Platelets
Platelets are the smallest blood cells.
Their main task is to participate in blood clotting, or more precisely, in the formation of a blood clot, which, like a plug, closes the lumen in the vessel wall and prevents the outflow of blood from the body. The formation of platelets - cells, in combination with other factors that ensure blood clotting, is carried out through megakaryocytopoiesis. The first in this series of hematopoiesis are megakaryoblasts, then megakaryocytes, as a result of the detachment of the cytoplasm of which platelets arise.
The origin of platelets from the cytoplasm of megakaryocytes has been proven by immunological and radioisotope methods and confirmed by both direct observation and time-lapse filming.
Factors controlling megakaryocytopoiesis. The formation of precursor cells for megakaryocytopoiesis is carried out according to the principle common to all granulocytes: an excess of platelets in the bloodstream inhibits megakaryocytopoiesis, thrombocytopenia stimulates it (through platelet keylon).
The regulation of platelet production is carried out by thrombopoietin, the molecular weight of which is 80-90 kDa, and the half-life is 20-40 hours. Receptors for thrombopoietin (c-mpl) are detected on platelets, megakaryocytes and a small number of precursor cells.
The fastest way to increase the number of platelets is final endomitosis of megakaryocytes. The patterns of aging of megakaryocytes, as found experimentally, are that it accelerates with enhanced regeneration, for example, after blood loss, and slows down under conditions of deficiency of vitamins, food ingredients or when exposed to antiplatelet antibodies, chemotherapy. The restored bone marrow reserve of megakaryocytes, according to the feedback principle, slows down the rate of cell proliferation in the sprout.
The cytoplasm of mature megakaryocytes always contains fully mature platelets, which, however, lack a wide, loose layer of the outer membrane (glycocalyx). It is the unique ability of nuclear division in the morphologically mature cytoplasm of the megakaryocyte, i.e. final endomitosis, that completes the formation of the glycocalyx and makes platelets complete.
In addition to platelets, the protein fibrin is involved in the formation of a blood clot. Its threads, precipitating, form a dense network in the damaged vessel wall, which blocks the path of blood. In addition to platelets, erythrocytes and leukocytes are also driven into this network. A clot forms and the bleeding stops. After the restoration of damaged tissue begins, the blood clot gradually dissolves and fibrin dissolves (fibrinolysis).
The process of blood clotting to a mild degree occurs constantly even in intact vessels. This is necessary for the formation of a fibrin film on the inner surface of the vessels, which prevents the release of red blood cells and blood plasma proteins from the vessels. To prevent the film from filling the entire lumen of the vessel, blood clotting is constantly accompanied by fibrinolysis.
The activity and number of platelets in the blood greatly depend on the state of health. Both a reduced quantity and an increased quantity are bad.
In the first case, the blood clotting process is disrupted. This happens, for example, with aplastic anemia.
Excess platelets increase the risk of heart attack and stroke, and can signal certain infectious diseases, such as mosquito-borne dengue fever.
Therefore, it is very important to have regular blood tests to monitor your platelets.
share on social media networks
Increased platelets and increased lymphocytes
Content
Quite often situations arise when a blood test shows that platelets are increased and lymphocytes are increased. In order to understand what this means, it is worth knowing what these blood cells are, their purpose and the reasons for the increase. A blood test is the first stage of diagnostic procedures, which is carried out during a medical examination of a patient. When assessing the finished results, medical workers have to decipher indicators that reflect an increase in the number of lymphocytes and platelets. An increased level of lymphocytes is called lymphocytosis, and platelets are called thrombocytosis, and only a doctor should determine what further diagnostic methods should be applied to the patient. So, why does it happen that lymphocytes and platelets are elevated in an adult?
What are lymphocytes and their norm
Lymphocytes are the main cells of the immune system, which are a type of white blood cell of the agranulocyte group and are responsible for the production of antibodies by the body. We can say that lymphocytes are the most important component of cellular immunity.
A blood test allows you to determine the number of lymphocytes in the human body without detailed characteristics of the T- and B-cell units.
The following indicators are the norm for lymphocytes:
- absolute value (this measurement represents the number of lymphocytes found in a liter of blood) – 1-4.5 g/l;
- relative value (the number of lymphocytes in relation to the number of leukocytes in the blood stream, expressed as a percentage) – 20-40%.
The decoding and evaluation of the finished results can be carried out using both values - this makes it possible to carry out a more accurate diagnosis.
In the presence of pathological inflammation, as a result of which the patient will require a more thorough diagnosis, a full study of the composition of lymphocytes at the cellular level is carried out, which can give the following options for an increased level of these cells that make up the human immune system:
- Absolute lymphocytosis is one of the laboratory situations during which increased levels of leukocytes are observed, caused by an increase in the number of lymphocytes in the body.
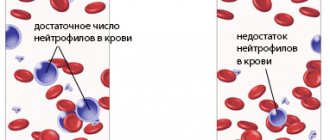
- Relative lymphocytosis - the patient has a high level of lymphocytes, while leukocytes are normal. In this case, the level of lymphocytes turns out to be increased due to a decrease in neutrophil leukocytes, which are part of the leukocyte formula known to everyone.
You must always remember that lymphocytes and leukocytes are two components of the immune system, which is responsible for protecting the body from the effects of harmful bacteria.
If during a blood test changes are detected based on the development of relative lymphocytosis in a person, it is imperative to determine the level of these elements in absolute values.
What causes an increase in lymphocytes
There are a variety of reasons for an increase in lymphocytes in the body.
These may be blood diseases. As one of the elements of the blood flow, lymphocytes reflect the state and functionality of hematopoiesis, which constantly occurs in the body.
For example, increased levels of leukocytes and lymphocytes occur with the development of diseases associated with disorders of the lymphatic system, as well as with worsening bone marrow function.
Changes in the leukocyte formula also appear in the following cases:
- acute and chronic form of lymphoblastic leukemia;
- radiation sickness;
- the development of malignant neoplasms occurring in the bone marrow;
- multiple myeloma;
- lymphoma or lymphosarcoma.
In this case, the diagnosis of diseases makes it clear about the presence of a particular disease.
Viral infections. As mentioned above, lymphocytes are immune cells that are responsible for protecting the body from various viruses. If an analysis reveals an increase in them in the peripheral blood, this often becomes evidence of infection of the body with various viruses, which occurs either during their active reproduction or during the formation of the immune system. And if in the first case the development of lymphocytosis is mainly explained by an increase in the level of T cells, then in the second case it is an increase in B cells.
