There are two main types of vascular formations on the skin: capillary angiodysplasia and hemangioma. You can mainly find nevi formed from capillaries.
This developmental defect is most common among newborns. As a rule, it does not cause any complications other than a cosmetic defect, but in some cases, without appropriate treatment, there is a possibility of bleeding, ulceration and infection.
Description
Capillary angiodysplasia is a consequence of improper formation of the circulatory system and appears as wine-colored, purple or bright red spots on the skin. The main difference from hemangiomas is the formation of large spots that increase as a person grows.
With age, the surface of nevi may become nodular and acquire a darker shade. Capillary angiodysplasia, the photo of which is presented below, does not harm the human body, but due to its location in open areas of the body, it brings moral discomfort and can contribute to the emergence of complexes.
This pathology belongs to the category of congenital malformations, which appears due to the expansion of a large number of blood vessels. Unlike capillary hemangiomas, such spots are already present on the skin of a newborn baby and are quite large in size.
As noted earlier, capillary angiodysplasia does not protrude above the skin, has an irregular shape and bright shades of purple and red. Most often it forms on the face; localization on other parts of the body is also possible. The presence of extensive formations may indicate the existence of more dangerous defects.

Angiodysplasia (vascular dysplasia): concept, causes, forms, treatment
© Z. Nelly Vladimirovna, doctor at the Research Institute of Transfusiology and Medical Biotechnology, especially for SosudInfo.ru (about the authors)
The name of the pathological process, which is characterized by an increase in the number of blood or lymphatic vessels and their changes, came to us from the Greek language (“αγγείο” - vessel, “δυσπλασία” - improper formation of tissues).
Angiodysplasia can be a congenital anomaly and can be diagnosed in children just born, or it can debut at any age (usually in old age) due to various reasons that, as a rule, remain unclear (for the most part this concerns intestinal vascular diseases).
In children, this pathology often catches the eye of others, since in most cases it chooses the area of the face or lower extremities for its localization; on the hands and other parts of the body, such “birthmarks” (as congenital vascular dysplasia, determined visually is popularly called) are less common.
Diagnostics
Capillary angiodysplasia, the treatment of which is selected individually for each person, is detected not only through an external examination. Doppler scanning of veins and arteries is used as a standard diagnostic method. In addition, ultrasound examination of adjacent tissues plays an important role in the diagnosis of the disease. The doctor must have sufficient experience in examining patients with a similar pathology, and special attention is paid to the quality of diagnostic equipment.
After capillary angiodysplasia has been determined, the type of formation and the depth of tissue damage are established. In severe forms, computed angiography and magnetic resonance imaging are recommended. The main disadvantage of such diagnostics is the high cost, but unlike conventional ultrasound diagnostics, they make it possible to identify the type of disease and the degree of damage with maximum accuracy.

Capillary angiodysplasia of the face: treatment
Previously, vascular formations were treated only in severe forms, this was due to the fact that burning and surgical removal contributed to the formation of deep scars. Today, to solve this problem, medical lasers are used, which do not damage healthy tissue and are capable of selectively coagulating blood vessels. This allows treatment to be carried out without consequences in the form of damage to the skin and scars. Typically, lasers are used that emit rays in the green and yellow spectrum. Their effect is to freely pass through the epidermis and accumulate in the capillary lumen, due to which thermal energy is generated that closes the vessel.
Types of lasers
Not only lasers emitting green and yellow light, but also infrared devices are quite common. The latter are somewhat inferior in efficiency due to less absorption of radiation by the blood.
Medical lasers are classified according to their emission spectrum and design features; the spot diameter is of particular importance. Devices that emit a small spot are suitable for treating minor lesions. Their use for large nevi is impractical due to slow processing and low efficiency. Lasers with a larger light spot (from 4 mm) make it possible to quickly stop even large angiodysplasia in a short time. Their advantage is also the low degree of radiation scattering, due to which they penetrate into the deepest layers of the skin. Increased treatment effectiveness is achieved through cold protection of the epidermis and minimal pulse duration.

Symptoms of angiodysplasia
Manifestations of angiodysplasia differ and depend on its type and location. Intestinal angiodysplasia causes anemia due to constant leakage of blood. Internal bleeding also occurs with vascular defects of the central nervous system.
Capillary dysplasia in newborns is manifested by “port-wine stains” - areas on the skin of a pink, bluish or purple color. Spots can be of any size - from pinpoint to extensive. If left untreated, they grow and become brighter in color. Angiodysplasia of the bone (a variant of capillary dysplasia) is most often localized on the lower limb. The diseased leg grows larger than the healthy one. Extensive blood pressure leads to lymphatic and venous insufficiency, causes severe pain and can result in limb amputation.
The clinical picture of pulmonary angiodysplasia is shortness of breath, cough, profuse or capillary pulmonary bleeding. This occurs due to the discharge of arterial blood into the veins through shunts. Insufficient pulmonary blood flow increases the load on the heart, and it enlarges.
Lymphatic AD causes stagnation of lymph in the lower extremities, causing them to swell and become larger, the tissues become denser, and the formation of trophic ulcers is possible. One leg or both may be affected. The appearance is the same as with elephantiasis.
Differential diagnosis of the disease
Of the congenital venous dysplasias, Parkes Rubashov Weber syndrome is characterized by the most severe symptoms. It is differentiated from gigantism, Recklinghausen's neurofibromatosis and acromegaly. These pathologies are not accompanied by dilation of the veins, increased oxygen content in the venous blood and vibration. The following clinical picture is characteristic of Parkes-Weber-Rubashov syndrome:
- an increase in local temperature by 4–8° compared to a similar area of a healthy limb;
- lengthening of the leg (the difference with a healthy one sometimes reaches 8 cm);
- venous walls are dense and do not compress well;
- the veins remain dilated in any position of the leg;
- a vibration similar to a cat’s purring is felt at the venous anastomosis;
- Trophic ulcers with frequent recurrent bleeding are formed.

