.
Diagnostics
Diagnosis of myocarditis is difficult due to the similarity of the clinical picture with many other diseases. One of the warning signs may be the appearance of shortness of breath two weeks after a viral infection. The diagnosis of “myocarditis” is made based on the medical history, laboratory data and special research methods. If an infectious nature of myocarditis is suspected, a blood test should be performed for certain viruses, bacterial or fungal infections. The scope of laboratory tests is determined by the attending physician based on the specific manifestations of the infectious process. In most cases, the decisive factor in making a diagnosis is a myocardial biopsy.
Laboratory research
- Complete blood count (without leukocyte count and ESR) Red blood cells and hemoglobin may be reduced in severe forms of myocarditis.
- Leukocytes. An excessive number of leukocytes with a shift in the leukocyte formula to the left (the appearance of young cellular forms in the blood) is observed in bacterial myocarditis. With myocarditis caused by a viral infection, significant changes in the leukocyte formula, as a rule, do not occur. The number of eosinophils may increase, indicating an allergic reaction.
- Rheumatoid factor is an antibody detected in the blood of people who suffer from certain connective tissue diseases. In myocarditis, a positive rheumatoid factor indicates the presence of an autoimmune component of inflammation.
- Antistreptolysin O - test for the presence of antibodies to streptococcus in the blood. Prescribed for suspected myocarditis of streptococcal origin.
- Total protein and protein fractions in the blood may be reduced in myocarditis. A significant decrease in total protein levels can be observed in severe forms of the disease.
- Alanine aminotransferase (ALT), Aspartate aminotransferase (AST). ALT and AST are enzymes mainly found in the cells of the liver, pancreas, and heart muscle. Their elevated levels in the blood serum may indicate destruction of myocardial cells.
- Fibrinogen. Fibrinogen is one of the main components of the blood coagulation system. Increased fibrinogen levels are typically observed during active inflammation in response to tissue damage. Fibrinogen produces another protein, fibrin, which is involved in the formation of blood clots. In myocarditis, elevated fibrinogen levels may indicate a risk of thrombotic complications.
- Markers of myocardial damage: troponin and creatine kinase-MB may increase during the acute phase of myocarditis. An increase in their level in the absence of clinical myocardial infarction is of diagnostic significance. Troponin I is one of the proteins present in cardiac muscle. When damaged, troponin is released and its concentration in the blood increases. Increases in troponin levels in myocarditis can be observed in the acute phase of the disease. Creatine kinase-MB is an enzyme found in the heart muscle and is released when its cells are destroyed. In myocarditis, just like troponin, it may indicate myocardial damage.
- Antibodies to the myocardium. An allergic or autoimmune component of inflammation is present in the vast majority of cases of the disease, both infectious and non-infectious in origin. The appearance of antibodies to the heart muscle is one of the main indicators confirming the diagnosis.
- A blood test for antibodies to individual pathogens may be prescribed to confirm the infectious nature of the disease. For myocarditis, blood tests for:
- Flu
- Hepatitis B
- Candidiasis
- Streptococcal infection
Additional tests for suspected myocarditis include:
- Ultrasound of the heart (echocardiography). Allows you to evaluate the size and function of the heart. An echocardiogram can detect an enlarged heart, signs of developing heart failure, the manifestation of which on echocardiography is a decrease in ejection fraction. It is estimated as the percentage of blood volume entering the aorta during heart contraction and remaining in it. The lower the ejection fraction, the more severe the degree of cardiac dysfunction. An indicator below 35% indicates a high risk of developing arrhythmias. Echocardiography can also help rule out other diseases that have similar symptoms.
- An ECG allows you to record changes in heart rate, disturbances in cardiac conduction and rhythm, and suspect previous myocarditis. In severe forms of myocarditis, changes on the cardiogram may resemble those during myocardial infarction.
- Cardiac magnetic resonance imaging (MRI). Allows you to see the position and size of the heart, its shape and structure. MRI can show signs of myocardial inflammation.