These changes can be caused by:
- the virus that causes rubella, chickenpox, or measles;
- respiratory viruses that can cause influenza, adenovirus, and so on;
- hepatitis viruses (A, B, C, etc.).
Viral infections are treated according to the regimen prescribed by the doctor.
Autoimmune diseases. Almost all diseases that are characterized by the destruction of tissue in the body by cells of the immune system are certainly accompanied by increased activity of lymphocytes. In a blood test, which is an important diagnostic method, this looks like an increase in the absolute or relative value of lymphocytes in comparison with their norm in the body.
The main diseases that are accompanied by lymphocytosis are:
- asthma;
- rheumatoid arthritis;
- lupus;
- chronic skin diseases (eczema, psoriasis).
They should be treated as soon as they are detected, otherwise they can lead to complications.
What are platelets and the reasons for their increase
Platelets or platelets are colorless blood cells that have a spherical shape. The size of platelets is 3 times smaller than that of red blood cells - on average it varies from 2 to 4 microns. These blood cells are produced in the bone marrow.
Platelets remain in the bloodstream for about 10 days, after which they are actively absorbed by the spleen and liver - while the bone marrow produces new cells without stopping.
Main functions of platelets:
- protection of vessel walls from ruptures, thinning and damage;
- prevention of blood loss due to the formation of a blood clot (thrombus) closing the wound;
- control of blood clotting.
Primary thrombocytosis can attack the human body when it develops diseases such as chronic myeloid leukemia and erythremia. It is worth knowing that with the development of these pathologies in the blood, both the level of platelets and leukocytes increases.
The development of secondary thrombocytosis can be explained by the following factors.
Inflammatory processes explain the production of interleukins that make up the human immune system. All this stimulates the development and utilization of platelets.
The main inflammatory processes that cause thrombocytosis are:
- chronic liver diseases;
- sarcoidosis;
- rheumatoid arthritis;
- rheumatic fever;
- collegiate disease.
Immediately after their detection and diagnosis, the doctor prescribes appropriate treatment that quickly restores a person’s health.
Deterioration of blood microcirculation occurs with the development of infection, which most often occurs under the influence of pathogenic bacteria, sometimes viruses or fungi.
In this case, diseases such as:
- candidiasis;
- hepatitis;
- pneumonia;
- meningitis.
In this case, the person’s treatment will be aimed at restoring microcirculation and normalizing the functionality of the body.
Iron deficiency. The full mechanism of iron deficiency on the increase in platelet levels has not yet been studied. To check the connection between iron deficiency and an increase in the amount of these elements, a test is performed to determine a positive protein in the body, which is responsible for storing iron in it, as well as its release through cells.
With increased platelet growth, the number of these cells increases steadily. The main danger of this condition is that the patient has an increased risk of thrombosis - blockage of blood vessels.
Rate this article:
We recommend reading:
boleznikrovi.com
Red blood cells, white blood cells and platelets
Red blood cells
- these are red blood cells that perform a respiratory function in the body: transport oxygen and carbon dioxide through the blood, and also regulate the content of amino acids and polypeptides in the plasma (
B. I. Zbarsky
). 1 mm3 of blood contains 4-5.5 million red blood cells. They are a biconcave disk surrounded by a membrane. The place of formation of red blood cells is mainly the bone marrow, as well as the spleen and liver. The lifespan of red blood cells in circulating blood is about 100 days. The process of maturation of erythrocytes is a complex and relatively long process, when erythrocytes are formed from nucleated cells through the stages of normoblasts and reticulocytes.
Of the red blood cell proteins, the most important is hemoglobin, the content of which can reach up to 41%. The entire number of human red blood cells contains approximately 800 g of hemoglobin. In whole blood, the amount of hemoglobin is 13-18 g%. Currently, various forms of hemoglobins have been discovered, differing in the amino acid composition of the globin - its protein part. In human embryos at 7-12 weeks, primitive hemoglobin (HbP) was detected, which is subsequently replaced by fetal hemoglobin (HbF). The latter makes up 70-90% of all hemoglobin in children. In an adult, the bulk of hemoglobin is hemoglobin A1 (HbA1).
In some diseases (sickle cell anemia, thalassemia), pathological forms of hemoglobins, designated C, D, S, etc., are found in the blood of patients. These diseases belong to hereditary pathology, which is based on a violation of the process of globin synthesis.
When the erythrocyte membrane is damaged under the influence of altered osmotic pressure and various toxins, hemoglobin is released into the plasma. This process is called hemolysis. A decrease in hemoglobin in the blood leads to the development of various anemias. A decrease in hemoglobin to 5% leads to death.
In the clinic, determining the amount of hemoglobin in the blood is of great importance. Its concentration in adults varies between 13-18 g%, in a child after birth it is 19.5 g%, by the second month it decreases to 11.5 g% and gradually reaches the level of adults by 12 years.
In the clinic, there are various methods for determining hemoglobin, of which the most common is the Sali method, when, after adding hydrochloric acid to the blood, hemoglobin is converted into brown hydrochloric acid hematin and the hemoglobin concentration is determined by comparing its color with the color of a standard solution. Another indicator used to analyze red blood cells is the color indicator. The latter allows you to get an idea of the hemoglobin content in red blood cells, on which the clinical classification of anemia is based. The erythrocyte sedimentation reaction (ERS) is one of the most important and widespread laboratory research methods. Its essence lies in the fact that blood, stabilized by some substances, left in a vertical vessel, after some time becomes clear due to the sedimentation of red blood cells and other blood cells. It has been established that the erythrocyte sedimentation rate in healthy people is approximately the same and amounts to 5-10 mm per hour. With a decrease in the A/G indicator (acute stage of rheumatism, malignant neoplasms, kidney diseases, anemia), ROE is accelerated. In heart and liver diseases, ESR is slowed down
In clinical practice, importance is also attached to methods for studying hemostasis, blood coagulation, and capillary fragility.
Leukocytes.
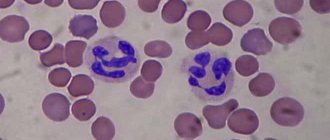
1 mm3 of blood contains 5-6 thousand white blood cells. They are divided into a number of forms depending on the shape of the kernel and the method of coloring.
Leukocytes participate in the processes of phagocytosis - the capture and digestion of foreign bodies and bacteria. In places of inflammation there are always a lot of leukocytes, which in their mass form pus.
Why do they take a smear?
