Decreased monocytes in the blood
Monocytopenia is a decrease in the number of monocytes in the blood to <500/µL or less (sometimes to almost zero). The risk of certain infections will be increased if monocytopenia develops. This condition is usually diagnosed by assessing a general blood test with the calculation of the leukocyte formula in percentage and absolute values. If the condition is severe, the number of monocytes and other cells along with it is sharply reduced, then treatment with hematopoietic stem cell transplantation (cells from the bone marrow) may be required.
Video - monocyte blood test
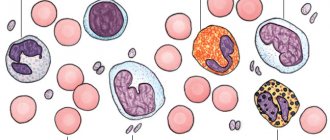
Monocytes are one type of leukocytes - white blood cells. They are large in size, without specific granularity and with a simple, non-segmented nucleus.
Like all white cells, monocytes are produced in the bone marrow. From there they enter the bloodstream not fully ripe. The ability of monocytes to absorb harmful microorganisms reaches its peak during this period.
They are the most prominent representatives of phagocytes. Monocytes bind pathogenic test cultures on their surface, envelop and digest them. This is how the cells fulfill their purpose - they protect the body from harmful particles and protect its health.
The proportion of monocytes among other leukocytes should not exceed 11%. An increase in their level or an increase in absolute quantity is an undesirable phenomenon. This often happens because pathologies begin to develop in the body. But it is possible that such changes in the composition of the blood are explained by physiological reasons.
What are monocytes?
Monocytes from the peripheral blood, where they are found in healthy people, migrate into tissues in the presence of special conditions - inflammation, infection, damage. There they become macrophages, with specific characteristics depending on the location and tissue affected. Thus, they are considered the main "orderlies" of the body and destroy broken cells, microbes or neoplastic tissues.
Monocytopenia may increase the risk of infection and may indicate a poor prognosis in patients with liver damage caused by drugs, toxins, or in people with thermal injuries (severe tissue burns). Peripheral blood monocytopenia does not usually indicate a decrease in the number of tissue macrophages. Typically, monocytes in the blood decrease in the acute stage of infection or injury, when all the cells go into the tissue to fight damage and the penetration of infection into the body, especially microbial ones.
In some cases, a decrease in monocytes in the blood may be associated with impaired granuloma formation in response to infections.
Monocytes are elevated in adults: reasons
Exceeding the norm by monocytes is called monocytosis. There are two types of this condition:
Absolute
– characterized by an increase in the total number of cells. Their number exceeds the established norm, the size of which for adults is 0.70 x 10 9 / l.
Relative
– the specific gravity of monocytes crosses the optimal upper limit of 11%.
The presence of monocytosis may be natural. The relative growth of monocytes often occurs under the influence of certain physiological factors, namely:
- emotional outbursts and stress. Both positive and negative experiences have the same impact;
- a hearty meal consisting of fatty and spicy dishes;
- ingestion of certain medications.
For women, the phase of the menstrual cycle is also important.
The individual characteristics of a particular person, his biorhythms can provoke the growth of monocytes.
Since the cells perform protective functions, their level and number increase when any inflammatory process occurs.
A slight monocytosis is observed when the body has suffered illnesses of varying severity and has already begun to recover.
Cell growth can be caused by poisoning with dangerous chemical elements such as phosphorus or tetrachloroethane.
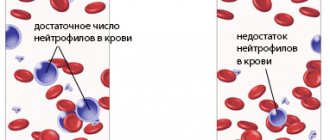
Causes of monocytopenia
Monocytopenia that does not resolve with repeated blood tests may result from:
- Myelosuppression (suppression of bone marrow activity) caused by chemotherapy (along with other cytopenias).
- Mutations of hematopoietic cells involving GATA2 (damage to hematopoietic growth, from which monocytes are formed).
- Neoplastic, cancerous disorders (eg, hairy cell leukemia, acute lymphoblastic leukemia, Hodgkin lymphoma).
- Infections (eg, HIV infection, Epstein-Barr virus, adenovirus infection, miliary tuberculosis).
- High-dose, long-term corticosteroid or immunoglobulin therapy for severe infections or autoimmune diseases.
- Gastric or intestinal resection (removal of part of the stomach or intestine due to tumor or damage).
Temporary monocytopenia can occur with endotoxemia (acute intestinal and other poisonings), hemodialysis or cyclic neutropenia.
What to do if the analysis shows a decrease in monocytes
If abnormalities are detected as a result of a blood test, you should consult a doctor. You need to visit the specialist who prescribed the diagnosis or therapist. If necessary, he will provide recommendations for highly specialized specialists.
The first thing the doctor does is rule out physiological prerequisites for abnormalities in the results of the OAC. He interviews the patient about recent illnesses, drug therapy, and compliance with the rules for preparing for analysis. After collecting anamnesis, the doctor will examine the patient to detect objective symptoms, which can narrow down the search for the causes of monocytopenia.
In order to correctly diagnose and select therapy, the OAC will have to be repeated (to refute or confirm the violations). To supplement the information received, they may assign:
- blood chemistry;
- urine test;
- PCR or ELISA diagnostics for common infections (AIDS, syphilis, STIs);
- Ultrasound, CT or MRI of internal organs;
- tumor markers;
- bone marrow biopsy.
