The portal vein (PV, portal vein) is one of the largest vascular trunks in the human body. Without it, normal functioning of the digestive system and adequate blood detoxification are impossible. The pathology of this vessel does not go unnoticed, causing serious consequences.
The hepatic portal vein system collects blood coming from the abdominal organs. The vessel is formed by connecting the superior and inferior mesenteric and splenic veins. In some people, the inferior mesenteric vein drains into the splenic vein, and then the junction of the superior mesenteric and splenic veins forms the trunk of the PV.
Anatomical features of blood circulation in the portal vein system
The anatomy of the portal vein system (portal system) is complex. This is a kind of additional circle of venous circulation, necessary to cleanse the plasma of toxins and unnecessary metabolites, without which they would immediately fall into the inferior hollow, then into the heart and further into the pulmonary circle and the arterial part of the large one.
The latter phenomenon is observed when the liver parenchyma is damaged, for example, in patients with cirrhosis. It is the absence of an additional “filter” on the way of venous blood from the digestive system that creates the preconditions for severe intoxication with metabolic products.
Having studied the basics of anatomy at school, many remember that most organs of our body include an artery that carries blood rich in oxygen and nutritional components, and a vein emerges that carries “waste” blood to the right half of the heart and lungs.
The portal vein system is structured somewhat differently; its peculiarity can be considered the fact that in addition to the artery, the liver enters a venous vessel, the blood from which again enters the hepatic veins, passing through the parenchyma of the organ. It is as if additional blood flow is created, the work of which determines the condition of the entire organism.
The formation of the portal system occurs due to large venous trunks merging with each other near the liver. The mesenteric veins transport blood from the intestinal loops, the splenic vein leaves the spleen and receives blood from the veins of the stomach and pancreas. Behind the head of the pancreas, the venous “highways” connect, giving rise to the portal system.
Between the layers of the pancreaticoduodenal ligament, the gastric, periumbilical and prepyloric veins flow into the PV. In this area, the PV is located behind the hepatic artery and the common bile duct, together with which it follows to the porta hepatis.
At the gates of the liver, or not reaching them one to one and a half centimeters, division occurs into the right and left branches of the portal vein, which enter both hepatic lobes and there break up into smaller venous vessels. Reaching the hepatic lobule, venules entwine it from the outside, enter inside, and after the blood is neutralized upon contact with hepatocytes, it enters the central veins emerging from the center of each lobule. The central veins gather into larger ones and form hepatic veins, which carry blood from the liver and flow into the inferior vena cava.
A change in the size of the vein is of great diagnostic importance and can indicate various pathologies - cirrhosis, venous thrombosis, pathology of the spleen and pancreas, etc. The length of the portal vein of the liver is normally approximately 6-8 cm, and the diameter of the lumen is up to one and a half centimeters.
The portal vein system does not exist in isolation from other vascular systems. Nature provides the possibility of dumping “excess” blood into other veins if a hemodynamic disturbance occurs in this section. It is clear that the possibilities of such a discharge are limited and cannot last indefinitely, but they make it possible to at least partially compensate for the patient’s condition in case of severe diseases of the liver parenchyma or thrombosis of the vein itself, although sometimes they themselves become the cause of dangerous conditions (bleeding).
The connection between the portal vein and other venous collectors of the body is carried out thanks to anastomoses, the localization of which is well known to surgeons, who quite often encounter acute bleeding from anastomotic areas.
Anastomoses of the portal and vena cava are not pronounced in a healthy body, since they do not bear any load. In pathology, when the flow of blood into the liver becomes difficult, the portal vein expands, the pressure in it increases, and the blood is forced to look for other outflow routes, which become anastomoses.
These anastomoses are called portocaval, that is, the blood that should have gone to the IV goes into the vena cava through other vessels that unite both blood flow basins.
This is interesting: Line of bioremedies
The most significant anastomoses of the portal vein include:
- Connection of gastric and esophageal veins;
- Anastomoses between the veins of the rectum;
- The junction of the veins of the anterior wall of the abdomen;
- Anastomoses between the veins of the digestive organs with the veins of the retroperitoneal space.
In the clinic, the anastomosis between the gastric and esophageal vessels is of greatest importance. If the movement of blood through the veins is disrupted, it is dilated, portal hypertension increases, then the blood rushes into the flowing vessels - the gastric veins. The latter have a system of collaterals with the esophageal, where venous blood that does not go to the liver is redirected.
Since the ability to discharge blood into the vena cava through the esophageal veins is limited, overloading them with excess volume leads to varicose veins with the likelihood of bleeding, often fatal. The longitudinally located veins of the lower and middle thirds of the esophagus do not have the ability to collapse, but are at risk of injury when eating, gag reflex, and reflux from the stomach. Bleeding from varicose veins of the esophagus and the initial part of the stomach is not uncommon in liver cirrhosis.
