A healthy person rarely feels how his heart works. The tireless organ reminds itself only in moments of strong excitement or great physical exertion, when its beating becomes stronger than usual. They say about such moments: “your heart is ready to jump out of your chest.”
If you don't take care of your heart, specific diseases can develop. Sometimes the cause of the disease is another disease that gives complications. This is how rheumatic carditis, an inflammatory heart disease caused by streptococcal infection, develops. Rheumatic carditis is often preceded by a common sore throat caused by streptococci. The toxins produced by these bacteria have a negative effect on the heart muscle.
However, rheumatic carditis, according to statistics, causes no more than 2% of mortality from the total number of deaths due to cardiovascular diseases. The main danger is posed by two acute cardiovascular diseases : myocardial infarction and stroke.
General information
Kidney infarction is much less common than other ischemic disorders of the urinary system.
This condition is almost never an isolated disorder, but acts as a complication of other, mainly cardiovascular, pathologies. There are no exact statistics regarding the incidence of the disease, since a certain proportion of patients do not turn to specialists due to the mild severity of symptoms. The disease should be differentiated from uric acid renal infarction in children, which is one of the stages of adaptation of the urinary system to extrauterine existence. Due to the peculiarities of the epidemiology of diseases that can be complicated by renal infarction, the pathology more often occurs in older people suffering from obesity and metabolic disorders.
Kidney infarction
Similarities of diseases
Heart attacks and strokes are becoming “younger” every year. This is facilitated by the presence of common causes of disease development due to the similarity of their pathogenesis. List of main factors:
- arterial hypertension;
- atherosclerotic vascular lesions;
- obesity;
- presence of bad habits;
- difficult physical labor conditions;
- physical inactivity;
- concomitant pathology of the pancreas, heart, kidneys, endocrine glands;
- poor nutrition;
- environmental pollution;
- stress, overwork.
The onset of the disease also has a similar pattern and is difficult to recognize. Patients may experience the following complaints:
- a sharp rise in blood pressure;
- dyspnea;
- numbness of the limbs;
- pain in the heart or head;
- short-term fainting;
- pale skin.
What is the difference between a heart attack and a stroke in the clinical picture, and how to distinguish them?
During a heart attack, pain is located in the region of the heart, radiating to the arm, lower jaw, left shoulder blade, and lasting more than half an hour. A stroke is accompanied by general cerebral (headache, nausea/vomiting, convulsions) and focal symptoms. Depending on the location of the damaged area and the functions it performs, the following symptoms appear:
- paralysis/paresis in areas of the body under their control;
- impaired pronunciation/understanding of speech;
- dysphagia (impaired swallowing);
- dysgraphia (with damage to the center responsible for written speech);
- amnesia;
- unsteadiness of gait;
- the appearance of hallucinations.
Hypertension: high blood pressure and stroke
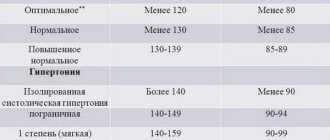
Arterial hypertension is understood as a persistent increase in blood pressure over 140 to 90 mm Hg.
As a rule, elevated blood pressure is not felt by the patient in any way.
Headache, dizziness, and “floaters” flashing before the eyes are not specific to hypertension. However, high blood pressure has an adverse effect on target organs - the brain, heart, blood vessels, kidneys, eyes. With arterial hypertension, the weight of the heart increases, the walls of blood vessels thicken, atherosclerosis develops at an accelerated pace, the vessels of the retina are affected, sclerotic processes develop in the renal tissue with the formation of renal failure.
Against the background of these processes, which occur unnoticed by the patient, life-threatening complications often develop: acute myocardial infarction and cerebral stroke. It’s not for nothing that arterial hypertension is called the “silent killer.”
The main goal of treatment for arterial hypertension is not only to achieve the target level of blood pressure, but also to minimize the overall risk of cardiovascular complications (myocardial infarction, cerebral stroke, heart failure), as well as prolong the life of patients in the long term.
Complications of arterial hypertension.
— influence of weather factors;
- incorrect treatment of hypertension.
3. Acute cerebrovascular accident (cerebral infarction):
- Hemorrhagic stroke is a bleeding into an area of the brain that causes cell damage.
- ischemic stroke - blockage of an artery and death of brain cells due to oxygen deprivation.