- Myocardial biopsy. Using a special instrument, you can take fragments of the heart muscle for examination under a microscope. In this case, characteristic signs of inflammation and edema in muscle tissue are visible, as well as destroyed myocardial cells in severe cases of the disease. The method has high diagnostic accuracy and allows you to confirm or refute the diagnosis of myocarditis in cases where other research methods are insufficiently informative.
- Coronarocardiography. A method in which a radiopaque substance is injected into the vessels of the heart using special catheters. The method is important for excluding coronary heart disease, which in many cases should be differentiated from myocarditis.
Treatment
Treatment of myocarditis depends on the cause that caused it and the stage of the disease. In mild cases, restriction of physical activity is indicated; in more severe cases, bed rest is indicated. Salt restriction is recommended. Drug treatment may include:
- Antibiotics - prescribed when the bacterial nature of myocarditis is confirmed
- Steroid hormones - to suppress the autoimmune reaction and the allergic component
- Drugs that lower blood pressure and affect heart rate may be prescribed to reduce the workload on the heart.
- Diuretics to reduce swelling
In severe cases with the development of chronic heart failure, a pacemaker may be required or a heart transplant may be considered.
Prevention
There is no specific prevention of myocarditis. Basic measures to prevent myocarditis include:
- Scheduled preventive vaccinations
- Limiting contact with persons suffering from acute viral infection
- Timely treatment of viral diseases
- Maintaining personal hygiene rules
- A healthy lifestyle that eliminates the risk of HIV infection, avoiding drugs, limiting alcohol.
Recommended tests
- Erythrocyte sedimentation rate (ESR)
- Leukocyte formula
- General blood analysis
- General urine analysis with sediment microscopy
- Total protein in urine
- Fibrinogen
- Serum albumin
- Total protein in whey
- Protein fractions in whey
- Serum creatinine
- Urea in serum
- Rheumatoid factor
- C-reactive protein, quantitative
- Total immunoglobulin A (IgA) in serum
- Total immunoglobulin G (IgG) in serum
- Antibodies to myocardium
- Troponin I (quantitative)
- Creatine kinase MB
- Influenza virus A/B (influenza viruses A/B), RNA [real-time PCR]
- HBV, DNA quantitative [real-time PCR]
- Candida albicans, IgG, titer
- Mumps Virus, IgG
- Varicella Zoster Virus, DNA [real-time PCR]
- Epstein Barr Virus, DNA [real-time PCR]
- HIV 1.2 Ag/Ab Combo (determination of antibodies to HIV types 1 and 2 and p24 antigen)
- Streptococcus pyogenes, DNA [real-time PCR]
Treatment
Treatment of myocarditis includes inpatient and outpatient (sanatorium) stages. A significant role in treatment is played by the patient's compliance with bed rest in parallel with drug therapy. In mild forms of myocarditis, bed rest should be adhered to for 3-4 weeks until the ECG normalizes or stabilizes. The course of moderate severity predetermines strict bed rest for at least 2 weeks, and then extended bed rest for 4 weeks. A severe course is an indication for transferring the patient to the intensive care unit, where strict bed rest is observed until the period of compensation for circulatory disorders, and subsequently an extended regimen is prescribed for a period of at least 4 weeks. The patient's diet should be complete, with sufficient protein and vitamins, limited salt, and a sufficient amount of foods containing potassium salts (dried apricots, raisins, figs, baked potatoes). Moderate and severe myocarditis require intensive drug therapy, which is aimed at eliminating inflammatory, autoimmune, allergic processes, reducing the damaging effects of anti-myocardial antibodies, reducing the production of biologically active substances, restoring and maintaining blood circulation, and affecting metabolism in the myocardium. If the connection of the disease with an infectious agent is confirmed, the prescription of antibacterial and antiviral drugs is indicated.