From the rectum, venous outflow occurs both into the venous system (upper third) and directly into the lower cavity, bypassing the liver. With an increase in pressure in the portal system, stagnation inevitably develops in the veins of the upper part of the organ, from where it is discharged through collaterals into the middle vein of the rectum. Clinically, this is expressed in varicose hemorrhoids - hemorrhoids develop.
The third junction of the two venous pools is the abdominal wall, where the veins of the peri-umbilical region take on “excess” blood and expand towards the periphery. Figuratively, this phenomenon is called the “head of Medusa” because of some external resemblance to the head of the mythical Gorgon Medusa, who had writhing snakes on her head instead of hair.
The anastomoses between the veins of the retroperitoneal space and the PV are not as pronounced as those described above, it is impossible to trace them by external signs, and they are not prone to bleeding.
Video: lecture on veins of the systemic circulation
Video: basic information about the portal vein from the notes
Structure of the portal system
The diameter of the portal vein is 1.2-1.5 cm, length - 6-8 cm, which makes it possible to determine it on ultrasound. The vessel collects blood from the unpaired organs of the peritoneal cavity - from the stomach to the upper rectum, spleen, gallbladder and pancreas. It includes 3 large veins - the superior and inferior mesenteric and splenic.
The portal system of the liver is called the “miraculous network.” This is due to the formation of a separate circle of blood circulation. The vessel enters the portal of the liver along with the artery and nerves and immediately divides into right and left branches, which are located in separate lobes of the liver. They are then divided into small veins. Afterwards, they form in a reverse ascending order into large vessels and exit as the hepatic vein, which goes to the inferior vena cava.
The journal Vessel Info published the findings of a study confirming that in 60 seconds there is up to 1500 ml of blood in the portal vein. This had an impact on the massiveness and size of the venous column.
Portal vein thrombosis
Portal vein thrombosis (PVT) is a dangerous condition in which blood clots appear in the PV, preventing its movement towards the liver. This pathology is accompanied by an increase in pressure in the vessels - portal hypertension.
4 stages of portal vein thrombosis
According to statistics, among residents of developing regions, LPG is accompanied by thrombus formation in the veins in a third of cases. In more than half of patients who die from cirrhosis, thrombotic clots can be detected postmortem.
The causes of thrombosis are considered:
- Cirrhosis of the liver;
- Malignant intestinal tumors;
- Inflammation of the umbilical vein during catheterization in infants;
- Inflammatory processes in the digestive organs - cholecystitis, pancreatitis, intestinal ulcers, colitis, etc.;
- Injuries; surgical interventions (bypass surgery, removal of the spleen, gallbladder, liver transplant);
- Blood clotting disorders, including certain neoplasias (polycythemia, pancreatic cancer);
- Some infections (tuberculosis of portal lymph nodes, cytomegalovirus inflammation).
Among the very rare causes of PVT include pregnancy and long-term use of oral contraceptives, especially if the woman has crossed the age of 35-40.
Symptoms of PVT include severe abdominal pain, nausea, dyspeptic disorders, and vomiting. Possible increase in body temperature, bleeding from hemorrhoids.
Chronic progressive thrombosis, when blood circulation through the vessel is partially preserved, will be accompanied by an increase in the typical picture of LPG - fluid will accumulate in the abdomen, the spleen will enlarge, giving characteristic heaviness or pain in the left hypochondrium, and the veins of the esophagus will dilate with a high risk of dangerous bleeding.
The main way to diagnose PVT is ultrasound, and a thrombus in the portal vein looks like a dense (hyperechoic) formation that fills both the lumen of the vein itself and its branches. If ultrasound is supplemented with Doppler ultrasound, then there will be no blood flow in the affected area. Cavernous degeneration of blood vessels due to dilation of small-caliber veins is also considered characteristic.
Small thrombi of the portal system can be detected by endoscopic ultrasound, and CT and MRI make it possible to determine the exact causes and look for possible complications of thrombus formation.
Video: incomplete portal vein thrombosis on ultrasound
Anatomy of the inferior vena cava, functions
The circulatory system of the human body has a complex structure. An important part of it are the veins, which are designed to collect waste blood. The largest of them is the inferior vena cava.
Irregularities in its functioning can lead to serious health consequences. Therefore, it is important to know the normal structure of this vessel and its possible anomalies.
Purpose and location of the inferior vena cava
The inferior vena cava is the largest vessel in the body. It has no valves. The answer to the question of where this vessel is located is clear.
This vein originates between the fourth and fifth vertebrae of the lumbar spine. The place of its formation is the connection of the left and right iliac veins. The vessel ascends along the front of the psoas muscle.
It then passes along the posterior surface of the duodenum, is located in the groove of the liver, penetrates through a special hole in the diaphragm and ends up in the pericardium. From this it becomes clear where the vein flows; its end is located in the right atrium. The left side is in contact with the aorta.
During the respiratory process, the diameter of the vessel changes. When you inhale, the vein contracts slightly, and when you exhale, it expands. Diameter fluctuations range from 2 to 3.4 cm, this is the norm.
