| Acquired heart defects | |
| ICD-10 | 34.-37., 05.-08., 22.-23. |
| ICD-9 | 394394-396396, 746746 |
| ICD-9-CM | 424.99[1] |
| MeSH | D006349 |
| Media files on Wikimedia Commons | |
See also: Congenital heart defects
Main article: Heart diseases
Acquired heart defects
, also called
valvular defects
, is a disorder of the heart caused by morphological and/or functional changes in one or more of its valves. Valve changes can be in the form of stenosis, insufficiency, or a combination of both. They are the result of infection, inflammation or autoimmune reactions, overload and dilatation of the heart chambers.
Content
- 1 Classification 1.1 According to the location of the heart lesion
- 1.2 According to functional form
- 1.3 Types of defects
- 4.1 Clinical manifestations of mitral valve insufficiency.
Etiology
The cause of congenital heart disease can be genetic or environmental factors, but usually a combination of both[2].
Genetics
The most well-known causes of congenital heart defects are point gene changes or chromosomal mutations in the form of deletion or duplication of DNA segments[3].
Major chromosomal abnormalities, such as trisomy 21, cause about 5-8% of congenital heart disease cases[2]. Trisomy 21 is the most common genetic cause[3]. Some genes are associated with specific defects. Mutations in the cardiac muscle protein α-myosin heavy chain (MYH6) are associated with atrial septal defects. Some proteins that interact with MYH6 are also associated with heart defects. The transcription factor GATA4 forms a complex with the TBX5 gene, which interacts with MYH6. Another factor, the homeobox protein NKX2-5, also interacts with MYH6. Mutations of all these proteins are associated with the development of atrial and ventricular septal defects. Additionally, NKX2-5 is associated with defects in cardiac electrical conduction, and TBX5 is associated with Holt-Oram syndrome. Another T-box gene, TBX1, is associated with DiGeorge syndrome, the deletion of which results in a variety of symptoms, including cardiac output defects and tetralogy of Fallot[4]. Examples of genetic products and associated expressions
| MYH6 | GATA4 | NKX2-5 | TBX5 | TBX1 | |
| Locus | 14q11.2-q13 | 8p23.1-p22 | 5q34 | 12q24.1 | 22q11.2 |
| Syndrome | Holt-Oram syndrome | DiGeorge syndrome | |||
| Atrial septal defects | ✔ | ✔ | ✔ | ✔ | |
| Ventricular septal defects | ✔ | ✔ | ✔ | ||
| Electrical conductivity disorders | ✔ | ✔ | |||
| Blood outflow disorders | ✔ | ||||
| Non-cardiac symptoms[5] | Upper limb defect | Small or absent thymus Small or absent parathyroid glands Facial defects |
Environmental factors
Genetic mutations occur due to the action of three main mutagens:
- Physical mutagens (mainly ionizing radiation).
- Chemical mutagens (phenols of varnishes, paints; nitrates; benzpyrene from smoking; alcohol consumption; hydantoin; lithium; thalidomide; teratogenic medications - antibiotics and CTP, NSAIDs, etc.).
- Biological mutagens (mainly the rubella virus in the mother’s body, leading to congenital rubella with the characteristic Gregg triad - congenital heart disease, cataracts, deafness, as well as diabetes mellitus, phenylketonuria and systemic lupus erythematosus in the mother).
Factors that increase the risk of congenital heart defects
Infections suffered by the mother during the first trimester of pregnancy can significantly increase the risk of congenital heart defects; chronic diseases of the mother; the age of one of the parents in case of late parenthood; bad habits of parents; a large number of abortions suffered.[6]
Relationship between congenital heart defects and gender
A study of the relationship between congenital heart defects and gender was conducted in the early 70s using data collected in several large cardiac surgery centers, as well as literature data.