A flora smear is a diagnostic method that involves studying material collected from the surface of the mucosa under a microscope. The analysis is done for everyone: both men and women.
Men undergo a smear to detect urological diseases. Material for research is taken from the urethra. In women, a smear can be taken from the urethra and vagina.
The study of the microflora and cytological composition of the biomaterial obtained by scraping or imprinting the mucous membrane makes it possible to diagnose infectious, including sexually transmitted and hormonal diseases, and to detect cancer, precancerous and background conditions.
A smear is taken for both therapeutic and preventive purposes. When undergoing a course of treatment for genitourinary diseases, a smear is usually taken before and after treatment.
Taking a smear is a completely painless procedure that helps to correctly assess the condition of a woman’s reproductive system.
The biomaterial is applied to a glass slide and a thin smear is made - a microslide suitable for study under a microscope.
The material for research is selected with a glass pipette or a sharp spoon, and then applied to the edge of a glass slide and smeared with the edge of a coverslip. The smear is lightly dried in air or in a burner flame and stained.
There are two ways to stain a vaginal smear. Monochrome is used in cytological analysis, polychrome is used for cytological and hormonal studies.
After all the manipulations performed, the microspecimen is considered ready for examination under a microscope.
Violation of the technology for preparing a smear will lead to unreliable results, but this situation is rare, since a vaginal smear is a standard test that does not require special qualifications from a health worker.
READ Structure and functions of red blood cells
Video:
A woman should come prepared for a smear test. For the analysis to be reliable, you need to abstain from sexual intercourse for two days, not douche, and not be treated with vaginal suppositories, ointments and creams.
It is recommended to urinate no earlier than two or three hours before visiting the gynecological chair. It is advisable to take the test on the 5th day of the cycle, as soon as your period ends.
Red blood cells
Red blood cells and white blood cells perform a very important function in the human body; for example, the supply of oxygen from the lungs to the rest of the body cells directly depends on red blood cells. This happens in the following way: red blood cells squeeze through the capillary vessels of the lungs, right up to the alveoli, but the walls of the vessels are very narrow and the red blood cells cannot pass completely; hemoglobin helps them in this. These cells contain iron, and it can reach the lung vesicles, which contain oxygen. Hemoglobin forms an unstable compound oxyhemoglobin with it. Next, the hemoglobin cell changes its color and the same happens with the blood, which becomes saturated with oxygen - from dark it becomes bright scarlet. Red blood cells carry oxygen throughout the body and cells use it to burn hydrogen obtained with food. The spent carbon dioxide is sent to the lungs, from where it is expelled out with human exhalation.
It is very difficult to provide oxygen to 10 trillion cells, so there must be a lot of red blood cells, about 25 trillion. Scientists theorists claim that if you pull red blood cells out of the body and put them in a chain, you can wrap them around the globe five times, because their length will be approximately 200,000 km. Every day, more than 200 billion red blood cells are produced in the bone marrow to maintain full human vitality. The lifespan of red blood cells is short; they, as a rule, self-destruct after 4 months in the spleen.
Red blood cells and leukocytes in the blood have certain standards; often the indicators may differ for different return categories. The number of red blood cells for women in normal condition is approximately 3.4-5.1 × 1012/l, for men 4.1-5.7 × 1012/l, in childhood 4-6.6 × 1012/l. Any deviations from these indicators may indicate disturbances in the functioning of the bone marrow and hematopoietic processes. A high level of red blood cells in the blood may indicate diseases such as:
- inflammation of the bronchi;
- laryngitis;
- pneumonia;
- heart muscle defects;
- erythremia;
- Aerz's disease;
- diphtheria;
- whooping cough;
- oncological formations in the kidneys, liver and pituitary gland.
It should be noted that increased red and white blood cells can be observed during a long stay in the mountains, where the production of cells by the bone marrow increases due to increased pressure in the air. Sometimes, a person may even feel an attack of shortness of breath without physical exertion and a lack of air. Red blood cell counts can be affected by dehydration, which is often observed with diarrhea and drinking disorders. Low red blood cells may be due to anemia. If red blood cell counts are low, the doctor can diagnose diseases such as:
- myxedema;
- presence of bleeding in internal organs;
- cirrhosis;
- hemolysis;
- neoplasms in the bone marrow or metastases in it;
- infectious diseases;
- lack of vitamin B and folic acid.
In addition to the above pathological processes, one can also include the period of pregnancy, during which there is a constant decrease in the number of red blood cells. During the process of bearing a child, this is the norm and does not require significant therapeutic correction; proper nutrition and vitamin therapy are sufficient.
Table of normal values and deviations from the norm
This table shows particle standards and possible deviations.
| № | Indicators | Normal for a woman | Normal for a man | Increased rate | Reduced rate |
| 1 | Red blood cells | 3.7-4.7 x 1 µl | 4-5.1 x 1 µl | Erythrocytosis. Reasons: dehydration, heart disease, lack of oxygen in the mountains. | Erythropenia. Causes: anemia, blood loss. |
| 2 | Platelets | 180-320 x 1 µl | 180-320 x 1 µl | Thrombocytosis. Cause: blockage of blood vessels. | Thrombocytopenia. Reason: increased bleeding. |
| 3 | Leukocytes | 4-9 x 1 µl | 4-9 x 1 µl | Leukocytosis. Causes: leukemia, heart attack, blood loss. | Leukopenia. Cause: viral infection. |
The number of red blood cells, leukocytes and platelets are interrelated. Despite the fact that the functions of each cell are different, each of them, individually and in interaction, pursues one goal - to ensure human life and protect the body.
Characteristics of blood cells (erythrocytes, leukocytes, platelets) and their role in the body
Erythrocytes are red blood cells containing the respiratory pigment hemoglobin. These anucleate cells are formed in the red bone marrow and destroyed in the spleen. Depending on their size, they are divided into normocytes, microcytes and macrocytes. Approximately 85% of all cells have a biconcave disk or lens shape with a diameter of 7.2–7.5 μm. This structure is due to the presence of the spectrin protein in the cytoskeleton and the optimal ratio of cholesterol and lecithin. Thanks to this form, the red blood cell is able to transport respiratory gases - oxygen and carbon dioxide.