The main purpose of the vessel is to collect waste blood from the entire body. It is transmitted directly to the heart.
Inferior vena cava syndrome
Inferior vena cava syndrome is more common in pregnant women. This condition cannot be called a disease; rather, it is a disruption in the process of adaptation of the body to the increased size of the uterus, as well as changes in blood circulation.
In most cases, such a deviation from the norm occurs in women who are carrying an overly large fetus or several babies at the same time. Since the walls of the vessel are too soft and the blood flow in it has low pressure, it is easily compressed.
The syndrome can be caused by the following reasons:
The course of the disease largely depends on the characteristics of a particular organism. More often, the base of the inferior vena cava becomes blocked and a blood clot forms.
The symptoms of the problem largely depend on the extent of the damage. Most often, the first signs appear in the third trimester. They intensify when the woman lies on her back. Among the main features are:
- A slight tingling sensation in the lower extremities.
- Dizziness.
- Swelling of the legs.
- Phlebeurysm.
- Pain in the limbs, weakness.
In most cases, compartment syndrome does not cause any particular harm to health. But in some cases, a collaptoid state may develop . If the compression during pregnancy is significant, it can negatively affect the condition of the fetus. Sometimes this leads to placental abruption, varicose veins, or blood clots.
Compression of the vessel leads to a decrease in cardiac output, therefore, less nutrients and oxygen reach the tissues. Hypoxia may develop.
Treatment is selected by the doctor individually, based on the characteristics of the patient. Since the use of medications during pregnancy is possible only in extremely severe cases, experts advise carrying out therapy by adjusting behavior and nutrition.
https://www.youtube.com/watch?v=snWMfccUeIY
The following rules must be observed:
- You cannot sleep in a supine position. This leads to increased unpleasant symptoms.
- It is prohibited to do exercises that involve lying on your back and also involve the abdominal muscles.
- When resting, it is best to lie on your left side or in a semi-sitting position. You can use special pillows that are placed under your back and legs.
- Walking will help normalize blood flow. It leads to active contraction of the leg muscles, which helps the blood rise up.
- Swimming gives a good effect. While in water, a compression effect is created, which removes blood from the lower extremities.
- The consumption of increased amounts of ascorbic acid and vitamin E is indicated.
Following these recommendations will help restore normal blood flow and improve your health.
Thrombosis
The structure of the inferior vena cava is simple. Pathologies in this area are rare. Sometimes there is a blockage of the lumen. It may occur due to the following reasons:
- Problems with blood clotting.
- Damage to the vein wall.
- Reduced blood flow speed.
Such factors lead to the formation of a blood clot. Infectious diseases, injuries, malignant tumors, and prolonged stay in an immobilized state can aggravate the situation.
The disease may be asymptomatic. Among its main symptoms are: redness and swelling of the extremities, fatigue, and drowsiness. In rare cases, bursting pain appears.
Treatment of such a disease is aimed at preventing thromboembolism, stopping the further development of thrombosis, reducing the degree of tissue swelling, and restoring the lumen of the vessel. Several methods are used for these purposes:
- Drug therapy. It includes the use of anticoagulants - drugs that thin the blood, as well as drugs aimed at dissolving a blood clot. If the disease is accompanied by severe pain, the doctor prescribes non-steroidal anti-inflammatory drugs. During the period when the disease occurs in the acute phase, wearing a special elastic bandage is indicated.
- Surgical intervention. It is recommended in cases where there is a high risk of thromboembolism. Depending on the severity of the lesion and the patient's condition, endovascular intervention or plication is performed.
The complex of therapeutic measures includes mandatory adherence to a dietary diet. The diet should include as many foods as possible containing vitamins K and C. When creating a menu, garlic and green pepper must be included in it.
Endovascular intervention
Endovascular dilatation involves the installation of a vena cava filter. It is a small device made of wire formed into the shape of an hourglass, umbrella or nest.
Such structures are resistant to corrosion and do not have ferromagnetic properties. They are easy to install. At the same time, they do their job perfectly. They are made from titanium, nitinol or high-quality steel.
This filter is selected individually for each patient. This takes into account the structural features of the inferior vena cava and its diameter. Vava filters are divided into three main groups:
- Permanent. It is impossible to delete them later. They are tightly fixed to the walls of the vessel using special antennae.
- Removable. After they have completed the assigned task, they are removed.
Indications for installing filters are: the impossibility of using anticoagulant therapy, a high probability of recurrent thromboembolism. Installation of such a device is not allowed if the narrowing of the lumen is critical or there is no free access to the vessel.
Plication
Plication of the inferior vena cava involves forming the lumen of the vessel using special U-shaped staples. As a result, the lumen is divided into several channels . The diameter of one channel does not exceed 5 mm. This value is enough to restore normal blood flow, while blood clots will not be able to pass further.
It is advisable to carry out plication when mounting vena cava filters is impossible for some reason. During the procedure, a blood clot formed in the vessel is removed. The indication for such an operation is the presence of a tumor in the abdominal cavity or retroperitoneal space.