An important component of treatment is the use of anti-inflammatory drugs, the effectiveness of which is determined by a decrease in the clinical manifestations of myocarditis, normalization of ECG parameters, and a decrease in laboratory activity tests. In most cases, the use of aminoquinoline drugs gives good results - they are used for a long time (within 6-9 months from the onset of the disease). Delagil (chloroquine, resokhin, plaquenil) is prescribed in a daily dose of 0.25-0.5 g. Taking drugs of this group in a larger dosage can lead to the development of changes in the fundus, deposition of pigment in the cornea, therefore long-term treatment with quinoline drugs should be carried out under under the supervision of an ophthalmologist. It is possible to use acetylsalicylic acid in a dose of 3-4 g per day for 4-5 weeks until the clinical and laboratory manifestations of inflammation decrease. Indomethacin at a dose of 75-100 mg per day for 5-6 weeks in combination with delagil has a good anti-inflammatory effect in myocarditis. As clinical and laboratory parameters improve, the dose is gradually reduced with subsequent complete discontinuation. Indomethacin is not indicated for peptic ulcers of various locations, during pregnancy and lactation, and in patients with mental disorders. Pyrazolone drugs are prescribed in some cases for exacerbation of myocarditis, but they are significantly less effective than other anti-inflammatory drugs. A positive aspect is the improvement of the patient’s well-being, mainly due to the analgesic effect of drugs of the pyrazolone group.
In the treatment of severe myocarditis or moderate myocarditis, the use of corticosteroid drugs is indicated. Glucocorticoids are indicated for patients with severe widespread myocardial damage, accompanied by cardiac enlargement and congestive circulatory decompensation. Their effect is most pronounced in allergic myocardial damage. Corticosteroids help reduce autoallergy rates and reduce clinical and electrocardiographic signs of the disease. The dose calculation for prednisolone is 30-40 mg per day. The drug is prescribed for 1.5-2 months with a gradual reduction in dose until complete withdrawal and switching to delagil.
The use of heparin increases tissue resistance to oxygen deficiency, inhibits fat peroxidation, and reduces the permeability of the vascular wall. Heparin is prescribed if blood clotting can be controlled. Heparin is administered subcutaneously, in the first 7-10 days at a dose of 10 thousand units 4 times a day, then 5 thousand units 4 times a day (7-10 days), and subsequently 5 thousand units 2 times a day (10-14 days).
In order to increase the immunological reactivity of the body (asymptomatic myocarditis, frequent colds, the presence of foci of chronic infection), levamisole is used at a dose of 150 mg per day for 2 days, followed by a break for 5-7 days. Then the administration of levamisole is repeated. Negative effects on the patient's body of biologically active substances are prevented by drugs with an anti-bradykinin orientation: angina (parmidin, prodectin), contrical (trasylol). The course of treatment is 1.5-2 months. Considering the presence of degenerative processes in the myocardium, in some cases anabolic steroids, cocarboxylase, riboxin, and potassium orotate are indicated. Metabolic and anabolic agents are used in combination with the above groups of drugs.
The presence of symptoms of circulatory failure is an indication for gradual digitalization in small doses (the therapeutic effect appears no earlier than 2 weeks from the start of therapy). For tachycardia, the following drugs should be prescribed: digoxin, digitoxin, cordigit. In patients with normo- and bradycardia, the following drugs are used: korglykon, adonis, isolanide. Cardiac glycosides for myocarditis should be used with great caution against the background of anti-inflammatory therapy in combination with potassium preparations and veroshpiron. Nitroglycerin in a dose of 5-10 mg is taken sublingually. The intervals between taking this drug are 15-20 minutes. Nitrosorbide is prescribed in a dose of 20 mg every 4-5 hours. For the treatment of severe heart failure, sodium nitroprusside is used: 50 mg of the drug is dissolved in 500 ml of 0.5% glucose solution and administered slowly over 10-12 hours. Sodium nitroprusside helps eliminate an attack of severe heart failure during the first hours from the start of administration.
For patients suffering from idiopathic myocarditis, the use of intensive therapy methods is indicated: catheterization of the right heart, drip administration of nitroprusside, phentolamine, dopamine. In severe cases, an artificial pacemaker is used.