Stroke is a dangerous condition associated with circulatory disorders in the brain, which can provoke irreversible changes in the body and sometimes lead to death.
In the last few years, stroke and one of its varieties called microstroke have been diagnosed not only in older people, but also in young people, and they can manifest differently in men and women.
To save a person’s life in this case, it is necessary to quickly identify the disease and deliver it to a medical facility within three hours, where professional assistance will be provided.
How to recognize the signs of stroke and micro-stroke in men, and how do these conditions differ from each other?
Characteristic
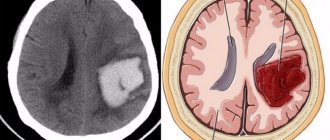
Stroke is a condition caused by cessation of blood supply to an area of brain tissue or intracranial hemorrhage, resulting in compression of nearby brain structures. A microstroke or TIA (transient ischemic attack) is a small form of stroke that is transient in nature, which implies a short-term disturbance.
A microstroke in men and women is a neurological failure that occurs suddenly and is associated with focal ischemic damage to a region of the brain. Symptoms of a microstroke, which resemble the signs of a stroke, in men and women are expressed in a short-term cessation of the functions of certain organs and parts of the body, depending on the location of the pathological focus in the brain.
The latent danger of a mini-stroke is irreversible damage to the brain. Ischemia (local deterioration of blood supply) covers a small area of nervous tissue, so the symptoms of a microstroke in women and men are mild, which can be overlooked if you do not pay attention. Unnoticed manifestations do not pass without a trace. Consequences of a microstroke in men and women:
- Increased risk of developing a major stroke (4-10% of patients during the next 2 days after TIA, 10-20% of patients during the next 90 days after TIA, 25-29% of patients during the next 5 years after the debut episode of TIA ).
- Damage to the medulla with a cumulative effect, resulting in the development of vascular dementia and slowly progressive neurological deficits.
- Increased risk of death due to myocardial infarction (6-10% of patients who have had a TIA annually).
On Wikipedia, a microstroke is listed as PNMK (transient cerebral blood flow disorder), manifested by general cerebral or focal symptoms, and the disorders are reversible and regress within 24 hours; after the episode, minor organic disorders are possible, such as deterioration of cognitive abilities, changes in the psycho-emotional background (frequent mood swings, irritability, depression), behavioral disorders.

TIA is rarely diagnosed at a young age. The pathology is common among middle-aged and elderly patients over 40-45 years old. Older age is a risk factor for developing an episode of TIA. Other provoking factors include a history of stroke, hereditary predisposition (presence of close relatives who have had a stroke), male gender (2.7% of cases among men over 65 years of age). In female patients, pathology is diagnosed less frequently (1.6% of cases among women over 65 years of age).
First aid for stroke
A few hours after the mini-stroke, the victim’s condition returns to normal, and the first symptoms disappear. Serious fears for the patient’s life arise if the symptoms of the disease become prolonged. Often the short duration of a micro-stroke allows the patient to calm down and continue to lead the lifestyle to which he is accustomed. But the consequences of the disease can be very serious and sooner or later lead to a stroke.
The first signs of the disease can be identified as follows:
- Ask the patient to smile. If the facial muscles are distorted, the blow can be determined with great confidence.
- Ask to hold your hands in front of you for a few seconds. In case of a stroke, this is impossible to do, since there is great weakness not only in the arms, but throughout the whole body.
- When asked to tell about his well-being, a person cannot answer, he gets confused in words, as if in a state of alcoholic intoxication.
In such situations, urgently need to call a doctor , as there are signs of a stroke.
What you can do before the ambulance arrives:
- Place the patient on a hard surface with something under his head. This will prevent brain swelling.
- If vomiting is observed, then you need to tilt your head to the side so that the person does not suffocate.
- Untie the tie and loosen the collar, unfasten the belt on the trousers. The main thing is to ensure air flow.