Such an intervention can be carried out even in late pregnancy. But before this, the woman will have to undergo a caesarean section and extract the fetus.
The inferior vena cava is an important component of the circulatory system. Her diseases are often asymptomatic, so it is necessary to undergo periodic medical examinations.
Source: https://prososud.ru/veny/nizniya-polaya-vena.html
| Table of contents of the topic “Abdominal part of the aorta. Lumbar plexus.”: 1. Retroperitoneal tissue. Layers of retroperitoneal tissue. Borders of the retroperitoneal tissue. 2. Abdominal part of the aorta. Topography of the abdominal aorta. Syntopy of the abdominal aorta. 3. Branches of the abdominal aorta. Branches of the abdominal aorta. 4. Aortic bifurcation. Iliac arteries. Topography of the iliac artery. 5. Inferior vena cava. Topography of the inferior vena cava. Syntopy of the inferior vena cava. 6. Lumbar plexus. Topography of the lumbar plexus. Branches of the lumbar plexus. 7. Sympathetic trunk. Topography of the sympathetic trunk. Branches of the sympathetic trunk. 8. Abdominal aortic plexus. Celiac plexus. Parasympathetic innervation of the abdominal organs. 9. Lymphatic system of the retroperitoneum. Lymph nodes of the retroperitoneum. 10. Kidneys. Bud. Topography of the kidney. Kidney structure. Inferior vena cava begins retroperitoneally at the level of the IV-V lumbar vertebrae from the confluence of two common iliac veins. This place is covered by the right common iliac artery. Further from its origin, the inferior vena cava rises up, in front and to the right of the spine towards the liver and its own opening in the diaphragm. Syntopy of the inferior vena cavaAnterior to the inferior vena cava there are the parietal peritoneum of the right mesenteric sinus, the root of the mesentery of the small intestine with the superior mesenteric vessels passing through it, the horizontal (lower) part of the duodenum, the head of the pancreas, the portal vein, and the posteroinferior surface of the liver. The inferior vena cava at its beginning is crossed in front by a. iliaca communis dextra, and above - a. testicularis dextra (a. ovarica). To the left of the inferior vena cava The aorta lies almost along its entire length. Right inferior vena cava adjacent to the psoas muscle, right ureter, medial edges of the right kidney and right adrenal gland. Above, the vein lies in the notch of the posterior edge of the liver, the parenchyma of which surrounds the vein on three sides. Next, the inferior vena cava enters the chest cavity through the foramen venae cavae in the diaphragm. Behind the inferior vena cava pass through the right renal artery and right lumbar arteries. Posteriorly and to the right is the lumbar region of the right sympathetic trunk. Into the inferior vena cava The following visceral and parietal veins drain retroperitoneally. Parietal veins of the inferior vena cava:1. Lumbar veins ,vv. lumbales, four on each side. 2. Inferior phrenic vein , v. phrenica inferior, steam room, flows into the inferior vena cava above the liver. |
Portal hypertension syndrome
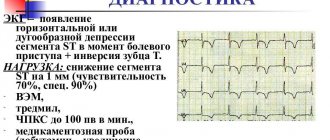
Portal hypertension is an increase in pressure in the portal vein system, which can accompany local thrombus formation and severe pathology of internal organs, primarily the liver.
Normally, the pressure in the IV is no more than ten mm Hg. Art, when this indicator is exceeded by 2 units, we can already talk about LNG. In such cases, portocaval anastomoses are gradually included, and varicose dilation of the collateral outflow tract occurs.
This is interesting: Lemon, garlic and honey in the treatment of blood vessels - cleansing and strengthening
The causes of LNG are:
- Cirrhosis of the liver;
- Budd-Chiari syndrome (liver vein thrombosis);
- Hepatitis;
- Severe heart defects;
- Metabolic disorders - hemochromatosis, amyloidosis with irreversible damage to the liver tissue;
- Splenic vein thrombosis;
- Portal vein thrombosis.
Clinical signs of LPG include dyspepsia, a feeling of heaviness in the right hypochondrium, jaundice, loss of body weight, and weakness. Classic manifestations of increased pressure in the venous vein are splenomegaly, that is, an enlargement of the spleen, which experiences venous stagnation, since blood is not able to leave the splenic vein, as well as ascites (fluid in the abdomen) and varicose veins of the lower segment of the esophagus (as a result of shunting of venous blood ).
An abdominal ultrasound with LPG will show an increase in the volume of the liver, spleen, and the presence of fluid. The width of the lumen of the vessels and the nature of blood movement are assessed using Doppler ultrasound: the venous vein is increased in diameter, the lumens of the superior mesenteric and splenic veins are dilated.
Diseases
Portal hypertension
Often this condition in humans is caused by viral hepatitis.
A syndrome manifested by excess pressure in the vein over 10 mmHg. Art. The causes of this pathology include:
- thrombosis;
- viral hepatitis;
- malignant neoplasm;
- hemochromatosis;
- cirrhosis;
- amyloidosis;
- heart failure.