As a result of the analysis of 31,814 patients suffering from congenital heart defects and great vessels, a clear connection between the type of defect and the gender of the patient was revealed (Table)[7]. Based on gender ratio, birth defects can be divided into three groups - “male”, “female” and “neutral”. Gender ratio of patients with congenital heart defects and large vessels
| Congenital defect | Sex ratio, M:F |
| Patent ductus arteriosus | 1 : 2.72 |
| Lautembacher's disease | 1 : 2.14 |
| Secondary atrial septal defect | 1 : 1.84 |
| Ventricular septal defect and patent ductus arteriosus | 1 : 1.51 |
| Tetralogy of Fallot | 1 : 1.45 |
| Eisenmenger complex | 1 : 1.40 |
| Partial atrioventricular septal defect | 1 : 1.36 |
| Primary atrial septal defect | 1 : 1.20 |
| Partial anomaly of the connection of the pulmonary veins | 1 : 1.19 |
| Ventricular septal defect | 1 : 1.02 |
| Defect of the septum between the aorta and pulmonary artery | 1 : 1.01 |
| Complete atrioventricular septal defect | 1 : 1.01 |
| Ebstein's anomaly | 1.02 : 1 |
| Pulmonary stenosis | 1.04 : 1 |
| Tricuspid valve atresia | 1.16 : 1 |
| Common truncus arteriosus | 1.21 : 1 |
| Tetralogy of Fallot | 1.35 : 1 |
| Coarctation of the aorta and patent ductus arteriosus | 1.37 : 1 |
| Total anomaly of the connection of the pulmonary veins | 1.39 : 1 |
| Transposition of the great vessels | 1.90 : 1 |
| Coarctation of the aorta | 2.14 : 1 |
| Aortic stenosis | 2.66 : 1 |
The most clearly defined female congenital defects are patent ductus arteriosus (1♂♂ : 2.72♀♀); Lautembacher's disease (1♂♂ : 2.1♀♀); secondary atrial septal defect (1♂♂ : 1.84♀♀); ventricular septal defect and patent ductus arteriosus (1♂♂ : 1.51♀♀); Fallot's triad, that is, a combination of atrial septal defect, narrowing of the pulmonary artery orifice and right ventricular hypertrophy (1♂♂ : 1.45♀♀).
The most clearly defined “male” congenital defects are congenital aortic stenosis (2.66♂♂ : 1♀♀), coarctation of the aorta (2.14♂♂ : 1♀♀), transposition of the great vessels (1.90♂♂ : 1♀♀), total anomaly of the connection pulmonary veins (1.39♂♂ : 1♀♀), coarctation of the aorta and patent ductus arteriosus (1.37♂♂ : 1♀♀). None of the male components of congenital heart defects correspond to a similar formation in a normal embryo or in human phylogenetic predecessors.[8][9]
The remaining congenital heart defects are of the “neutral” type. Their frequency is approximately the same in both sexes. Among them, one can also distinguish simple (aortopulmonary septal defect, primary atrial septal defect, pulmonary stenosis) and complex (partial and complete atrioventricular septal defect, Ebstein's anomaly, tricuspid valve atresia, etc.).
Simple vices of this group, like female vices, are atavistic, but unlike female ones, they represent a return to a distant past in the ontogonetic and phylogenetic sense. They can be considered as a consequence of cardiac development arrest in the early stages of embryogenesis (the first 2-3 months of embryonic life, during which the anatomical formation of the heart occurs), and at earlier stages of phylogenesis compared to female defects. With complex defects of the neutral group, the sex ratio depends on the predominance of the female and male components in them.
Theories
Rokitansky (1875) believed that congenital defects are explained by arrest in the development of the heart at various stages of ontogenesis [10]. Spitzer (1923) interprets them as a return to one of the stages of phylogenesis[11]. Krymsky, synthesizing the two previous points of view, considers congenital heart defects as an arrest of development at a certain stage of ontogenesis, corresponding to one or another stage of phylogenesis[12]. Only atavistic heart defects (female and neutral) fit into the framework of these theories, and the entire group of male defects does not find an explanation, since none of the male components of congenital heart defects corresponds to a similar formation in a normal embryo or in human phylogenetic predecessors[8][ 9]. The application of the “Teratological Rule of Sexual Dimorphism” makes it possible to explain all three groups of defects.
