Indications for measuring CVP are:
— monitoring hemodynamic parameters (blood pressure in the pulmonary circulation);
— monitoring the effectiveness of infusion therapy.
There are no contraindications to the procedure in the presence of a subclavian catheter.
At the preparatory stage of measuring CVP, the necessary equipment is collected: a metal ruler, clean gloves, a patient monitoring card. Then the patient is placed in a strictly horizontal position without a pillow.
The manipulation itself consists of determining the zero reference level and directly measuring the central venous pressure.
Without closing the clamp, the intravenous administration system is disconnected from the bottle with the transfused solution. The system tube, starting from the subclavian catheter, is laid along the patient’s chest to the mid-axillary line at the level of the 2-3rd intercostal space (projection of the right atrium), the free end of the tube is raised vertically upward.
When blood from the subclavian catheter stops flowing into the system tube and its horizontal level is established (the boundary between the blood and the transfused solution), the height of the blood column is measured with a metal ruler from the mid-axillary line to the horizontal level.
During blood transfusion, CVP is measured after replacing it with saline solution, otherwise it is impossible to determine the horizontal level.
At the end of the manipulation, the intravenous infusion system is reconnected to the bottle with the transfused solution, having previously displaced the air from the tube. These measurements are entered into the patient's observation chart.
CVP is determined in millimeters of water and is normally 6-12 cm H2O. Art.
Didn't find what you were looking for? Use the search:
Best sayings:
For students, there are even, odd and test weeks.
9465 – | 7448 – or read all.
78.85.5.224 © studopedia.ru Not the author of the materials posted. But it provides free use. Is there a copyright violation? Write to us | Feedback.
Disable adBlock! and refresh the page (F5)
very necessary
Central venous pressure (abbreviated as CVP) is an integral level that characterizes indicators in the right atrium and, partially, in the pulmonary circulation at the moment of greatest relaxation of the muscular organ. That is, diastole. It is measured in mm, but not in the column of mercury, but in the water column.
An assessment of this level is not always necessary. There are several indications. All of them, one way or another, relate to urgent, critical conditions. For example, acute heart failure, cardiogenic shock and others.
In this case, the task of diagnosis is not only to determine the severity of the disorder, but also to evaluate the effectiveness of the infusion of drugs (infusion therapy).
CVP is a kind of marker, an indicator of myocardial contractility, pumping function, and hemodynamic quality. Any deviations indicate dangerous violations. In such a situation, the condition that caused the jumps in numbers is corrected.
Norms for adult patients
As for adequate indicators, they vary widely. According to studies, the normal central venous pressure in adults is from 30 to 90-100 mm water column.
Changes in value in one direction or another indicate critical disorders in the functioning of the cardiovascular system.
Measurements are carried out using invasive methods, by catheterization of large veins, therefore they do not resort to diagnosis without sufficient grounds.
The study has undeniable advantages: clarity of the indicator, monitoring of dynamic changes in real time, the ability to assess the quality of the treatment. But highly qualified personnel are required.
What does central venous pressure depend on?
Central venous pressure is determined by several factors:
- The volume of blood that is currently circulating in the body. If there is a lack of liquid connective tissue, after, for example, an injury, an open injury, a sharp drop in the level occurs, which indicates a decrease in the quality of the heart. The condition can result in the death of the patient if a transfusion is not performed.
Even after this, the level of central venous pressure rises and stabilizes gradually, not abruptly.
With an increase in the volume of circulating blood, against the background of pronounced edema, the pressure accordingly increases, which also does not bode well for the patient.
Such processes are also observed in a healthy person, but due to the body’s ability to self-regulate, no one notices this.
- Intensity of heart contractions. If the systole is full, the pumping function is normal, the liquid connective tissue is pumped sufficiently, the central venous pressure indicators are within adequate limits.
In critically ill patients, continuous measurement of the central venous pressure level allows one to notice the onset of a decline in myocardial contractility. That is, worsening heart failure.
Other methods do not provide such accurate results in real time.
- Central venous pressure depends on respiration, but the values in this situation vary within normal limits. We are not talking about a static number, but about a range that is accepted in medical practice.
Some lung diseases, especially those accompanied by respiratory failure, are accompanied by abrupt changes in central venous pressure, including outside critical conditions.
These include, for example. COPD, bronchial asthma, emphysema, bronchiectasis and others. The influence of pathologies of the respiratory system on the measurement results must be taken into account.
- Situational short-term changes are possible when using diuretics. Especially loop or osmotic diuretics, vasodilating medications.
There are also physiological changes in the level of central venous pressure. In the morning, the numbers are minimal, close to the lower limit of an adequate indicator; in the evening they are much higher.
The reason is muscle movements, tension (for example, straining when coughing, physical activity).
In bedridden patients, the changes are not so noticeable, but they also exist, because vascular tone and pressure in the right atrium deviate for natural reasons.
Procedure for measuring central venous pressure
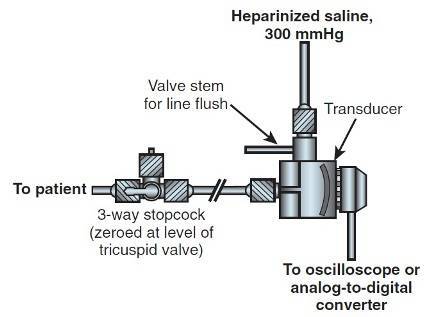
Although CVP can be determined using a manometric column assembled at the patient's bedside, the most common measurement method is an electronic sensor connected to a monitoring system.
Standard adapters have a valve for connecting an infusion system with saline solution, which makes it easy to flush the system.