- You should not give the patient anything to eat or drink, as his swallowing function may be impaired and he will simply suffocate.
- Measure the pressure. In case of high levels, you can give medicine prescribed by the doctor. You cannot decide on the treatment of emerging hypertension on your own.
Differences between stroke and mini-stroke
A microstroke differs from a stroke in its shorter duration and weaker severity of symptoms, which often results in ignoring the problem. Many patients suffer a mini-stroke on their feet, not paying attention to warning signs. The difference between a TIA and a stroke is the speed of recovery from an episode of cerebral blood flow disruption.
Typically, the signs of a microstroke in women and men regress within 24 hours, while after a stroke, severe disorders can be observed for 3 days and subsequently require rehabilitation, the period of which usually exceeds 3 months. To distinguish TIA from stroke, an MRI examination is performed.
The difference between TIA and stroke is the reversibility of structural changes in the brain matter. TIA is not accompanied by the formation of an area of neural tissue necrosis (cerebral infarction), which is confirmed by the results of MRI (diffusion-weighted imaging). With TIA, the occurrence of a heart attack is unlikely if the duration of blood supply failure does not exceed 1 hour.
To understand that there was a stroke or a micro-stroke, you need to know the differences between them, for example, such as the duration of the attack of cerebral insufficiency. The duration of a TIA episode usually does not exceed 1 hour, in most cases the episode lasts no more than 5 minutes. In ischemic stroke, severe neurological deficits are observed for much longer.
Kinds
Thinning of the vascular wall, as a result of which it ruptures, leads to hemorrhagic stroke. Signs characteristic of this species:
- The patient falls, becomes disorientated, and coma may occur;
- Breathing is accompanied by wheezing;
- There is a pressure surge;
- The eyes move involuntarily;
- Vomiting may occur;
- Paralysis occurs on the side opposite to the affected hemisphere.
Ischemic stroke is characterized by impaired blood circulation in the brain, causing neurological changes in the psyche. The patient's condition becomes serious after a couple of days.
Causes and pathogenesis
A microstroke is a violation of cerebral blood flow that occurs due to polymorphic causes, which determines its symptoms. The reasons that cause a micro-stroke are similar to those that provoke the development of a large-scale disorder of cerebral blood flow that occurs in an acute form. The main reason is obstruction (obstruction) of the vascular bed, provoked by factors:
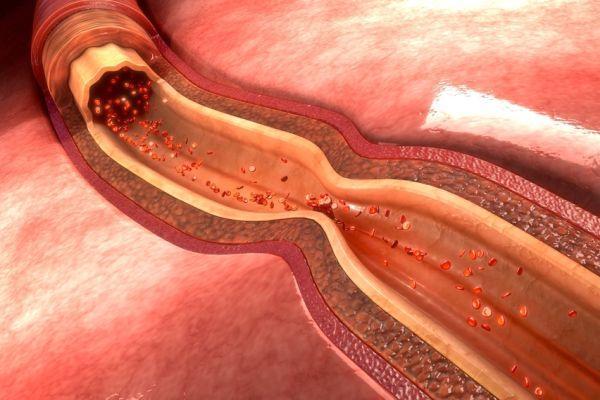
- Atherosclerotic lesion of arteries. When atherosclerosis develops, atherosclerotic lipid plaques form, which grow, block the vascular lumen and impede blood flow.
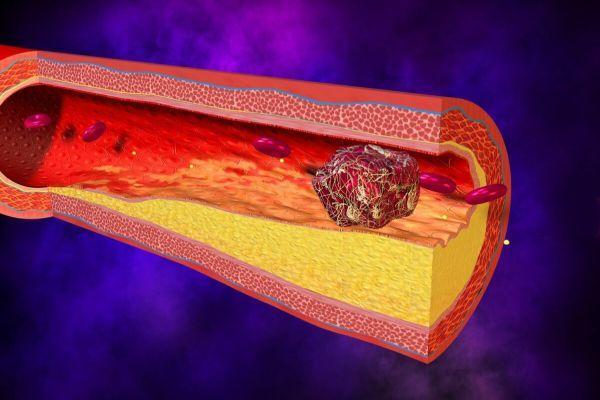
- Embolism (a pathological process accompanied by the presence and circulation in the blood of emboli - atypical particles that are normally absent in the blood and lymph). Embolism often leads to occlusion (blockage) of the vascular lumen, which is associated with insufficient blood supply in the local area.