- rapid, irregular heartbeat;
- shortness of breath during physical activity and during rest, at rest;
- sharp increase in weakness;
- poor night sleep, awakening due to lack of breathing;
- weight gain due to fluid accumulation;
Myocardial infarction is a disease in which there is a complete cessation of blood supply to one of the arteries supplying the heart, as a result of which the corresponding section of the heart muscle dies. The main classic symptom of myocardial infarction is pressing or burning pain behind the sternum, which can radiate (radiate) under the left shoulder blade, into the left arm or lower jaw.
5. Kidney failure - the kidneys are both a regulator of blood pressure and a victim of its increase. Fatigue, lethargy, swelling, loss of protein in the urine, increased amount of urine are early signs of kidney damage.
Acute cerebrovascular accident
Vascular diseases of the brain are among the most significant medical and social problems, since they make a significant contribution to the structure of morbidity and mortality of the population and are characterized by high rates of temporary and permanent disability. Mortality from cerebrovascular diseases ranks 3rd in the structure of overall mortality.
Arterial hypertension is one of the leading correctable risk factors for acute cerebrovascular accident (ACVA). According to international studies, for every 20 mmHg. systolic growth or 10 mmHg. diastolic blood pressure increases mortality from stroke by 2 times. Isolated systolic hypertension increases the risk of stroke by 2-4 times. This determines the high socio-medical significance of measures aimed at reducing blood pressure in the populations of all countries.
In the city of Minsk in 2013. 1,385 people died from stroke (1,568 in 2012), of which in 1,279 cases stroke developed against the background of arterial hypertension (92.3% of all stroke). Mortality from stroke in 2013 decreased and amounted to 72.1 cases per 100 thousand population compared to 82.5 in 2012. In working age, mortality from cerebrovascular diseases in 2013 amounted to 18.3 per 100 thousand. population (2012 - 22.1), from acute stroke 16.4 and 20.3, respectively.
A stroke is an acute disorder of the blood circulation in the brain, leading to damage and death of nerve cells. A stroke occurs when a blood vessel in the brain is either blocked (by a plaque or blood clot - ischemic stroke) or ruptured (hemorrhagic stroke). After some of the nerve cells die, the body loses one of the functions for which the dead cells were responsible: paralysis, loss of speech and other serious disorders occur. The larger the area of death in the brain, the more serious the consequences of a stroke.
The prognosis for stroke depends on the extent of brain damage, but also on the quality of first aid provided, the speed of delivery of the patient to the hospital, and subsequently on the correctness and scope of rehabilitation measures. Great patience and hard work are required from the relatives and friends of a post-stroke patient in order to provide him with proper care during rehabilitation.
What's happening?
A stroke occurs when the blood vessels supplying the brain are compressed, blocked, or ruptured.
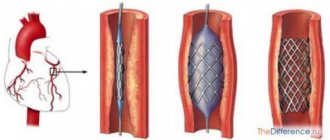
Most strokes are ischemic. According to the mechanism of development, such a stroke is very similar to a myocardial infarction (in fact, it is a cerebral infarction): an atherosclerotic plaque located in one of the cerebral arteries is destroyed, and a blood clot forms at the site of damage - a thrombus that closes the lumen of the vessel.
Brain cells lack oxygen, and if neighboring arteries cannot take over the blood supply to this area, they die within a few minutes. Much less often, the lumen of the artery is blocked by droplets of fat or air bubbles (fat and air embolism), blood clots from the left ventricle of the heart, or is compressed from the outside as a result of injury or tumor.
The cause of hemorrhagic stroke is bleeding. This occurs less frequently, but is much more life-threatening. In this case, the wall of the defective artery ruptures. The cause may be an aneurysm, or a violation of the integrity of the vascular wall due to the same atherosclerosis, and the provoking factor may be an increase in blood pressure.
A harbinger of a stroke can be a transient cerebrovascular accident, or transient ischemic attack (TIA). It can occur weeks or months before the actual stroke. This is a “small stroke” that temporarily stops blood circulation in the brain. Due to lack of blood, the brain cannot function normally.
Certain areas of the brain are responsible for the movement of arms, legs, speech, vision, etc. Therefore, the consequences of a stroke directly depend on which part of the brain the disaster occurred. This may be paralysis (complete immobility) or paresis (partial impairment of movements) of an arm or leg on the side opposite to the lesion, serious speech and writing impairments, memory disorders, sensory impairment, etc.