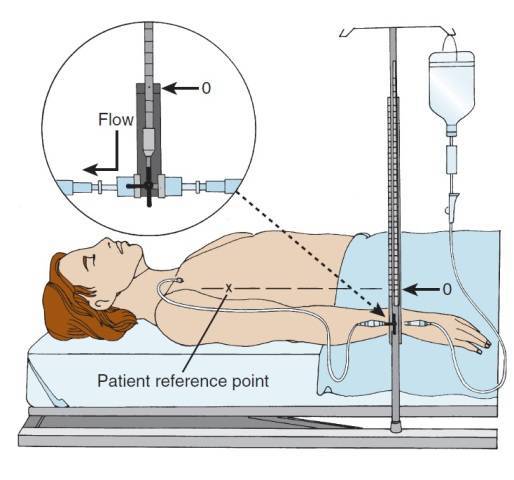
To carry out the measurement, attach the sensor to the patient's central venous access with a flexible but sufficiently elastic tube filled with saline solution. A three-way stopcock is located between the patient and the transducer to facilitate line flushing and calibration.
Remove any air bubbles from the system by opening the faucet and flushing the line with saline solution. Do not allow air bubbles to enter the patient's body. Even tiny bubbles remaining in the tubing will dampen the CVP waves and potentially cause errors in venous pressure measurements.
After the system has been flushed, the adapter (with sensor) is installed at the level of the patient's tricuspid valve. Calibrate the sensor to zero at the level of the tricuspid valve, which is projected onto the skin surface at the intersection of the midaxillary line and the fourth intercostal space. Open the adapter tap to connect the sensor to the patient’s venous catheter.
In patients with spontaneous breathing, readings are taken at the end of a normal inspiration. If the patient is on positive pressure ventilation, central venous pressure changes during the respiratory cycle, increasing with inspiration and decreasing with expiration. In these patients, readings are taken at the end of expiration.
Thus, both during spontaneous breathing and during mechanical ventilation, it is useful to estimate the average CVP value.
To ensure optimal measurement, the patient should be in a supine position. Whenever the patient moves, care must be taken to ensure that the sensor is calibrated to the patient's new position.
Indications for monitoring
There are not many reasons for measuring central venous pressure. These are always life-threatening conditions. Among them.
- Formation of acute heart failure. Without adequate therapy, the deviation in almost 95% of cases ends in the death of the patient within a matter of hours or days. The response to the therapy is needed immediately; the high speed of data acquisition is precisely what ensures control of the central venous pressure. Another indication for assessing the level is also partially touched upon here.
- Study of the safety and effectiveness of intravenous drugs for heart failure. Dysfunction of cardiac structures requires careful infusion of pharmaceuticals, because there is a change in hemodynamics and fluid volume. It is not known how the muscular organ will react even to such a minor intervention. In case of severe insufficiency, measurement of central venous pressure is indicated as part of the therapy and to determine its safety and effectiveness.
- Assessment of the state of the cardiovascular system, pumping ability of the myocardium after surgical interventions. It is not always required, usually if there is a tendency to cardiac dysfunction, a diagnosis of heart failure has already been made, or after surgical treatment of blood vessels and abdominal structures. The task is to prevent collapse and death of the patient from spontaneous changes.
- Massive blood loss. In such a situation, even the transfusion itself carries enormous danger. Sharp jumps in central venous pressure can lead to the opposite effect: a decrease in myocardial contractility, critical heart failure, or even stoppage of organ function (asystole). Pressure control is used as a monitoring method.
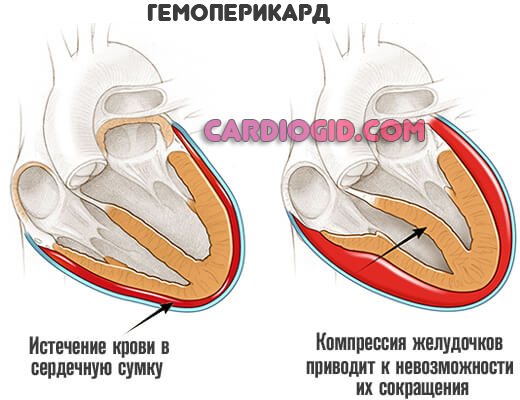
- Pericardial tamponade or suspicion of this condition. The essence is the accumulation of fluid or blood in a special membrane that encloses the heart itself. If the pressure in this bag exceeds the levels in the cardiac structures, the patient will stop and die. Careful monitoring can prevent such an outcome.
- Finally, it makes sense to carry out measurements during the acute phase of blood poisoning, sepsis. To avoid the development of a shock state or timely recognition of it.
Based on objective data, specialists adjust therapy and infusion volumes.
Normalization
Therapy, if arterial and venous pressure is disturbed, consists of eliminating the factors that caused such deviations. Increasing the reduced values consists of intravenous administration of crystalloid solutions. In addition, venotonics are used, which lead to an improvement in the tone of the vascular bed. With high central venous pressure, diuretic drugs are indicated, as well as drugs to eliminate inflammatory diseases and normalize the permeability and tone of the main venous vessels.
