The brain is the most important human organ, the center of the nervous system. When problems begin in the brain, pathologies arise, and all internal body systems suffer.
There are a lot of brain diseases, some of which medicine has not yet learned to fight, only predicting their course thanks to statistical data and symptoms that appear in the patient. In the fight against others, experts have identified effective targeted techniques that help, if not completely get rid of the disease, then at least alleviate the symptoms and prolong the patient’s life for several years.
Brain diseases can be conditionally divided according to their nature and underlying causes into:
- diffuse;
- focal.
Diffuse brain lesions are characterized by the fact that they cover all brain tissues uniformly. This can manifest itself gradually, while the pathology spreads in any case to all healthy and living cells, destroying them or transforming them into foreign bodies. Diffuse brain diseases occur due to general circulatory disorders, serious traumatic brain injuries, and powerful viral infections. The main condition and difference between diffuse lesions is the coverage of the tissues of the entire brain. Signs of such diseases appear immediately - chronic fatigue, constant apathy, severe dull and pressing headaches along the entire contour of the skull, drowsiness, disruption of the sensory organs and a significant decrease in performance.
Focal brain lesions are characterized by the fact that the pathology operates within a specific area - the focus. The reasons, again, may be disturbances in blood flow or damage to blood vessels, but precisely in a separate, specific area of the brain. The same can be said about traumatic brain injury; sometimes its consequences do not grow to the borders of the brain, but cover only a small area. Scientists also identify multifocal brain damage; it is easy to guess that it manifests itself in the fact that there are more than one such foci (damage areas). In this case, pathology can, in the process of development, cover neighboring tissues, also turning them into foci of anomalies.
In the process of focal brain lesions, foreign neoplasms can arise, both malignant and benign. In general, focal pathologies are manifested by the fact that their prerequisites are compression and damage to nerve tissue by any body or, for example, by the bony processes of the spine. In this case, in addition to damage to cells and tissues, there is a deterioration and inhibition of blood circulation in the same area of the brain.
Signs of focal damage do not appear immediately. It can all start with ordinary headaches, but as the tumor grows and the anomaly develops, the symptoms intensify and become varied, typical of many neurological diseases. This is why focal lesions are quite difficult to diagnose, and doctors usually resort to magnetic resonance or computed tomography procedures, because in very rare cases it is possible to determine the type of lesion based on a person’s complaints and symptoms and prescribe the correct treatment.
Clinical picture
A variety of symptoms may indicate focal brain lesions.
- Headache. Most often they appear suddenly, for no apparent reason. They are intense, reminiscent of a migraine. The pain may surround or be localized on one or both sides of the brain.
- Blood pressure increases. With focal damage, an increase in blood pressure indicates that the body is trying to compensate for the lack of nutrition that occurred due to vascular dystrophy of the brain.
- There is impairment of hearing, vision, and coordination of movement.
- Memory deteriorates, fatigue increases, and weakness appears.
- There is nausea and vomiting, which does not bring relief.
- Fainting conditions.
- Tremor of the limbs, convulsions, in some cases paralysis.
- Loss of reflexes.
- Breathing is impaired.
- A person is disturbed by psycho-emotional disorders, stress, and irritability increases.
Epileptic seizures and strokes may occur, which directly indicate the presence of focal brain damage. All these symptoms may be pronounced or may not appear at all.
Any clinical signs of the disease are associated with neurology, since nerve tissue is affected in focal lesions, which causes changes in autonomic function.
Focal symptoms of brain damage
Focal symptoms of brain damage are either
absent or mildly expressed and are transient
character. When basal arteries rupture
aneurysms, damage to the cranial brain is often observed
nerves, most often the oculomotor, sometimes suffers
optic nerve or chiasm. When an anterior aneurysm ruptures
section of the circle of Willis due to vasospasm
there may be signs of focal lesions
basin of the anterior cerebral arteries - leg paresis, changes
psyche of the “frontal” type, the presence of grasping
reflex, etc. When a middle aneurysm ruptures
cerebral artery focal symptoms are also common
in the form of hemiparesis, etc. The presence of these symptoms is due to
ischemia of the medulla, sometimes with the formation
cerebral infarctions due to prolonged angio-
spasm. With convexital localization of subarachnoia
distant hemorrhage may be observed focal
epileptic seizures, transient monoparesis, aphasia
and other disorders of cortical functions.
Often with subarachnoid hemorrhages there are
mental disorders - delirious-hallucious
nauseous state, mnestic and other disorders.
In many cases there is stagnation
in the fundus, they sometimes appear very quickly -
after a few hours or days; are often noted
hemorrhages in the retina, in the sclera. In the first days of the disease
almost all patients have a fever
(usually up to 38-39°C), changes occur in
blood in the form of moderate leukocytosis and neutrophilia.
In severe cases, subarachnoid hemorrhage
accompanied by severe disturbances of vital
functions - cardiovascular activity and respiration.