- Thrombosis (a pathological process accompanied by the intravital formation of blood clots). Blood clots prevent the free flow of blood in the vessels.
The lacunar form develops against the background of a violation of the neurohumoral regulation of the tone of the vascular walls, which causes a sharp narrowing (spasm) of small arteries and arterioles. The main provoking factors in all cases are diabetes mellitus and arterial hypertension - diseases accompanied by damage to the vascular wall. Other provoking factors:
- Dyslipidemia (lipid metabolism disorder, increased concentration of lipids in the blood).
- Smoking, alcohol abuse.
- Obesity of the abdominal type (deposits of fatty tissue mainly in the abdominal cavity).
- Physical inactivity (low physical activity).
- Diet with a predominance of animal fats.
- Chronic stress, depression.
- Heart diseases (myocardial infarction, infectious endocarditis, atrial fibrillation).
- Vasculitis (a systemic disease accompanied by inflammation and damage to the walls of blood vessels).
Insufficient blood supply to the brain tissue leads to the development of specific reactions called the ischemic cascade. Ischemic processes in the area of the medulla during a microstroke can spread to other parts of the brain if the patient is not provided with timely assistance.
Occlusions of thrombotic origin, embolism of cerebral vessels, occlusion of small-caliber cerebral vessels of non-thrombotic origin, stenosis of cerebral arteries that occurs against the background of hypotension and reduces the volume of cerebral circulation in the main arteries are the most common reasons for the development of microstroke in women and men.
In the general group of PNMK, TIA, cerebral dysfunction (short-term paroxysms in the form of fainting) and cerebral crisis of hypertensive origin are distinguished. In cerebral crisis, a sharp and significant increase in blood pressure plays a decisive role in the pathogenesis.
Episodes of cerebral dysfunction occur as a result of intense compression (compression) of the vertebral artery, which is caused by sudden turns of the head. To understand how a microstroke occurs, it is important to understand the development mechanism. Main stages of pathogenesis:
- Violation of autoregulation of blood circulation in the brain - spasm of the muscles of the vascular wall with the development of a state of stagnation of blood in the veins and capillaries.
- Blockage of the vascular bed with micro-emboli and micro-thrombi against the background of changes in blood aggregation characteristics.
- The development of perifocal edema due to an increase in the volume of extracellular space as a result of an increase in the permeability of the membrane of the cells that form the capillary endothelium. Membrane permeability is higher in cells located in the affected area.
- The appearance of local foci of ischemia against the background of thrombosis of small arteries or obliteration (closure) of the vascular lumen while maintaining compensatory (replacement) blood supply in the area of the circle of Willis.
- Stenosis (persistent narrowing of the lumen) of the main arteries as a result of a decrease in blood pressure.
- Intracranial micro-hemorrhage (local foci of hemorrhage).
An episode of TIA is most often caused by embolism of the cerebral arteries (carotid, vertebral). Sometimes attacks occur against the background of hypoperfusion (a decrease in the volume of blood passing through the nervous tissues) - a condition that occurs as a result of severe hypoxemia (oxygen deficiency) and leads to structural changes in the medulla with the appearance of focal neurological symptoms.
Other causes of a TIA episode include a deterioration in the function of oxygen transport in the blood (for example, due to anemia or carbon monoxide intoxication), an increase in blood viscosity (for example, against the background of polycythemia - an increase in the concentration of red blood cells and platelets in the blood). The listed diseases are especially dangerous if they occur against the background of stenosis of the arteries supplying the brain.
