Leukocytosis - definition, causes, mechanism of development
Leukocytosis is an increased number of white blood cells (leukocytes) in a person's blood for reasons not related to malignant diseases.
Much less frequently, but with more serious consequences, this disease occurs if it is associated with primary bone marrow disorders (those that do not have third-party causes, but occur as a result of genetic disorders or other factors).
The normal response of the bone marrow to infection or inflammation results in an increase in the number of white blood cells, predominantly polymorphonuclear leukocytes and their less mature cellular forms.
Physical stress (for example, after stress, anesthesia or overexertion) can also affect the increase in the number of white blood cells.
Drugs commonly associated with leukocytosis are corticosteroids, lithium, and beta-agonists (beta-agonists). An increase in the number of eosinophils or basophils as a result of various infections, allergic reactions and other reasons can also lead to leukocytosis.
Bone marrow disorders are usually suspected in patients whose white blood cell count is very high and at the same time an abnormality of red blood cells or platelets.
Causes of leukocytosis
The main reasons for the development of leukocytosis are:
- infection, inflammation or tissue damage;
- immune reactions accompanying an attack of asthma or allergies;
- bone marrow diseases such as leukemia or thrombocytopenia;
- drugs to relieve inflammation or treat mental disorders, cancer;
- severe physical or emotional stress;
- Stressful situations are chronic.
The most common bone marrow disorders can be divided into acute leukemia, chronic leukemia and myeloproliferative diseases.
Acute leukemia is the most dangerous form of the disease, the symptoms of which appear suddenly and acutely. Chronic leukemia is diagnosed accidentally in most cases.
A white blood cell count of more than 100,000 mm3 (100 x 109 per L) means that the patient needs emergency medical attention due to the high risk of cerebral infarction and hemorrhage.
Leukocytosis is diagnosed when the white blood cell count exceeds 11,000 per mm3 (11 x 109 per L), often diagnosed through a routine blood test.
An elevated white blood cell count usually reflects a normal bone marrow response to an infectious or inflammatory process.
Sometimes leukocytosis is a sign of primary bone marrow pathology and a consequence of cell apoptosis associated with leukemia or myeloproliferative disorders.
Leukocytosis can be a reaction to various infectious, inflammatory, and in some cases physiological processes (for example, stress, exercise).
This response is based on substances that are released into the blood or activated in response to a stimulating event. Such factors include, for example, granulocyte colony-stimulating factor of granulocyte-macrophages, colony-stimulating factor, as well as various cytokines, such as interleukin-1, interleukin-3, interleukin-6, interleukin-8.
Peripheral leukocytosis is determined by several mechanisms, including the rate of release of cells from storage areas in the bone marrow, the rate of transfer of blood cells from blood vessels into tissues, and the rate of consumption of cells by tissues, such as when they are lost.
Growth factors, adhesion molecules and cytokines control all the processes mentioned above. .
Hyperleukocytosis (white blood cell count > 100 x 109/L, or > 100 x 103/μL) occurs in leukemia and myeloproliferative diseases.
This pattern is caused by the presence of autonomous growth potential of malignant cells. Hyperleukocytosis often causes blockage of blood vessels, resulting in ischemia, hemorrhage and swelling of the affected organs.
This problem is most often seen in acute myeloid leukemia with high white blood cell counts. Patients may also present with mental status changes, strokes, and renal or pulmonary failure.
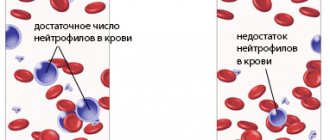
If the number of neutrophils exceeds 30,000/μl in response to external factors, say, infection, this reaction is called leukemoid.
Leukocytosis often occurs as a result of stress, both physical and emotional.
Manifestations of leukocytosis caused by stress are the following conditions:
Kinds
Today there are several types of disease, which we will now talk about.
- Short-term leukocytosis. This type of illness develops when there is a sudden release of white blood cells into the blood (for example, stress). In such situations, the disease disappears along with the provocateur of its occurrence. This form of the disease is observed in typhus, scarlet fever, diphtheria, septic diseases and lobar pneumonia.
- Pathological symptomatic appearance. It usually develops during purulent-inflammatory processes and some infections.
- Physiological leukocytosis can occur after eating, heavy physical exertion, etc.
- The eosinophilic type of the disease develops as a result of the formation or release of eosinophils into the blood. The main causes are medications and allergic reactions (even to vaccines).