Some clinical symptoms indicate a violation of the systemic circulation. The myocardium of the right parts of the heart hypertrophies, its contractile function weakens, and heart failure develops. Hence - shortness of breath, tachycardia, edema.
Features of treatment
Capillary angiodysplasia of the face and body is treated with a laser using local anesthetics and does not require general anesthesia, unlike surgical excision. The procedure has no contraindications and does not contribute to the formation of crusts and flaky surfaces. During treatment there is no pain, in some cases a slight burning sensation is possible. To completely remove a birthmark, several procedures are necessary with an interval of 3-4 weeks, their number directly depends on the size of the formation. Capillary angiodysplasia becomes lighter in color with each procedure until it disappears completely.
Other treatments
The specifics of treatment are determined depending on the patient’s age, existing complications, size of the spot and form of formation. The greatest effectiveness is observed during treatment in childhood, this helps prevent the development of complications and changes in the nutrition of adjacent tissues.
Sclerotherapy is the best option for relieving venous forms of angiodysplasia. It is produced by filling the affected areas with a special sclerosing composition. In this way, complications arising from surgical treatment can be avoided.

Treatment of the disease
In most cases, treatment is based on conservative methods of therapy, which include:
- taking medications;
- use of special compression garments;
- physiotherapeutic procedures;
- adjusting the diet.
Drug therapy may include the following drugs:
- hormonal drugs;
- to improve blood circulation;
- blood thickeners.
The doctor may also prescribe the wearing of third-class compression garments.
In more complex cases, surgery may be used to remove the affected area of the intestine or colon.
Capillary angiodysplasia: causes
The main factor in the appearance of port-wine stains is the adverse effect on the child during intrauterine development. Hormonal disorders, the use of drugs with a teratogenic effect, and infectious diseases suffered by the mother during pregnancy have an impact. Chromosome abnormalities and other important factors can also be the cause. All this affects the formation of the circulatory system of the unborn child and the capillary bed. The result is arteriovenous formations, which impede skin nutrition and blood circulation at the site of the spot.

Causes
Pathological vascular changes occur during intrauterine development during pregnancy. Among the reasons that provoke the pathological process are:
- infectious diseases of the expectant mother;
- injuries during pregnancy;
- severe toxicosis;
- drinking alcohol, smoking during pregnancy.
An important period of gestation is 5-20 weeks, when the formation and development of not only vascular structures, but also many other organs occurs. In babies, dysplasia can appear immediately after birth or later.
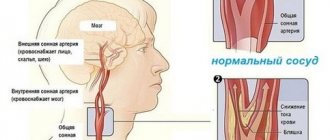
Venous angiodysplasia
Clinical symptoms of the disease can occur at any age due to intoxication, injury, pregnancy or hormonal changes. At the site of formation, blood circulation is impaired, venous insufficiency and frequent blood stagnation occur. There is also a negative effect on the arterial beds. In particular, the elasticity of the walls of the arteries decreases, and their thinning and atrophy are also possible. A frequent complication is insufficient blood supply to the affected area. There are certain symptoms that help diagnose the disease:
- a large number of spider veins on the skin;
- varicose processes, which are extremely rare in children;
- increased sweating;
- hypertrophy of surrounding soft tissues;
- when the limbs are affected, intolerance to increased loads is noted.
A congenital disease characterized by the appearance of wine-colored spots on the skin is called capillary angiodysplasia. The cause of the disease is the effect of a damaging factor on the body of a pregnant woman. As the child grows, the spots increase in size and turn from pink to dark red, the predominant localization is the face, neck and hands. For treatment, coagulation is performed with laser light.
Vascular angiodysplasia - types, causes, complications, diagnosis
According to popular belief, pink, purple, brown, blue, and red spots on the body of newborns are a fright experienced by a woman during pregnancy.
Vascular angiodysplasia develops with degenerative changes in their basins. The hereditary disease is detected in 2.5% of children immediately after birth. It looks like a birthmark on the leg, arm, face.
May affect the brain, lungs, and gastrointestinal tract.
What kind of pathology is this
With pathology, the vessels are formed incorrectly, expand cavernously, and cannot function normally during the period of fetal formation and development. Blood flow is disrupted in affected areas. A state of ischemia is created in which the leg tissues are left without oxygen and nutrition.
The anomaly does not always manifest itself in children, as long as the cardiovascular system compensates for the changes. It can progress later - during the period of hormonal changes and puberty, pregnancy in women. It happens that it flares up suddenly, in people of advanced age, without any provoking factors.
Types and classification
Types of angiodysplasia (ICD code 10) are distinguished depending on the location of the anomaly in a particular structure of the vascular system:
- Arterial - a rare form in which the arteries are absent, underdeveloped, or a sac is formed as an expansion and congenital aneurysm.
- Venous angiodysplasia, if the deep, superficial or muscular veins are affected. In case of defects, phlebectasia and valvular insufficiency are diagnosed. With an abnormality of the superficial veins, blood vessels grow. Diffuse or limited angiomatosis is observed.
- Arteriovenous type with the formation of fistulas. Messages are deformed and incomplete.
- The lymphatic form, in which the lymphatic capillaries are dilated and incomplete. Lymphangiomatosis, aplasia, hypoplasia, and dilatation of lymphatic vessels are manifested.
Causes
Scientists agree that vascular angiodysplasia is the result of a negative effect on the fetus during intrauterine development. Angiomas are formed in the blood and lymphatic vessels at the time of the formation of the bloodstream (from 5 to 20 weeks of pregnancy).