Subclavian syndrome (a symptom complex that occurs due to occlusion of the proximal segment of the subclavian artery, which leads to a compensatory weakened blood flow in the vertebral or internal thoracic artery) in combination with intense physical work with the hands provokes increased blood supply to the upper extremities.
As a result, the volume of blood entering the vertebral artery is reduced. The main blood flow goes in the direction of the subclavian artery, which is accompanied by a reduction in the volume of blood entering the vertebrobasilar basin. As a consequence of the pathological process, signs of ischemia appear, including episodes of TIA.
TIAs often occur in young people and children against the background of heart pathologies, accompanied by high hematocrit values (concentration of red blood cells in the blood) and the development of embolism. To understand how to recognize a microstroke, it is important to know its symptoms.
Pre-stroke condition: symptoms in women and men, treatment, consequences
Not a single acute cerebrovascular accident (ACVA, stroke) occurs by chance.
A life-threatening condition always has a prehistory, and it is not necessarily a chronic, severe illness. Sometimes strokes occur against a background of stress or physical strain, and they are almost always based on incorrect prioritization. A person neglects his health, ignores painful symptoms due to being too busy at work or in the family, and sometimes simply does not take care of himself.
We invite you to talk about what a pre-stroke condition is, how it manifests itself, and what to do to avoid trouble.
Possible reasons for development
There are two types of stroke: hemorrhagic and ischemic (cerebral infarction).
Hemorrhagic stroke occurs as a result of a rupture of a cerebral vessel or a partial violation of its integrity, in which blood begins to leak through the wall of the vessel. In medical terminology, this condition is called cerebral hemorrhage.
An ischemic stroke is caused by a temporary blockage of arteries in the brain, as well as large arteries such as the carotid or vertebral arteries.
As a result, oxygenated blood stops flowing to a certain area of the brain.
Most often, the blockage of blood flow is associated with a blood clot or atheroma, which, together with the bloodstream, enters the narrow vessels and arteries of the brain, completely blocking their patency.
If incomplete blockage of the vessel occurs, then this condition is temporary and, with emergency treatment, reversible. It's called a transient ischemic attack.
At this time, a person begins to experience characteristic symptoms that precede a future stroke. Unlike a stroke itself, a transient ischemic attack does not cause serious brain damage, but is still very dangerous.
It is impossible to establish a reliable reason why at some point a blood clot or atherosclerotic plaque breaks off and enters the general bloodstream.
There is an assumption that this occurs under the influence of factors that provoke a jump in blood pressure and spasm of the arteries of the brain:
- temperature effects (overheating, heat stroke, hypothermia);
- consumption of drinks containing ethyl alcohol;
- severe emotional shock;
- prolonged exposure to stress;
- physical exercises performed with high frequency and large amplitude.
In addition, a pre-stroke condition includes a hypertensive crisis and its complication – hypertensive encephalopathy. They can be caused by a sharp sudden increase in blood pressure as a result of advanced hypertension, eclampsia, nephritis in the acute stage and other serious diseases.
Dangerous symptoms of pre-stroke
Two conditions are precursors to strokes: transient ischemic attack (TIA) or hypertensive crisis. The symptoms of both pathologies overlap with each other, but there is an important difference - with TIA the patient always loses consciousness, with a hypertensive crisis this rarely happens. It also matters how long the TIA lasts.
If the duration of the attack exceeds a day, the attack almost always ends in a stroke. In case of a hypertensive crisis, the scenario is slightly different - if the attack can be stopped quickly, there is no need to fear a stroke. If the rise in blood pressure occurred suddenly and first aid was not provided to the patient in a timely manner, the next step may be a stroke.
Important: Episodes of TIA are a warning to the patient about the threat of a stroke. A stroke can occur within 5 years after the attack.
The clinical picture of pre-stroke directly depends on the ischemic or hemorrhagic type of future circulatory disorder.