- Neutrophilic leukocytosis is caused by a high level of formation or release of neutrophils into the blood. This type of disease is observed in chronic inflammation, acute infections and myeloproliferative diseases.
- The lymphocytic form of leukocytosis is characterized by a high percentage of lymphocytes in the blood. It is observed in chronic and some acute infections.
- The basophilic type of the disease is characterized by an increase in the formation of basophils. Occurs with nonspecific ulcerative colitis, pregnancy and myxedema.
- Monocytic leukocytosis is very rare. It develops in sarcoidosis, malignancies and some bacterial infections.
Causes of leukocytosis
This condition in most cases is the body’s reaction to factors that can change the constancy of the internal environment (homeostasis).
Conventionally, they can be divided into physiological, pathological factors and blood diseases themselves.
Physiological factors
The impact of this group of causes is not a manifestation of the disease; the number of cells increases temporarily and returns to normal on its own. These include:
- Eating leads to a slight increase in leukocytes to 10-12 x 109 per liter of blood, their return to normal occurs within a few hours. Therefore, it is recommended to donate blood for clinical analysis on an empty stomach.
- Physical activity – during muscular work, lactic acid accumulates in the body, causing an increase in white blood cells.
- Exposure to high or low temperatures.
- Stress, nervous tension.
- Leukocytosis during pregnancy is associated with changes in a woman’s hormonal levels in the second trimester of pregnancy. To exclude pathology, additional studies are carried out.
- Physiological leukocytosis in newborns - after the birth of a child, this is necessary for the baby to meet the external environment, for its additional protection from aggressive factors and infections.
Pathological factors
This group of causes leads to persistent leukocytosis; its return to normal does not occur on its own, but only after appropriate treatment aimed at eliminating the causative factors, namely:
- Bacterial infection - all pathogenic bacteria, entering the body, cause an inflammatory reaction and leukocytosis due to neutrophils.
- Viral infection - lymphocytes increase, which destroy cells affected by the virus.
- Allergic reactions - when an allergen enters the body, eosinophils and basophils are activated, they secrete specific substances responsible for the manifestations of allergies.
- Infarctions of various organs are the death of organ cells due to acute disruption of blood circulation in it, leading to aseptic (non-bacterial) inflammation. In this case, monocytes and neutrophils utilize dead cells.
- Extensive burns - neutrophils and monocytes utilize dead cells of damaged tissues.
- Significant blood loss - the number of all blood cells increases due to a decrease in the volume of its liquid part (plasma).
- Removal of the spleen - the spleen is responsible for the disposal of leukocytes and red blood cells, in the absence of which old cells accumulate in the blood.
- Uremia - an acute disorder of the kidneys causes an increase in the concentration of unresolved protein breakdown products, leading to intoxication (poisoning).
Blood diseases
These diseases include leukemia, which is characterized by the uncontrolled division of malignant cells in the bone marrow.
Moreover, almost all leukocytes are defective, unable to perform their functions. Depending on the severity, several forms of leukemia are distinguished.
- leukemic - the number of leukocytes is 50-80 x 109 per liter;
- subleukemic – 10-50 x 109 per liter;
- leukopenic – in this form – reduced;
- aleukemic – almost complete absence of them.
It is worth noting that the causes of leukocytosis in children are the same as in adults, but the speed and severity of the increase in the number of leukocytes is much higher.
So, with the same infection, a child’s body’s reaction will be more pronounced than an adult’s.
The process of growth of leukocytes in the blood can be pathological or physiological in nature.
Classification and characteristics of white blood cells
Approximately half a century ago, the lower limit of normal leukocytes fluctuated between 5.5-6.0 G/l; currently this level has dropped to 4.0 G/l, or even less . This is due to widespread urbanization, increased radioactive background, and the use of a large number of medications, sometimes unjustified. However, leukocytosis has not disappeared anywhere and, under certain circumstances, makes itself felt as a symptom of some disease, since it is not an independent nosological unit.
The following types of leukocytosis are distinguished:
- Physiological ( redistribution
or, as they used to call it,
relative
), due to the redistribution of an increased number of white blood cells between the vessels of various organs; - Pathological
(
reactive
or
absolute
), associated with a violation of leukopoiesis in the pathology of the hematopoietic organs or arising as a response of the body to infectious, purulent-inflammatory, septic and allergic processes.