Manifestations of stroke.
Stroke most often occurs early in the morning or late at night. Its first signs are:
- sudden numbness or weakness in the muscles of the face, arm, or leg, especially on one side of the body;
- unexpected difficulties in articulation or perception of speech or text;
- sudden deterioration of vision in one or both eyes;
- sudden loss of coordination of movements, unsteadiness of gait, dizziness;
- sudden sharp and unexplained headache.
1. Ask the person to SMILE, showing his teeth. With a stroke, the smile becomes tense (similar to a grin) or crooked;
2. Invite the victim to close his eyes, raise his HANDS UP and hold them in this position for 10 seconds. During a stroke, the muscles weaken and the patient cannot hold his hands.
3. Ask to SPEAK. Offer to pronounce a simple sentence clearly and intelligibly. For example: “The sun is shining outside the window.” Speech disturbances are characteristic of a stroke.
4. Ask the victim to stick out his tongue. And if the tongue is curved or irregular in shape and falls to one side or the other, then this is also a sign of a stroke.
If the victim has a problem with any of these tasks, it is necessary to call an ambulance.
Diagnostics
First, doctors need to determine the type of stroke. To do this, computed tomography (CT) or magnetic resonance imaging (MRI) of the brain is performed, which allows one to distinguish a hemorrhagic stroke from an ischemic one and exclude other diseases, as well as establish the exact location and size of the affected area of the brain.
When diagnosed with hemorrhagic stroke, cerebral angiography and Dopplerography of the cerebral vessels are necessary to determine the cause of the hemorrhage. If necessary, consultation with a neurosurgeon may be required.
How to prevent a stroke
About half of strokes can be prevented. This is possible because many risk factors for stroke can be controlled. Risk factors that can be prevented:
- high blood pressure (above 140/90 mmHg);
- atrial fibrillation (a heart rhythm disorder that leads to the formation of blood clots in the cavities of the heart);
- diabetes mellitus without adequate treatment;
- elevated cholesterol levels;
- smoking;
- alcohol abuse;
- obesity;
- male gender;
- age over 50 years;
- atherosclerosis (deposition of cholesterol on the walls of blood vessels);
- presence of strokes in close relatives;
The risk of stroke increases with age, but the disease has become much younger these days. It's no longer uncommon for a 40-year-old to have a stroke. After age 55, the risk of stroke doubles with every ten year increase in age.
Rehabilitation
During a stroke, a focus of dead nerve cells forms in the brain, the position and size of which determine the degree of impairment of a particular function. And around and near it there are cells, as they say, temporarily inactivated, “inhibited.” It is they who need to return to activity. There are also those who were not previously involved in ensuring movement and speech, but are ready to reorganize and, to one degree or another, take on the “responsibilities” of the dead.
Myocardial stroke
How is a stroke different from a myocardial infarction, and what do these diseases have in common?
A stroke is an acute disorder of the blood circulation of the brain, as a result of which a section of brain tissue is deprived of nutrition and dies. When talking about a heart attack, we most often mean damage to the heart and its muscular component – the myocardium.
However, this term can also be applied to the kidneys, intestines, lungs, and also to the brain - cerebral infarction is sometimes called ischemic stroke due to softening of the brain tissue at the site of the lesion.
In both cases, due to insufficient blood circulation, acute ischemia develops and the cells die.
What is more dangerous, stroke or heart attack?
The main difference between a stroke and myocardial infarction, if you do not take into account the localization of the pathology, is the nature of the developing acute vascular disorders. In the case of a stroke, they are associated with subsequent neurological deficits; in the case of a heart attack, they are associated with heart failure.
The primary differential diagnosis between two acute diseases is carried out according to the primary symptoms - a patient with a heart attack will point to the heart and hold on to it, since the pain during an attack is extremely intense. A stroke is usually also characterized by sharp, intense pain, but not heart pain, but headache pain.
Stroke has a large list of long-term complications that reduce the quality of life and often lead to disability of the patient. Often you have to spend a lot of time and effort on treatment and recovery, ensuring that the brain structures regain their lost functions, and in this regard, a stroke is worse than a heart attack.