1. respiratory (associated with the presence of hemoglobin and potassium bicarbonate, due to which the transfer of respiratory gases occurs);
2. nutritional (associated with the ability of the cell membrane to adsorb amino acids and lipids, which are transported through the bloodstream from the intestines to the tissues);
3. enzymatic (due to the presence on the membrane of carbonic anhydrase, methemoglobin reductase, glutathione reductase, peroxidase, true cholinesterase);
4. protective (carried out as a result of the sedimentation of microbial toxins and antibodies, as well as due to the presence of blood clotting factors and fibrinolysis);
Since red blood cells contain antigens, they are used in immunological reactions to detect antibodies in the blood.
Red blood cells are the most numerous formed elements of blood. Thus, men normally contain 4.5–5.5 × 10 12 /l, and women – 3.7–4.7 × 10 12 /l. However, the number of blood cells is variable (an increase is called erythrocytosis, and a decrease is called erythropenia).
Red blood cells have physiological and physicochemical properties:
1. Plasticity
. Plasticity is largely due to the structure of the cytoskeleton, in which the ratio of phospholipids and cholesterol is very important. This ratio is expressed as a lipolytic coefficient and is normally 0.9. The plasticity of erythrocytes is the ability to undergo reversible deformation when passing through narrow capillaries and micropores. With a decrease in the amount of cholesterol in the membrane, a decrease in the stability of red blood cells is observed.
2. Osmotic resistance
(red blood cells are able to withstand destructive osmotic effects).
3. Availability of creative connections
, thanks to which erythrocytes are ideal carriers, transport various substances and carry out intercellular interaction.
4. Ability to settle
. The ability to settle is due to the specific gravity of the cells, which is higher than all blood plasma. Normally, it is low and is associated with the presence of proteins in the albumin fraction, which are capable of retaining the hydration membrane of red blood cells. Globulins are lyophobic colloids that prevent the formation of a hydration shell. The ratio of albumin and globulin fractions of blood (protein coefficient) determines the erythrocyte sedimentation rate. Normally it is 1.5–1.7.
5. Aggregation.
Aggregation is observed with a decrease in blood flow velocity and an increase in viscosity. With rapid aggregation, “coin columns” are formed - false aggregates that disintegrate into full-fledged cells with a preserved membrane and intracellular structure. With prolonged disruption of blood flow, true aggregates appear, causing the formation of a microthrombus.
6. Destruction
. Destruction (destruction of red blood cells) occurs after 120 days as a result of physiological aging. It is characterized by:
· gradual decrease in lipid and water content in the membrane;
· increased yield of K and Na ions;
· predominance of metabolic changes;
· deterioration in the ability to restore methemoglobin to hemoglobin;
· decreased osmotic resistance, leading to hemolysis.
Aging red blood cells, due to a decrease in the ability to deform, get stuck in the millipore filters of the spleen, where they are absorbed by phagocytes. About 10% of cells are destroyed in the vascular bed.
Leukocytes are nucleated blood cells whose sizes range from 4 to 20 microns. Their lifespan varies greatly, ranging from 4–5 to 20 days for granulocytes and up to 100 days for lymphocytes. The normal number of leukocytes in men and women is the same and is 4–9 × 10 9 /l. However, the level of cells in the blood is not constant and is subject to daily and seasonal fluctuations in accordance with changes in the intensity of metabolic processes.
Fluctuations in white and red blood cell levels
Depending on the presence of pathological or physiological factors, the concentrations of leukocytes and erythrocytes in the blood can fluctuate significantly, both upward and downward.
Red blood cells
The relative norms for the content of erythrocytes in the blood are the range of values from 3.8 to 5.2 * 1012 degrees of components per 1 liter of blood. A slight increase in their number may be associated with taking diuretics, excessive diarrhea, or the consequences of a burn. An excess concentration of red blood cells is called erythrocytosis and can form in the following cases:
- A variety of neoplasms, both benign and malignant;
- Taking loading doses of corticosteroids;
- Cushing's syndrome at any stage;
- Polycythemia vera;
- Long-term systemic treatment with steroids;
- Hydrocele of the renal pelvis.
A decrease in the concentration of red blood cells in the blood relative to the norm can be caused by the following circumstances:
- Late stage pregnancy;
- Various forms of anemia;
- Moderate or severe blood loss;
- Systemic infusion therapy with regular injection of large amounts of fluid into the bloodstream;
- Various diseases and pathologies associated with accelerated cell destruction, as well as a decrease in the intensity of their formation in the bone marrow.
Leukocytes
The relative norms for the content of leukocytes in the blood are the range from 4 to 8 * 109 formed elements per 1 liter of biological fluid. The concentration of leukocytes above normal is called leukocytosis and can be caused by the following circumstances (you will learn more about the increased level of leukocytes in the blood in this article):
- Pregnancy at the end of the last trimester of fetal development, as well as intensive breastfeeding;
- Impact physical activity on a regular basis;
- Myocardial infarction of any stage;
- A variety of soft tissue injuries, purulent processes and sepsis;
- Acute inflammatory diseases of an infectious nature, in particular viral, fungal, bacterial lesions;
- Certain autoimmune processes of a systemic nature.
A leukocyte concentration below normal (leukopenia) may indicate the following reasons:
- Viral diseases of wide etiology;
- Aplasia and partial destruction of bone marrow;
- Variations of typhus;
- Broad spectrum collagenoses;
- Acute leukemia , including radiation sickness or other exposure to ionizing radiation;
- Myelofibrosis and various myelodysplastic syndromes;
- Metastasis to the bone marrow;
- Hypersplenism, both secondary and primary in nature;
- Pernicious anemia and plasmacytoma;
- External influences when using medications and a number of substances.
Formed elements of blood
The formed elements of blood provide its versatility
Formed elements provide the versatility of blood functions. They create the body’s defense against pathogenic microbes, transport oxygen and nutrients, cleanse the circulatory system and remove waste products, restore damaged tissues and prevent blood loss, stopping bleeding.
All elements originate in the bone marrow from a single stem cell. As cells develop, they differentiate and transform into one of the types of formed elements: red blood cells, platelets and leukocytes. In total, they make up 40 - 48% of blood volume, the remaining 52 - 60% are plasma. The ratio of the total number of formed elements is called hematocrit. Sometimes hematocrit is calculated based on the number of red blood cells only, since they are the main cellular elements of blood.
Which blood cells do not have a nucleus - Treating the heart
Leukocytes do not have a nucleus, since the main function is the transfer of oxygen, the nucleus takes up extra space. Therefore, in the process of evolution it disappeared
If the answer for the subject Biology is missing or it turns out to be incorrect, then try using the search for other answers in the entire site database.