This is interesting: Cerebrasthenic syndrome (CAS) in children and adults: causes, signs, how to treat
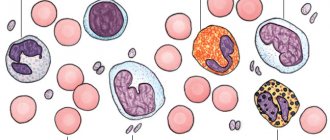
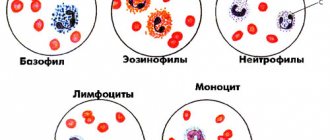
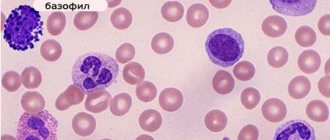
Classification of leukocytes and leukocytosis is based on the types of white blood cells, their functions and behavior. White blood cells, depending on the presence or absence of specific granules in the cytoplasm, are divided into two series: granulocytic
and
agranulocytic
.
What kind of cells are these - leukocytes? Why do they behave this way and why do they care? What do the terms “ neutrophilic and eosinophilic leukocytosis”
” that doctors often mention? Why is leukocytosis dangerous or is it not dangerous at all?
And you can understand this if you know the basic properties of leukocytes.
Basic properties of leukocytes, their tasks and functions
The size of leukocytes, depending on the type, ranges from 7.5 to 20 microns; they contain many enzymes (peptidases, lipases, diastases, proteases), which in a quiet state are isolated (in lysosomes) and are called lysosomal enzymes. Leukocytes perform their functions outside the vessels, and they use the vascular bed only as a road. They are characterized by an amoeboid movement, with the help of which they penetrate the endothelium of the capillaries ( diapedesis
) and are directed to the lesion (
positive chemotaxis
).
The reverse movement of leukocytes from the source of irritation is called negative chemotaxis
.
If we talk about the norm of leukocytes, then the range of variation here is quite wide (4.0-9.0 G/l) , moreover, blood taken from a finger contains information about only a sixth of white cells, because their main habitat is fabrics. And in order to understand where the norm is and where the pathology is, of course, you need to know what the population of leukocytes is, what tasks it performs, what they are needed for and whether you should worry at all if suddenly a high content of white cells is detected in a general blood test.
The lifespan of leukocytes depends on the type and ranges from several days to 20 years or more. Those leukocytes that have turned into “memory cells” are destined to live long, since even after a long period of time they are obliged to recognize the “foreign” that they met many years ago. Having “remembered” it, they must immediately “inform interested” species. They, in turn, must “give the command” to destroy the stranger.
The main tasks of white blood cells can be represented as follows:
- Leukocytes take part in the formation of cellular and humoral immunity, which constitutes their protective
function; - They enter the gastrointestinal tract, capture nutrients and transport them into the blood, which is especially important for newborns who, while breastfed, receive ready-made, unchanged maternal immunoglobulins along with milk, which can protect a small person from many infections. That is why a child under one year old is not afraid of, for example, the flu. Nature has thought of everything, endowing leukocytes with a metabolic
function; - They dissolve (lyse - lysis) damaged tissues and carry out the histolytic
task; - They destroy various bookmarks that are not needed at all, even in the embryonic period - a morphogenetic
function.
A detailed blood test involves counting not only the total number of leukocytes, but also the percentage of all types of white blood cells in the smear. By the way, the percentage must be converted into absolute values ( leukocyte profile
), then the information content of the analysis will increase significantly.
Granulocyte series
The progenitors of leukocytes (myeloblasts), belonging to the granulocytic series, originate in the bone marrow, where they pass through several stages and do not enter the bloodstream until the end of maturation. In the peripheral blood, under some pathological conditions (or purely by chance - 1 cell), metamyelocytes can be found. These are young (juvenile) cells, they are also the precursors of granulocytes. However, if for some reason young ones appear in the blood, and at the same time they can not only be seen, but counted in a smear, then we can judge a shift to the left
(for leukemia, infectious and inflammatory diseases).
An increase in the stroke of older forms indicates a shift of the formula to the right
.
formation of blood cells from stem cells in the bone marrow
Cells of the granulocyte series are endowed with pronounced enzymatic and metabolic functions, therefore their characteristic neutrophilic, eosinophilic and basophilic granularity is closely related to the activity of the cell and is strictly specific
, i.e., cannot transform from one type to another.
Representatives of granulocytes
Mature granulocytes include:
I. Neutrophils
Neutrophils
represent the largest group of white cells and make up 50-70% of the entire population. The granules located in their cytoplasm have high bactericidal activity (myeloperoxidase, lysozyme, cationic proteins, collagenase, lactoferrin, etc.). In addition, neutrophils have receptors for immunoglobulins (IgG), cytokines and complement proteins. Only 1% of these cells are normally found in the blood, the rest are concentrated in tissues.