Both stroke and heart attack have a high mortality rate in the first hours after the attack, but we can say that a heart attack is worse - often with an extensive transmural infarction, medical workers do not even have time to catch the patient alive. In case of a stroke, there is usually a little time left (2-3 hours).
Changes in the shock organ, i.e., the brain, during a stroke can be either irreversible (usually when medical help did not arrive in time) or reversible. Deep necrotic changes in the tissues of the heart muscle are irreversible - the affected part of the muscle is lost forever, and a connective tissue scar will remain at the site of the infarction.
If a patient has had a heart attack, in most cases he will be able to return to normal life much faster than a patient with a stroke, who requires a long recovery time.
Another difference between a stroke and a heart attack is that a heart attack is more likely to recur. After a heart attack, heart failure develops for the rest of your life, and the larger the affected area, the higher the stage of failure.
In short, a heart attack is more dangerous because it causes instant death, and a stroke is more dangerous because there is a higher likelihood of disability.
What is a stroke
Stroke can be ischemic or hemorrhagic. A stroke occurs due to oxygen starvation of brain cells, which are very demanding for the presence of sufficient oxygen. In its absence, cells die and neural connections are disconnected.
In the first case, it is caused by a blockage of the vessel by a cholesterol plaque, thrombus or embolus, in the second - with hemorrhage in the brain. The released blood pushes aside, compresses the brain structures, leads to disruption of their function, and the ischemic tissue dies.
- hypertension - a constant increase in pressure has a detrimental effect on the vascular wall, promotes its degeneration, which accelerates the wear and tear of the vessel and increases the risk of rupture;
- atherosclerosis - leakage of the walls of blood vessels with fatty-protein detritus deprives the vessels of elasticity. Later, platelets and fibrin join the inflammatory process, and an atherosclerotic plaque is formed, blocking blood flow;
- thrombosis - when a blood clot breaks off, it enters free circulation, after which it can enter a brain vessel and clog it;
- congenital pathology of cerebral vessels.
These reasons, coupled with the influence of risk factors such as smoking, physical inactivity, diabetes and others, lead to stroke. Its signs are:
- numbness, paralysis of the face on one side;
- numbness of the limbs, muscle weakness on the side opposite to the lesion;
- speech disorders;
- disorientation in space;
- cognitive impairment;
- disturbances of consciousness of varying severity.
First aid consists of immediately calling an ambulance, transferring the patient to a lying position with the head turned to one side to avoid aspiration of vomit. The patient should not be left alone until the ambulance arrives.
Source: https://starlab-mdc.ru/insult/insult-miocarda.html
Main causes of heart attacks and strokes
In the vast majority of cases, the condition is ischemic in nature and is caused by embolism of the main renal vessels. Most often, the embolus is represented by a thrombotic clot; less often, fragments of atherosclerotic plaques and fatty masses can act as such. A picture similar to embolism of the branches of the renal artery is sometimes provoked by arteriovenous fistulas or bleeding. Thus, the main cause of the disease is the presence of emboli in the arterial part of the systemic circulation, which can form in the following pathologies:
- Endocarditis. Inflammation of the inner lining of the left ventricle or atrium is often complicated by the formation of a mural thrombus. Its fragments periodically enter the systemic circulation and can clog the lumen of the arteries of the kidneys.
- Arrhythmias and heart defects. Various heart rhythm disturbances are accompanied by hemodynamic disturbances inside the cavities of the heart, which sometimes leads to thrombus formation. A similar mechanism for the formation of blood clots is observed with mitral valve insufficiency or prolapse of its leaflets.
- Atherosclerotic lesion. Severe atherosclerosis of the aorta or coronary arteries is one of the most common causes of renal infarction. Blockage of a vessel can be caused either by a fragment of the atherosclerotic plaque itself or by a blood clot that has formed on its surface. Atherosclerosis of the renal vessels can lead to dissection of their walls, which also provokes blockage of the lumen and acute ischemia.
- Periarteritis nodosa. This condition of unknown etiology, if the renal vasculature is involved in the pathological process, can cause heart attacks.
- Medical manipulations. Various diagnostic and therapeutic manipulations on the organs of the urinary system can be complicated by vascular stenosis with the development of acute ischemia of the renal tissue.