Ischemic type
Let's look at what symptoms determine the pre-stroke condition, in which treatment is aimed at eliminating ischemia.
Symptoms of ischemic pre-stroke increase gradually and occur in people over 50 years of age. Here are the most common manifestations:
- speech disorders - a person confuses syllables, pronounces words unclearly, or cannot speak at all,
- pronounced pallor of the skin and severe joint weakness,
- asymmetry of the face, its numbness - the corner of the mouth drops, the tongue deviates to the side,
- weak pulse filling and chest pain,
- double vision, monocular blindness.
Important: This symptomatology is possible against the background of normal blood pressure and temperature.
Hemorrhagic type
Unlike ischemia, hemorrhagic pre-stroke is characterized by a sudden onset. The following symptoms are observed:
- severe weakness or motor agitation,
- sudden fainting,
- sudden changes in emotional state - sudden joy, depression, rage,
- involuntary movements - the patient slaps his hand on his body, waves his hands, etc.,
- heavy sweating,
- severe hyperemia, bluishness of the face or, on the contrary, severe pallor,
- convulsions,
- difficulty breathing.
Features of age and gender
As we noted earlier, in pre-stroke conditions, symptoms occur more often in men than in women. The most common age group is working men over 45 years of age, but under 60 years of age.
If a person does not have the chronic pathologies that we described above, the development of the disease is associated with previous intense physical work and bad habits.
Often, a pre-stroke condition develops as a complication of alcohol withdrawal or alcohol withdrawal syndrome.
Signs of a pre-stroke condition rarely occur in women of reproductive age. More often, the attack begins in elderly women who have crossed the 60-year mark. In the postmenopausal period, women develop vascular pathologies, the level of cholesterol in the blood increases, and arterial hypertension appears, which leads to pre-stroke.
It is hardly reasonable to talk about the isolation of symptoms and consider some signs only male, and others only female. The type of condition matters - ischemic or hemorrhagic and the presence of concomitant pathologies.
Who is at risk?
Most often, stroke is diagnosed in older people over 50 - 60 years old, but it can also happen in young people. That is, in fact, at any age.
The risk group with a predisposition to vascular accidents includes people suffering from:
- high blood pressure (hypertension);
- heart rhythm disturbances;
- diabetes mellitus;
- pathologies of the blood coagulation system;
- obesity (especially abdominal type);
- low mobility;
- diseases accompanied by high cholesterol levels;
- abnormalities in the development of cerebral vessels;
- alcohol and nicotine addiction.
Treatment
It is carried out using several methods. There are three tasks. Relieve symptoms and residual signs, eliminate the root cause and prevent relapses.
Drug correction involves the use of the following drugs:
- Antihypertensives if there is a stable increase in blood pressure. ACE inhibitors, beta blockers, calcium antagonists, centrally acting agents, diuretics with a mild potassium-sparing effect.
- Statins. For the rapid removal of cholesterol and the elimination of already formed plaques, provided that they have not hardened due to calcium salts. Atoris as the main one.
- Anticoagulants and antithrombotic. Eliminate blood clots. They are not allowed to form. Restore the fluidity and rheological properties of liquid connective tissue. Heparin or Aspirin-Cardio.
- Angioprotectors. Protects blood vessels from destruction.
Other medications as indicated. If medications are ineffective or obviously ineffective, surgical treatment is prescribed.
It is mainly needed for advanced atherosclerosis, vascular defects, such as congenital anomalies or aneurysms, and other processes.
Source: https://neuro-orto.ru/bolezni/ynsult/predynsultnoe-sostoyanie.html
Symptoms
To find out whether a woman or a man had a microstroke, you need to be able to recognize the manifestations of pathology, such as sudden darkness and confusion, loss of the ability to understand someone else’s speech and pronounce words.