The division of congenital heart defects and large vessels into male, female and neutral allows the patient’s gender to be used as a diagnostic symptom. At the same time, male and female defects have a fairly large coefficient of diagnostic value. For example, taking into account information about the patient’s gender increases the probability of diagnosis for patent ductus arteriosus by 1.32 times [13].
Classification
Play media file
The mechanism of development of mitral valve pathology. English with Russian subtitles.
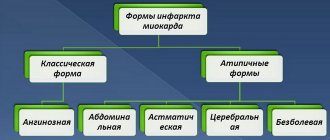
Many classifications of acquired defects have been proposed.
- By etiology: rheumatic, atherosclerotic, as a result of bacterial endocarditis, syphilitic, etc.
- according to the severity of the defect, which determines the degree of disturbance of intracardiac hemodynamics: a defect without a significant effect on intracardiac hemodynamics, moderate and severe severity
- according to the state of general hemodynamics: compensated, subcompensated and decompensated defects[2]
By location of heart damage
- Monovalvular defects (one valve is affected)
- Mitral valve
- Aortic defect
- Tricuspid defect
- Combined defects (two or more valves are affected)
- Two-valve defects Mitral-aortic defect
- Aortic-mitral valve disease
- Mitral-tricuspid defect
- Aortic-tricuspid disease
- Three-valve defects
- Aortic-mitral-tricuspid disease
- Mitral-aortic-tricuspid disease
According to functional form
- Simple vices
- Stenosis
- Failure
- Combined defects - the presence of stenosis and insufficiency of several valves.[3]
- Combined - the presence of stenosis and insufficiency on one valve.
Types of defects
| Affected valve | Stenosis | Failure |
| Aortic | Aortic valve stenosis | Aortic valve insufficiency |
| Mitral | Mitral valve stenosis | Mitral valve insufficiency |
| Tricuspid | Tricuspid valve stenosis | Tricuspid valve insufficiency |
| Pulmonary valve | Pulmonary valve stenosis | Pulmonary valve insufficiency |
Structure
The tricuspid valve consists of the following anatomical structures:
- three valves: septal (septal), anterior and posterior;
- chordae tendineae (first, second and third order);
- papillary muscles (from 3-4 to 7-10);
- fibrous ring.
Tricuspid valve dysfunction may occur as a result of certain diseases that lead to cardiac dysfunction. It can manifest itself in the form of stenosis (narrowing) and/or insufficiency.
The tricuspid valve, according to the scientific literature, is also called tricuspid. When the heart moves, all processes occur synchronously. If a blockage occurs in one of the departments, a minor temporary one, the body immediately senses that the condition changes significantly. The state of health immediately worsens, it becomes difficult to breathe and it is impossible to move.
The tricuspid valve is located on the left side of the sternum. It is part of the pumping system for pumping blood. It is a kind of cap that opens under the pressure of ejected blood.
Incomplete closure of the tricuspid valve occurs due to relaxation of the heart muscle, when it is no longer able to function normally. Due to a violation of the redistribution of internal pressures, tissues begin to break down, which as a result threatens the formation of heart disease. Some diseases become provocateurs of such pathology.
Clinical picture
With minimally expressed valve defects, the disease may not manifest itself clinically. With decompensation, a clinic of hemodynamic disorders appears in the pulmonary or systemic circulation. The most common symptoms are shortness of breath during exercise, cyanosis of the skin, swelling, palpitations, pain in the heart area, and cough.
Clinical manifestations of mitral valve insufficiency.
See also: Mitral valve prolapse
Subjectively
— in the compensation stage there are no complaints; with a decrease in the contractile function of the left ventricle and an increase in pressure in the pulmonary circulation, complaints appear about:
- shortness of breath, initially during exercise, and then at rest
- heartbeat
- pain in the heart area of an ischemic nature (due to delayed development of coronary collaterals with myocardial hypertrophy)
- dry cough
As the symptoms of right ventricular failure increase, swelling in the legs and pain in the right hypochondrium appear (due to enlargement of the liver and stretching of its capsule).