The indirect cause of the pathology is sometimes drug addiction associated with frequent intravenous infusions (opioid or ephedrine addiction). In the case of using non-sterile instruments, specific endocarditis develops with the formation of numerous blood clots. Various forms of renal infarction are found in 20-30% of injection drug users. Multiple foci of infarction in the renal tissue also occur with disseminated intravascular coagulation (DIC syndrome).
Myocardial infarction is an ischemic heart disease in which necrosis occurs in the organ due to insufficient blood supply.
Half of men and a third of women encounter this disease in their lives. Today, the previously generally accepted lower limit of the disease from 35 years has dropped to 20 years. Let's figure out what can cause a heart attack.
There are a number of diseases, the presence of which in the body makes people more vulnerable to heart attack. Below we discuss those diseases and pathologists that doctors list as the causes of myocardial infarction. We separate them by the systems they affect.
Types of diseases and their connections
There are 2 types of strokes:
- hemorrhagic;
- cardioembolic, also called ischemic.
Yes, in both cases the vessels of the brain are affected. But the reason for their defeat varies. If in the first case, hemorrhage in the brain occurs directly due to ruptures of cerebral vessels, then in the second the cause of the lesion is coronary heart disease.
Ischemic stroke occurs 4 times more often than hemorrhagic stroke, and it is much more dangerous.
This danger lies in the fact that, most often, the consequence of coronary disease (and ischemia is simply blockage of blood vessels) can be the formation of blood clots not only in the vessels of the brain, but also in other parts of the human circulatory system.
Pathogenesis
The fundamental link in the pathogenesis in more than 90% of cases of renal infarction is considered to be the formation of emboli, which cause blockage of the organ’s vessels. As a result, the supply of oxygen and nutrients to the area of the kidney tissue is disrupted. In terms of oxygen demand, the kidneys are second only to nervous tissue and myocardium, which is why, as a result of ischemia, dystrophic changes quite quickly occur in nephron cells. The size of the lesion depends on the caliber of the arterial vessel blocked by the embolus - the larger it is, the more widespread the infarction zone. The characteristic shape of the ischemic zone is wedge-shaped or triangular with the apex at the renal hilum and the base facing the cortex. This is due to the peculiarities of the distribution of blood vessels in the organ.
After the cessation of arterial blood supply, the degeneration of nephron cells gradually increases, giving way to their death and the formation of areas of necrosis. At the same time, irritation of the juxtaglomerular apparatus occurs with the formation of large quantities of the hormone angiotensin 2, which leads to the development of vasorenal hypertension and a cascade of associated disorders (increases the risk of myocardial infarction or stroke). The breakdown products of necrotic tissue are absorbed into the systemic bloodstream and cause intoxication of the body, manifested by fever, headaches, and nausea. The outcome of necrosis is the proliferation of fibrous tissue and the formation of a scar.
Nature of pathologies
To better understand how these diseases differ, it is necessary to turn to the origins of their occurrence. Experts classify them as one subgroup of cardiac disorders. Wherein:
A heart attack is a disruption of the functioning of a cardiac organ, with local or all-encompassing negative changes. The nature of such manifestations is thrombosis of the vessels supplying the organ, tissue ischemia. Within a few hours, the condition worsens - necrosis. Diagnostic procedures help clarify the localization of such phenomena.
Stroke is understood as a significant disturbance of vascular circulation in the nervous structures, more often in the human brain. There are several options for manifestation - the main difference is in the form of a blood clot, or hemorrhage, or a sharp spasm of the artery. The pathology is accompanied by significant dysfunction, for which the damaged area of the brain is directly responsible.
Another distinctive feature of a stroke is the ability of neighboring neurocytes to take on an additional function - to replace dead cells. That is why rehabilitation measures for brain stroke are most effective, in contrast to developed heart attacks.
Treatment of kidney infarction
The clinical picture of the disease is characterized by varying severity of symptoms, which primarily depends on the volume of ischemic and necrotic kidney tissue. With minor heart attacks, there are no subjective complaints; pathology is detected by chance based on altered data from diagnostic studies. In the case of more extensive lesions, the symptoms become pronounced, but most manifestations are nonspecific - lower back pain, hematuria, decreased volume of urine excreted.