Pathology develops in early pregnancy in women due to a number of provoking factors:
- infection (herpes, rubella, cytomegalovirus, toxoplasmosis);
- alcoholic, drug toxicosis due to abuse of alcohol, hormonal, antibacterial and psychotropic drugs, drugs (cocaine);
- hormonal imbalances;
- deficiency of microelements, vitamins;
- diabetes;
- poisoning with salts of heavy metals, lead, carbon monoxide.
According to scientists, vascular dysplasia develops due to adverse effects on the fetus during intrauterine development. The cause may be a hereditary predisposition or chromosomal damage with the formation of an anomaly at the genetic level.
Also, if a woman abuses drugs with a teratogenic effect in the early stages of pregnancy or suffers from untreated infectious diseases.
Mechanism of disease development and localization
Under the influence of certain factors, veins and arteries are formed incorrectly, and a full capillary bed cannot be formed. Shunts begin to form, interfering with the normal outflow of blood and tissue nutrition.
Shunts, like messages, expand in diameter. Venous insufficiency and congestion begin to progress. The bed of the arteries is subject to pathological changes, the walls of which become thinner and elasticity decreases. This is how chronic ischemia of a particular organ or lower extremities develops.
If fistulas form on large arteriovenous communications, the heart increases in size. Heart failure develops. If trophism and tissue nutrition cease, bones stop growing normally. The patients' legs swell and increase in size. Hypertrophy is observed.
Possible complications
If left untreated, complications that threaten health and life will follow:
- hemorrhages in internal organs, causing pulmonary hemorrhage, stroke;
- extensive bleeding causing hypovolemic shock;
- thrombosis;
- extensive tissue dysplasia with malignancy into a malignant tumor, although the phenomenon is rare.
Fortunately, malformations rarely biotransform into malignant lesions. Venous dysplasia of the brain is dangerous. May result in hemorrhage and disability.
Another problem is that blood vessels are subject to pathological changes. Blood flows from the right ventricle of the heart to the left atrium, bypassing the lungs. They are not saturated with oxygen.
Patients experience shortness of breath, causeless fatigue, and cough with blood. If blood clots enter the general bloodstream through the arteries of the lungs, they can cause a stroke, cerebral edema, or thrombosis.
Manifestations
Symptoms depend entirely on the form of the pathology:
- Arterial. Tissue trophism is disrupted, and the growth of the lower extremities in the affected area slows down.
- Congenital venous. Its chronic form is observed, trophic disorders due to impaired blood outflow, lymphostasis accompanied by edema and an increase in the volume of the limbs. Varicose veins and age spots on the body do not bother you. Hyperhidrosis progresses, tissue trophism is impaired, stagnation due to decreased blood flow speed, hyperkeratosis.
- Arteriovenous malformation. It is distinguished by the absence of a capillary network in patients. Arterial blood is pumped directly into the venous system. It manifests itself in the form of bleeding and pain during heart contractions during blood movement.
- Capillary dysplasia. Pinpoint or extensive port-wine stains appear on the human body. If at first birthmarks practically do not bother you, then over time they can expand their boundaries and cause discomfort. Especially when localized on the face near the eyes, interfering with the normal functioning of the organ of vision.
If the signs of malformation in childhood often do not bother and simply go unnoticed, then closer to the age of 20-30 they begin to make themselves known. More often - during puberty.
Observed:
- hypoglycemia (decreased oxygen levels in the blood);
- trembling, varicose veins;
- hotness of the affected area;
- manifestations on the skin;
- periodic bleeding;
- painful sensations.
Women after childbirth should be alerted by the constant crying of the child, for no apparent reason at first glance. Angiodysplasia provokes damage to the gastrointestinal tract, so the child will probably be bothered by colic, onset of nausea, pallor of the skin, weakness, and the passage of feces of an abnormal color.
If the pathology progresses, then visual manifestations may be as follows:
- stretching, lengthening of limbs;
- bruises on the body or legs, with pulsating veins underneath.
A feature of angiodysplasia is the discharge of arterial blood into the veins through shunts. This means that with increased physical activity against the background of insufficient pulmonary blood flow, the heart may increase in size, causing pulmonary capillary bleeding, dry cough, and shortness of breath.
Diagnostics
Diagnosis of angiodysplasia begins with identifying the extent of the lesion. The main method is duplex color scanning, which determines the volume of the lesion, shape, circulatory problems and congestion.
Other types of dysplasia recognition:
- angiography with the introduction of a contrast agent for x-ray examination;
- computed tomography to visually track volumetric patterns of blood flow;
- MRI to assess the degree and localization of vein damage, functional features, anatomical changes in their structure;
- radiography if there is a suspicion of an enlarged heart, pathological changes in the pulmonary circulation;
- venography to determine the location of the defect, to examine the lumen of the affected vessel.
Who's at risk
People with a hereditary predisposition are at risk of getting venous dysplasia if close relatives have previously suffered a myocardial infarction or stroke. The risk group also includes:
- hypertensive patients;
- suffering from acute vascular diseases, cardiac ischemia, diabetes mellitus.
Provoking factors in a person’s life may include smoking, alcohol or drug abuse, and frequent stress as a powerful factor in the outbreak of vascular diseases.
Angiodysplasia of the intestines, blood vessels, brain and spinal cord is a congenital anomaly, a consequence of intrauterine disturbances in the anlage and development of the fetus. Malformations located in the upper layers of the skin are successfully treated. With angiodysplasia of internal organs (brain, lungs, intestines), the prognosis is disappointing.