Cerebrospinal fluid usually leaks
under elevated pressure, it is detected on the first day
an admixture of fresh blood, on the 3rd-5th day - xantho-
chromium. From the 3rd day, neutrophilic pleocytic
tosis, later, from the 5-6th day, the number of lymphocytes increases
and mononuclear cells. A spinal tap is performed
with the patient lying down, the fluid is released
https://www.youtube.com/watch?v=IBPdOwK_kJI
carefully (3-10 ml), preventing with a mandrel
hemorrhages are observed more often with cerebral aneurysms
vessels; used for diagnosing aneurysms
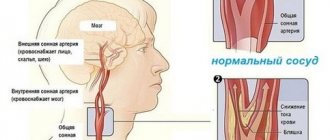
Focal brain lesions are caused by damage to blood vessels, which lose elasticity with age. For some, this manifests itself minimally, while for others, the disorders develop into a pathological form. Can appear:
- High blood pressure caused by a lack of oxygen due to the degenerative state of the cerebral vessels.
- Epileptic seizures, during which a person should not put metal objects in his mouth, pour water on him, hit him on the cheeks, etc.
- Mental disorders, memory impairment, distorted perception of reality, atypical behavior.
- Stroke or pre-stroke condition, which can be detected on CT or MRI.
- Increasing throbbing headache in the back of the head, eye sockets, superciliary areas, radiating across the surface of the entire skull.
- Uncontrolled muscle contractions, tremors of the limbs, chin, eyes, neck.
- Ear noise, ringing, congestion leading to nervousness.
- Regular attacks of dizziness leading to nausea and vomiting.
- Photophobia, decreased hearing acuity, blurred vision, double vision, noticeable blurred vision.
- Constant fatigue, apathy.
- Slurred speech.
- Sleep disturbances.
- Muscle paresis, pathological reflex reaction of the limbs.
Many people ask what diseases are caused by focal brain damage, what it is, and why it occurs. It is known that the causes of this disorder may lie in:
- Vascular disorders associated with natural aging, cholesterol accumulations in the walls of blood vessels.
- Osteochondrosis of the neck.
- Oxygen starvation.
- Neoplasms.
- Injuries, open and closed head injuries (age is not important here).
Conventionally, all clinical symptoms can be divided: general, focal neurological, and mental. General symptoms include weakness, drowsiness, increased body temperature, chills, decreased appetite, headaches, and dizziness. An experienced neurologist will be able to determine the site of damage in the brain with 90% accuracy based on the patient’s complaints and clinical symptoms.
If the focus is located in the cortex of the frontal lobe, then speech and its perception suffer, the tone of some muscles increases, a disorder in the movement of the eyes, head, and limbs occurs, and balance is lost when walking.
When the parietal lobe is damaged, the ability to read, write, count is impaired, and tactile sensitivity changes or is lost. The patient cannot correctly determine the position of his limbs in space.
Various visual impairments (changes in color and light perception, visual illusion, complete blindness) speak in favor of damage to the occipital lobe.
It is useful to read how cerebral microangiopathy manifests itself: causes, symptoms, consequences.
Lesions in the cerebellum affect balance and gait. In fact, in practice there are much more focal neurological symptoms: paresis, paralysis, impaired sensitivity of the limbs, fainting, tremors. Even with single focal changes in the substance of the brain, breathing problems, convulsions, and coma can occur.
Psychiatric symptoms accompany neurological symptoms but sometimes occur on their own. Mental disorders may include foolishness, depression, irritability, sleep disturbances, anxiety disorder, restlessness, panic attacks or aggression.
It should be noted that when diagnosing focal lesions, specialists need to be more careful, since the symptoms of focal pathologies are very diverse and often coincide with other neurological disorders. And an incorrect diagnosis always leads to incorrect treatment.
Despite this, it is also important for the doctor to know what problems the patient is experiencing, what complaints he has and what signs have already manifested themselves quite clearly.
So, the signs of focal brain lesions are:
- headaches, head throbbing, dizziness;
- increased blood and intracranial pressure, in other words, hypertension and hypertension;
- epileptic seizures;
- disturbances in the functioning of the sense organs - vision and hearing, tinnitus;
- the phenomenon of photophobia or increased sensitivity to light;
- apathy, indifference to everything around;
- chronic fatigue, decreased performance, loss of interest in the environment;
- nausea and vomiting;
- frequent fainting;
- speech defects, handwriting disorders;
- muscle weakness, loss of tone, subsequent atrophy;
- sleep disturbance, loss of appetite;
- convulsions, tremors of limbs;
- irritability, mental and emotional disorders, stress;
- muscle paralysis;
- breathing problems;
- loss of some reflexes.
All these symptoms are of a general nature, that is, some may manifest themselves as clearly as possible, while others may remain on the sidelines. If you pay attention to them, it will become clear that they are all somehow connected with neurology, because in the process of focal pathologies, nervous tissues are affected, which can serve as a reason for disruption of autonomic functions, coordination of movements, etc.
Causes of GM damage
Focal lesions can be caused by a variety of reasons.
In case of focal lesions of the brain of a dyscirculatory nature, the cause may be a lack of nutrients caused by circulatory disorders (with ischemic heart disease, stroke and other pathologies). Often the cause of the disease is a neoplasm. It has a negative effect on neighboring areas of the brain, causing various changes in them, including the death of brain cells.
What else leads to illness?
Focal pathologies can be caused by traumatic brain injuries, hematomas, and edema.