Algorithm for measuring venous pressure
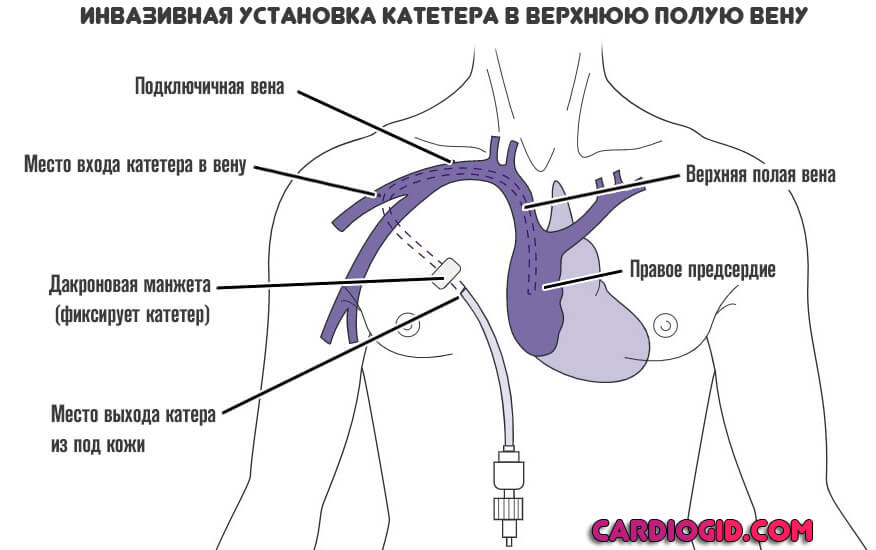
The study is carried out using an invasive method.
The list of actions is as follows:
- The doctor performs a puncture (puncture) of the jugular or superior vena cava using a special catheter with a tube leading to the system. This is a phlebotonometer or the so-called Waldmann apparatus. The device is relatively old, mechanical, but has great accuracy if installed correctly and all technological diagnostic features are observed.
- The catheter is passed to the right atrium and fixed in this state. Any movements are excluded to avoid dangerous consequences.
- A system for administering solutions and infusion therapy (dropper) is connected to the device. Then begin infusions of saline solution to fill the scale. The phlebotonometer itself is positioned so that the zero line, the beginning of the reference point, is at the level of the patient’s atrium. This will eliminate false indicators and errors.
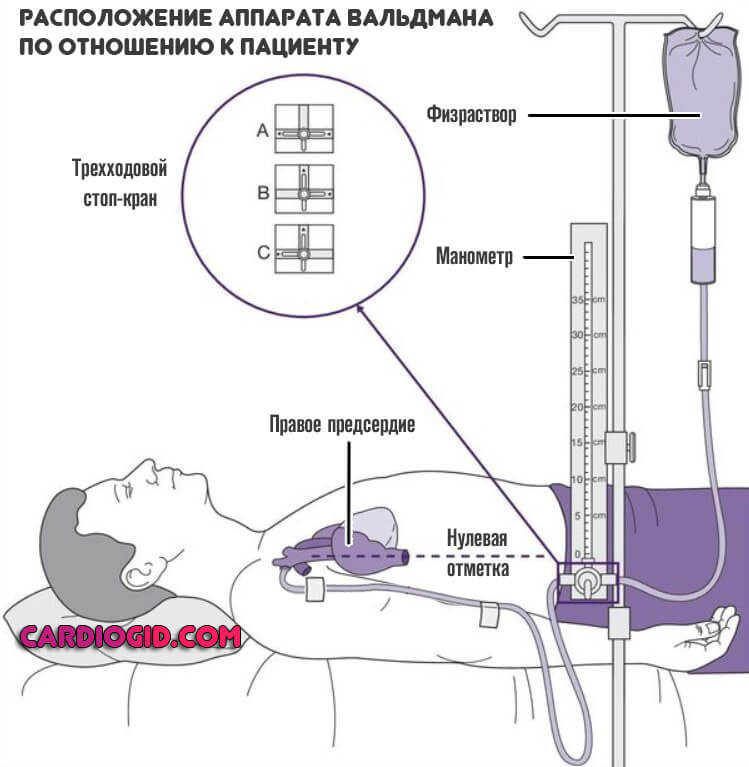
- After filling the flotonometer scale with saline solution, you can disconnect the tube leading to the infusion therapy system. After a few minutes, the device begins to show measurement results.
Although the measurement technique is old, it is still widely used in medical practice. The mechanical phlebotonometer is being replaced by electronic analogues.
They are able to build graphs and display visual indicators on the screen. In addition, they do not require such qualifications from personnel and are easier to install.
Otherwise, the algorithm for measuring CVP is the same: insertion of the catheter, fixing it, checking the technique of performing the procedure, obtaining and processing the results.