The material was prepared specifically for the website venaprof.ru, edited by doctor N.A. Glushakova. Specialty: therapy, cardiology, family medicine.
Source: https://venaprof.ru/angiodisplaziya-sosudov/
What do venous changes look like in children?
As a rule, disturbances in the structure of blood vessels occur during fetal development and appear in newborns in the form of flat spots with a rich pink tint. Upon examination, they turn out to be a multilayered vascular network growing in the superficial layers of the skin. This distinguishes them from a tumor - hemangioma, which rises above the skin and has the appearance of a bruise.
Capillary angiodysplasia in young children
Capillary angiodysplasias do not resolve spontaneously, but tend to increase in size of the spots. Their color becomes more saturated over time, acquiring a characteristic red-violet hue, which gives rise to the name “wine stains.”
In addition to the visible cosmetic defect, this disease has a traumatic effect on the psychological state of the child and inhibits his social adaptation in children's and then adult groups.
We recommend reading the article about hemorrhagic vasculitis on the body. From it you will learn about the causes and forms of the disease, as well as symptoms, diagnosis and treatment.
And here is more information about the best treatment options for hemangioma.
Causes of capillary angiodysplasia
The disease is rarely inherited; its occurrence is associated with disruption of the formation of the vascular network during fetal development. There are known factors that can provoke capillary angiodysplasia:
- use of alcohol and drugs by a pregnant woman;
- smoking;
- taking medications;
- infectious diseases;
- diabetes mellitus with decompensated course;
- thyrotoxicosis;
- exposure to ionizing radiation, harmful production conditions.
When examining the tissues of the “port-wine stain,” it was found that the disease involves underdevelopment or complete absence of nerve fibers in the dilated capillaries. The vessels of the affected area cannot fully constrict due to insufficient supply of impulses to the smooth muscle fibers, so their diameter increases.
Prevention
Due to the fact that at the moment the exact etiological factors have not been established, there are no targeted preventive measures. In general, you should follow recommendations regarding a healthy lifestyle and promptly consult a doctor if you feel unwell.
What to do?
If you think you have Angiodysplasia
and the symptoms characteristic of this disease, then doctors can help you: a vascular surgeon, a gastroenterologist, a therapist.
Source
Did you like the article? Share with friends on social networks:
Signs of congenital port-wine stains
Capillary vessel pathology can occur in any area of the body, but the most common areas of port-wine stains are:
- head, especially often along the branching of the trigeminal nerve;
- neck (sides and back);
- upper limbs.
A regularity has been established - the farther capillary malformations are located from the midline, the more persistent their course and the richer their color. The size of the spots can range from 2 - 5 mm to half the surface of the body. There is a gradual penetration of the lesion into the deeper layers of the skin, which contributes to an increase in the dark shade and the formation of nodules from dilated capillaries.
"Wine Stains"
In adult patients, angiodysplasia can rise above the skin level and look like a solid spot with a bumpy surface . The skin over it becomes thinner, easily injured and bleeds, and is susceptible to infection. The disease can lead to deformation and asymmetry of facial features; some malformations transform into malignant neoplasms.
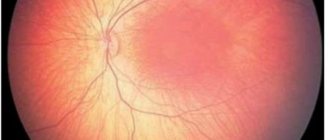
An isolated spot on the skin is not always the only sign of angiodysplasia; it can be accompanied by similar changes in blood vessels in the brain, causing a slowdown in the growth and development of the child, convulsive syndrome, and impaired movement in the limbs. About a third of patients develop glaucoma and impaired corneal transparency, various anomalies in the structure of the skull and valve apparatus.
Forecast
The prognosis for angiodysplasia of the colon is favorable. In most cases, operations bring relief to patients, although a complete cure of the disease cannot be achieved. Small foci of capillary dysplasia on the skin are successfully eliminated and do not recur. Pathologies that appear after 40–50 years of age are more favorable in terms of course and cure.
Arteriovenous angiodysplasia of the lower extremities in the absence of adequate treatment leads to the death of the patient from decompensation of cardiac circulation, gangrene and other complications.
The location of vascular malformation in the brain, lungs and other vital organs requires constant monitoring and treatment. If in children the course of the disease is aggressive, rapidly progressing and reaches the stage of impossibility of excision of pathological vessels, supportive treatment and prevention of ulcerative skin changes are used.

Can angiodysplasia turn into cancer?
Angiodysplasia extremely rarely leads to vascular cancer and only in the complete absence of treatment. This risk exists for nevi, but provided:
- the vascular formation has a traumatic localization;
- located at the site of constant inflammation;
- not protected from sunlight (increased insolation);
- Therapeutic radiation sessions were carried out for other malignant pathologies.
Alarming signs of the beginning of the process are a sharp increase in the spot, itching and burning, a change in the color of the nevus to blue or black, the appearance of lumpiness on it, and a change in contours.
Vascular diagnostics
Most often, the diagnosis can be made based on external signs; if the doctor suspects a violation of brain functions, then an additional examination is carried out:
- radiography of the skull bones;
- CT and MRI of the brain;
- electroencephalography.
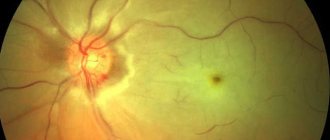
Consultation with an ophthalmologist to measure visual acuity, pressure inside the eye, examination of the cornea, internal media, biometrics.
We recommend reading the article about benign and malignant vascular tumors. From it you will learn about the types and signs of vascular tumors, diagnostic methods and treatment options for tumors.
And here is more information about childhood congenital heart defects.
Treatment methods in children
Before the introduction of laser coagulation into medical practice, capillary angiodysplasia was considered an incurable condition. There is no alternative to this method. In pediatric practice, pulsed radiation options are most often used, which tend to be absorbed by the dye. Hemoglobin plays the role of such a substance in the skin. Therefore, damaged vessels are the focus of action, and healthy tissues do not change their structure.