The following can also lead to the development of lesions:
- Spinal pathologies. One of the most common causes is osteochondrosis, in which nerves and blood vessels are compressed. As a result, an insufficient amount of blood enters the brain, cell nutrition is disrupted, and lesions of the brain arise.
- Fractures of the cervical spine. Within the neck there are two large vessels. When fractured, they can be damaged (torn, compressed). Impaired blood flow in the cervical region leads to inhibited blood supply to the brain. As a result, cells suffer from a lack of oxygen and nutrients.
- Excess weight. This reason is considered secondary. Obesity can lead to impaired brain function. Obesity with lack of physical activity is especially dangerous.
- Atherosclerosis. With this pathology, cholesterol plaques form in the vessels. They clog the lumen of the vascular bed, which leads to a lack of nutrients.
- Endocrine pathologies.
Differential diagnosis
An important point is the differential diagnosis of dilated Virchow-Robin spaces and other brain pathologies.
Lacunar infarction
Criblurs, with their large size and fusion with each other, can be mistaken for a lacunar infarction. Often confusion arises due to the same localization - in the basal ganglia region.
The difference is that during a heart attack, the lesions usually exceed 5 mm in size. Also, the lesions are asymmetrical. An experienced radiology doctor will be able to distinguish using various imaging modes: T1, T2, FLAIR.
The differential diagnosis between an enlarged perivascular space and a stroke is important, since if left untreated, a more extensive brain catastrophe may subsequently occur with the formation of a neurological deficit.
Stroke treatment is carried out under the supervision of a neurologist.
Cystic periventricular leukomalacia
This disease occurs in premature babies due to impaired breathing. The brain suffers from oxygen deficiency and stroke lesions appear along the vessels, which are very similar to Virchow-Robin spaces.
In most cases, the disease does not require therapy. If the cysts reach large sizes, surgical removal is possible.
Multiple sclerosis
Foci of this demyelinating disease can be located in any part of the brain, including around the cortical vessels.
A distinctive feature is that in multiple sclerosis the lesions originate from the lateral ventricles, forming the so-called “Dawson's fingers”.
When clinical signs of multiple sclerosis are identified, DMT therapy is prescribed.
Cystic tumors
Often, dilated perivascular spaces may resemble a cystic neoplasm. In this case, the cyst has different intensity inside the neoplasm and accumulates contrast. In this case, you need to contact an oncologist and neurosurgeon.
Diagnostics
MRI allows you to determine the presence of a lesion, as well as conduct a comparative analysis of the obtained images with images of a healthy brain. On them, almost all lesions look like light spots of various sizes.
In addition, magnetic resonance imaging helps to accurately determine the number of lesions. Single changes in the brain are observed in all patients over the age of 50 years. In such cases, it is necessary to monitor the dynamics of the development of the lesion, as well as take measures to eliminate the causes of damage to the brain.
Prevention
How to prevent the above pathologies? It can be concluded that older patients are more susceptible to such diseases. Therefore, all people over 60 years of age need to regularly visit a neurologist and undergo an MRI examination of the brain.
It is also important to constantly monitor blood cholesterol levels and blood pressure. After all, diseases accompanied by pathological changes in the white matter most often develop against the background of atherosclerosis and hypertension.
Numerous lesions
Patients who have multiple lesions deserve special attention. They are a sign of a serious pathology and may even serve as a symptom of a brain tumor. In the early stages, such diseases can only be detected after MRI.
If it is necessary to study blood vessels, an MRI with contrast is prescribed. As a result of the injection of a contrast agent, the blood is painted a different color, which is reflected in special shades on MRI images. When analyzing them, the doctor sees how blood flows through the vessels, in what directions and whether there are damages, blood clots, or aneurysms.
When expansion of perivascular spaces is normal
Perivascular canals can only be seen using MRI.
Often Virchow-Robin spaces are not visualized even on MRI images due to their small area. The resolution of the tomograph matters. A size of up to 2 mm is normal and occurs in all people.
Enlarged perivascular spaces are called criblures.
Signs of dilated perivascular spaces on MRI
Their increase does not always indicate pathology. The mechanism of their expansion is still being studied. This is possible due to inflammation of the vessel wall, when the latter becomes thinner and becomes more permeable. The released liquid causes the criblure to expand. Another reason is a violation of the flow of cerebrospinal fluid, and another is the lengthening of blood vessels.
Scientists and practicing doctors have not come to a consensus on what is considered pathology and what is not. As a rule, fixation of spaces on MRI images in people of the older age group is a variant of the norm.
Criblures in the brain are often found in children in the first year of life.
They are usually localized in three areas:
- Along the course of the lenticular arteries supplying blood to the basal ganglia - the caudate nucleus, internal capsule, fence.
- Along the course of certain arteries that enter the brain from its outside , and not like most branches of the carotid and vertebral arteries from the inside.
- Along the vessels supplying the midbrain (posterior thalamoperforating and median mesencephalothalamic arteries).
Appear symmetrically. Most often, expansion of the perivascular spaces occurs in the region of the lower basal structures and very rarely in the cerebellum. As a rule, the dimensions do not exceed 5 mm.
CSF flows in the perivascular canals, so on MRI the criblures have the same plane as the latter and appear isodense.
There are 2 projections in which MRI images of the brain are usually taken: frontal and axial. In the first case, the expanded spaces appear in the form of stripes, and in the second they take on a round or oval shape corresponding to the cross-section.