The danger of this pathology is the rapid transformation into liver failure, disruption of the gastrointestinal tract and spleen. When examining the abdominal wall, dilated veins are visible, which is called the “head of the jellyfish”, since ascites, an accumulation of fluid in the peritoneum, develops in parallel. And also, there is a pathological enlargement of the spleen and dyspeptic disorders. If help is not provided in time, hepatic encephalopathy may develop.
Thrombosis of the portal vessel
Many pathological factors influence the formation of blood clots in the vessel.
The etiological factors of thrombosis can be blood clotting disorders, inflammatory processes, cancer of the head of the pancreas, and mechanical injuries during operations. In this case, a total or partial blockage of the vessel by a thrombus occurs, and this makes further passage of blood impossible. As a result, expansion of the portal vein occurs with the development of portal hypertension syndrome. When the lumen is partially closed, a chronic form of thrombosis occurs, when symptoms increase gradually.
Pylephlebitis
This is a disease that has an inflammatory nature of the portal vessel of the liver. Pathological microorganisms penetrate the gate due to abscess formation of acute appendicitis. The problem of diagnosis is the nonspecificity of the manifestations of the pathology. High body temperature, fever, chills, jaundice, nausea and vomiting, and pain occur. To make a diagnosis, it is necessary to conduct complex studies - MRI, CT, angiography.
Other diseases
Sometimes a person may be diagnosed with an aneurysm of this vessel.
The following diseases are less common:
- congenital pathologies of the venous wall;
- aneurysm;
- cavernous transformation;
- anomalies in the location of the vessel.
When performing ultrasound diagnostics of the liver, the size of the portal vein is always determined, since the symptoms of circulatory disorders are rarely specific.
Cavernous transformation
With SPH, PVT, congenital malformations of the liver veins (narrowing, partial or complete absence), a so-called cavernoma can often be found in the area of the portal vein trunk. This zone of cavernous transformation is represented by many intertwining vessels of small diameter, which partially compensate for the lack of blood circulation in the portal system. Cavernous transformation has an external resemblance to a tumor-like process, which is why it is called cavernoma.
The discovery of a cavernoma in children can be an indirect sign of congenital anomalies of the vascular system of the liver; in adults, it more often indicates developed portal hypertension against the background of cirrhosis and hepatitis.
General characteristics[ | ]
Unlike arteries, veins do not carry blood to the organs and tissues of the body, but collect it from them and carry it in the opposite direction in relation to the arteries: from the periphery (tissues and organs) to the heart. The wall of veins is built according to the same plan as the walls of arteries. However, the walls of veins are thinner and less elastic (causing empty veins to collapse) than those of arteries because the blood pressure in the veins is low (15-20 mm Hg). The veins widely anastomose with each other, sometimes forming venous plexuses (usually near organs). Connecting with each other, smaller veins ultimately form large venous trunks - veins that flow into the heart [3].
The outflow of venous blood begins through postcapillary venules, which continue into the veins. The movement of blood through the veins is carried out due to the suction action of the heart and the fact that negative pressure arises in the chest cavity every time during inhalation due to the difference in pressure in the cavities, contraction of the muscles of the organs and a number of other factors. The reverse outflow of venous blood through the veins is prevented by venous valves (Latin valvulae venosae), which are a feature of the venous wall. The valves are formed by folds of endothelium containing a layer of connective tissue. The valves face their free edges towards the outflow to the heart and thus do not interfere with the outflow of blood in this direction, but at the same time they can prevent its reverse flow. Also, vein valves protect the heart from unnecessary energy expenditure to overcome the oscillatory movements of blood that occur in the venous bed under the influence of various external factors (fluctuations in atmospheric pressure, muscle compression, etc.). The veins of the internal organs, the brain and its membranes, the hypogastric, iliac, inferior and superior vena cava and pulmonary trunk do not have valves[1].
Veins are characterized by certain features of their angioarchitectonics - the order of their formation, the relationship of their tributaries and connections with each other, their distribution among body parts. There are superficial and deep veins, which are connected to each other by a large number of anastomoses, which provide better blood flow when it is disrupted in an uncomfortable body position or due to pathologies. Superficial veins lie in the subcutaneous tissue and provide thermoregulation of the skin of the body. The deep veins lie parallel to the arteries along their course, have the same names in the anatomical nomenclature and, uniting with the nerve trunks, form neurovascular bundles. Each artery is accompanied by 2-3 deep veins of the same name, due to which the capacity of the veins is 2-3 times greater than the capacity of the arteries [1].
Inflammatory processes
an example of the development of pylephlebitis due to diverticulum of the sigmoid colon
Rare lesions of the portal vein include acute purulent inflammation - pylephlebitis, which has a distinct tendency to “develop” into thrombosis. The main culprit of pylephlebitis is acute appendicitis, and the consequence of the disease is abscess formation in the liver tissue and the death of the patient.