Blood cells
, or
blood cells
, are cells that are part of the blood and are formed in the red bone marrow during hematopoiesis. There are three main types of blood cells: erythrocytes (red blood cells), leukocytes (white blood cells), and platelets (blood platelets).
The portion of blood volume per cell is called hematocrit. In women, its normal value is 0.37-0.47, in men - 0.4-0.54. More than 99% of the hematocrit comes from red blood cells.
Blood cells perform a variety of functions: they carry oxygen and carbon dioxide (red blood cells), ensure the functioning of the immune system (leukocytes) and blood clotting (platelets) [1].
Sometimes red blood cells, platelets and leukocytes are collectively called blood cells
due to the fact that platelets are fragments of the cytoplasm of megakaryocytes, do not have their own nucleus [2] and are not considered cells by some scientists [3].
History of the study [edit | edit code ]
In 1658, the Dutch naturalist Jan Swammerdam first saw red blood cells through a microscope, and in 1695, Antonie van Leeuwenhoek sketched them, calling them “red corpuscles.” After this, new types of blood cells were not studied, and only in 1842 the French physician Alfred Francois Donnet discovered platelets.
The following year, his compatriot and colleague Gabriel Andral described leukocytes simultaneously and independently with the English physician William Addison. As a result of these discoveries, a new field of medicine was born - hematology.
Further progress in the study of blood cells began in 1879, when Paul Ehrlich published his method of differential staining of blood cells [4].
Red blood cells [edit | edit code ]
Mature erythrocytes (normocytes) are anucleate cells in the form of a biconcave disk with a diameter of 7-8 microns.
Red blood cells are formed in the red bone marrow, from where they enter the blood in an immature form (in the form of so-called reticulocytes) and reach final differentiation 1-2 days after entering the bloodstream. The lifespan of an erythrocyte is 100-120 days.
Used and damaged red blood cells are phagocytosed by macrophages of the spleen, liver and bone marrow. The formation of red blood cells (erythropoiesis) is stimulated by erythropoietin, which is formed in the kidneys during hypoxia [5].
The most important function of red blood cells is respiratory. They carry oxygen from the alveoli of the lungs to the tissues and carbon dioxide from the tissues to the lungs. The biconcave shape of the red blood cell provides the greatest ratio of surface area to volume, which ensures its maximum gas exchange with blood plasma.
The iron-containing protein hemoglobin fills red blood cells and carries all the oxygen and about 20% of the carbon dioxide (the remaining 80% is transported as the bicarbonate ion). In addition, red blood cells participate in blood clotting and adsorb toxic substances on their surface. They transport a variety of enzymes and vitamins, amino acids and a number of biologically active substances.
Finally, on the surface of red blood cells there are antigens - group characteristics of blood [5].
Leukocytes [edit | edit code ]
Leukocytes are nuclear spherical cells. Depending on the type of granules in the cytoplasm, they are divided into granulocytes (neutrophils, eosinophils, basophils) and agranulocytes (lymphocytes and monocytes). A distinctive feature of leukocytes is their mobility, which is ensured by the contractile proteins actin and myosin.
They can even leave blood vessels, penetrating between endothelial cells. The main function of leukocytes is protective.
They phagocytose microorganisms, foreign particles, tissue breakdown products, synthesize and inactivate various biologically active substances, mediate reactions of humoral [en] * and cellular immunity [6].
The most numerous type of leukocytes are neutrophils. After leaving the bone marrow, they circulate in the blood for only a few hours, after which they settle in various tissues. Their main function is phagocytosis of tissue debris and opsonized microorganisms. Thus, neutrophils, along with macrophages, provide the primary nonspecific immune response [7] .
Eosinophils remain in the bone marrow for several days after formation, then enter the bloodstream for several hours and then migrate to tissues in contact with the external environment (mucous membranes of the respiratory and genitourinary tracts, as well as the intestines). Eosinophils are capable of phagocytosis and are involved in allergic, inflammatory and antiparasitic reactions. They also secrete histaminases, which inactivate histamine and block mast cell degranulation [7].
Basophils are a very small type of leukocytes (no more than 0-1% of the total number of leukocytes in the blood), their granules contain histamine and heparin. They exit the bloodstream into tissues, where they participate in allergic reactions, releasing histamine and other vasoactive [en] substances [7].
Monocytes are the largest white blood cells. After several days of circulation in the bloodstream, they enter the tissues and turn into macrophages. Macrophages are phagocytic cells and are found in all tissues and organs.
They phagocytose denatured proteins, aged red blood cells, cell debris and extracellular matrix from the blood.
They also absorb opsonized bacteria in tissues and, after activation, secrete a variety of enzymes, transport proteins, interleukins, growth factors, thromboxanes, as well as lysozyme and endogenous pyrogens [8].
Lymphocytes are divided into T lymphocytes and B lymphocytes depending on the site of their maturation (thymus or red bone marrow, respectively). They constantly enter the bloodstream with lymph from the lymph nodes. Lymphocytes provide specific immunity. B lymphocytes secrete antibodies.
T lymphocytes are divided into killer T cells, which provide the cellular immune response, T helper cells, which support the proliferation and differentiation of B lymphocytes, and T regulatory cells, which suppress the T cell immune response after the threat has been eliminated.
There is also a special group of lymphocytes - natural killer cells, which destroy cancer cells, cells infected with viruses, and foreign cells [9].
Platelets [edit | edit code ]
Platelets circulating in the blood (two thirds of all platelets, the rest accumulate in the spleen) are involved in blood clotting and restoration of the integrity of the vessel wall after damage.
They adhere to each other and to the walls of blood vessels, and also secrete growth factors that stimulate wound healing.
Platelets are formed in the bone marrow from megakaryocytes, which at a certain point break up into many blood platelets [10].
Education [edit | edit code ]
All blood cells come from hematopoietic stem cells found in the bone marrow. They first separate into populations of lymphoid cell precursors and myeloid cells.
Lymphoid cell precursors give rise to natural killer cells, T lymphocytes, and B lymphocytes. Myeloid cell precursors develop within a population of megakaryocytes (platelet precursors), red blood cell precursors, mast cells, and myeloblasts.
Myeloblasts give rise to basophils, neutrophils, eosinophils and monocytes [11].
The formation of red blood cells (erythropoiesis) is stimulated by erythropoietins when there is a lack of oxygen in the tissues. Leukocytes in the blood are regulated by thymus hormones. Thrombopoietin is synthesized in the liver, which stimulates the formation of megakaryocytes. Bone marrow stromal cells and T lymphocytes produce interleukin 3, which acts on hematopoietic stem cells [12].