Painful sensations that initially occur on both sides gradually shift towards the affected kidney - bilateral infarctions are extremely rare. The intensity of the pain syndrome is sometimes comparable to renal colic; the pain is eliminated only by taking strong narcotic analgesics. The severity of hematuria during renal infarction can also vary greatly - from microscopic amounts of red blood cells in the urine to its bright scarlet color and profuse renal bleeding.
Sometimes real renal colic is observed, caused by the passage of a blood clot or piece of necrotic tissue through the urinary tract. Manifestations of renal failure are usually mild, especially when the functional activity of the second kidney is preserved. With a total infarction, toxic damage to the paired organ is possible, which is manifested by the development of acute renal failure - anuria, the smell of ammonia from the mouth and from the patient’s skin.
General symptoms of the disease are reduced to an increase in body temperature up to 38 degrees, symptoms of intoxication (nausea, vomiting, fatigue), chills. In some cases, due to impaired blood supply to the kidney, stimulation of the juxtaglomerular apparatus occurs, causing an increase in blood pressure. The above manifestations are usually combined with symptoms of the underlying pathology, which provoked ischemia and infarction of the renal tissue. These may include pain in the heart area, cardiac arrhythmias, signs of circulatory disorders due to valve defects (cyanosis, increased blood pressure in the pulmonary circulation).
The main goals of therapy for this disease vary depending on the stage of the pathological process. At the initial stages, the primary task is to restore adequate blood flow in the excretory organs, which helps to minimize the negative consequences of ischemia. In the future, the elimination of bleeding (macrohematuria), the phenomena of general intoxication and the preservation of the functionality of the remaining part of the organ comes to the fore. Often, drugs with opposite effects are used for these purposes (for example, anticoagulants and hemostatics), so the specialist is required to be especially careful when prescribing them. Conservative treatment of heart attack is reduced to the use of the following medications:
- Painkillers. The pain can be very intense; in some cases, the pain syndrome is eliminated only by powerful narcotic analgesics - morphine, fentanyl and others.
- Thrombolytic agents. These include streptokinase and other drugs of this group, the purpose of their use is to eliminate a blood clot in the vessel and restore adequate blood flow. Medicines are used only in the first stages of the disease, before the development of severe hematuria. After the start of blood excretion in the urine, the use of these drugs is strictly prohibited.
- Hemostatic drugs. Used for severe hematuria and profuse renal bleeding. The main drug in this group is sodium ethamsylate, the administration of which allows to minimize blood loss and improve the prognosis of the disease.
- Anticoagulants. At any stage of the pathology, it is recommended to take measures to normalize the functioning of the blood coagulation system; for this purpose, direct-acting anticoagulants (for example, heparin) are prescribed. The regimen, dosage and duration of use are strictly individual and are determined after studying the patient’s coagulogram.
- Antiplatelet agents. Antiplatelet agents (for example, acetylsalicylic acid) are rarely used in the acute period of the disease. They are prescribed 1-2 weeks after the disappearance of hematuria to reduce the risk of relapse and long-term complications. The dosage and duration of treatment is determined taking into account the functional activity of the excretory system.
In severe cases (for example, total renal infarction), surgical treatment is performed, which in the initial stages of the disease is reduced to restoring the patency of the main arteries and renal blood flow. In case of late diagnosis and the development of necrotic changes in the kidney, according to indications, surgical removal of the infarction area is performed, up to nephrectomy (if the patient has a second healthy organ). Among the auxiliary therapeutic measures, hemodialysis is used (for renal failure), diuretics, antihypertensives and other drugs are prescribed according to indications.
Common features and additional differences
The symptoms and causes of these diseases (heart attack, stroke) are quite similar.
General signs
- increased blood pressure;
- pale skin;
- numbness of the face;
- impaired respiratory function and shortness of breath;
- painful sensations in the head, heart;
- loss of consciousness.
A stroke often leads to partial or even complete paralysis, as the areas responsible for a person’s movement and coordination are affected. Myocardial infarction is characterized by characteristic signs: blue lips, darkening of the earlobes and the face as a whole, which indicates cardiac arrest.
Additional differences between heart attack and stroke
- A heart attack represents tissue death due to impaired nutrition of the affected organ. Stroke is an acute form of cerebrovascular accident and subsequent tissue damage.
- A heart attack refers to a fairly common form of stroke – ischemic stroke.