The use of various MRI modes, especially T-2, helps in diagnosis. In this mode, Virchow-Robin spaces do not have a darker rim around the filled area, which indicates that this is part of the subarachnoid membrane, and not the wall of a cavity, lesion or neoplasm.
Criblurs on MRI images
Types of lesions
There are several types of focal GM diseases. The most dangerous are neoplasms. In the early stages, brain tumor symptoms can be confused with migraines and other illnesses. But with growth, the functioning of neurons deteriorates and signal transmission to the brain is disrupted. If the tumor grows, it begins to invade more and more new territories, and the clinical picture begins to increase.
Another type of focal disease is a cyst (a small cavity with liquid contents). For a long time, cavities do not make themselves felt until they begin to grow and increase in size. Despite the fact that they are not prone to growth and increase in size, like neoplasms, they are also considered a foreign body. Cysts can cause compression of blood vessels, which complicates the flow of blood to the brain.
Treatment of focal ailments
Each specific disease has its own treatment characteristics. Any focal damage to the cerebral cortex leads to serious consequences. However, therapy should be carried out taking into account the cause that led to the onset of the disease.
The doctor may include vitamins, painkillers, sedatives and other drugs in a comprehensive treatment regimen. Soothing baths, physiotherapy, and lifestyle changes play an important role.
Brain diseases are always quite serious. Of course, any problems in the body require attention, but in the case of the brain, even the smallest problem must be carefully considered.
One of the brain diseases is gliosis. This term refers to the process of replacing dead nerve cells with special glial cells. They protect the nervous system, help neurons transmit impulses and form new connections.
Their number is 10 times higher than that of other cells of the nervous system, but it is the accumulation of glia in a certain area of the organ that is called cerebral gliosis.
Perivascular zone, its structure and functions
Virchow-Robin spaces (VRO) are slit-like formations surrounding the cerebral vessel along its path from the subarachnoid region into the brain tissue.
There is still no single point of view on what perivascular spaces are. Most scientists believe that this is the area between the middle (arachnoid, arachnoid) and inner (pia) meninges. This area normally surrounds the substance of the brain and, together with the vessels, is drawn into the brain, surrounding them. The subarachnoid region, located in the cerebral cortex, is called the Virchow-Robin space.
There is no single point of view; only arteries or also veins surround the perivascular spaces. It was revealed that they continue to the level of capillaries.
It is believed that this formation is involved in the movement of cerebrospinal fluid and ensures the exchange of necessary substances between cerebrospinal fluid and neurons.
Another function is to isolate intravascular blood from brain tissue. The blood contains a number of toxic substances that normally should not enter the brain substrate due to the presence of the blood-brain barrier. Additionally, toxins are absorbed within the perivascular region.
Another challenge is immune regulation.
Causes
Gliosis of the white matter of the brain interferes with the full functioning of the nervous system, but it is necessary to fight this disease not directly, but by investigating its cause.
Basically, the catalysts for the appearance of glial accumulations are infectious or other causes of diseases of the nervous system, such as:
- hereditary diseases associated with the death of neurons;
- multiple sclerosis - destruction of nerve tissue fibers in the brain and spinal cord;
- tuberous sclerosis is a genetic disease in which benign tumors develop;
- epilepsy;
- trauma at birth (in infants);
- head and back injuries;
- high blood pressure and encephalopathy;
- cerebral edema;
- chronic or acute cerebrovascular accident (CVA/CVA);
- hypoxia – acute lack of oxygen in tissues;
- neuroinfections such as leukoencephalitis, encephalomyelitis, etc., caused by viruses or bacteria;
- low blood sugar;
- high consumption of animal fats;
- previous operations;
Glial accumulations are often observed in athletes who have suffered head concussions, as well as in those who are exposed to bad habits such as alcohol and drugs that contribute to the destruction of neurons. These changes may also occur in patients taking narcotic-based medications.
Causes
Enlarged perivascular Robin-Virchow spaces are not always a sign of pathology. This diagnostic result is also observed in completely healthy people. Most often, expansion of criblures is observed in elderly patients and is associated with age-related changes in the brain.
However, in some cases, dilated perivascular spaces may be a sign of the following diseases and conditions:
- brain atrophy;
- leukoaraiosis;
- cerebral ischemia (including cerebral infarction);
- disseminated encephalomyelitis.
Symptoms
Gliosis is a disease that can masquerade as a number of problems associated with the cardiovascular and nervous systems. Its most common symptoms are:
- constant headaches, migraines, dizziness;
- sudden changes in blood pressure;
- the appearance of problems with vision or hearing;
- memory and attention disorder;
- the appearance of convulsions, paralysis.
These problems can also appear in a number of other diseases that are completely different from gliosis, so for an accurate diagnosis you need to contact a specialist. Sometimes cerebral gliosis is detected already with an MRI of the brain, although the patient does not feel any negative changes.
The distribution of glial cells occurs in different ways. Depending on their location in the body, their foci are divided into:
- anisomorphic – irregular order of glia distribution;
- isomorphic – correct formation of glial cells;
- marginal – growth of glial cells in the intrathecal spaces of the brain;
- diffuse – accelerated spread of gliosis both in the brain and spinal cord;
- perivascular or vascular - gliosis located along the vessels. Most often it appears after atherosclerosis.