Neutrophils are the first to rush to foci of inflammation, phagocytose (capture) and destroy harmful agents; they are the body's main defenders from microbes and toxins. With various infections, their number can increase 5-10 times (neutrophilic leukocytosis), and then not only mature, but also young cells, up to myelocytes, begin to enter the peripheral blood. In such cases, they speak of a leukocyte formula with a shift to the left.
II. Eosinophils
Eosinophils
make up 1-5% of all leukocytes. They got their name because they lend themselves well to staining with eosin dye. They remain in the bloodstream for several hours, and then are sent to the tissues, where they are destroyed. Eosinophils perform phagocytic and detoxification functions (neutralize toxins), destroy foreign proteins, neutralize antigen-antibody reaction products by capturing histamine and other substances, produce histaminase, participate in the formation of plasminogen, that is, they are a part of fibrinolysis. In addition to the listed advantages, eosinophils contain:
- Antiparasitic alkaline protein;
- Prostaglandins;
- Leukotrienes;
- Histaminase;
- Inhibitors of mast cell and basophil degranulation;
- They have receptors for IgE, IgG, IgM.
This is interesting: Sclerotherapy of leg veins: an effective method for undeveloped varicose veins
Given such a wide composition of leukocytes of this type, eosinophilic leukocytosis is a significant diagnostic indicator for helminthic infestations and allergic reactions, when the number of eosinophils increases, and an encouraging sign for ARVI and some other infections. Elevated levels of eosinophils in such cases indicate impending recovery.
III. Basophils
Basophils are literally rare in a smear, only 0-1%. Their task is to produce histamine, which dilates capillary vessels and promotes wound healing, and heparin, which is a natural anticoagulant (anti-clotting system of the blood). They, along with mast cells, are also called heparinocytes. Basophils contain platelet activating factor (PAF), prostaglandins, and leukotrienes. They are equipped with IgE receptors, which play an important role in the release of histamine and the manifestation of allergic reactions (urticaria, anaphylactic shock, bronchial asthma).
Granulocytes are also interesting because they replenish energy reserves through anaerobic glycolysis and thrive in oxygen-poor tissues, which is why they rush to areas of inflammation that are poorly supplied with blood. The neutrophils themselves, when they die, release lysosomal enzymes, which soften the tissue and form a purulent focus (abscess), so the pus consists of destroyed neutrophils and their fragments.
Non-granular agranulocytes
The importance and significance of agranulocytes in all immunological reactions can hardly be overestimated, since they play a leading role in ensuring cellular and humoral immunity. Certain types of leukocytes-agranulocytes are designed to perform the following tasks:
Monocytes
Monocytes
make up 2-10% of the entire leukocyte community (macrophages).
They arrive at the scene of the incident (damage zone) immediately behind the neutrophils, have powerful bactericidal properties (especially in an acidic environment), phagocytize microorganisms, destroyed leukocytes and dead tissue cells, freeing the inflammation zone, for which they are called “ the body’s wipers
”;
Lymphocytes
Lymphocytes - (20-40% of all Le) cells that have left the blood vessel, following their specialization, do not return back. In addition, they live for a long time - tens of years, especially “memory cells”.
Lymphocytes
– are the central link of the immune system (immunocompetent cells), they take care of maintaining the constancy of the internal environment of the body and are able to recognize “theirs” and “theirs”. In addition, the activity of lymphocytes is not limited to these tasks:
- They synthesize antibodies ( B lymphocytes
); - Lyse foreign cells. This function belongs to natural killers (N-killers), which are called zero because they do not belong to either the B or T lymphocyte
communities; - Provide immunological reactions “graft versus host” and “host versus graft”;
- Destroy their own mutant cells;
- They bring the body into a state of sensitization when foreign proteins enter.
Lymphocytes are formed from a common stem cell. Some are sent to the thymus gland (thymus), where they undergo “training” and become T-lymphocytes of various “professions”:
- T-helpers or assistants (they know everything and give commands);
- T-suppressors (suppress the immunological reaction when it is no longer needed);
- T-killers (they themselves kill at the level of cellular immunity);
- T-amplifiers (effectors, accelerators of immune processes);
- Immunological memory cells that carry information about past diseases (why many people get an infection once in their life).
B cell differentiation occurs in the red bone marrow and lymphoid organs. Their main function is active antibody formation and providing all stages of humoral immunity.
Only a small portion of lymphocytes circulate in the peripheral blood; the rest constantly migrate through the lymph nodes, spleen and bone marrow.
Symptoms of leukocytosis
Leukocytosis is not an independent disease, and therefore its symptoms coincide with the signs of the diseases that caused it.