If damage to the ophthalmic artery occurs, amaurosis is observed - monocular blindness of a transient type. Amaurosis is absolute blindness that occurs without obvious anatomical disturbances in the structure of the eye. The main cause of amaurosis is deterioration of blood circulation in the circulatory network formed by the carotid arteries. Frequently occurring disorders are accompanied by paresis of the facial nerve, which is manifested by the absence of facial expressions (the face resembles a frozen mask).
The first signs of a micro-stroke in women and men may go unnoticed, so patients do not consult a doctor; the consequences of a stroke suffered on the legs are expressed in a deterioration in general well-being and cognitive abilities (memory, mental activity), decreased performance, and rapid fatigue. The first signs of a microstroke in women and men are identical to the symptoms of stroke:
- Paresthesia (sensitivity disorder). Feeling of numbness, burning sensation, tingling, crawling sensations mainly in the area of the limbs and face.
- Visual dysfunction (double vision, loss of visual fields, spots, dots, foreign objects in the field of view, less often visual hallucinations). Most often, the vision disorder affects one eye.
- Pain in the head area is sudden and acute.
- Dizziness, inability to maintain balance.
- Impaired gait and motor coordination.
- Difficulty swallowing (dysphagia).
- Convulsive attacks of a short duration.
To recognize a microstroke in men and women, attention is paid to disorders that occur against the background of damage to the brain, such as the inability to raise the arm, paralysis of the facial muscles, expressed in the absence of facial expressions in one half of the face. TIA in older people may present with the following symptoms:
- Contralateral (in one half of the body, on the side opposite to the pathological focus) hemiparesis. When the anterior cerebral artery is damaged, the leg is predominantly involved; damage to the middle cerebral artery is mainly manifested by muscle weakness in the arm and face.
- Urinary incontinence.
- Aspontaneity (lack of motivation for speech, motor and other types of activity).
- Hemianesthesia (loss of skin sensitivity in one half of the body).
- Pathological reflexes (for example, the Babinski reflex, which occurs as a result of line irritation of the sole of the foot and is manifested by extension of the big toe, or grasping, which occurs as a result of line irritation of the palm with an object, which the patient in response involuntarily and strongly squeezes in his hand).

Some patients experience hemiballismus - hyperkinesis, manifested by sudden, uncontrolled movements of large amplitude with a rotational component in one half of the body. A frequent symptom is apraxia (a condition characterized by a violation of voluntary complex motor activity while maintaining the ability to perform purposeful elementary movements).
With TIA, neurological symptoms are short-term and mild, so patients often do not notice signs of pathology. Symptoms of TIA appear suddenly, last 2-30 minutes, then regress without a trace. The frequency of episodes varies significantly. Some patients may have several attacks throughout the day, while others may have several episodes throughout the year.
Signs of a microstroke suffered on the legs
Due to increased busyness and confidence in their own indestructible health, not all patients can promptly recognize the symptoms of a mini-stroke. Some suffer a relapse on their feet. Since the symptoms are mild, the man is not even aware of the threat to life and health. The first signs of the pathological process are blurred vision and severe dizziness, which forces the patient to take a horizontal position.
Other noticeable symptoms of transient ischemic attacks suffered on the legs:
- increased irritability, weakness;
- distortion and numbness of the face and body;
- impaired coordination of movements;
- increased sensitivity to loud noises and bright lights;
- fever, sensation of heat, severe chills.
Diagnostics
Pathology is diagnosed based on clinical manifestations. To confirm suspicions, instrumental diagnostics are performed, mainly CT and MRI. To determine a microstroke in a person at home, they rely on such an important criterion as the reversibility of the neurological deficit. In patients who have suffered a TIA, the functions of the nervous system are fully restored within 1 hour.
Diagnosis of a microstroke will be helped by methods that are used to identify the causes of PNMC, for example, such as a blood test that shows the concentration of lipids and glucose in the blood, or angiography that allows you to determine the state of the elements of the circulatory system that feeds the brain. Echocardiography reflects the functional state of the heart.