Establish a correspondence between the trait and the type of blood cell for which it is characteristic: for each element of the first column, select the corresponding element from the second column.
| SIGN | BLOOD CELL TYPE |
A) do not have a constant body shape
B) they contain hemoglobin
B) transport oxygen from the respiratory organs to all cells of the body
D) provide immunity
D) in a mature state they have a nucleus
Write down the numbers in your answer, arranging them in the order corresponding to the letters:
Red blood cells: they contain hemoglobin and carry oxygen from the respiratory system to all cells of the body. Leukocytes: do not have a constant body shape, provide immunity, and in a mature state have a nucleus.
Source: //serdce-help.ru/kakie-kletki-krovi-ne-imejut-jadra/
Red blood cells: structure and functions
Red blood cells - erythrocytes
Red blood cells (RBCs) are anucleate, biconcave, round cells. The diameter of a developed cell is about 7 - 8 µm, thickness - 2.2 µm at the edges and 1 µm in the central part. The shape and structure of the cell determine the optimal performance of its functions by red blood cells. The concave shape increases the surface of the red blood cell by 1.7 times compared to a spherical cell, and also allows it to move through the thinnest capillaries - penetrating into narrow vessels, red blood cells are able to stretch and twist. The nucleus is lost as the cell matures, making room for hemoglobin molecules.
Red blood cells move smoothly along the bloodstream, lining up in the form of columns, the ends of which are connected to each other, forming rings, which facilitates the movement of blood. Each cell contains about 300 million hemoglobin molecules, which reversibly bind to oxygen and then distribute it to the tissues of various organs. Hemoglobin is a complex protein containing 574 amino acids and consisting of 4 subunits. Each of them includes heme, an iron complex that provides the red color of the cell, and the collection of red blood cells gives the red color to the blood.
The main function of red blood cells is to transport oxygen and remove carbon dioxide from tissues. A decrease in the number of blood cells, changes in their shape and flexibility due to various diseases lead to a lack of hemoglobin and oxygen starvation of all organs. Red blood cells take part in immune reactions and maintaining acid-base balance, and transport nutrients. Also, these cells carry about 400 antigens on their surface; antigens of blood group systems are of primary importance, that is, antigens of blood groups II, III, IX and the Rh factor.
leukocytes or red blood cells do not have a constant shape
1. The ability of cells to rapidly multiply is characteristic of tissue: A) muscle B) nervous C) connective D) epithelial 2. The abdominal muscles include A) abdominal muscles B) triceps C) biceps D) deltoid 3. Human vocal cords are located in A) larynx B) nasopharynx C) trachea D) oral cavity 4.
The systemic circulation begins from A) the right atrium B) the right ventricle C) the left atrium D) the left ventricle 5.
The human autonomic nervous system is involved in A) the implementation of voluntary movements B) the perception of visual, taste and auditory stimuli C) the regulation of metabolism and the functioning of internal organs D) the formation of speech sounds 6.
Arteries are vessels through which blood moves: A) to the heart B) from the heart C) with maximum speed D) with maximum pressure 7. Proteins are digested A) in the mouth B) in the stomach and duodenum C) only in the stomach D) only in the duodenum 8. Organs performing the excretory function: A) lungs B) muscles C) kidneys D) liver 9.
The central nervous system includes: A) nerves B) brain C) nerve ganglia D) nerve ganglia 10. The visual zone is located in the lobe: A) frontal B) parietal C) occipital D) temporal 11. Auditory receptors are located in A) middle ear B) auditory canal C) cochlea of the inner ear D) semicircular canals of the inner ear 12.
The function of red bone marrow is A) hematopoiesis B) support C) protection D) transport 13. Diseases of the organ of vision include A) dwarfism B) myopia C) gigantism D) acromegaly 14. Epithelial tissue consists of A) cells with short and long processes B) long cells with contractile protein and one or more nuclei C) cells tightly adjacent to each other
D) cells with a significant amount of intercellular substance
Part B. C 1. Establish a correspondence between the characteristics of blood cells and their belonging to a certain group. Characteristics Group of cells A) do not have a constant shape 1) red blood cells B) do not contain a nucleus 2) leukocytes C) contain hemoglobin A B C D E
E
D) have the shape of a biconcave disk D) are capable of active movement
E) capable of phagocytosis
B 2. Establish the sequence in which light rays pass through the structures of the optical system of the human eye: A) vitreous body B) pupil C) cornea D) lens
D) retina
C 1.What is the barrier function of the liver?
C 2. Why does the heart work all its life without getting tired?
B 2. Establish the sequence in which light rays pass through the structures of the optical system of the human eye: C) cornea B) pupil D) lens A) vitreous body
D) retina
Source: otvet.mail.ru
- Physiology
- History of physiology
- Physiology methods
Blood is a liquid connective tissue that consists of a liquid part - plasma and cells suspended in it - formed elements: erythrocytes (red blood cells), leukocytes (white blood cells), platelets (blood platelets). In an adult, formed elements of blood make up about 40-48%, and plasma - 52-60%.
Blood is a liquid tissue. It has a red color, which is given to it by erythrocytes (red blood cells). The implementation of the main functions of the blood is ensured by maintaining an optimal plasma volume, a certain level of blood cellular elements (Fig. 1) and various plasma components.
Plasma devoid of fibrinogen is called serum.
Rice. 1.
Formed elements of blood: a - cattle; b - chicken; 1 - red blood cells; 2, b — eosinophilic granulocytes; 3,8,11 - lymphocytes: medium, small, large; 4 - blood platelets; 5.9 - neutrophil granulocytes: segmented (mature), band (young); 7 - basophilic granulocyte; 10 - monocyte; 12 - erythrocyte nucleus; 13 - non-granular leukocytes; 14 - granular leukocytes
All formed elements of blood - red blood cells, white blood cells and platelets - are formed in the red bone marrow.
Despite the fact that all blood cells are descendants of a single hematopoietic cell - fibroblasts, they perform various specific functions, at the same time, their common origin has endowed them with common properties.
Thus, all blood cells, regardless of their specificity, participate in the transport of various substances and perform protective and regulatory functions.
Rice. 2. Blood composition
shaped elements
Red blood cells in men are 4.0-5.0x 10 12 /l, in women 3.9-4.7x 10 12 /l; leukocytes 4.0-9.0x 10 9 /l; platelets 180-320x 10 9 /l.