- If a heart attack is characterized by a malnutrition of an organ or a separate part, then a stroke is a violation of tissue integrity due to malnutrition or sudden hemorrhage.
In the first minutes after the onset of an attack, it is necessary to provide timely assistance to avoid serious complications. A heart attack quite often leads to instant death. Perhaps this is the most significant difference between these diseases. In the event of a stroke, competent actions before the arrival of doctors can not only save life, but also increase the likelihood of complete restoration of body functions.
Center for contractual medical services
- Home /
- Information section /
- Information materials /
- Complications of arterial hypertension
Today, arterial hypertension is the most common disease among non-communicable diseases, the consequences of which can lead to various complications. The most dangerous complications of hypertension that pose a threat to human life are severe damage to the brain and heart muscle - stroke and myocardial infarction.
First aid for stroke and heart attack
Signs of stroke and heart attack develop suddenly, rapidly and can take you by surprise at home, at work or on vacation. Providing first aid for a heart attack and stroke begins with calling an ambulance.
At home in case of a heart attack you need to:
- calm down;
- provide access to fresh air;
- give a comfortable position with the head end of the bed raised;
- let chew 300 mg. aspirin (“aspirin cardio”, “magnicor”).
If the patient loses consciousness, it is necessary to assess the presence of spontaneous breathing and pulse. If breathing and pulse in the carotid artery are not detected, begin a set of resuscitation measures, according to the algorithm, as in the video in this article:
With a stroke, everything is more complicated. Without knowing the mechanism of development of the disease, you should not start any measures. Medicines for stroke and heart attack are different. Using the same medications at home can be dangerous.
A patient with stroke symptoms must be provided with complete rest, access to fresh air, and high blood pressure reduced, but not more than 10% of the initial level (tissue hypoperfusion can lead to a worsening of the condition).
Patients in a coma need to ensure airway patency. You can place the patient on his side in a stable position, and if the tongue is retracted, perform the Safar maneuver, as in the photo:
Reception of Safar
If convulsions develop, you need to lay the patient on a flat surface and place a pillow under the head or roll up a blanket so that the patient does not get injured.
Stroke as a complication of hypertension
The early and most severe complication of renal infarction is the development of acute renal failure. AKI is observed quite rarely, since this requires the presence of a number of conditions - a bilateral nature of the infarction or the presence of only one kidney in the patient. With total ischemia, failure may occur due to excessive load on the second organ or due to its toxic damage.
In the long term, due to the formation of scars in the affected kidney, its functional activity decreases, which creates the preconditions for the occurrence of chronic renal failure in the future. In a number of patients, after resolution of the infarction, a persistent increase in blood pressure persists due to circulatory disorders in the kidneys.
In Russia in 2004 42 million cardiovascular diseases have been registered, this year is called an epidemic. For the first time, 5 million new cases of illnesses have been identified. Almost the majority of the total is arterial hypertension, which in 56% of cases led to the development of myocardial infarction and strokes.
Because of this, 36% of the working age population lost their jobs, social significance, and became disabled. 12% of the Russian population, unfortunately, suffered complications and joined the list of deaths. Women, as statistics show, are treated more often and resort to the help of doctors more often; 1.5 million people are not treated.
Men visit doctors less often, are treated less often, but more often suffer from complications of the disease and more often die from myocardial infarction; 2 million people are not treated. These are the sad statistics when such “silent killers” are hidden behind seemingly only elevated blood pressure numbers. Why is the situation like this?
The reasons for “REJUVENATION” of strokes are the following: • not paying attention to the first symptoms of the disease in young people • being too busy at work, there is no time to pay attention to one’s health • late presentations, when the disease has already developed • basic illiteracy of the population • old arguments that hypertension illness of the elderly • the idea that this is overwork and it will pass • avoiding medical examinations • incorrect treatment and self-medication • taking medications that do not affect the prognosis of the disease • refusing treatment when it gets better • irregularly taking medications prescribed by a doctor • herbal medicine, treatment with dietary supplements • following advertising products that healing will occur instantly, etc. As you can see, there are many reasons, and all of them are sometimes associated with our illiteracy.
What's worse: a heart attack or a stroke?
Both pathologies occupy leading positions among cardiovascular diseases and are the most common causes of death among the population of older age groups. It is difficult to say unequivocally what is more dangerous than a stroke or a heart attack. It is worth noting that brain damage can lead to more severe consequences than necrosis of a section of the heart muscle.