In children, leukocytosis is often asymptomatic, which is why doctors recommend that parents periodically have their child’s blood tested in order to detect abnormalities in the composition of the blood at an early stage.
The most dangerous, although the rarest type of leukocytosis is leukemia, or blood cancer, and therefore it is necessary to know its symptoms so as not to miss the onset of the disease. So, with leukemia, the common symptoms of leukocytosis are as follows:
- Unreasonable malaise, weakness, fatigue;
- Increased body temperature, increased sweating at night;
- Spontaneous hemorrhages, frequent formation of bruises;
- Fainting, dizziness;
- Pain in the legs, arms and abdomen;
- Labored breathing;
- Poor appetite;
- Unexplained weight loss.
If you find yourself with two or more of the listed signs, you should consult a doctor and take a blood test.
Common signs of the disease are:
- visual impairment;
- difficulty breathing;
- dizziness;
- increased sweating;
- weakness;
- causeless fatigue;
- frequent leakage or bleeding;
- increased body temperature;
- tingling or pain in the arms and legs;
- sudden weight loss.
However, very often leukocytosis occurs without symptoms, or only signs of the underlying disease are present.
The main symptoms of leukocytosis are:
- weight loss;
- bleeding;
- formation of hematomas;
- enlarged liver and spleen;
- inflammation of the lymph nodes;
- fever;
- feeling tired, weak;
- dizziness, fainting;
- tingling in the legs, arms, abdominal area;
- poor appetite;
- labored breathing.
Diagnostics
To identify this disease you may need:
- take a general blood test;
- take a complete blood test;
- perform a bone marrow biopsy;
- perform a lymph node biopsy;
- do a biopsy of the liver and spleen;
- give a peripheral blood smear.
The analysis should be deciphered by an experienced therapist who, based on the results, can confirm or refute the diagnosis.
If alarming symptoms are observed in a child, diagnosis and examination must be done by a pediatrician. It should be remembered that treatment of leukocytosis cannot be carried out without identifying the cause that caused it.
An increase in the number of leukocytes can be detected during a general blood test.
It is also indicated to donate urine, in which the appearance of white cells can be detected. When examining pregnant women and women after childbirth, leukocytosis is detected in the smear. Once the diagnosis is confirmed, a treatment plan is drawn up.
Treatment of leukocytosis
Treatment is entirely aimed at eliminating the causes, for which various approaches are used:
- antibiotics for bacterial infections;
- antiviral drugs;
- antiallergic drugs;
- restoration of tissues and organs after burns or heart attacks;
- detoxification therapy for uremia;
- chemotherapy and bone marrow transplantation in case of leukemia;
- increase in plasma volume after bleeding.
An important stage in the treatment process is proper individual nutrition. In the case of a low level of leukocytes, the diet should be enriched with foods that stimulate the production of hemoglobin.
It is best to eat foods enriched with vitamin B9, legumes, and drink milk. You should also limit your consumption of meat products, completely excluding kidneys and liver.
Prevention
For prevention it is recommended:
- preventing the development of bacterial and infectious diseases;
- regular examinations with a therapist;
- regular testing;
- systematic increase in immunity;
- preventive examinations by specialists;
- following the principles of rational nutrition;
- maintaining a healthy daily routine;
- for pregnant women - healthy sleep at least eight hours a day and good nutrition.
An experienced therapist should treat leukocytosis in the blood. You may need the help of an infectious disease specialist, gastroenterologist, nephrologist, urologist, gynecologist, urologist, etc.
Complications from bad blood
If the disease is advanced and no treatment occurs, then a high level of leukocytes in the blood leads to a large number of complications, such as:
- The appearance of purulent inflammations (abscesses, furunculosis).
- In the presence of cancer, the risk of developing metastases increases.
- The occurrence of immune pathologies (dermatitis, lupus).
- The appearance of peritonitis.
- Untreated leukocytosis during pregnancy can cause miscarriage, premature birth, and various fetal pathologies.
- For newly born babies, it is dangerous due to all sorts of disorders and developmental delays.
An elevated level of leukocytes is a reason to pay attention to your own health. Despite the fact that sometimes the disease can be short-term, it may indicate that the body has some concomitant diseases that require mandatory therapy.
Only medical research will help to accurately determine the real cause of the high level of leukocytes, and the doctor will prescribe the appropriate treatment. Therefore, there is no need to postpone a visit to the doctor and refuse medical examination in order to exclude complications and major problems regarding your body.