- fibrous – processes of glial cells exceed the size of their bodies;
- marginal - glial elements are located on the surface of the brain;
Foci of gliosis according to their size can be divided into single, few (up to 3 foci) and multiple. Accordingly, isolated areas of development of glial cells can occur in old age, when the body can no longer carry out proper tissue regeneration, for example, the spread of gliosis in the frontal lobes.
General and focal neurological symptoms
focal lesions Focal brain lesions can be caused by trauma, infectious disease, vascular atrophy and many other factors.
Often, degenerative changes are accompanied by problems associated with disruption of normal vital functions and coordination of human movement.
MRI for focal brain lesions helps to identify the problem in the early stages and coordinate drug therapy. If necessary, based on the results of the examination, minimally invasive surgery may be prescribed.
All disorders of brain activity are reflected in the natural daily functions of human life. The location of the lesion affects the functioning of internal organs and the muscular system.
Changes in vascular genesis can lead to mental disorders, cause increased blood pressure, stroke and other unpleasant consequences. On the other hand, subcortical lesions may not have clinical manifestations and be asymptomatic.
One of the obvious signs of the presence of a focal lesion is:
- Hypertension - a lack of oxygen supply to the brain caused by vascular dystrophy leads to the brain speeding up and increasing blood circulation.
Signs of single focal changes in the brain substance of a dyscirculatory nature on magnetic resonance imaging mean that the patient has certain deviations in the functioning of the vascular system. Most often this is associated with hypertension. The diagnosis and explanation of the study results will be provided by the attending physician.
The picture of focal changes in the substance of the brain of a dystrophic nature is observed, according to various sources, from 50 to 80% of all people as they age. Ischemia, as a result of which normal blood supply is stopped, causes provoking changes in the soft tissues. Resonance imaging helps to identify the causes of disorders and conduct a differential analysis of the disease.
Small focal changes that do not cause concern at first can eventually cause a stroke. In addition, foci of increased echogenicity of vascular origin may indicate an oncological cause of the disorders.
Timely identification of the problem helps prescribe the most effective therapy. A focus of dyscirculatory origin, clearly visible on MRI, may indicate the following pathologies:
- In the cerebral hemispheres - indicates the following possible causes: blocking the blood flow of the right vertebral artery due to a congenital anomaly or atherosclerotic plaque. The condition may be accompanied by a herniated cervical spine.
If the MRI report indicates the diagnosis: “signs of multifocal brain damage of a vascular nature,” this is a reason for certain concerns. The attending physician will be required to establish the cause of the changes and determine methods of conservative and restorative therapy.
On the other hand, microfocal changes occur in almost every patient after 50 years. The lesions are visible in angiography mode, if the cause of occurrence is disturbances in genesis.
If a dystrophic focus is detected, the therapist will definitely prescribe a general medical history of the patient. In the absence of additional reasons for concern, it will be recommended to regularly monitor trends in the development of pathology. Substances may be prescribed to stimulate circulation.
Changes in the brain substance of a dyscirculatory-dystrophic nature indicate more serious problems. Pressure and lack of circulation can be caused by injury or other causes.
Signs of small-focal brain damage with a vascular etiology of moderate expansion can cause the diagnosis of encephalopathy, congenital and acquired. Some medications can only make the problem worse. Therefore, the therapist will check the relationship between medication and ischemia.
Any pathological and degenerative changes should be well studied and tested. The cause of the focal lesion was determined and, based on the MRI results, prevention or treatment of the detected disease was prescribed.
Foci of gliosis of vascular origin in the brain lead to disturbances in brain activity and tissue atrophy. Treatment of cerebral gliosis is impossible, because it is not an independent disease, but a consequence of the appearance of various pathological processes in the body.
Foci of gliosis are a kind of scar that tends to expand in the area of damage. This is due to the influence of aging processes on neurons, which are subsequently replaced by glia, which leads to the formation of spongy structures in the brain.
Gliosis of the brain and its essence lies in the fact that in the area of passive neurons that have died due to any specific reason, neuroglial cells begin to grow. They represent a specific scar in the brain area, their treatment is problematic. When gliosis is detected at a relatively young age, it is recommended to look for the cause of this phenomenon in order to begin treatment.
Glial cells located in the brain support and ensure the normal functioning of neurons. As already noted, gliosis is not an independent diagnosis, but rather a consequence of various disorders and abnormalities associated with brain atrophy or necrotic tissue phenomena. Single supratentorial foci of cerebral gliosis of vascular origin - arise as a result of birth trauma or natural aging processes.
Dizziness and seizures - if the cause of gliosis is trauma or surgery, a convulsive symptom appears in the postoperative period. The consequences of gliosis are primarily associated with the localization of the catalyst that caused the pathological changes. Tomography – brain examinations using CT and MRI are generally accepted examination standards.
Only in this case is a complete cure for the disease possible. The size of glial foci is a specific value that can be easily calculated using CNS cells and glial cells per unit. volume. It follows from this that the quantitative indicators of such growths are a value that is directly proportional to the volume of healed damage in the soft tissue area.