According to various sources, after a stroke, only 20% of patients return to normal life, another 25% become disabled. Almost 20% die within the first month, another 25 within the first year.
Mortality from myocardial infarction accounts for about 35-40% of all cases of the disease. Patients who have had a heart attack are at risk: mortality in this category is 3.5 times higher than in people without a history of heart attacks. If a patient is diagnosed with a heart attack and stroke at the same time, the chances of survival are reduced several times.
Diagnostics
The determination of renal infarction is complicated by the nonspecificity of symptoms, since lower back pain, deterioration of general condition, and hematuria are also characteristic of other nephrological diseases. In many cases, a nephrologist or urologist needs to collaborate with other medical specialists (for example, a cardiologist) to clarify the diagnosis. The speed of identifying the disease is of particular importance, since its outcome depends on the timeliness of treatment measures, and with improper treatment, the risk of complications increases. Among the diagnostic measures, the following groups of methods are distinguished:
- Interview and general examination. During the interview, attention is focused on the patient’s subjective symptoms and complaints. What matters is the severity and location of pain, the presence or absence of urination disorders. The history determines the presence of cardiovascular, hematological or other diseases that can provoke ischemia of the kidney tissue.
- Laboratory research. In a general urine test, the presence of red blood cells is almost always determined - from severe gross hematuria to microscopic blood impurities, proteinuria often occurs. In a biochemical study of urine, a specific sign of a heart attack is an increase in the level of lactate dehydrogenase (LDH), a similar increase is observed in the blood serum. In most patients, slight leukocytosis is also detected, the coagulogram parameters change - the latter is performed to assess the need to use anticoagulants.
- Instrumental research. Usually, if a renal infarction is suspected, Doppler ultrasound (USDG of the renal arteries) is performed, which allows one to assess blood flow in the main vessels of the organ. Even more information is provided by selective contrast renal angiography, the results of which reveal an area of ischemic tissue that does not accumulate contrast. As an alternative to the latter study, MSCT or MRI with contrast and subsequent 3D modeling of the renal vascular network may be prescribed.
- Endoscopic studies. Cystography for this disease is performed for the purpose of differential diagnosis. Using this method, the likelihood of bleeding from the bladder (observed with tumors, injuries) is eliminated and the one-sided nature of the lesion is clarified.
Differential diagnosis of renal infarction is carried out with tumor lesions of the urinary tract (pyelocalyceal system, ureters, bladder and urethra) and bleeding from them. Sometimes the manifestations of the disease create a false clinical picture of glomerulonephritis - it is excluded when the unilateral nature of the process is confirmed and the presence of an ischemic tissue area. With the help of additional studies, renal infarction is differentiated from renal colic due to urolithiasis and dissection of the wall of the abdominal aorta.
What is the difference?
The mechanism of development of both pathologies is based on a violation of the supply of oxygen and nutrients to tissues, which leads to their ischemia and death. So what is the difference between a heart attack and a stroke? The term "heart attack" has a broad meaning. It is called pathological damage to an organ that occurs as a result of the death of its cells. Thus, a heart attack can occur in the lungs, heart, brain, kidneys, liver, and intestines.
When making a diagnosis, the affected organ must be indicated. The most common and dangerous type of heart attack is myocardial pathology as a result of impaired oxygen delivery to the tissues of the heart.
The poor prognosis for the disease is due to the high mortality rate from the disease itself or from complications.
By stroke we mean an acute decrease in blood flow to the brain tissues, which entails their damage with the formation of focal, cerebral symptoms. This term is used in neurology when formulating a diagnosis. Depending on the factor that caused the cerebrovascular accident, strokes are divided into ischemic and hemorrhagic.
It is not difficult to distinguish strokes from each other. A characteristic feature of ischemic stroke is that during its development the patient is conscious and signs of focal neurological symptoms predominate. Numbness of the limbs occurs, turning into paresis/paralysis. Hemorrhagic stroke most often affects young people. It develops suddenly with a sharp headache, dizziness, fainting, and convulsions. Most patients experience increased blood pressure and temperature. The clinical picture is dominated by meningeal signs ("pointing dog" posture, Kernig's and Brudzinski's symptoms).