Under the influence of light in the green and yellow spectrum, dilated capillaries are subjected to intense heating, which causes the cessation of their functioning, and the surface layers of the skin remain unaffected. The coagulation technique is carried out using a point method, that is, with some intervals between places of exposure.
Within three days, the surface of the treated skin wrinkles and becomes covered with a crust. It goes away on its own after a week, revealing a red spot underneath that remains unchanged for up to 2 weeks.
A noticeable result can be seen only after the third month of treatment. To achieve a lasting effect, you need:
- undergo at least 5 sessions for medium lesions, 1 - 3 for small ones and about 10 procedures for large ones;
- after the procedure, use ointments with an antibacterial effect;
- You cannot remove the crusts, as tissue regeneration occurs underneath them;
- the start of laser therapy should be as early as possible; coagulation can be used in infants from the second month;
- For young children, treatment involves the risk of involuntary movements, so it involves the use of general anesthesia.
Capillary angiodysplasia appears in newborns as pink spots on exposed parts of the body. The development of pathology is associated with a disruption in the formation of a network of nerve fibers around blood vessels. Clinical manifestations may be limited to port-wine stains only, or skin signs may be combined with brain signs. For treatment, laser coagulation is performed according to an individual scheme.
general information
Short description
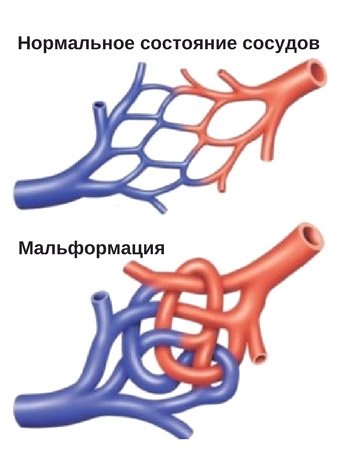
Definition: Arteriovenous malformations (AVMs) or angiodysplasias refer to vascular malformations that occur during embryogenesis. Under the influence of dysembryological factors, the excess of the initial capillary network, which is formed at 5-10 weeks of embryonic life, may not be reduced over time, as a result of which the rudiment of angiodysplasia is formed [1,2,3].
Protocol name : Congenital angiodysplasia.
Protocol code:
ICD-10 code(s): Q27.3 Peripheral arteriovenous malformation Q27.8 Other specified congenital anomalies of the peripheral vascular system Q87.2 Syndromes of congenital anomalies primarily involving the limbs (Klippel-Trenaunay syndrome) D18.0 Hemangioma of any location D18.1 Lymphangioma of any location
Abbreviations used in the protocol:
| AVM - arteriovenous malformation ABC - arteriovenous fistula BP - blood pressure APTT - activated partial thromboplastin time CT - computed tomography CTA - computed tomography angiography INR - international normalized ratio MRA - magnetic resonance angiography MRI - magnetic resonance imaging MSCT – multislice computed tomographic angiography UAC – general blood test OAM – general urine analysis PT – prothrombin time PTI – prothrombin index UD – level of evidence USAS – ultrasound angioscanning USDG – Doppler ultrasound ultrasound – ultrasound examination |
Angiodysplasia, malformation or hemangioma?
According to ICD-10, the disease is classified as a congenital defect, but experts define vascular intestinal dysplasia detected in adults as an acquired form.
It should be noted that until now scientists involved in the study of angiodysplasia have not come to a consensus regarding the use of terminology describing vascular defects; the signs of this pathology are perceived and interpreted differently, therefore in the literature you can find other names for the disease - congenital arteriovenous malformation or even hemangioma.
Angiodysplasia is the result of malformations of blood or lymphatic vessels at different stages of embryogenesis, that is, the disease originates during the stay and formation of a new organism in the womb. The localization of the pathological process can be very diverse: visible parts of the body, lungs, brain, limbs, gastrointestinal tract, etc.
The cause of vascular dysplasia is often the troubles that befell a woman during such a crucial period (gestation) or risk factors that she provoked herself:
Anomalies that form at the genetic and chromosomal level (usually these are defects arising from risk factors such as the woman’s age, harmful chemicals received by the expectant mother under various circumstances in the first trimester of pregnancy);
- Viral and bacterial infections (rubella, cytomegalovirus, toxoplasmosis, herpes, tuberculosis);
- Injuries;
- Reckless use of medications (hormonal, psychotropic or antibacterial drugs);
- Use of alcohol, drugs (cocaine), smoking;
- Metabolic disorders (hormonal disorders, diabetes mellitus, endemic goiter);
- Lack of vitamins and microelements;
- Work in hazardous working conditions;
- Poisoning with carbon monoxide, salts of heavy metals (lead);
- Non-compliance with diet, work and rest by a woman expecting the birth of offspring.
All this is especially dangerous during the period of active formation of the circulatory and lymphatic systems. True, there is an opinion among the people that the pink (red, blue, purple, brown) spots with which the baby was born arise from the fact that the woman was very frightened during pregnancy and grabbed some part of her body in fear (“forbid God”, touch your face with your hands and then angiodysplasia of the child’s face is guaranteed?). Of course, this is nothing more than “women’s zabobons” (superstitions).
Angiodysplasia of the vessels of the lower extremities
- Pale skin
- Painful bowel movements
- Abdominal pain
- Limb stretching
- Hot skin
- Red spots on the skin
- Bleeding from the anus
- Malaise
- Mood swings
- Vein pulsation
- Irritability
- Vomit
- Weakness
- Drowsiness
- Nausea
- Enlargement of limbs in volume
Angiodysplasia is a pathological process that results in an increase in the number of subcutaneous vessels. In the case of the gastrointestinal tract, this can lead to internal bleeding, which is extremely life-threatening. It is noted that this vascular disease can be congenital. In newborns, capillary angiodysplasia is localized in the face, lower extremities, and less often the arms.