Erythrocytes, or red blood cells, were first discovered by Malpighi in the blood of a frog (1661), and Leeuwenhoek (1673) showed that they were also present in the blood of humans and mammals.
Erythrocytes are anucleate red blood cells of a biconcave disc shape. Thanks to this shape and elasticity of the cytoskeleton, red blood cells can transport a large number of different substances and penetrate through narrow capillaries.
The red blood cell consists of stroma and a semipermeable membrane.
The main component of red blood cells (up to 95% of the mass) is hemoglobin, which gives the blood its red color and consists of globin protein and iron-containing heme. The main function of hemoglobin and red blood cells is the transport of oxygen (02) and carbon dioxide (CO2).
There are about 25 trillion red blood cells in human blood. If you put all the red blood cells next to each other, you will get a chain about 200 thousand km long, which can encircle the globe along the equator 5 times. If you put all the red blood cells of one person on top of each other, you will get a “column” more than 60 km high.
Erythrocytes have the shape of a biconcave disk; when viewed in a cross section, they resemble dumbbells. This shape not only increases the surface of the cell, but also promotes faster and more uniform diffusion of gases across the cell membrane. If they had the shape of a ball, then the distance from the center of the cell to the surface would increase 3 times, and the total area of erythrocytes would be 20% less.
Red blood cells are highly elastic. They easily pass through capillaries that have half the diameter of the cell itself. The total surface of all red blood cells reaches 3000 m2, which is 1500 times greater than the surface of the human body.
Such ratios of surface and volume contribute to the optimal performance of the main function of red blood cells - the transfer of oxygen from the lungs to the cells of the body.
Unlike other representatives of the chordate type, mammalian erythrocytes are anucleate cells. The loss of the nucleus led to an increase in the amount of the respiratory enzyme - hemoglobin. An aqueous red blood cell contains about 400 million hemoglobin molecules. Deprivation of the nucleus has led to the fact that the erythrocyte itself consumes 200 times less oxygen than its nuclear representatives (erythroblasts and normoblasts).
The blood of men contains on average 5 • 10 12 / l of erythrocytes (5,000,000 in 1 μl), in women - about 4.5 • 10 12 / l of erythrocytes (4,500,000 in 1 μl).
Normally, the number of red blood cells is subject to slight fluctuations. With various diseases, the number of red blood cells may decrease. This condition is called erythropenia and is often accompanied by anemia or anemia. An increase in the number of red blood cells is called erythrocytosis.
Source: https://folkmap.ru/krov/ne-imeyut-postoyannoy-formy-leykotsity-ili-eritrotsity/
Leukocytes: structure and functions
White blood cells - leukocytes
White blood cells (WBC) are a group of cells, each of which has a specialized protective function. Leukocytes contain nuclei; the cells contain hydrolytic enzymes, a protein synthesis system, biologically active compounds and other organelles. Leukocytes have the ability to migrate through the vascular wall, rushing towards foreign particles to capture and destroy them. The destruction of harmful cells is carried out by leukocytes using the process of phagocytosis - absorption and digestion. Leukocytes include 5 groups of protective cells.
1. Basophils (BAS). They make up only 1% of all leukocytes. These cells are round in shape, their diameter is approximately 12 - 15 microns. Basophils contain irregularly shaped granules that contain histamine, heparin, serotonin, prostaglandin and other substances. If necessary, basophilic leukocytes release the contents of their granules, participating in allergic reactions, blocking poisons, protecting blood vessels from the formation of blood clots, and attracting other helper cells to the site of inflammation.
What are leukocytes responsible for?
Leukocytes are cells of the immune system. Their main function is to fight pathogens and foreign proteins that enter the body. They are very diverse in their composition, which allows white blood cells to perform their functions most successfully.
Leukocytes are white blood cells
Their life cycle is more complex than that of red blood cells, and unlike red blood cells, white blood cells originate from two different hematopoietic lineages:
- Myeloblasts and lymphoblasts (IV class of hematopoietic cells) are the ancestors of two different lineages of leukocytes. Special tests of the bone marrow, where progenitor cells are mainly located, can distinguish them from each other. Their appearance in the blood is a sign of malignant lesions of the hematopoietic system.
- Class V leukocytes includes several stages. Descendants of myeloblasts become myelocytes and accumulate granules containing enzymes in the cytoplasm. The composition of the contents of the granules is different; it determines the function of the future leukocyte. Among those cells that a general blood test reveals, this group includes young and band neutrophils. Immature lymphocytes are also found in the blood, but during a general blood test they cannot be distinguished from mature cells.
- Mature leukocytes (class VI) are full-fledged blood cells that pass through two stages of existence - blood and tissue. This class includes myeloid and lymphoid lineages.
Read: Meaning, diagnosis and normal hemoglobin in humans
Myeloid lineage:
- Neutrophils (segmented) - destroy foreign proteins by phagocytosis (eating), are present in the blood, enter the tissue for phagocytosis, and then die.
- Basophils - produce various substances that take part in immune reactions. They are present in the blood for a short time and quickly move to the tissue stage - mast cells.
- Eosinophils are responsible for antiparasitic immunity and also participate in allergic reactions. The tissue stage of life is short-lived.
- Monocytes - have the ability to phagocytose, but unlike neutrophils they are able to capture large objects (virus or bacterial cell), the blood stage is short-lived, they quickly pass into tissues, becoming tissue macrophages, and support local immunity.
Lymphoid sprout:
- Lymphocytes are cells whose main specialization is the production of antibodies. There are two types of them: T- and B-lymphocytes, but a general blood test does not reveal these differences.
The ratio of different types of leukocytes is called the leukocyte formula. It may indicate favorable or unfavorable changes in the human immune system.
More information about the general blood test can be found in the video:
Normal blood levels by age
The table shows the normal values of various types of leukocytes for different age groups, the content is indicated in 10 * 9 / l. The normal white blood cell count in women varies within wider limits. This is due to the characteristics of the menstrual cycle.
| Newborns | Up to 1 year | Up to 2 years | Up to 6 years | Teenagers | Adults | Elderly | |
| Men | 7-32 | 6,0-18,5 | 5,0-17 | 5,0-16,5 | 4,5-13,5 | 4,2-9,0 | 3,9-8,5 |
| Women | 7-32 | 6,0-18,5 | 5,0-17 | 5,0-16,5 | 4,5-11,0 | 3,9-10,4 | 3,7-9,0 |
Read: Advanced blood test - deciphering the main indicators
This is interesting: Pain in the calf muscle on the leg, for several days, when walking, running, after a cramp. Reasons what to do
The normal leukocyte formula in an adult is as follows:
- Young granulocytes – 1-5%
- Mature neutrophils 47-76%
- Eosinophils – 1-5%
- Basophils – up to 1%
- Monocytes – 2-10%
- Lymphocytes – 18-40%
In children, this ratio changes - in newborns the percentage of immature forms of cells is much higher; as the body grows and develops, they are replaced by mature ones and come to the adult ratio.