Reasons for the increase
Among the possible factors that provoke an increase in central venous pressure:
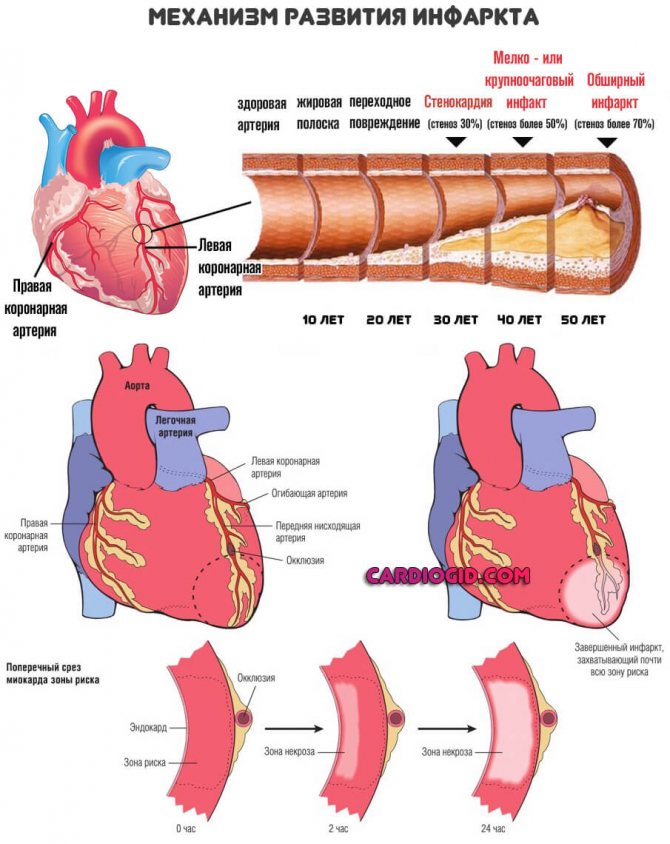
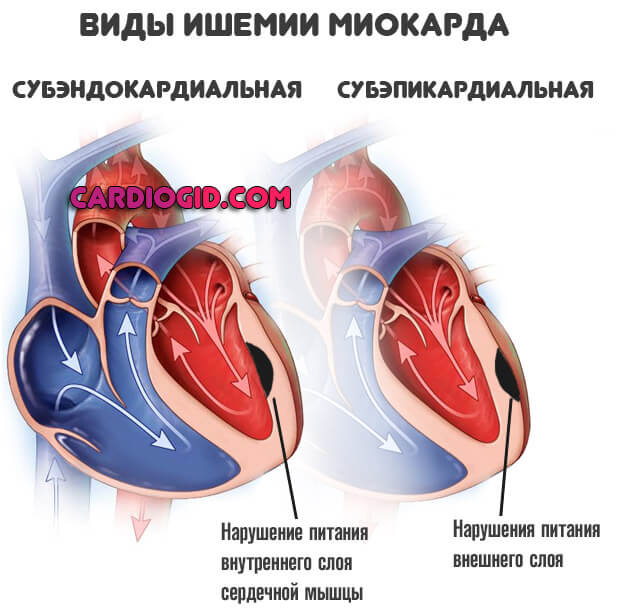
- Heart attack. Acute nutritional disorder of the heart muscle and myocardium. It is accompanied by a critical increase not only in central venous pressure, but also in blood pressure and general dysfunction of cardiac structures. Monitoring the indicator is not always necessary; the feasibility is determined by the doctor based on the current condition of the patient.
- Cardiogenic shock. Urgent, critical disorder. Mortality even with therapy is more than 90%. As is typical for pathology, it is extremely demanding on the quality of treatment and the professionalism of doctors; the slightest mistakes cost the patient his life. Measurement of central venous pressure in cardiogenic shock is always indicated.
- Pericarditis. An accumulation of fluid (hydropericardium) or blood (hemopericardium) in a special membrane, a sac, enclosing the heart. Develops as a result of trauma, medical diagnostic or therapeutic interventions. Spontaneous formation is also possible.
In any case, control of pressure in the right atrium and pulmonary circulation is a vital measure.
- Injuries of cardiac structures. Any, especially those accompanied by a violation of the anatomical integrity of certain tissues.
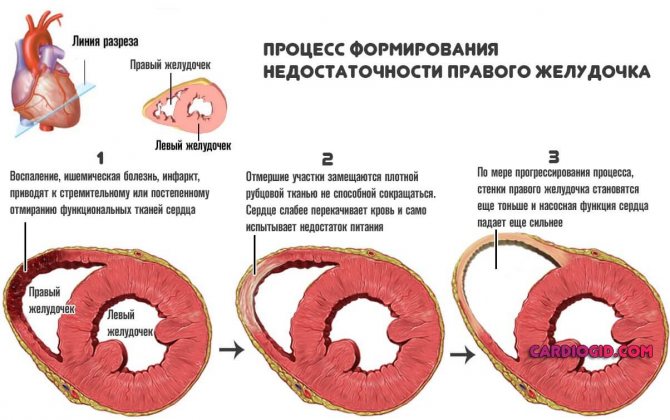
- Acute heart failure. For this disease, a dangerous sharp drop in myocardial contractility and the pumping function of the muscular organ is pathognomonic (typical).
As a result, insufficient trophism of all systems and tissues is formed. There is little nutrition, as well as oxygen, ischemic processes begin, including in the heart itself, which receives useful substances along with blood through the coronary arteries.
The venous indicator increases as a result of a reflex reaction, which the body is unable to correct.
Control of central pressure is also required during decompensation of chronic heart failure, when the disease becomes actualized and enters the acute phase.
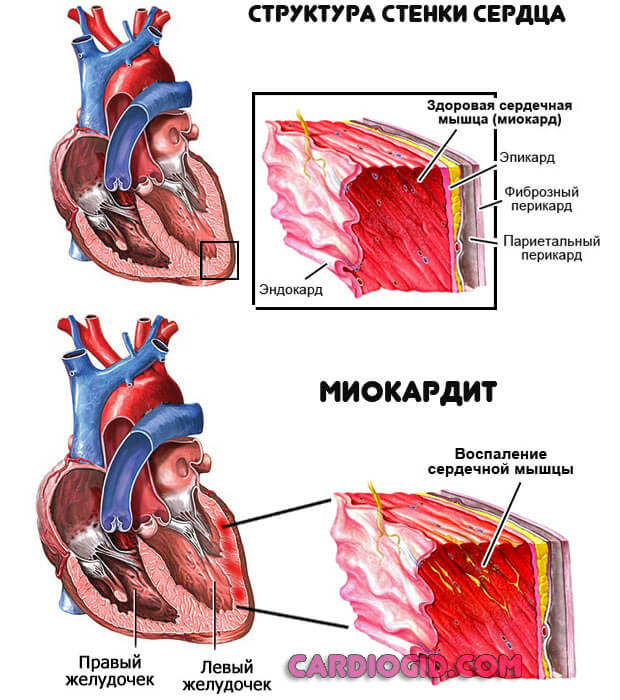
- Inflammatory lesions of the heart. In particular myocarditis. It is usually of infectious origin. An autoimmune variant is possible; the body attacks the cells of the muscular layer of the heart itself, as a result of an erroneous reaction or failure.