Only a doctor can establish an accurate diagnosis by conducting a physical examination and carrying out all the necessary diagnostic procedures.
According to the International Classification of Diseases, Tenth Revision, this disease belongs to the section “congenital malformations” and has an ICD 10 code Q20–28. A separate code has angiodysplasia, which affects the gastrointestinal tract - refers to other intestinal diseases, code K55-63.
Etiology
The development of this disease can be provoked by both congenital anomalies in the development of the child and acquired factors. In general, vascular angiodysplasia can be caused by the following pathological processes:
- spasms of the large intestine;
- diseases of the cardiovascular system;
- chronic diseases of the gastrointestinal tract;
- von Willebrand disease;
- pathological processes in the liver and kidneys;
- diseases of the hematopoietic system.
It should also be noted that until now the exact etiological factors of this disease have not been established.
Separately, risk factors for the development of this pathological process should be highlighted:
- age over 60 years;
- previous gastroenterological diseases that can provoke internal bleeding;
- chronic alcoholism;
- long-term treatment with heavy medications;
- the presence of malignant or benign tumors in the brain;
- a history of traumatic brain injury;
- ischemic stroke.
Due to the fact that there is no exact etiology of this disease, these factors can only be considered as predisposing ones.
Classification
Based on the nature of localization, they are distinguished:
- upper and lower limbs;
- head;
- Gastrointestinal tract.
The most common is angiodysplasia, which affects the gastrointestinal tract, namely the intestines and colon.
Symptoms
In this case, it is impossible to identify a general clinical picture, since everything will depend on which part of the body the pathological process is localized.
Intestinal angiodysplasia is characterized by the following symptoms:
- bleeding from the anus, which can only intensify during physical exertion and excessive physical activity;
- pain during defecation, while blood may be present in the stool;
- abdominal pain, the nature and intensity of which will depend on the severity of the development of the pathological process;
- pale skin;
- weakness, general malaise;
- nausea;
- vomiting, often mixed with blood;
- constant feeling of fatigue, which is accompanied by drowsiness;
- irritability, sudden mood swings.
The congenital form of this vascular disease in a child appears almost immediately after birth and is characterized by the following clinical picture:
- formation of red spots, bruises on the face, head, lower or upper extremities;
- stretching of limbs;
- increased skin temperature;
- pulsation of veins;
- affected limbs increase in volume;
- moodiness, constant crying.
Due to the fact that the clinical picture of both angiodysplasia of the colon and damage to the blood vessels of other body systems is ambiguous, treatment can only be prescribed by a doctor after an accurate diagnosis. Self-medication, including folk remedies, is unacceptable.
Diagnostics
Diagnosis of this venous-vascular pathological process takes place in two stages. First of all, the doctor conducts a thorough physical examination of the patient, palpating the painful area and obtaining a general history. Palpation is carried out extremely carefully, since excessive physical impact may increase internal bleeding.
During the initial assessment, the clinician should determine the following:
- how long ago the symptoms began to appear, the nature of the pain and the intensity of the clinical picture;
- whether there was a history of chronic gastroenterological or systemic diseases;
- whether the patient has undergone surgery on the cardiovascular system or is currently undergoing treatment.
The diagnostic program may include the following:
- analysis of stool for occult blood;
- general blood and urine analysis;
- neurosonography;
- CT scan of the brain;
- examination of the fundus vasculature if the eyelid is affected;
- colonoscopy with biopsy;
- angiography;
- scintigraphy;
- irrigoscopy;
- Ultrasound of the abdominal organs.
Based on the results of the study, the doctor can make a final diagnosis and determine the most effective treatment tactics. Self-medication, even with an accurate diagnosis, is unacceptable.
Treatment
In most cases, treatment is based on conservative methods of therapy, which include:
- taking medications;
- use of special compression garments;
- physiotherapeutic procedures;
- adjusting the diet.
Drug therapy may include the following drugs:
- hormonal drugs;
- to improve blood circulation;
- blood thickeners.
The doctor may also prescribe the wearing of third-class compression garments.
In more complex cases, surgery may be used to remove the affected area of the intestine or colon.
Prevention
Due to the fact that at the moment the exact etiological factors have not been established, there are no targeted preventive measures. In general, you should follow recommendations regarding a healthy lifestyle and promptly consult a doctor if you feel unwell.
Angiodysplasia (AD) is a vascular malformation that occurs at the stage of embryonic development. The human vascular system is complex and diverse, therefore groups of dysplasias are represented by different variants of malformation.
Features of the disease
Pathological changes affect different vascular systems. In terms of frequency, the first place is occupied by vascular defects of the brain and spinal cord. The first clinical symptoms appear between 20 and 40 years of life. From 5 to 20% of cases of angiodysplasia occur in the extremities, and in third place are vascular malformations of the head and neck.
Defects are additional vessels formed in various combinations between the arterial, venous and lymphatic parts of the circulatory system. “Unauthorized” discharge of arterial blood occurs along them, which impairs the nutrition of organs located below the site of the vessel lesion (along the blood flow). The vessels themselves have aneurysms and cavernous expansions.