Objectively:
- examination: acrocyanosis, swelling of the jugular veins
- palpation: increased diffuse apical impulse, shifted to the left and often down in the 5th or 6th intercostal space; cardiac hump (with hypertrophy and dilatation of the right ventricle)
- percussion: expansion of the relative dullness of the heart, first to the left, up, and then to the right.
- Auscultation: the first sound at the apex of the heart is weakened or absent (since there is no “period of closed valves”); systolic murmur at the apex, spreading along the V and VI ribs to the axilla and to Botkin’s point and decreasing at the end of systole (arises due to the passage of blood from the left ventricle into the left atrium through a narrow gap between the valve leaflets); emphasis of the second tone over the pulmonary artery and its splitting (due to the rapid slamming of the valves with increasing pressure).
- characteristics of pulse and blood pressure: no characteristic changes.
Clinical manifestations of mitral stenosis
Main article: Mitral valve stenosis
Subjectively
- complaints about:
- shortness of breath, first during physical activity, then at rest; with a sharp rise in pressure in the pulmonary circulation, cardiac asthma may occur
- cough is dry or with a small amount of mucous sputum
- Hoarseness of voice (Ortner's sign)
- hemoptysis (siderophages appear in the sputum - “cells of heart defects”)
- pain in the heart area, palpitations, interruptions; atrial fibrillation often develops
- weakness, increased fatigue (as characterized by fixation of cardiac output - lack of adequate increase in cardiac output during physical activity)
Objectively:
- examination: against the background of pale skin, a sharply defined purple “mitral” flush of the cheeks with cyanosis of the lips and tip of the nose (facies mitralis) is revealed; increased epigastric pulsation of the right ventricle (“heartbeat”); absence or weakening of the apical impulse (since the left ventricle is not enlarged in volume and is displaced by the hypertrophied right ventricle)
- palpation: when palpating the apex of the heart, especially after physical exertion in the position on the left side while exhaling, diastolic trembling (“cat’s purring” is due to fluctuations in the blood as it passes through the narrowed mitral orifice); symptom of Nesterov’s two hammers - if you put your hand with your palm on the top and your fingers on the area of the 2nd intercostal space to the left of the sternum, then the flapping 1st tone is felt by the palm as the first “hammer”, and the accented 2nd tone is felt by the fingers as the second “hammer”; heart hump.
- percussion: displacement of the borders of relative dullness of the heart upward (due to hypertrophy of the left atrium) and to the right (due to expansion of the right ventricle), while the borders of absolute cardiac dullness increase more than relative ones (since due to expansion of the right ventricle, the heart, spreading the edges of the lungs, presses against the chest wall with its right enlarged half).
- Auscultation: increased (popping) 1st sound above the apex of the heart (in diastole, the left ventricle is not filled with blood sufficiently and contracts rapidly); additional III sound at the apex (the sound of the mitral valve opening; associated with a sharp movement of the mitral valve leaflets at the beginning of diastole); I tone + II tone + click of the opening of the mitral valve - three-part rhythm at the apex of the heart - ri; diastolic murmur at the apex of the heart, occurring at various periods of diastole: protodiastolic murmur - occurs at the beginning of diastole, associated with the movement of blood through a narrowed opening due to the difference in pressure in the atrium and ventricle; decreasing, low rumbling timbre (palpatory equivalent - “cat purring”), heard in a limited space, better after physical activity, on the left side, on exhalation, not performed.
- presystolic murmur - occurs at the end of diastole due to active atrial systole; has an increasing character, disappears with atrial fibrillation
Clinical picture of aortic stenosis
Main article: Aortic valve stenosis
See also: Aortic heart disease
Subjectively
- is asymptomatic for a long time, the main complaints appear when the aortic opening is narrowed by 2/3 of the norm (less than 0.75 cm2):
- compressive pain behind the sternum during physical activity (decreased coronary circulation).