Monocytopenia due to GATA2 mutation
Patients with mutations in the hematopoietic transcription factor gene, GATA2, may experience severe deficiency or absence of monocytes. Dendritic cells are reduced, and there may also be lymphocytopenia (mainly natural killer cells and B cells).
Despite the almost complete absence of circulating monocytes, tissue macrophages usually persist. Also, normal immunoglobulin levels usually remain even when circulating B cells are depressed. Bone marrow is hypocellular (produces few cells) and may have fibrosis (replacement of some cells with connective tissue) and dysplasia—changes in cellular composition. Karyotypic disorders, including monosomy 7 and trisomy 8, may be present in some people.
Reduced monocytes in the blood of adults: what to look for?
Infections with Mycobacterium avium complex (tuberculosis microbes) or other non-tuberculous mycobacterial infections (MonoMAC syndrome) are common in monocytopenia. Fungal infections (eg, histoplasmosis, aspergillosis) are also common causes of monocytopenia. Human papillomavirus (HPV) infections may occur more frequently, with a subsequent risk of progression to secondary cancers. There is a high risk of progression to hematological disorders (myelodysplasia, acute myelogenous leukemia, chronic myelomonocytic leukemia, lymphomas) with a poor prognosis.
Unvaccinated patients should receive the HPV vaccine.
Any infections are treated with appropriate antimicrobial agents. Allogeneic hematopoietic stem cell transplantation should be considered for patients with severe symptoms of infections.
Alena Paretskaya, pediatrician, medical columnist
just today
( 49 votes, average: 4.24 out of 5)
Increased monocytes in the blood: possible causes of pathology
Lymphoblastic leukemia: symptoms and treatment
Related Posts
The child's neutrophils are low and lymphocytes and monocytes are high
When the doctor says that the blood test is unfavorable and there are problems, many people panic. This is especially noticeable when studies talk about a child’s illness.
When white blood cells are higher or lower than normal, this means the following:
- neutrophils are decreased;
- lymphocytes are higher than normal;
- simultaneously increased level of lymphocytes and decreased level of neutrophils.
The reasons are different, and the attending physician has to identify them and help the patient get rid of them. Lymphocytes in the blood will help find the sources of problems.
Immune system cells
Neutrophils and lymphocytes are among the white cells. Among ordinary people they are known as leukocytes. A certain type of cell in this broad group has a specific function aimed at protecting against disease. When performing a blood test, the doctor takes into account the relative content of each type of white blood cell, not just the level of white cells.
What are leukocytes? These include colorless blood cells that form a “dam”, a shield that will not allow infection to pass through. These cells contain substances with which the body gets rid of pathogenic organisms. They are able to neutralize the decay products of harmful microorganisms.
What functions do lymphocytes perform?
Lymphocytes are specific cells that are formed in the bone marrow. They are a defense mechanism against infections and are therefore considered the main components of the immune system.
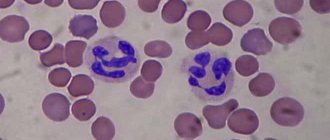
Neutrophils are the most numerous class of immune cells (their part ranges from 45 to 72%). The function of neutrophil cells is to destroy bacteria. If foreign bodies enter the body, this type of white blood cell immediately rushes to the part of the body from where they came. Ultimately, infections are absorbed by neutrophil cells and digested.
Other leukocyte cells and their significance
In order for the picture to be complete, it will be necessary to consider blood components that are less significant for the body (but not for the immune system). These groups of leukocytes include the following:
- Monocytes. Large elements related to phagocytes. Diseases develop depending on the number of monocytic type cells. An increase in the percentage of monocytes indicates relative monocytosis. If monocytes are increased in number, then doctors diagnose absolute monocytosis. Sometimes other blood cells can change their numbers along with monocytes. Lymphocytes and monocytes are rarely elevated at the same time in a child. The main cause of the phenomenon is infections.
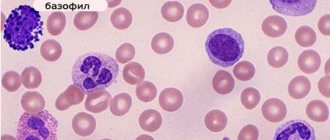
- Basophils. They are classified as scouts. Basophils contain histamine, serotonin and other highly active components. Upon contact with allergens, they burst and their contents affect the allergen.
- Eosinophil cells. Eosinophils are a population of leukocytes that perform a marker function. Disease cells are identified. The norm of eosinophils for humans is from 1 to 5%. When lymphocytes and eosinophils are elevated, this indicates the body is allergic. If eosinophils are elevated in a child, an analysis is performed for helminthic infestations, rhinitis, scarlet fever and chickenpox.
All cells associated with leukocytes should be normal. If levels are low or high, therapy should be carried out immediately to stabilize them.
The role and indicators of the number of neutrophils in the blood
Neutrophil balance is an important indicator for the body. The number of these cells is normal if their percentage ranges from 45 to 72%. A lower value is typical for children under one year old, and the older the child, the more leukocytes of this type are in the body.
Note! The percentage of cells may increase, but their number remains the same with age.