Source: https://BoliGolovnie.ru/varikoz/angiodisplazija-sosudov-nizhnih-konechnostej.html
Complex classification
Vascular dysplasia is a congenital defect, but it is not always detected at birth, since any of the systems (arterial, venous, lymphatic) can undergo pathological changes and the deformities can be deeply hidden. This does not exclude the presence of defects at the level of different vessels (hemolymphatic malformation) or the dominance of defects in only one system (arterial or venous angiodysplasia). In this regard, vascular dysplasia is classified depending on which vessels have undergone more pathological changes and, based on this, several forms are distinguished:
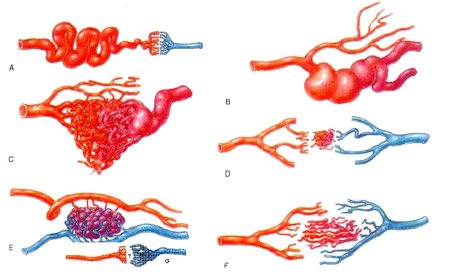
types of vascular malformations
Arterial (rare);
Vascular malformation is also divided by location, for example, in the literature and in life one can more often than not come across the concepts: angiodysplasia of the face, intestines, lower extremities.
Facial angiodysplasia , as a rule, is noticeable from birth; it will be discussed in the “capillary angiodysplasia” section.
Causes of pathology
Vascular malformation, being a congenital pathology, is not always hereditary. Most scientists identify two etiological factors:
- genetic, associated with changes in chromosomes;
- adverse effects on the embryo - infections in the mother, medication, hormonal changes, alcohol toxicosis.
The causative factors for the appearance of angiodysplasia have not been fully studied. The dangerous period in terms of the formation of vascular malformations is considered to be from 5 to 20 weeks. Also, the question of the reasons for the manifestation of clinical signs at different ages remains poorly understood.
Pathological changes in the intestinal vessels of an acquired nature most often affect the large intestine (more than 92% of cases). AD of the small intestine is also less common with concomitant pathologies - blood diseases, liver cirrhosis, aortic stenosis, which are the cause of deformation of local vessels and the opening of arteriovenous shunts.

Capillary angiodysplasia
Capillary angiodysplasia (so-called “port-wine stains”) is the most common type in the group of this pathology (up to 1% of all newborns are “marked” in this way).
Capillary angiodysplasia in the classic version has the form:
- Pinkish spots, although the color can vary from pale pink to bluish and brown;
- The spots do not rise above the skin, however, they can occupy very impressive areas on the body.
It should be noted that, although in rare cases, capillary angiodysplasia can create considerable problems in the functioning of the entire organism, disrupting certain important functions. Expanding their boundaries as a person grows, “birthmarks” can interfere with the normal functioning of individual organs (for example, the organs of vision - facial angiodysplasia) or, located in places of contact with clothing (neck, torso), they can bleed and ulcerate.
The saddest thing, of course, is if these “marks” are localized on the face, because they spoil the appearance and leave an imprint on the person’s character (people around them can not only fix their gaze, but also comment using unpleasant expressions).
Fortunately, this congenital vascular pathology is now amenable to laser treatment, which can be used in children. As a result, a girl or boy may subsequently not even know about the anomaly that took place.

Hemangioma, similar in appearance to capillary angiodysplasia, is different in origin. This is a benign vascular tumor. It can also be congenital, can form in the brain and internal organs and, if it chooses a superficial location, in most cases it rises above the skin (although this is also not at all necessary).
Angiodysplasia - types of abnormal vascular development
Angiodysplasia (vascular malformation) is a pathological change in the vessels of the circulatory or lymphatic system resulting from a violation of the intrauterine development of the embryo.
The name angiodysplasia comes from the Greek words angio - “vessel”, and dysplasia - abnormal formation of tissues. The frequency of this congenital defect of the structure and functioning of blood vessels among all patients with vascular pathologies is about 2.6%.
Types of angiodysplasia
With all types of angiodysplasia, several types of vessels are involved to a greater or lesser extent in the process; depending on the main lesion, several types of angiodysplasia are distinguished.
- Venous - when the veins are affected, venous formations are clearly visible, the organ in which the venous malformation is localized increases in size.
- arteriovenous malformations, characterized by a direct connection of arteries with veins without the participation of capillaries.
- Veins and lymphatic vessels.
- Capillary.
- Pathologies of lymphatic vessels are rare and manifest in asymmetrical damage to the limbs. The patient's leg swells, in appearance the disease is similar to “elephantiasis”. Unlike this disease, angiodysplasia in a short time can lead to the appearance of trophic ulcers on the skin of the affected leg.
Vascular malformations are also classified according to the speed of blood flow in the lesion.
- High-speed - these include arterial dysplasia, aneurysms, arteriovenous fistulas.
- Low-speed - venous, capillary, lymphatic dysplasia.
Symptoms
Depending on the localization of the process and the nature of the malformation, a number of manifestations of angiodysplasia are possible.
Venous and lymphatic angiodysplasias
Veins and lymphatic vessels involved in the pathological process form painful lumps under the skin. Externally, such a bump resembles a mole. If the lump is formed by lymphatic vessels, it may leak lymph fluid and will require treatment with antibiotics or surgery. The lump formed by the veins may bleed.
Arteriovenous
The pathology can occur anywhere in the body and is characterized by the absence of a capillary network, which leads to direct reflux of arterial blood into the venous system.
The main symptom of arteriovenous angiodysplasia is bleeding and pain that occurs when blood moves from the arteries to the veins during heart contractions.
Arteriovenous malformations are most often localized in the bladder, intestines, uterus, and brain.
Angiodysplasia in the brain leads to hemorrhages. The danger lies in the absence of specific symptoms; in some cases, bleeding becomes the first symptom of the disease, which causes high mortality and disability.
Pulmonary arteriovenous angiodysplasias
The peculiarity of this type of pathological change in blood vessels is that the blood is not saturated with oxygen in the lungs, but flows directly from the right ventricle of the heart to the left atrium. This results in shortness of breath and fatigue from lack of oxygen in the tissues.