Platelets: structure and functions
Red blood platelets - erythrocytes
Platelets (PLT) are platelets with a diameter of 2 - 11 microns. These cells do not contain nuclei and are round or oval in shape. But their shape changes when bleeding occurs. As soon as a vessel is damaged, the platelet takes on a spherical shape and releases pseudopods, with the help of which it connects with other platelets and aggregates to the site of damage.
The granules contain the elements necessary for coagulation: coagulation factors, fibrinogen, calcium ions, and growth factor. Some anticoagulants and coagulation factors may be on the surface of the plates.
The main function is to ensure the integrity of the circulatory system through the process of coagulation. When the vessel wall is damaged, collagen is released, to the fibers of which nearby platelets adhere. By releasing the contents of the granules, platelets trigger a chain of reactions that form a blood clot that prevents blood loss.
In addition to participating in the hemostasis system, platelets promote tissue regeneration by releasing growth factors from their granules, which stimulate cell proliferation. Another function is to nourish the endothelium of the blood vessels of the circulatory system.
What is the function of platelets?
Platelets are the smallest flat, anucleate blood cells
Platelets, or blood platelets, are not full-fledged blood cells. Their predecessors are megakaryocytes, large bone marrow cells that accumulate in the cytoplasm proteins necessary for the formation of blood clots.
Fragments of the cytoplasm of giant cells are split off, enter the bloodstream and become platelets.
Their functions are as follows:
- Participation in the formation of blood clots - the formation of a platelet plug, the formation of fibrin threads, the release of vasoconstrictor substances.
- Regulation of metabolic processes in the walls of blood vessels.
- Adhesion (sticking) of some antigens and pathogens.
Platelets are an integral part of a complex blood coagulation system, which is in constant dynamic equilibrium with the anticoagulant system, due to which the blood is maintained in a liquid state, but if the vessel is damaged, a blood clot is formed.
Normal blood levels by age
The platelet count is the most variable indicator in a general blood test. Its norm depends little on age; this indicator is the same for men and women.
An increase in the number of platelets occurs after physical activity, and a decrease occurs when drinking alcohol. The normal value for an adult is 140-450*10*9/l.
Structure and function of red blood cells
Erythrocytes are red blood cells
Red blood cells are the main formed elements of blood. It is to them that she owes her red color. Their main purpose is to transport oxygen and carbon dioxide, but they also perform other important functions. Unlike most other cells, human red blood cells do not have a nucleus.
Red blood cells are formed in the bone marrow, and in their development they go through several stages, during which the structure of the red blood cell and its ability to perform a transport function change.
In the early stages of hematopoiesis, future blood cells are not yet differentiated:
- Erythroblasts (class IV hematopoietic cells) are found in the bone marrow. They have a nucleus and full cytoplasm, but there is an active accumulation of hemoglobin, the main protein of red blood cells. These cells are found in the bone marrow; their presence is not detected in the blood. Their quantity is important in the diagnosis of malignant diseases of the hematopoietic system.
- Reticulocytes, or young red blood cells (class V hematopoietic cells). Unlike erythroblasts, they no longer have a nucleus, but some intracellular structures are partially preserved. Most of the internal space of the cell is occupied by hemoglobin. This is a transitional stage between erythroblasts and mature red blood cells; their life expectancy is short, therefore there are quite a few of them in the bone marrow and blood. Their number is an indicator of the ability of the erythrocyte germ to recover.
- Mature red blood cells (class VI). The final stage of red blood cell development. They completely lack cytoplasm, the entire internal space is occupied by hemoglobin.
The main function of red blood cells is to transport oxygen
The lifespan of a mature red blood cell is 2-3 months, after which it is destroyed. Functions of red blood cells:
- Gas transport - hemoglobin binds oxygen and carbon dioxide, forming unstable compounds.
- Transportation of biologically active substances capable of forming bonds with erythrocyte proteins.
- Determination of group affiliation - red blood cells carry specific proteins that determine the blood group and Rh factor.
- Participation in immune reactions and the formation of blood clots is far from a key role for red blood cells in these processes.
- Regulation of blood pH by binding carbon dioxide.
Leukocytes
We already know that red blood cells carry oxygen and carbon dioxide. We are convinced that they contain substances that determine what blood type a person has. Their relatives, leukocytes - as scientists call white blood cells - bear little resemblance to them. They perform completely different tasks. Wherever pathogens penetrate, many leukocytes immediately gather. They make their way through the capillaries into the tissue affected by the disease and fall on the enemy. The real war begins.
Granulocytes, like other white blood cells, act as protectors of the body. During an infectious disease, their number increases sharply. This figure shows how a granulocyte-phagocyte attacks a rod-shaped bacterium and devours it, that is, it captures the bacterium, absorbs and digests it.
Some white blood cells secrete substances that kill the invading bacteria. Others pounce on fragile guests, absorbing and digesting them. In this fight, the leukocytes themselves die. But their sacrifices are justified: dead leukocytes emit substances that lure their fellows. Other white blood cells rush to the site of the disease. The ranks of fighters protecting the body are closing more and more tightly. Finally, leukocytes surround the site of the disease. They act like an army encircling the enemy. This phenomenon, called phagocytosis, was discovered in 1883 by the Russian scientist Ilya Ilyich Mechnikov, one of the founders of microbiology and immunology. Mechnikov called leukocytes “devouring” - phagocytes. Sometimes, from the remains of destroyed cells, bacteria and leukocytes, a viscous yellow liquid is formed - pus. Later, the leukocytes themselves clear the site of the former “battle.” Now it is clear why the number of white blood cells in the blood of a person infected with bacteria increases sharply. This also happens after a patient has had someone else’s—donor—organ transplanted. Leukocytes perceive foreign tissue as their enemy and try to destroy it at all costs. Therefore, organ transplantation often ends in failure - the body rejects it.
There are several types of white blood cells: granulocytes, lymphocytes, monocytes. They are distinguished by their form and place of formation - in the bone marrow and in the lymph nodes. Leukocytes of different types have one thing in common: they all protect the body.