The symptoms of inflammation in the IV are extremely nonspecific, so it is very difficult to suspect this process. Until recently, the diagnosis was made mainly posthumously, but the possibility of using MRI has somewhat changed the quality of diagnosis for the better, and pylephlebitis can be detected during life.
Signs of pylephlebitis include fever, chills, severe intoxication, and abdominal pain. Purulent inflammation of the veins can cause an increase in pressure in the vessel and, accordingly, bleeding from the esophageal and gastric veins. When infection enters the liver parenchyma and purulent cavities develop in it, jaundice will appear.
Laboratory examinations for pylephlebitis will show the presence of an acute inflammatory process (ESR will increase, leukocytes will increase), but ultrasound, Doppler, CT and MRI help to reliably judge the presence of pylephlebitis.
Complications of varicose veins
Varicose veins do not go away without a trace. Complications are not uncommon and lead to serious consequences. Self-medication in such cases is unacceptable. Below we will look at the main complications that varicose veins lead to.
Vein thrombosis
What is venous thrombosis and why did it happen? This is the first question that comes to a person who is faced with this complication for the first time. By its nature, a thrombus is a blood clot located in the lumen of a vessel and obstructing the flow of blood. It is formed either due to a violation of the properties of the blood itself, or due to changes in the vascular wall. Sometimes a blood clot can completely block the lumen of the veins. In this case, blood flows from the extremities with difficulty, and significant swelling and pain occur. A dangerous feature of vein thrombosis is a situation in which the thrombus “floats” (the loose head of the thrombus fluctuates freely in the lumen of the vessel) and can break away from the base. This situation is critical for the health and life of the patient, since the blood clot rushes into the lungs, where it clogs smaller vessels, leading to acute respiratory failure.
Thrombosis of superficial veins
Thrombophlebitis is an inflammation of the vein wall, accompanied by thrombosis. The veins of the lower extremities are most often affected, but in some situations, for example with injection drug addiction, the veins in the arms are also affected. Externally, the vein looks swollen, tense, and along its course a dense area is identified - vein thrombosis. The situation is accompanied by pain, weakness, and increased body temperature. What to do? Seeking medical help is the very first and most important point in the treatment of such diseases. Self-medication will not lead to regression of the disease, but will only worsen the situation. At the clinic, such a patient will receive the following treatment: bed rest, elastic compression, blood thinning drugs (disaggregants or anticoagulants as indicated). In addition, ointments with heparin are applied superficially, and analgesic and anti-inflammatory therapy is carried out. In some cases, surgical treatment will be required. In case of timely treatment, vein thrombosis regresses, the clot dissolves and the patient is discharged with the doctor’s recommendations.
Deep vein thrombosis
Phlebothrombosis is the name given to the occurrence of a blood clot in the deep veins of the extremities. However, the symptoms in this case will be different. The severity of symptoms of vein damage depends on the degree of blockage (obliteration) of the vessel by a thrombus. With complete blockage, visible swelling of the foot, leg, and sometimes thigh occurs, accompanied by severe pain and filling of the superficial veins. Seeking medical attention immediately is also very important. During an external examination, it is difficult to make a diagnosis of deep vein thrombosis, since a number of diseases can repeat the clinical symptoms. It is necessary to perform an ultrasound of the veins and prescribe treatment only after confirming the diagnosis. Such patients are subject to mandatory hospitalization in the surgical department. Treatment includes strict bed rest, elastic compression, administration of direct anticoagulants (heparin and its analogues), and anti-inflammatory therapy. After a week, direct anticoagulants are replaced with indirect anticoagulants (Warfarin).
Bleeding from varicose veins
As already mentioned, with varicose veins, changes occur in the vascular wall. It becomes thinner, becomes less elastic, and due to expansion it protrudes above the surface of the skin, which can lead to injury and bleeding. Sometimes blood loss with this type of complication can be massive, and in this case the person must be hospitalized. First aid consists of compressing the bleeding site with a pressure bandage and lifting the limb upward. In a hospital setting, it is possible to stitch a bleeding vessel to stop bleeding, correct blood loss through infusion therapy, monitor and prevent re-bleeding.
Trophic ulcers
Varicose veins and accompanying chronic venous insufficiency are the main cause of trophic ulcers of the lower extremities. Ulcers are located on the front and side surfaces of the leg, most often in its lower third. Both single and multiple ulcers occur; both small and gigantic, encircling the entire lower leg. Ulcers can last for many months and even years, bringing significant discomfort to a person’s life. Their treatment is lengthy and sometimes ineffective. Prevention of trophic disorders should begin with the treatment of the underlying disease - treatment of varicose veins. You should not start the disease in the early stages and self-medicate, hoping that the disease will go away on its own.
Movement of blood through the veins[ | ]
The linear velocity of blood flow in the veins, as in other parts of the vascular bed, depends on the total cross-sectional area, therefore it is the smallest in the venules (0.3-1.0 cm/s), the highest in the vena cava (10-25 cm/s). With). The flow of blood in the veins is laminar, but at the point where two veins flow into one, vortex flows arise that mix the blood, its composition becomes homogeneous.