The condition is unstable and reacts unpredictably to the administration of intravenous drugs, therefore constant monitoring of objective indicators of central venous pressure is necessary.
These are the key reasons. However, the list is incomplete; there are other factors for changes in venous pressure. For example, severe arrhythmia with instability of the contraction frequency, brain injuries that affect the regulation of the functioning of cardiac structures.
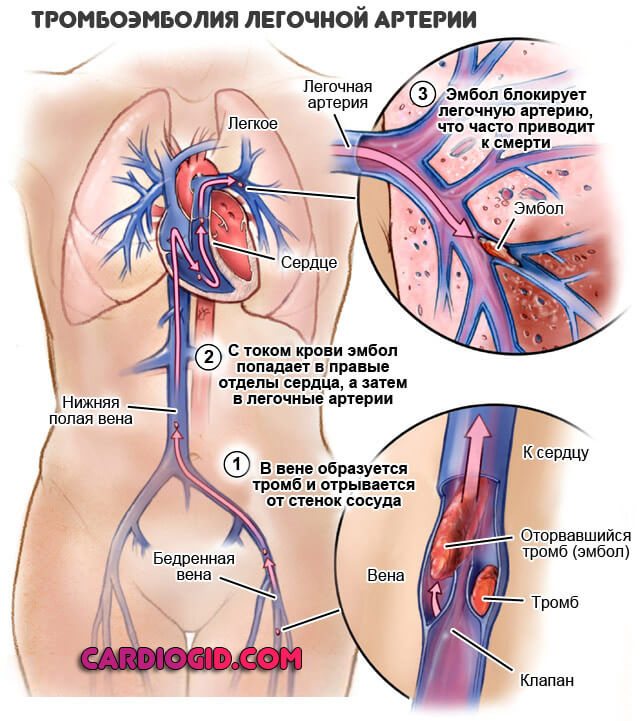
Provocation of the disorder is possible after the development of pulmonary embolism, pneumothorax, and injuries to the respiratory system. We are talking about exceeding the level, that is, from 90-100 mm aq. pillar or more.
Anything in this range is normal; dynamic changes are bound to happen throughout the day. They are not manifestations of pathology.
This must be taken into account during continuous measurements, including in bedridden patients.
Physiology
Simply put, CVP is the pressure exerted by blood on the walls of the vena cava. CVP reflects the pressure at which blood enters the right atrium, since the pressure in the great veins of the chest is almost equal to the pressure in the right atrium.
Central venous pressure produces two significant hemodynamic effects. First, pressure helps to fill the heart during diastole, a factor that helps determine cardiac output. Secondly, CVP has a significant impact on the amount of venous blood return to the heart.
The value of CVP is determined by the complex interaction of intravascular volume, the work of the right atrium and ventricle, the tone of the venous bed and intrathoracic pressure.
To accurately measure CVP, it is necessary to place a catheter in the vena cava or in the right atrium. It is also possible to use the femoral vein for measurement if there are no signs of increased intra-abdominal pressure.
Reasons for decreased central venous pressure
There are no fewer culprits for a drop in central venous pressure, but they relate to specific conditions.
- Cardiogenic shock. Oddly enough, this change can provoke both an increase and a decrease in CVP levels. Because the process itself is unstable, sharp jumps occur. This is extremely dangerous.
- Dehydration. Heavy. By restoring the volume of fluid circulating in the body, a complete cure can be achieved. But control of central venous pressure is needed to prevent acute heart failure or to stop it in time, in the initial period.
- Central venous pressure drops with other forms of shock: traumatic, anaphylactic. However, this is a consequence. When the primary cause is corrected, it is possible to stabilize the levels and bring the body back to normal. The advisability of installing a catheter and measuring CVP in such situations is controversial and is decided at the discretion of specialists.
- There may be problems in the functioning of the heart due to pulmonary embolism, acute respiratory failure. However, these are rather exceptions to the rule. Such pathological processes are mainly accompanied by jumps in central venous pressure with a parallel decrease in myocardial contractility.
Indications and contraindications for measuring central venous pressure
There are 5 main indications for CVP monitoring
- Acute circulatory failure.
- Massive blood transfusion for fluid replacement therapy.
- Gentle infusion therapy in patients with cardiovascular failure.
- Suspicion of cardiac tamponade.
- Infusion therapy in the complex treatment of severe sepsis.
The procedure is contraindicated when other resuscitation, treatment and diagnostic interventions through central venous access take precedence over the installation of a central venous pressure sensor.
A common misconception is that CVP consistently reflects the pressure in the left side of the heart. The indicator that best determines the pressure in the left atrium is the pulmonary capillary wedge pressure (PCWP). To measure it, pulmonary artery catheterization is necessary.
Central venous pressure is the most useful parameter in patients without a history of severe cardiac disease. Numerous studies highlight the apparent unreliability of monitoring right-sided hemodynamics in patients with underlying cardiac or pulmonary disease. However, CVP is an important indicator in assessing central hemodynamics.
Visual assessment of the patient
An increase in venous pressure can be accurately detected only by measurement results. For this you need a device, a phlebotonometer.
However, changes can be suspected through simple observation, assessment of some visual factors and palpation of blood vessels.
The following points are characteristic of an increase in the level of central venous pressure:
- Swelling of the veins in the neck. At rest, they look large, are clearly visible, and can be palpated without problems. In this case, there is no reaction to changes in body position; the reason is stagnation of blood, impaired outflow.