Arteriovenous plexuses can bleed in the lungs, causing a cough mixed with blood clots.
There is a danger of blood clots entering the general bloodstream through the arteries of the lungs, which can lead to thrombosis of cerebral vessels and cause stroke and cerebral edema.
Vascular cutaneous nevi
Vascular skin lesions are classified as a separate group of diseases - nevi. This group includes:
- Capillary angiodysplasia;
- hemangioma.
Capillary angiodysplasia
The disease is the result of a malformation of blood vessels; capillary angiodysplasia (port-wine stains) manifests itself in pink, purple spots on the skin that do not protrude to the surface, often occupying large areas. This malformation occurs in 1% of newborns. Without treatment, the spot persists throughout life, increasing as the person grows.
Hemangioma
The appearance of hemangioma and capillary angiodysplasia are similar, but the nature of these vascular disorders is different.
Hemangioma is a red vascular benign tumor that rises above the surface of the skin.
Hemangiomas appear in the first three months after birth, go through stages of development from insignificant to very impressive, and are shaped like a strawberry. When buried deeply, they acquire a bluish tint over time.
Causes
Pathological development of blood vessels begins during pregnancy.
The cause of the formation of malformations of the blood and lymphatic vessels of the fetus during intrauterine development are infectious diseases of the mother, trauma, drug and alcohol toxicosis.
The period of formation of the bloodstream, from 5 to 20 weeks of pregnancy, is especially dangerous in terms of the formation of angiomas.
After the birth of a child, some types of angiodysplasia appear immediately, and some of them exist in the form of arteriovenular dysplasia, venulsinusoids, and accumulation of excess capillaries. Congenital angiodysplasia in children can be expressed as a vascular anomaly that develops in a child after birth to three months of age.
Different forms of vascular dysplasia
Arterial angiodysplasia as an isolated variant is quite rare; it is predominantly observed in combination with arteriovenous or venous angiodysplasia. Clinically, this form is manifested by signs of chronic ischemia of arterial vessels, slower growth of the lower limb in the affected area and impaired tissue trophism.
Congenital venous angiodysplasia has a clinical picture of varicose veins of the lower extremities, chronic venous insufficiency, impaired blood outflow and trophic disorders. In other cases, age spots and varicose veins may be absent, but other signs can indicate the disease:
- Reduced blood flow speed, blood stagnation, increased venous pressure;
- Lymphostasis (edema, increased volume of the limb, impaired tissue trophism);
- Increased sweating of the feet (hyperhidrosis);
- Thickening of the stratum corneum of the epidermis and its accelerated desquamation (hyperkeratosis).
An independent type of venous angiodysplasia includes Klippel-Trenaunay syndrome, which is characterized by damage exclusively to the blood vessels of the lower extremities. However, the classification of this option is also controversial - experts again disagree...
- Increased temperature in the affected area;
- Trembling;
- Dilation of veins, which is easy to detect visually;
- Phenomena of ischemia and ulceration manifested on the skin;
- Pain and periodic bleeding.
In the absence of treatment, heart failure often develops with all the ensuing consequences.
As for arteriovenous malformations of the peripheral vessels (lower limbs, pelvis, shoulder girdle), they are mostly noticeable at the birth of the baby or in the very early years of life. Pigment spots, varicose veins, signs of partial gigantism will not hide from the “watchful eye” of parents and doctors observing the child.
Features of the disease
Pathological changes affect different vascular systems. In terms of frequency, the first place is occupied by vascular defects of the brain and spinal cord. The first clinical symptoms appear between 20 and 40 years of life. From 5 to 20% of cases of angiodysplasia occur in the extremities, and in third place are vascular malformations of the head and neck.
Defects are additional vessels formed in various combinations between the arterial, venous and lymphatic parts of the circulatory system. “Unauthorized” discharge of arterial blood occurs along them, which impairs the nutrition of organs located below the site of the vessel lesion (along the blood flow). The vessels themselves have aneurysms and cavernous expansions.
Most angiodysplasias are compensated for a long time by the cardiovascular system. And they do not affect the human condition in any way. The impetus for the appearance of clinical signs is hormonal changes (puberty), trauma, poisoning, pregnancy, increased blood pressure, inflammation. Pathology can appear suddenly without any provoking factors.
Treatment
In conclusion, I would like to warn the reader that attempts to get rid of vascular dysplasia on your own and with folk remedies will not lead to anything good. All variants of this pathology are treated by a phlebologist, and only he can decide which method will be the most optimal and effective. Depending on the nature of the pathological process, the patient (or parents) will be offered one of the methods of treating the disease:
- Laser - it is used for a large affected area with a deep location of the malformation;
- Sclerotherapy is the preferred method in the case of arteriovenous forms;
- Endovascular treatment – this is often used if arteriovenous fistulas occur;
- Embolization is a method effective for damage to the pulmonary vessels.
Radical surgery for vascular dysplasia is now used less and less, because it leaves scars that can look even uglier than the disease itself, especially if it is asymptomatic.
Treatment of angiodysplasia
Today, there are several methods for treating the disease:
- The surgical method is now rarely used, as more advanced methods have been developed.
- Endovascular surgery is used for angiovenous fistulas.
- Sclerotherapy is effective for arteriovenous malformations. It is carried out by introducing a special solution (sclerosant) into the affected area, which leads to the gluing of blood vessels.
- Laser therapy is carried out even for newborns. Success is achieved with extensive skin lesions (hemangiomas) and venous malformations.
- Embolization is carried out under X-ray control using a special cannula, through which a drug is selectively administered to block the blood vessels.