What happens when neutrophil activity increases or decreases?
If neutrophils are elevated, then this is neutrophilia. Most often, the disease is caused by the development of inflammation. By examining the number of neutrophil granulocytes, conclusions are drawn about the scale of inflammatory processes and the resistance of the immune system. If children are 1 year old, then there is no need to worry about neutrophilia when their percentage of corpuscles is about 30%.
If a child’s neutrophils are low and lymphocytes are high, then it makes sense to consider not only viral infections. The reasons why neutrophils are reduced and lymphocytes are increased in adults or children are malignant tumors, radiation and medications. If, when neutrophils decrease, other cells increase, then the immune system fights the disease.
A decrease in neutrophils is associated with the following factors:
- infection of the body with viral infections;
- advanced inflammation;
- use of radiation therapy;
- exposure to radiation;
- development of agranulocytosis (signals that there are no granulocytes and lymphocytes in the blood).
Low neutrophils in the blood can be caused by medications, or rather, side effects from them.
Therefore, in the deciphering process, it is worth considering the number of neutrophils, since their increase or decrease indicates violations. If you pay attention to these changes in time, you can avoid some of the negative consequences caused by inflammatory processes.
Functions and norm of lymphocytes
Lymphocytes are responsible for the adaptive function of the immune system. This means that the ability to resist infection adapts to the environment as we age.
These particles belong to one of the following categories:
- T-lymphocytes – contribute to the formation of thymus and thymus cells; play an auxiliary role in the process of synthesis of signal substances;
- B-lymphocytes - take part in the production of bone marrow cells, which allows us to call them the “parents” of the body’s immune function; with their help, antibodies are produced.
- natural “killers” – secrete cytotoxins that help cope with pathological cells.
Note! Lymphocytes are low when their content in the blood of adults and children under 6 years of age is less than 25 and 45%, respectively.
High lymphocytes make it clear that the body has the following ailments:
- viruses;
- tuberculosis;
- lymphocytic leukemia;
- hyperthyroidism – increased production of thyroid hormones;
- lymphosarcoma.
Depending on the increased or decreased portion of the corpuscles, the state of the body and the presence of diseases of viral etiology are judged. Elevated lymphocytes will indicate inflammation. Therefore, it is imperative to visit a doctor after a disappointing analysis.
It is worth noting the possibility of human vaccination, which opens up thanks to lymphocytes. This is possible due to the fact that the bodies contain memory cells. They store antigens in a coded state.
Analysis and its features
Lymphocytes and neutrophils can tell a lot about a patient's condition. Therefore, it is recommended to take a general blood test once a year. Deciphering will allow you to detect hidden pathological processes caused by low levels of leukocytes or their high proportion in the blood.
Low corpuscle count is determined by blood test
An increased or decreased proportion of corpuscles indicates disease.
- Acute viral infection. It is indicated by an increase in the number of leukocytes, low neutrophils and an increased content of lymphocytes.
- Chronic viral infection. Here the analysis is ambiguous. Therefore, the following picture is observed:
- the quantitative content of leukocytes is optimal or reduced;
- increased lymphocytes or their presence at the upper limit of the normal value;
- the low content of neutrophils is insignificant or they are close to the lower limit of normal.
- Acute bacterial infection. There is a reduced level of lymphocytes. The total number of leukocytes increases, the level of neutrophils is high.
- Chronic or local bacterial infection. The same symptoms are noted as in the previous case. But they are closer to normal levels.
Counting the number of white cells will identify many infections. By analyzing the high or low percentage of white blood cells, the doctor will order tests and make a diagnosis. The analysis will help detect rare autoimmune diseases, blood diseases and immune deficiencies. When white blood cells decrease or some of them increase, the quality of chemotherapy is judged.
The process involves taking fluid from a vein and finger. Most often, material collection for diagnostics is carried out without complications. But sometimes it happens that the doctor cannot find the vein or the needle gets stuck in the muscle.
Data decryption
What does the high content of certain cells or their reduced number indicate? If some cells increase, accompanied by a decrease in others, then this indicates one thing - there is inflammation, which the body is fighting.
If lymphocytes are elevated, the following diseases should be diagnosed:
- tuberculosis;
- thyroid disorders;
- lymphocytic leukemia;
- illnesses of viral etiology (this is evidenced by decreased cells).
Medicines can cause a reduced number of lymphocytes. Radiation therapy for cancer can affect the indicators. And if the test results exceed the norm or the number of cells is reduced, then you should think about the reasons. Only the attending physician will tell you why lymphocytes are increased in an adult and neutrophils are decreased.
A high proportion of leukocytes will indicate problems with immunity
It is worth considering other decryption options that are encountered. If segmented neutrophils are reduced in an adult, and lymphocytes are increased, this indicates that the disease has passed. There will soon be no trace of the increase or decrease - the leukocytes will return to normal.
Important! Segmented cells are called mature cells, i.e. those that interacted with infections.
Application of ionizing radiation also results in low or high white blood cells. Therefore, this should not be ruled out. There may be many or few leukocytes in the case of immune agranulocytosis. This disease represents the death of neutrophils even before formation.