Blood pressure in the veins is significantly lower than in the arteries and can be lower than atmospheric pressure (in the veins located in the chest cavity - during inhalation; in the veins of the skull - when the body is in an upright position); venous vessels have thinner walls, and with physiological changes in intravascular pressure, their capacity changes (especially in the initial section of the venous system); many veins have valves that prevent the reverse flow of blood. The pressure in postcapillary venules is 10-20 mmHg. Art., in the vena cava near the heart it fluctuates in accordance with the phases of respiration from +5 to -5 mm Hg. Art. - therefore, the driving force (ΔP) in the veins is about 10-20 mm Hg. Art., which is 5-10 times less than the driving force in the arterial bed. When coughing and straining, central venous pressure can increase to 100 mmHg. Art., which prevents the movement of venous blood from the periphery. The pressure in other large veins also has a pulsating nature, but pressure waves propagate through them retrogradely - from the mouth of the vena cava to the periphery. These waves are caused by contractions of the right atrium and right ventricle. The amplitude of the waves decreases as they move away from the heart. The pressure wave propagation speed is 0.5–3.0 m/s. Measurement of pressure and blood volume in veins located near the heart in humans is often carried out using phlebography of the jugular vein. The venogram reveals several successive waves of pressure and blood flow, resulting from obstruction of blood flow to the heart from the vena cava during systole of the right atrium and ventricle. Phlebography is used in diagnostics, for example, in case of tricuspid valve insufficiency, as well as in calculating the value of blood pressure in the pulmonary circulation.
The main driving force is the difference in pressure in the initial and final sections of the veins created by the work of the heart. There are a number of auxiliary factors that influence the return of venous blood to the heart.
1.
Movement of the body and its parts in a gravitational field
In a tensile venous system, the hydrostatic factor has a great influence on the return of venous blood to the heart.
Thus, in the veins located below the heart, the hydrostatic pressure of the blood column is added to the blood pressure created by the heart. In such veins the pressure increases, and in those located above the heart it decreases in proportion to the distance from the heart. In a lying person, the pressure in the veins at the level of the foot is approximately 5 mmHg. Art. If a person is transferred to a vertical position using a turntable, the pressure in the veins of the foot will increase to 90 mm Hg. Art. In this case, the venous valves prevent the reverse flow of blood, but the venous system is gradually filled with blood due to the inflow from the arterial bed, where the pressure in the vertical position increases by the same amount. The capacity of the venous system increases due to the stretching effect of the hydrostatic factor, and an additional 400-600 ml of blood flowing from microvessels accumulates in the veins; accordingly, venous return to the heart decreases by the same amount. At the same time, in the veins located above the level of the heart, venous pressure decreases by the amount of hydrostatic pressure and may become lower than atmospheric pressure. Thus, in the veins of the skull it is 10 mm Hg below atmospheric pressure. Art., but the veins do not collapse, as they are fixed to the bones of the skull. In the veins of the face and neck, the pressure is zero, and the veins are in a collapsed state. The outflow occurs through numerous anastomoses of the external jugular vein system with other venous plexuses of the head. In the superior vena cava and the mouth of the jugular veins, the pressure in the standing position is zero, but the veins do not collapse due to the negative pressure in the chest cavity. Similar changes in hydrostatic pressure, venous capacity and blood flow velocity also occur with changes in the position (raising and lowering) of the arm relative to the heart. 2. Muscle pump and venous valves
When muscles contract, the veins passing through their thickness are compressed.
In this case, the blood is squeezed towards the heart (venous valves prevent backflow). With each muscle contraction, blood flow accelerates, the volume of blood in the veins decreases, and the blood pressure in the veins decreases. For example, in the veins of the foot when walking, the pressure is 15-30 mmHg. Art., and for a standing person - 90 mm Hg. Art. The muscle pump reduces filtration pressure and prevents the accumulation of fluid in the interstitial space of the leg tissues. In people who stand for long periods of time, the hydrostatic pressure in the veins of the lower extremities is usually higher, and these vessels are more stretched than in those who alternately strain the muscles of the lower leg, as when walking, to prevent venous stagnation. If the venous valves are defective, contractions of the lower leg muscles are not as effective. The muscle pump also enhances the outflow of lymph through the lymphatic system. 3. The movement of blood through the veins to the heart
is also facilitated by the pulsation of the arteries, leading to rhythmic compression of the veins.
The presence of a valve apparatus in the veins prevents the reverse flow of blood in the veins when they are compressed. 4. Respiratory pump
During inhalation, the pressure in the chest decreases, the intrathoracic veins dilate, and the pressure in them decreases to -5 mm Hg.