- dizziness, fainting (deterioration of cerebral circulation);
Subsequently, with a decrease in the contractile function of the left ventricle, the following appear: attacks of cardiac asthma; shortness of breath at rest; increased fatigue (due to the lack of an adequate increase in cardiac output during physical activity). When congestion occurs in the systemic circulation, patients complain of: swelling of the lower extremities; pain in the right hypochondrium (associated with liver enlargement and capsule stretching).
Objectively:
- examination: pallor of the skin (due to spasm of skin vessels as a reaction to low cardiac output), acrocyanosis (with decompensation), swelling of the lower extremities, swelling of the neck veins, pronounced apical impulse.
- palpation: a diffuse “high” resistant apical impulse is palpated, displaced downwards (VI intercostal space) and to the left (to the anterior axillary line); at the Botkin point and especially in the second intercostal space to the right of the sternum (above the aorta), systolic trembling (“cat purring”) is often detected, resulting from the turbulence of the blood as it passes through the narrowed aortic opening.
- percussion: expansion of the left border of the relative dullness of the heart, an increase in the size of the diameter of the heart (aortic configuration of the heart).
- auscultation: the first sound is weakened (due to the slow contraction of the left ventricle and prolongation of systole), the second sound is weakened above the aorta (and if the fused leaflets of the aortic valve are immobilized, it can completely disappear); a rough, increasing-decreasing systolic murmur with an epicenter above the aorta, carried out on the carotid arteries, intensifies when listening to the patient on the right side with breath-holding during exhalation.
- characteristics of pulse and blood pressure: pulse is small, slow and rare (blood passes into the aorta slowly and in smaller quantities); systolic blood pressure is reduced, diastolic blood pressure is normal or increased, pulse pressure is reduced.
Clinical picture of aortic insufficiency
Main article: Aortic heart disease
Subjectively
- in the stage of compensation of the defect, the general state of health is satisfactory, only sometimes patients feel palpitations (due to compensatory tachycardia) and pulsation behind the sternum (due to the movement of an increased volume of blood from the left ventricle to the aorta and back), with decompensation complaints of:
- pain in the heart area of an anginal nature, poorly or not relieved by nitroglycerin (caused by relative coronary insufficiency due to myocardial hypertrophy, deterioration of blood supply to the coronary arteries with low diastolic pressure in the aorta and due to compression of the subendocardial layers by excess blood volume)
- dizziness, tendency to faint (associated with impaired brain nutrition)
- shortness of breath, first during physical activity, and then at rest (appears when the contractile function of the left ventricle decreases)
- swelling, heaviness and pain in the right hypochondrium (with the development of right ventricular failure)
Objectively:
- examination: pallor of the skin (caused by low blood supply to the arterial system during diastole); pulsation of peripheral arteries - carotid (“carotid dance”), subclavian, brachial, temporal; rhythmic shaking of the head, synchronous with the pulse (Musset's symptom); a rhythmic change in the color of the nail bed and lips with light pressure with a transparent glass on the mucous membrane of the lips, at the end of the nail, the so-called capillary pulse (Quincke's symptom).
- palpation: the apical impulse is determined in the sixth, sometimes in the seventh intercostal space, outward from the midclavicular line, diffuse, intensified, lifting, dome-shaped.
- percussion: the border of relative cardiac dullness is shifted down and to the left, the diameter of the heart and the width of the vascular bundle are increased (aortic configuration).