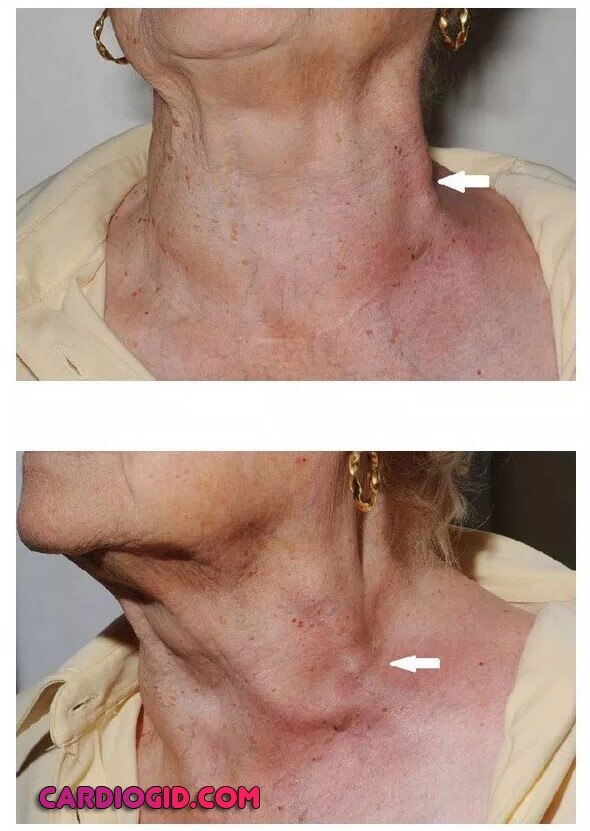
- When performing a special test with pressure on the right hypochondrium, the pulsation intensifies and signs of swelling become more noticeable.
These methods are not informative enough, but they are good for rough estimates.
A decrease in central venous pressure is detected somewhat more difficult, using a ruler.
The patient is placed on the couch with his head and torso elevated. Approximately 45 degrees so that the body is higher than the legs. Pulsation of the jugular veins (in the neck) should be visible at a level of 3.5-4.5 cm above the collarbone. Its absence indicates a low indicator.
As for the diagnosis of the underlying pathology, it is carried out urgently or begins after correction of the disease, partial stabilization of the condition.
The list of measures depends on the specific disorder. At a minimum, this is an ECG, blood pressure measurement, ECHO-CG, if necessary, coronography, MRI, duplex scanning, etc.
Methodology for determining the indicator
How to measure central venous pressure? The procedure is carried out using a Waldman medical device. It consists of a glass manometric tube and a scale with divisions from 0 to 250 units.

The most popular and accurate way to determine central venous pressure is using a Waldmann apparatus
The diagnostic procedure is performed as follows:
- The patient is placed on his back and his arm is slightly moved to the side.
- A special tube is filled with saline solution and the zero mark of the scale is determined.
- The patient's shoulder is secured with a tourniquet, then the cubital vein is punctured and the blood is released through the tube.
- Next, the tourniquet is removed, and after 1-2 minutes the level of measured pressure is determined on a scale.
Central venous pressure is measured only in the morning on an empty stomach. In addition, before the start of the session the patient must be in a horizontal position (20-30 minutes). Normal CVP values vary from 40 to 120 mm of water column. Significant changes may indicate serious problems and the need for proper treatment.
Treatment methods
Treatment depends on the specific condition. So, against the background of a decrease in the volume of circulating fluid or connective tissue, intravenous solutions are administered, and if necessary, blood transfusions are prescribed.
Cardiogenic shock and heart failure are corrected symptomatically. Then the disorder is corrected (after the patient has been removed from the emergency condition).
Pericardial tamponade requires puncture, drainage of the cavity, pumping out fluid, exudate or blood.
It is important to monitor CVP levels throughout the initial treatment, reducing or increasing the dose of the drug if necessary.
Treatment measures for deviations from the norm
The value of central venous pressure in combination with the assessment of other indicators helps to clarify the functional diagnosis and determine the nature and scope of treatment measures. Normal values of the parameter vary widely, and pressure is influenced by many different factors. The most important thing is to track the indicator over time.
In some cases, a test is performed with the introduction of a small amount of infusion solution and subsequent assessment of changes in pressure in the central veins. For example, if in response to the load the indicator increases by more than 5 cm of water. Art., the administration of fluids is stopped, since such an increase indicates impaired myocardial contractility. If the value increases by 2 cm water. Art. or less, then the decrease in pressure is probably associated with a decrease in the volume of circulating blood, and the administration of the solution should be continued. It is important to simultaneously evaluate blood pressure numbers, the volume of urine excreted, hemoglobin oxygen saturation and other indicators.
Correct interpretation of central venous pressure over time, together with other parameters, helps to avoid complications of inadequate infusion therapy. Giving too much fluid (overhydration) leads to increased levels, damage to the kidneys and other organs, and an increased risk of death.
Treatment of high or low pressure in the central veins is determined by the disease that caused the increase in the indicator:
- The presence of heart failure requires measures to restore the contractile function of the myocardium.
- Hypovolemia – a decrease in the volume of circulating blood in the body – is an indication for intravenous administration of fluids or blood substitutes.
- In case of shock, they strive to eliminate its cause and restore the functioning of vital organs.
- In case of cardiac tamponade associated with the accumulation of exudate in the pericardial cavity, a puncture is performed to remove excess fluid.

In patients who have undergone cardiac surgery, high central venous pressure may be caused by bleeding and cardiac tamponade.
Forecast
Prospects again depend on the primary disease and the quality of the therapy provided.
- Cardiogenic shock is fatal in most cases; heart failure ends in death in almost 45-60% of situations.
- Myocarditis, the accumulation of fluid, gives a mortality rate of about 25-30%. The same applies to a heart attack.