Such a pathological process is most often determined by chance during an examination, because clinical manifestations of the changes that have occurred in the body may be absent. It is these changes that cause the appearance of such aging problems as deterioration of coordination of movements, memory and slowness of reactions.
Such changes in the body lead to the aging process. This fact has not been scientifically proven, but has been demonstrated in laboratory conditions. A similar reason for the development of the disease occurs no more often than in 25% of cases with an autosomal recessive type of inheritance. In the first months of life, this pathology does not affect the development of the newborn.
Most often, a diagnosis such as gliosis is made unexpectedly, during an examination for other indications. MRI gives very clear answers about how long ago the foci of gliosis appeared, which greatly simplifies the search for the causes of the disease.
Gliosis is a fairly serious pathology, so it is recommended to start fighting the disease as early as possible, eradicating the causes of its development. Gliosis is not an independent disease, but a specific compensatory reaction of the brain substance to the death or damage of neural connections.
Depending on how common gliotic changes are and what their nature is, 7 types of process are distinguished. The first of these is a condition called anisomorphic form, in which cellular-type elements are formed in greater numbers than fibrous ones. There is also a fibrous form, in which the fibrous compounds in the intercellular component take advantage.
In the vast majority of cases, when cerebral gliosis is not provoked by a chronic neurological disease (multiple sclerosis), manifestations are 100% absent. Multiple foci of gliosis in the brain are nothing more than pathological proliferations of glial cells replacing damaged neurons. Treatment of cerebral gliosis of vascular origin is carried out with the help of agents that strengthen the walls of the arteries and restore their elasticity.
“Nature abhors a vacuum” and forms foci of gliosis in the white matter of the brain. Glia are one of the types of tissue in the structure of the white and gray matter of the brain. which normally takes up to 50%.
Role of glia
It is like a support and auxiliary basis for neurons. Glial cells cannot perform the function of neurons as cells of higher nervous activity, but they can provide neurons with normal functioning and the occurrence of biological life-sustaining reactions in them.
In case of injuries and any pathologies of the brain substance, which are accompanied by the death of neurons, gliosis is triggered. Glial cells grow and occupy the space emptied by dead neurons, thus helping to optimize the vital activity and functioning of surviving neurons.
That is, the focus of gliosis in the brain resembles a scar of connective tissue in other organs. There are single and multiple foci of cerebral gliosis. Naturally, the smaller the number of healthy neurons and the more glial foci, the lower the possibilities of higher nervous activity in a person.
Important! Gliosis is always secondary.
It cannot be called a typical disease, since in case of injury, focal gliosis of the brain ensures the vital activity of the surviving neurons and the constancy of the functioning of the metabolic processes necessary for the continuation of life in them.
- Hypertension - a lack of oxygen supply to the brain caused by vascular dystrophy leads to the brain speeding up and increasing blood circulation.
- Epileptic seizures.
- Mental disorders - occur with pathology of the subarachnoid spaces, accompanied by hemorrhage. At the same time, congestion in the fundus may occur. A characteristic feature of the pathology is the rapid formation of darkening, burst vessels and retinal rupture, which makes it possible to determine the probable location of the focal lesion.
- Strokes - clearly defined focal changes in the brain of a vascular nature on MRI make it possible to establish a pre-stroke state and prescribe appropriate therapy.
- Pain syndrome - chronic headaches, migraines may indicate the need for a general examination of the patient. Ignoring symptoms can lead to disability or death.
- Involuntary muscle contractions.
Diagnostics
Detection of this disease is impossible without the use of special electronic equipment. Diagnosis can be carried out using one or more methods:
- Magnetic resonance imaging (MRI) – obtaining images of internal organs and tissues by exposing the object of study to electromagnetic waves. This method is used to find abnormalities in the functioning of organs, tumors and improper tissue regeneration;
- computed tomography (CT) – obtaining images of internal organs using x-rays and subsequent data processing on a computer. It helps to identify changes associated with blood vessels, for example, obstructed blood circulation, thrombosis, etc.;
- electroencephalography (EEG) - measurement of brain activity using electrodes and computer data processing. It is applicable when it is necessary to record problems of the nervous system, such as seizures or epilepsy.
All these methods are applicable in specialized clinics equipped with modern medical devices.
Microangiopathy of the brain - what it is, causes, diagnosis and treatment
Many have heard of, and some have even encountered, such a disease as cerebral microangiopathy.
What is it? This is a pathological process that affects capillaries and small vessels, acquiring a chronic form. Blood circulation in the brain is impaired.
Since oxygen and glucose are responsible for normal blood flow, a long-term lack of these substances leads to disruption of the small vessels of the brain.
Kidney pathology can cause a moderate edematous syndrome, in which there will be a situation associated with the expansion of the spaces under the meninges. Sometimes this may be due to poisoning with heavy metal salts. Chronic alcohol intoxication may also be a cause.
https://www..com/watch?v=https:tv..com
Of course, all these conditions are more typical for adults. In children, the predominant causes are congenital anomalies. The cause may also be birth trauma, which disrupts the circulation of fluid in the cranial cavity.
Causes of conditions associated with expansion of the subarachnoid space
All causes can be either congenital or acquired. In the first version, the pathology concerns infants. As for the second option, people of different age categories are susceptible to this. The following situations can lead to such conditions:
- Processes associated with inflammation of the meninges. We are talking about meningitis, meningoencephalitis, arachnoiditis. Moreover, all of them can be caused by both infectious and non-infectious causes.