- Auscultation: the first sound at the apex of the heart is weakened (the mitral valve leaflets close with less amplitude due to the left ventricle being overfilled with blood, the pressure in the cavity of the left ventricle increases slowly in the absence of periods of closed valves); The second tone on the aorta in case of rheumatic disease is weakened, in case of syphilitic and atherosclerotic disease it is sonorous, sometimes intensified and even with a metallic tint; murmurs: organic murmur - soft, blowing protodiastolic murmur over the aorta, conducted to the apex of the heart; with rheumatic disease, this noise is not rough, it is better heard at the Botkin-Erb point, with syphilitic disease - the noise is rougher, better heard in the second intercostal space on the right
- functional murmurs: systolic murmur at the apex (relative mitral valve insufficiency with large dilatation of the left ventricle); diastolic, presystolic Flint murmur (reverse blood flow during diastole from the aorta to the ventricle occurs with considerable force and pushes back the mitral valve leaflet, which creates functional stenosis of the mitral orifice, and during diastole an obstacle is created to the flow of blood from the left atrium to the ventricle).
On the femoral artery, a double Traube sound is heard (as a result of vibrations of the vessel wall during systole and during diastole) and a double Vinogradov-Durozier murmur (the first stenotic murmur is caused by blood flow through a vessel narrowed by a stethoscope; the second is due to the acceleration of reverse blood flow towards the heart during diastole time).
- characteristics of pulse and blood pressure: pulse is fast, high, large (due to high pulse pressure and increased volume of blood entering the aorta during systole); systolic blood pressure increases, diastolic blood pressure decreases, and pulse pressure increases.
Causes
Etiology • Rheumatism • Infectious endocarditis • Subendocardial fibroelastosis • Congenital anomalies (Ebstein's anomaly, etc.) • Idiopathic calcification • Myxoma of the right atrium • Secondary tumors of the right atrium (nephroblastoma sprouting from the inferior vena cava, metastases).
Pathophysiology • Hemodynamic abnormalities are similar to those of tricuspid regurgitation. The differences are that there are no changes in the pancreas, and stagnation in the systemic circulation occurs and progresses much faster • Since in the vast majority of cases, tricuspid stenosis is accompanied by insufficiency and defects of other valves, the general pathogenesis consists of the corresponding individual disorders • Based on the degree of narrowing of the valve opening, they are distinguished moderate (2.5–3 cm2), severe (1.5–2.5 cm2) and severe (less than 1.5 cm2) stenoses.
Clinical picture and diagnosis
• For complaints, see Tricuspid valve insufficiency.
• Valve symptoms •• Strengthening of the first tone, a click of the opening of the tricuspid valve •• With sinus rhythm - fusiform low-frequency diastolic murmur (intensifies on inspiration) •• The intensity and duration of the noise depend on the diastolic transtricuspid pressure gradient •• Auscultatory diagnosis of the defect is difficult due to the sound phenomena associated with concomitant anomalies of other valves.
• For symptoms of circulatory failure in the systemic circle, see Tricuspid valve insufficiency.
• Symptoms of the underlying disease (rheumatism, myxoma of the heart).
Among the established causes of weakening of the tricuspid valve are the following:
- Carcinoid syndrome.
- Consequences of developed rheumatism.
- With endocarditis of infectious origin.
- Mechanical damage to the papillary muscles or rupture of the chordae.
- Consequence of myocarditis.
- After cardiomyopathy.
- A consequence of severe conditions of thyrotoxicosis.
Congenital pathologies often occur together with other abnormalities in the structure of the heart. Tricuspid valve stenosis can lead to chest retraction, which the doctor detects by palpation.
However, murmurs can only be detected in acute failure. Less severe symptoms are often ignored. For an accurate diagnosis, instrumental examination using devices is required.
Diagnostics
Currently, the most effective diagnostic method is echocardioscopy with Dopplerography, which allows one to assess the severity of the defect and the degree of its decompensation.
In addition, an ECG and daily ECG monitoring are performed to establish the heart rhythm, as well as phonocardiography to record heart sounds and murmurs. To clarify the type of heart defect, an x-ray is taken.
Do not forget about 4 standard diagnostic methods: inspection, palpation, percussion, auscultation. In particular, with mitral stenosis, you can listen to a three-part tone - the rhythm of a quail.