The diagnosis of TIA is made retrospectively, based on descriptions of episodes that occurred in the past. The main criteria are symptoms of ischemia in a specific arterial basin, which completely regress after 1 hour. The clinical picture of TIA does not include such signs as isolated stupefaction, loss of consciousness, or isolated paralysis in the area of innervation of the facial nerve.
To check whether there has been a microstroke, it is necessary to undergo an examination by an ophthalmologist, who carries out diagnostic procedures such as examining the fundus of the eye and determining the condition of the blood vessels of the eye. Sometimes, during an ophthalmological examination, a retinal infarction is detected, which is associated with atrophic processes in the area of the optic nerve.

How does stroke manifest in men?
In men, signs of stroke and micro-stroke are expressed as follows:
- hearing loss;
- the person’s consciousness is confused;
- he cannot navigate;
- feeling of heat;
- "viscosity" of speech.

These symptoms are complemented by the same signs as in women - increased sweating, severe headache, loss of balance. The damage depends on which parts of the brain are affected.
Treatment
Having discovered typical signs of a microstroke, you need to arrange for the patient to be transported to a medical facility, where they will conduct an examination and prescribe treatment. Early contact with your doctor is associated with a lower risk of complications and negative consequences, such as the development of recurrent attacks.
In cases where TIAs are associated with changes in the rheological characteristics of the blood, therapy with antiplatelet agents (suppress the process of platelet accumulation and their adhesion to the endothelium of the vascular wall) and anticoagulants (prevent the formation of blood clots by reducing the activity of the protein involved in the blood clotting process) is indicated.
A microstroke caused by reasons such as atherosclerosis or thrombosis of the carotid artery often requires surgical treatment, which reduces the risk of stroke. In these cases, a carotid endarterectomy is performed (removal of plaques, thrombi, emboli from the arterial bed that obstruct blood flow) or a stenting procedure (installation of a cylindrical frame - a stent into the vessel cavity to prevent narrowing of the lumen) of the carotid artery.
To find out how to treat a microstroke, you need to make an appointment with a neurologist, who, based on the results of a diagnostic examination, will select a therapy program. Patients who have suffered a TIA are prescribed drug treatment (antiplatelet agents, anticoagulants, statins) aimed at preventing the occurrence of stroke. At the same time, risk factors are corrected - treatment of arterial hypertension, hypercholesterolemia, diabetes mellitus, and heart pathologies.

Prevention
It is known that it is better to avoid health problems than to carry out treatment or resuscitation measures. How to prevent the development of a microstroke?
- Give up bad habits and become a supporter of a healthy lifestyle.
- Treatment of the underlying existing disease.
- Clinical observation and implementation of all recommendations of the attending physician (for example, with high blood pressure).
- If a microstroke has occurred, measures must be taken to prevent a recurrence. To do this, it is necessary to determine the individual causes of the disease. When the first symptoms appear, you should seek medical help as soon as possible.
- To remain healthy and able to work, a man should make changes to his lifestyle and diet.
Be healthy!
First signs
The focus of a stroke can be located either on the right side of the brain or on the left. With a right-sided stroke, pain appears in the left side of the body, and with a left-sided stroke, vice versa. Based on the nature of the lesions, strokes are classified into ischemic and hemorrhagic strokes. Most often, ischemic stroke occurs in men; the second type of this disease is less common, but is more dangerous.
There is another type of stroke called a microstroke. This is a short-term disturbance of cerebral circulation, lasting from several minutes to several days and going away on its own. During a micro-stroke, damage to small vessels occurs, which does not pose a threat to life and does not cause severe functional damage to the brain and body. Most often, the patient does not even suspect that he has suffered such a stroke.
Harbingers of an impending stroke or mini-stroke are the following changes in health and behavior:
- headaches that occur several times a day and are not relieved by analgesics;
- dizziness;
- weakness;
- nausea;
- sharp pain in the back of the head;
- noise in ears;
- high blood pressure;
- violation of motor functions: coordination, accuracy, clarity of movements;
- redness of the face as a result of a rush of blood to the head;
- unilateral numbness of the arms and legs;
- rapid breathing;
- "goosebumps;
- incoherence of speech;
- mood swings.