Art., blood is sucked in, which contributes to the return of blood to the heart, especially through the superior vena cava. Improved blood return through the inferior vena cava is facilitated by a simultaneous slight increase in intra-abdominal pressure, which increases the local pressure gradient. However, during exhalation, the blood flow through the veins to the heart, on the contrary, decreases, which neutralizes the increasing effect. 5. The suction action of the heart
promotes blood flow in the vena cava during systole (expulsion phase) and during the rapid filling phase. During the expulsion period, the atrioventricular septum moves downward, increasing the volume of the atria, as a result of which the pressure in the right atrium and adjacent sections of the vena cava decreases. Blood flow increases due to the increased pressure difference (suction effect of the atrioventricular septum). At the moment of opening of the atrioventricular valves, the pressure in the vena cava decreases, and the blood flow through them in the initial period of ventricular diastole increases as a result of the rapid flow of blood from the right atrium and vena cava into the right ventricle (suction effect of ventricular diastole). These two peaks of venous blood flow can be observed on the curve of the volumetric flow velocity of the superior and inferior vena cava.
Classification[ | ]
The walls of the vein consist of three layers, or membranes: the inner or endothelium (consists of a layer of endothelial cells located on the connective layer), the middle (elastic elastic tissue and smooth muscle fibers) and the outer - adventitia (consists of connective tissue). The development of these membranes and the features of their structure in different veins vary significantly [4].
Based on the development of muscle elements in the walls of venous vessels, they are divided into two groups: veins of non-muscular (fibrous) and muscular types. Veins of the muscular type, in turn, are divided into veins with weak, medium and strong development of muscle elements in the wall [4].
Veins of the muscleless type[ | ]
Veins of the amuscular
or
fibrous type
are characterized by thin walls and the absence of a middle shell. This type includes veins of the dura and soft meninges, veins of bones, spleen, retina and placenta. The veins of the meninges and retina can stretch greatly, but the blood they contain can, under the influence of its own gravity, flow relatively easily into venous trunks that are larger in diameter. The veins of the bones, spleen and placenta are also passive in terms of the movement of venous blood through them, which is due to the fact that they are tightly fused with the dense elements of their corresponding organs and are not able to collapse, due to which the outflow of venous blood easily occurs through them. Endothelial cells, which form the inner layer of the wall, have much more tortuous boundaries than those in arterial vessels. Outside this layer is adjacent a basement membrane and a thin layer of fibrous loose connective tissue, which fuses with nearby surrounding tissues[4].
Muscular type veins[ | ]
Muscular veins
(lat. venae myotypicae) are distinguished by smooth muscle cells in their membranes, the location and number of which in the walls are determined by hemodynamic factors.
It is customary to distinguish veins with weak, medium
and
strong development of muscle elements
. Veins with weak development of muscle elements may vary in diameter. Veins of this type include veins of small and medium caliber (with a diameter of no more than 1-2 mm), which accompany the muscular-type arteries in the upper body, face and neck, as well as some large veins (for example, the superior vena cava). In these veins, venous blood largely moves passively under the influence of its gravity. This type of vein also usually includes the veins of the upper limb. The walls of veins with weak development of muscle elements are somewhat thinner than arteries of similar caliber, contain fewer muscle cells, and on histological preparations are usually in a collapsed state [4].
Veins with weak development of muscle elements of small and medium caliber are distinguished by a poorly defined subendothelial layer, as well as the presence of a small number of muscle cells in the middle tunica. In a number of small veins, for example in the veins of the gastrointestinal tract, the smooth muscle cells of the tunica media form separate “belts” located at a great distance from each other. Thanks to this structural feature, these veins have the ability to greatly expand and thereby also perform a depository function. In the outer shell of small veins with weak development of muscle elements, there may be single longitudinally located smooth muscle cells. Among large-caliber veins with weak development of muscle elements, the most typical is the superior vena cava, in the middle shell of the wall of which there is a small number of smooth muscle cells, which is explained by the upright posture of a person - blood flows through this vein to the heart due to gravity, as well as the respiratory movements of the chest cells[4].
The brachial vein is a medium-sized vein with average development of the muscular elements of the wall. The endothelial cells that form its inner lining are shorter than those in the artery of the same name. The subendothelial layer is formed by connective tissue fibers and cells oriented mainly along the vessel. The inner lining of vessels of this type forms the valve apparatus. The internal elastic membrane in these veins is not expressed. At the border between the inner and middle shells there is only a network of elastic fibers, which are connected with the elastic fibers of the middle and outer shells, due to which a single frame is formed. The medial layer of this type of vein is much thinner and consists of circularly oriented bundles of smooth myocytes separated by layers of fibrous connective tissue. There is no outer elastic membrane, which is why the connective tissue layers of the middle shell pass directly into the loose connective fibrous tissue of the outer shell. Elastic and collagen fibers located in the outer shell have a predominantly longitudinal orientation. Veins with strong development of muscle elements include large veins of the lower limb and lower half of the body. These veins are characterized by the presence of developed bundles of smooth muscle cells in all 3 membranes, while in the inner and outer membranes these bundles are characterized by a longitudinal direction, and in the middle - circular [4].