Treatment
Drug treatment of tricuspid stenosis
Your doctor may recommend regular monitoring of your tricuspid valve disease, with or without predominant stenosis. Clinic visits during which medical examinations are performed may occur once a year or more frequently, depending on your doctor's orders. Diagnostic tests are repeated at certain intervals.
Medicines may also be prescribed by a doctor to relieve symptoms of the disease. Medicines include drugs to relieve symptoms of heart failure or control irregular heart rhythms.
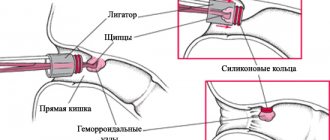
Surgical treatment of tricuspid valve insufficiency
If the pathology is very serious, surgical treatment or valve replacement is prescribed. In cases of tricuspid regurgitation, primary tricuspid valve disease, or disease associated with other valve pathologies, a procedure called ring valve annuloplasty is preferred.
If the valve cannot be restored, it is completely replaced with a biological or mechanical prosthesis.
Treatment[ | ]
Treatment of congenital heart disease can be fundamentally divided into surgical (in most cases it is the only radical treatment) and therapeutic (usually auxiliary).
Surgery. Depends on the phase of the vice.
- In the first phase - an operation for emergency indications (if the ICC is enriched - artificial stenosis of the pulmonary artery according to Müller-Albert, if the ICC is depleted - artificial ductus botalus). The expediency of these operations, however, is an ambiguous and highly individual issue.
- In the second phase - surgery as planned (specific for a specific defect). The timing of implementation is a controversial issue and is constantly being revised (in the literature, the timing varies from intrauterine surgery to puberty, but is still more inclined towards early surgery).
- In the third phase, surgery is not indicated.
Therapeutic treatment[ | ]
It is rarely shown as radical. A classic example is PDA, when the administration of indomethacin according to the appropriate regimen leads to obliteration of the ductus botalus.
As symptomatic therapy includes:
- Acute left ventricular heart failure (cardiac asthma, pulmonary edema).
- Dyspnea-cyanotic attacks (OCA).
- Chronic heart failure.
- Arrhythmia.
- Myocardial ischemia.
Symptoms of tricuspid stenosis
Since isolated tricuspid stenosis occurs infrequently, and is usually combined with mitral or mitral-aortic disease, symptoms of other defects (shortness of breath, hemoptysis, dizziness, tendency to faint) come to the fore. In heart tumors, manifestations of the malignant process predominate, due to the localization of the primary tumor or its metastases.
The intrinsic signs of tricuspid insufficiency are general weakness and fatigue, tachycardia, heaviness or pain in the epigastrium and right hypochondrium. Dyspeptic disorders are of concern: nausea, belching, flatulence. When examining patients with tricuspid stenosis, cyanosis is detected in combination with jaundice of the skin, edema of the lower extremities, ascites, congestive swelling and pulsation of the neck veins and liver. Against the background of increased venous pressure, arterial hypotension is noted. With severe tricuspid stenosis, liver cirrhosis, exhaustion, anasarca, and splenomegaly develop. In the stage of decompensation of tricuspid stenosis, phlebothrombosis and thromboembolism of the pulmonary arteries often occur.
As in the case of tricuspid insufficiency, pregnancy in a woman with tricuspid stenosis can be complicated by the development of gestosis, fetoplacental insufficiency and premature birth.
Prognosis and prevention of tricuspid stenosis
The natural history of tricuspid stenosis is extremely unfavorable: the average life expectancy of patients is 23 years. The outcome of the disease is influenced by the condition of the mitral and aortic valves, the contractile function of the myocardium, and the activity of the rheumatic process. Postoperative long-term results are very encouraging: 5-year survival rate after valve replacement is 65%, after annuloplasty - 70.4%.
To prevent tricuspid stenosis, the most effective is targeted prevention of rheumatism and infective endocarditis, which should be carried out under the guidance of a rheumatologist and cardiologist. Great importance is attached to the treatment of foci of chronic infection (chronic tonsillitis, dental caries), and hardening.