Progressive symptoms of a pre-stroke condition manifest themselves in more severe health problems. The first signs of stroke in men are divided into 3 groups:
- Vegetative, which include:
- profuse sweating;
- tachycardia;
- feeling of dry mouth, thirst;
- feeling of heat.
- General cerebral:
- severe headaches;
- nausea;
- clouding of consciousness;
- impaired coordination of movements;
- loss of orientation in time;
- weakening of memory, concentration;
- loss of mental clarity;
- apathy or increased excitability.
- Focal, caused by damage to one or the other hemisphere and manifesting itself in the form of:
- numbness of the limbs or their paralysis;
- paresthesia, expressed as a decrease in the sensitivity of the epidermis on the affected side of the body;
- speech disorders;
- loss of consciousness;
- increased salivation;
- uncontrolled urination and bowel movements;
- swallowing dysfunction;
- visual and hearing impairments;
- drooping eyelids;
- slowing heart rate;
- memory loss;
- dilation of the pupil on the side of the affected part of the body.
The same symptoms indicate that a micro-stroke is beginning, but they are mild, short-lived and perceived by a man as a mild ailment.
A micro-stroke suffered on the legs is dangerous because it increases the possibility of developing a full-blown stroke, the treatment of which will be more difficult and the chances of a full recovery are less. You should consult a doctor if you have been observing for several days and then go away on their own:
- temperature increased to 37°С;
- dizziness;
- sweating or chills;
- unsteady gait;
- recurring difficulties with vision, hearing or speech;
- slight tingling or numbness in the extremities;
- deterioration in coordination of movements.
In alcoholism, the symptoms of an incipient stroke are:
- glassy look;
- facial redness;
- Pain in the eyes;
- state of stupor;
- indistinct muttering, burr, lisp;
- increasing headache;
- uneven breathing;
- pulsation in temples;
- nausea that gets worse when trying to stand up or sit down;
- vomit.
Young men 30-40 years old are not at risk, but sometimes they have strokes. Signs of a stroke in a 30-40 year old man may not be obvious to others, but he will definitely feel sudden attacks of throbbing headache, noise in the head, and photophobia. Timely help will only come if the man recognizes the internal symptoms and immediately consults a doctor.
A stroke at 30 years of age, like a heart attack, is extremely rare in men and is the result of traumatic brain injury or congenital pathologies associated with diseases of the cardiovascular system and hypertension. There are no external signs of the disease, so if the person is conscious, the doctor will ask questions to understand what the patient is feeling.
Ischemic stroke
In 80% of cases, men have ischemic stroke. Its main symptom is narrowing or blockage of the supply vessel. However, the blow does not occur immediately; it develops over 4-5 days and is accompanied by:
- dizziness;
- persistent weakness;
- severe headaches that are not relieved by antispasmodics;
- short-term numbness of the limbs;
- decreased visual acuity.
These sensations intensify and after a short time lead to failure of one side of the body. In most cases, the patient remains conscious, but sometimes clouding of consciousness occurs, accompanied by bouts of vomiting.
If the area of brain damage has stopped expanding, the victim may experience a feeling of improvement and the thought that there is no need to see a doctor. However, such an effect is deceptive, short-lived and should not mislead either the victim himself or those nearby.
Hemorrhagic stroke
Hemorrhagic stroke is much less common, but the outcome of the disease is more severe: the possibility of death is several times higher, and in case of recovery - disability. This type of stroke occurs as a result of a rupture of an artery, which in most cases is a consequence of a sharp increase in blood pressure. Two factors simultaneously pose a danger: rapid blood loss and the filling of brain tissue with blood, which leads to narrowing and compression of other blood vessels, the development of hypoxia and necrosis.