- Traumatic injury to the skull and brain.
- Defects in the development of the central nervous system.
- Processes associated with hemorrhage localized under the meninges.
- Brain swelling.
The manifestation of pathology in children varies and is determined by the severity of the process. You can suspect the presence of such a condition based on the following signs:
- In response to light and noise stimuli of medium intensity, the child responds with an extremely negative reaction.
- Such children experience frequent regurgitation.
- The child is excessively restless and has sleep disturbances.
- The pupils of the left and right eyes are different in size, and strabismus may occur.
- The size of the head clearly does not correspond to his age.
- The fontanel overgrows very slowly.
- The child often shudders, and tremor of individual parts of the body can be observed objectively.
As you can see, all these symptoms do not have any specificity and it is impossible to establish an accurate diagnosis using them alone. It is necessary to contact a pediatrician who will refer the child for a consultation with a pediatric neurologist.
As for adults, the dominant symptom will be headache. It can have varying degrees of intensity. It also differs in its duration. Dizziness, nausea, and inability to fully perform your professional duties with high quality may occur. The headache is especially severe in the morning.
At the peak of pain, the patient feels a pronounced pulsation. Sometimes vomiting occurs. Patients are restless and anxious. As intracranial pressure increases, headaches become more intense. Sleep is disturbed. Even if the patient manages to fall asleep, his sleep is intermittent and with obvious signs of anxiety. During the day, patients, on the contrary, show severe drowsiness.
This condition cannot continue indefinitely, and a moment comes when the symptoms characteristic of encephalopathy become clear. This is due to dystrophic changes in the cerebral cortex.
Memory becomes worse, visual disturbances are observed, and the level of intelligence decreases. Patients constantly feel severe fatigue. Characterized by endless repetition of headache attacks.
If the perivascular spaces of the basal ganglia are expanded, changes in gait may be observed, coordination of movements may be significantly impaired, and fine motor skills may be impaired. As a result, ability to work and activity in lifestyle are impaired.
Characteristic signs of microangiopathy
This brain pathology occurs as a result of disruption of the smallest vessels. This does not appear immediately, so it is very difficult to diagnose such a disease at an early stage.
Cerebral microangiopathy mainly occurs in older people. Those suffering from Alzheimer's disease are a particular risk group. With this disease, amyloid (glycoprotein) begins to accumulate on the walls of the veins. It is also worth noting that the pathology is difficult to diagnose and treat.
Lenticulostriate microangiopathy often affects children and is not a disease, but a feature of the circulatory system. Constant monitoring is required.
Diabetic microangiopathy occurs due to poor circulation in the brain, which provokes diabetes.
Hypertensive microangiopathy is caused by a disruption of the circulatory system that occurs due to hypertension. It is necessary to keep blood pressure under control and avoid sudden jumps.
Clinical manifestations of the disease depend on the specifics of organs and tissues, damage to which occurred under the influence of certain external factors. Patients most often complain of pain and burning in the legs, decreased vision, bleeding from the stomach and nose, the development of intermittent claudication, dry skin of the feet, and hemoptysis.
Thus, the following signs of microangiopathy are distinguished:
- the integrity of small vessels is compromised;
- renal failure develops;
- red blood cells are damaged;
- the blood clotting process is disrupted;
- there is a high probability of subcutaneous hemorrhages.
Inflammation as the main cause
Inflammations associated with both the membranes and the brain itself lead to the formation of adhesions in the cranial cavity. Naturally, this disrupts the circulation of cerebrospinal fluid, complicates its outflow and leads to the formation of hydrocephalus. This, in turn, causes the expansion of not only the ventricles of the brain, but also the subarachnoid space.
When inflammation occurs, all pathomorphological and pathophysiological changes associated with it come to the fore. The permeability of the vascular walls increases significantly.
The liquid part of the blood freely penetrates into the space between the cells, which forms swelling. In addition, the production of liquor itself increases significantly.
Pathomorphologically, in this phase one can observe thickening and congestion of the meninges and expansion of the space under the meninges.
Symptom complex of expansion of perivascular spaces
The development of microangiopathy occurs against the background of other diseases. This could be diabetes mellitus, oncology, liver pathology, hemolysis.
https://www..com/watch?v=ytadvertise
Among the main reasons are the following:
- viral infections (measles, rubella);
- pathologies that contribute to blood damage;
- diabetes;
- hypertension;
- elderly age;
- hereditary pathologies that cause vascular tone;
- various injuries;
- severe intoxication;
- abuse of bad habits.
Most often, pathology develops as a result of the following processes:
- Necrosis is the death of tissues and cells of the body.
- Hyalinosis is a lack of protein due to hyaline deposition.
- Increased vascular permeability. As a result, the fibers and structural elements of connective tissue undergo irreversible changes.
- Thrombosis, characterized by the formation of a blood clot in the lumen of a vessel, resulting in impaired blood flow.
- Dysfunction of the vascular endothelium, which leads to their spasm. In this condition, the production of antithrombin and prostacyclin decreases, and the concentration of thromboxane increases.