The numbers are very approximate. Specific forecasts depend on the situation.
In medicine, CVP is used to assess heart function in emergency conditions, the dynamics of the disorder, and study the quality of therapy.
Whether monitoring of the indicator is necessary is determined by the doctor based on the details of the clinical case.
Category: Nursing in critical care/Resuscitation and intensive care for acute cardiovascular failure
In intensive care patients, great importance is attached to the value of central venous pressure (CVP). It is not only its absolute value, normally from 90 to 120 mm, that matters. water Art., but also its change in dynamics
.
To measure central venous pressure, a Waldmann apparatus is used
. The main part of this device is a pressure gauge - a glass graduated tube with a diameter of 3 mm and a length of 40-50 cm. A rubber tube extends from the lower end of the pressure gauge, which is connected to a catheter located in the central vein (subclavian or jugular). The device is filled with sterile isotonic sodium chloride solution. The patient lies on his back in a strictly horizontal position. The term "CVP" refers to pressure in the right atrium. The projection of the right atrium corresponds to the border of the upper and middle third of the anteroposterior size of the chest in a lying person. At this level the zero mark of the pressure gauge is set. When connecting the Waldmann apparatus to a venous catheter, the fluid level in the manometer will show the CVP in mm. water Art..
See resuscitation and intensive care for acute cardiovascular failure
- Zaryanskaya V. G. Fundamentals of resuscitation and anesthesiology for medical colleges (2nd ed.) / Series 'Secondary vocational education'. - Rostov n/D: Phoenix, 2004.
- Barykina N.V. Nursing in surgery: textbook. allowance/N. V. Barykina, V. G. Zaryanskaya.- Ed. 14th. - Rostov n/d: Phoenix, 2013.
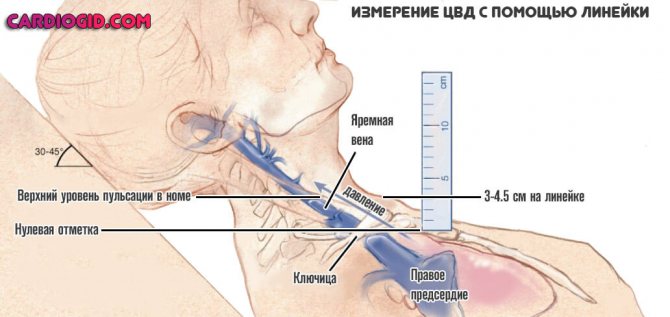
• Position the patient so that he can clearly see the internal jugular veins and their pulsation. It is recommended to start the study with the head positioned at an angle of 45°, but in fact the angle does not matter, the main thing is that the veins are well visualized. If it is not possible to see the internal jugular veins, CVP is measured on the external ones.
• Determine the highest point of pulsation of the internal jugular vein (the "meniscus"), which is usually visible during exhalation and coincides with the maximum of the A and V waves. This will act as a bedside pressure gauge.
• Find the angle of Louis (where the manubrium meets the body of the sternum). This point is taken as “zero” when determining the pressure in the jugular vein (JVP), in contrast to the standard point for measuring CVP - the center of the right atrium.
• Measure the vertical distance in centimeters from the sternal angle to the point of maximum pulsation of the veins. To do this, place two rulers at right angles: one horizontally (parallel to the meniscus), and the other vertically, touching the first ruler and the angle of the sternum. The distance between the angle of the sternum and the meniscus will be equal to the central venous pressure.
• To obtain the CVP value, add 5 cm to the NVP.
The method is based on the fact that the center of the right atrium (where venous pressure is assumed to be zero) is approximately five centimeters below the sternal angle. This ratio is typical for people with normal build and height, and does not depend on body position.
Thus, when using the sternum angle as a reference point, the vertical distance in centimeters to the top of the blood column in the jugular vein is equal to the PUD. Adding 5 cm to the JVP allows you to get the CVP value.
How to pronounce a surname correctly: “Louis” or “Lewis”?
It depends on situation. If you mean the angle of the sternum, then you should pronounce it in the French manner, since the term was proposed by the French surgeon Antoine Louis who first described it (Dr. Louis is better known for his joint invention with the therapist Joseph-Ignace Guillotin, which cut off the heads of aristocrats just above the angle of the sternum) .
If you are talking about the procedure for measuring CVP relative to the angle of the sternum, then you should pronounce the surname in the English manner, since it was the British doctor Sir Thomas Lewis (a student of MacKenzie) who first discovered that normally the pulsation of the jugular veins is visible 2-3 cm above the angle of Louis.
Subsequently, this technique (estimation of central venous pressure by adding 5 cm vertically relative to the level of the internal jugular veins above the angle of Louis) was called the “Lewis method”. So it doesn't really matter what you call it, both names are correct.
What is the normal value of central venous pressure?
When assessed using the Lewis method, a normal central venous pressure should be less than 7 cm water column (some experts suggest a value of 8 cm water column). This means that the jugular venous pressure (i.e. pulse pressure) should not exceed 2-3 cm (two fingers' width) above the angle of Louis.
How can you assess central venous pressure even faster?
A wonderful, quick and convenient method is to sit the patient down. If the veins of the neck are visible in a sitting patient, it means that his central venous pressure exceeds 7 cm of water. Art., which is a pathology. The collarbones are located 2 cm above the angle of the sternum, which means that with normal central venous pressure the veins behind them will not be visible.
5. Are there alternative methods for determining central venous pressure?
Yes, but they are not sufficiently tested:
• von Recklinghausen method
. The patient, who is in a supine position, is asked to place the palm of one hand on the thigh, and the palm of the second on the bed (i.e., 5-10 cm below the first hand). If the veins in both arms are swollen, then the central venous pressure is increased. If, on the contrary, the veins are swollen only in the lower arm, the central venous pressure can be considered normal.