Microangiopathy of the brain has the following symptoms: the patient begins to complain of memory impairment, clouding of consciousness, causeless weakness and headaches.
They appear due to the fact that blood circulation is disrupted in the capillaries of the brain.
The resulting damage to the walls of small vessels activates the oxidative processes of lipids, free radicals are formed, which have a destructive effect on brain cells.
As the disease progresses, the patient becomes inattentive and forgetful. He develops an unsteady gait, convergence disorder, pupil diameters become different, and visual functions deteriorate. In addition, frequent nose and stomach bleeding, discomfort in the legs at rest, dryness and peeling of the skin of the feet, and blood clots in the urine appear.
Diagnostics
If there is a suspicion of brain pathology, it is important to diagnose where the foci of microangiopathy are located and what is the degree of damage to the vascular walls. For this, the following diagnostic methods are used:
- MRI of the brain;
- nuclear magnetic resonance;
- Doppler ultrasound.
To get as much information as possible, they use a fairly safe procedure for the human body, such as MRI of the brain, the price of which is a little steep.
This diagnostic method is considered the most popular.
It allows you to identify signs of the disease such as cerebral atrophy, leukoaraiosis, expansion of perivascular spaces, microscopic hemorrhages, lacunar infarctions.
The magnetic nuclear resonance method allows one to study the brain tissue itself and the vascular network. In this case, signs of arterial hypoplasia are clearly visible. Foci of infarctions that arise due to vascular occlusion, cerebral hypoperfusion, and microscopic hemorrhages are easily visible.
The Doppler ultrasound method allows you to identify abnormalities in blood vessels, blockages or narrowing of the lumen.
Diagnostic measures include an external examination with a thorough history taking. Laboratory and instrumental research methods help in diagnosis. This may include a general clinical blood test, ultrasound of the brain, CT or MRI. Neurosonography provides good assistance in making a diagnosis.
Treatment
Corrective treatment therapy depends on the cause of this condition. If the culprit is an infection, then a course of antibacterial therapy is prescribed (Sumamed, Zinnat, Flemoxin). If a tumor is present, antitumor drugs are prescribed (Cosmegen, Adriblastin).
Symptomatic treatment is carried out. In the presence of seizures, anticonvulsants are prescribed (Carbamazepine, Primidone). Measures are being taken to reduce swelling. In the presence of severe pain, analgesics and non-steroidal anti-inflammatory drugs (Spazmalgon, Pentalgin, Ibufen) are indicated.
If conservative therapy does not produce results, surgical intervention is resorted to. Shunting is used. By performing shunts, cerebrospinal fluid is diverted into the chest or abdominal cavity.
It should be said that often in adults, the expansion of the perivascular space can be asymptomatic. In this case, making a diagnosis is difficult.
Patients do not always understand when they are diagnosed with cerebral microangiopathy, what it is and whether it can be cured. The doctor usually prescribes complex therapy.
First of all, the patient must take medications that normalize blood pressure. To eliminate the lack of oxygen in the brain, antihypoxants are used, for example Emoxipin. It is also important to correct lipid levels using statins, fibrates, and bile acid sequestrants. These may be the following drugs: Atorvastatin, Simvastatin, Rosuvastatin.
Also, if microangiopathy is diagnosed, treatment should be carried out using nootropics that improve brain nutrition. These are Piracetam, Nootropil, Cerebrosilin, Encephabol. To normalize blood circulation, nicotinic acid preparations are used: “Picammilone”, “Xanthylone nicotinate”.
Conclusion
https://www..com/watch?v=https:accounts.google.comServiceLogin
Thus, we have analyzed a disease such as cerebral microangiopathy. What it is, you now know. This is a serious pathology that requires immediate intervention. The sooner it is found out where the focus of this disease is localized and what the degree of vascular damage is, the easier it will be to minimize the consequences of such a disease.
Source: https://firma77.ru/lakunarnoe-rashirnie-tserebralnykh-perivaskulyarnykh-prostranstv/
Prognosis (how long people with the disease live)
Brain gliosis can be caused by diseases associated with the cardiovascular and nervous systems, but it can also provoke the appearance of diseases of this nature. Regardless of age, both adults and children have the same conditions for dealing with this problem.
But as a rule, such people do not live more than 2-3 years.
Of course, only a doctor can determine how life-threatening glial tumors are, so first of all you should contact a specialized clinic as early as possible and identify the cause of their appearance, which will help you understand further actions and develop the necessary therapy.
Disseminated encephalomyelitis
Disseminated encephalomyelitis (DEM) is an acute pathology of the central nervous system. In this disease, the myelin sheath of nerve fibers is destroyed. The perivascular Virchow-Robin spaces are dilated due to damage to the white and gray matter. The MRI image shows foci of demyelination.
This pathology is of autoimmune origin. The clinical picture of the disease resembles signs of multiple sclerosis. Patients experience gait and movement disturbances, speech disorders, dizziness, and inflammation of the optic nerve.
Unlike many other demyelinating diseases, REM is treatable. Patients are prescribed corticosteroids to suppress the autoimmune reaction:
After a course of therapy, 70% of patients experience complete recovery. In advanced cases, patients may still experience the consequences of the disease: impaired sensitivity of the limbs, gait disturbances, and visual disturbances.