• Alternative but similar method
consists of examining the veins of the back of the hand while slowly passively raising the arm of the patient lying on his back. The height of the level at which the veins collapse is measured in relation to the Louis angle. This value is taken equal to the central venous pressure.
Both methods may produce falsely high CVP values due to local obstruction or constriction of the peripheral veins. Therefore, these methods are not recommended for widespread use.
6. How accurate is the clinical measurement of CVP?
If done correctly (and if the patient is stable), the measurement can be very accurate. The results of an approximate assessment of central venous pressure at the patient's bedside in 90% of cases differ from the indicators obtained during venous catheterization by no more than 4 cm of water. Art. However, the results obtained by different researchers (and by the same researcher) may differ by 7 cm of water. Art.
The problem becomes especially relevant in the unstable condition of the patient, in which the accuracy of the assessment plays a critical role. For example:
• When examining 50 patients in intensive care units, CVP indicators coincided very accurately among students and resident doctors, less often among students and consultant doctors, and even less often among residents and staff doctors. Factors that influenced the accuracy of the assessment included: changes in the patient's body position, poor external lighting, confusion between the determination of venous and carotid pulsations, and changes in central venous pressure during breathing.
• During the second study, a consultant physician, an intensive care unit employee, a resident, an intern and a student assessed CVP in 62 patients on a scale: low, normal, high, very high. The responses were compared with the results of right heart catheterization. The sensitivity of the clinical study was 0.33, 0.33 and 0.49 for low (7 mmHg) CVP, respectively. The specificity of the study was found to be 0.73, 0.62 and 0.76, respectively.
The measurement accuracy was higher with a low cardiac index (18 mmHg). Measurements were less accurate in patients who were in a coma or on mechanical ventilation. Higher reliability (interobserver agreement) did not lead to greater accuracy.
• In a third study, Eisenberg and his associates compared clinical examination data from critically ill patients with those obtained from pulmonary artery catheterization. Various hemodynamic parameters, including central venous pressure, were compared. Physicians were asked to predict, based on clinical data, whether the CVP would be 6 mmHg. Art. The results were correct only in 55% of cases. More often, doctors underestimated the CVP value (in 27% and 17% of cases, respectively).
So, what can be concluded about the clinical significance of CVP assessment?
Compared with catheterization values, clinical assessment of central venous pressure is generally inaccurate, especially in severely ill patients. For example, in the above-described examination of 50 patients who were in extremely critical condition, the overall measurement accuracy was 56%. All physicians who performed the measurements (students, residents, and staff) tended to underestimate the magnitude of the central venous pressure (see question 96), and a higher level of education did not guarantee the accuracy of the measurement.
In fact, the correlation coefficient between clinical assessment of central venous pressure and venous catheterization was highest among students (0.74), slightly lower among residents (0.71), and lowest among staff physicians (0.65). The comparability of results improved slightly after excluding mechanically ventilated patients from the study, because It is believed that CVP is more reliably determined when the patient is breathing spontaneously. Therefore, assessment of CVP at the patient’s bedside can be accurate only in the following most severe cases:
• At low central venous pressure
According to clinical assessment, the likelihood of detecting low CVP during catheterization increases threefold. In this case, it becomes unlikely to obtain high CVP values.
• High central venous pressure
, measured at the bedside (pulsation of the neck veins three or more centimeters above the angle of Louis), four times increases the likelihood of obtaining high CVP values during catheterization. None of the patients with clinically high CVP had low results from instrumental measurements.
• And finally, normal results of clinical evaluation of central venous pressure
diagnostically insignificant (likelihood ratio approaches 1). Thus, if a normal CVP is clinically obtained, no conclusions can be drawn regarding the patient's true CVP.
Why does clinical evaluation of central venous pressure tend to underestimate the result?
Because the partially or fully erect body position required to visualize the neck veins increases the distance between the angle of Louis and the reference point (“zero”) by 3 cm. To avoid this underestimation, many doctors measure CVP during expiration.

Recommended by our visitors:
Errors when measuring CVP
A number of external factors can affect the accuracy of the CVP value. In addition to patient position, these factors include changes in intrathoracic pressure, catheter tip malposition, catheter obstruction, and miscalibration.
Activities that increase intrathoracic pressure, such as coughing or straining, can cause falsely high readings. Make sure the patient is relaxed during the measurement and is breathing normally.
In mechanically ventilated patients, CVP is directly proportional to ventilation pressure and inversely proportional to mechanical compliance of the lungs. Particular attention should be paid to high values because the ventilator-induced increase in central venous pressure leads to significant changes in the patient's hemodynamic physiology. As in spontaneously breathing patients, CVP measurements are taken only in a quiet, sedated or muscle-relaxed state.
Another cause of incorrect readings may be incorrect position of the catheter tip. If the catheter tip has not advanced far enough into the central venous system, for example due to peripheral venous spasms or venous valves, the resulting pressure reading may not correspond to the true CVP.
If the catheter tip is in the right ventricle, this will cause an overestimation of the CVP data. Displaying a typical right ventricular pressure graph on the patient monitor will help identify this error. This form of the CVP graph can occur with the correct positioning of the catheter if there is severe tricuspid regurgitation or atrioventricular dissociation.
Inaccurate low venous pressure values are recorded when there is obstruction of the catheter by thrombotic masses or contact of the catheter tip with the venous wall. As mentioned earlier, attenuation of waves due to air bubbles in the sensor or line also leads to incorrect readings.
Using a poorly calibrated system may result in inaccurate measurements that may be interpreted as a change in the patient's condition when in fact nothing has happened.