Does myocardial infarction depend on blood pressure?
In the classic course of a heart attack, there is a certain connection between the period of its development and fluctuations in blood pressure. Even an experienced specialist cannot say exactly what pressure and pulse are during a myocardial infarction. A clear relationship between changes in its level and the progression of tissue necrosis has not been established. An attack can develop both when blood pressure is relatively normal, and when it is elevated or decreased.
It is assumed that the “behavior” of pressure depends on the patient’s tendency to arterial hypertension before a heart attack. That is, in hypertensive patients it, as a rule, increases during an attack; in people with normal blood pressure, blood pressure remains within the normal range or slightly exceeds it.
Clinical signs of myocardial infarction are often vague. The situation is the same with blood pressure: not in all cases it increases and decreases according to the classical pattern.
Treatment of the disease
In case of a heart attack, an ambulance takes the person to the hospital. To dissolve the clot and restore blood flow to the heart, the patient is given thrombolytics in the first 2 hours. Later, medications are prescribed to prevent the rupture of lipid plaques, maintain muscle function, reduce pain, and increase blood pressure. If there are exacerbations, the treatment regimen is adjusted. In most cases, surgery is indicated.
The patient will have to remain in bed and avoid minimal physical activity. Recovery lasts about 10 weeks. Heart failure is often associated. If help is delayed, blood pressure drops sharply and complications arise. In any case, for a person who has had a heart attack, doctors prescribe medications that must be taken constantly. The rehabilitation period lasts a long time, which depends on where the scar is located and how damaged the muscle is.
Fluctuations in pressure against the background of the general symptomatic picture
There are five stages of infarction development: pre-infarction, acute, acute, subacute and post-infarction. Each of them is characterized by certain blood pressure indicators.
Pre-infarction period
The pre-infarction (prodromal) period is characterized by impaired coronary blood flow and lasts from 2-3 minutes to 10 days:
- attacks of unstable angina are observed, the heart rate accelerates, and dizziness occurs;
- moderate pain in the chest, radiating to the epigastric area, between the shoulder blades, and the cervical-occipital part;
- symptoms of heart failure are noted: sweating, chills, feeling of coldness in the extremities, difficulty breathing;
- there is no effect from taking nitroglycerin (or it is minimal);
- anxiety increases, unreasonable fears appear;
- Heart sounds are characterized by a certain muffledness.
In the pre-infarction period, there is an increase in blood pressure with a subsequent decrease immediately at the beginning of the transition to the most acute stage.
On the electrocardiogram you can already see characteristic signs of a future heart attack. At this stage, the attack can still be avoided if adequate therapeutic measures are taken.
The most acute period
The most acute (febrile) period lasts from 30 minutes to 4 hours. Characterized by tissue death (necrosis) in the area of myocardial ischemia:
- pain in the center or left half of the chest becomes unbearable; patients describe it as pressing, burning, squeezing, bursting, “dagger-like”;
- the pain syndrome has a wave-like character: it may subside, but will soon return;
- the heart rate changes: the pulse during a heart attack can either slow down (up to 50 beats/min) or speed up (up to 100 beats or more); with an uncomplicated course it remains within standard limits;
- the patient experiences shortness of breath, severe weakness, headache, dizziness;
- a growing feeling of restlessness, anxiety, doom;
- increased sweating, chills, nausea, vomiting are observed;
- a person’s lips, nose, ears, and subungual spaces become bluish, and the skin becomes pale.
The behavior of blood pressure in the acute period is determined by those indicators that were characteristic of the patient before the attack. In normotensive patients with an uncomplicated heart attack, the pressure increases slightly, which is associated with spasm of the coronary vessels, but then quickly normalizes. In hypertensive patients, the increase is more significant - up to 190/100 mm Hg; in hypotensive patients, blood pressure is in the range of 120-130/80-90 mm Hg.
Acute, subacute and post-infarction period
Acute is the period of the next 12-14 days after the attack. It is characterized by the completion of the formation of a necrotic focus. Blood pressure at this stage is usually low or normal.
In the subacute (up to 60 days after the attack) and post-infarction period (from 2 months to the end of life), scar tissue forms at the site of myocardial damage, and the cardiovascular system adapts to new operating conditions. The risk of developing life-threatening complications, as well as the likelihood of a second heart attack, is significantly reduced.
In most patients suffering from hypertension before the attack, blood pressure again begins to exceed standard values, which indicates the need to take antihypertensive drugs. Some patients experience decreased levels.
There are observations that in females the symptoms of all periods are less pronounced than in males. Blood pressure during myocardial infarction in women is not subject to sharp fluctuations, the heart rhythm is relatively stable. If a woman did not suffer from hypertension before the attack, then it is often possible to diagnose a heart attack only with the help of an ECG and a biochemical blood test.
Can a hypotensive person have a myocardial infarction?
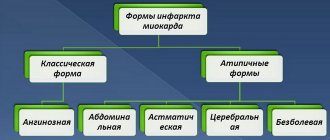
The symptomatic picture of the disease is very diverse. The attack often has an asthmatic, arrhythmic, cerebrovascular, abdominal (masked as an upset stomach) and even painless form. Naturally, with an atypical course of the disease, it is difficult to track the presence of any changes in blood pressure.
A heart attack with low blood pressure is rare, but possible. Most often it is characteristic:
- for people suffering from chronic hypotension;
- for patients with diabetes, the elderly;
- with extensive or repeated heart attacks;
- with the collaptoid form of the disease.
It is important to understand that with low blood pressure, nitroglycerin - traditionally used for a heart attack - is contraindicated, as it provokes an even greater decrease until the development of collapse.
Blood pressure after myocardial infarction
After an attack, daily monitoring of blood pressure levels is of utmost importance. In a person who has had a heart attack, the pressure should not exceed 130/80 mm Hg. The measurement is taken at rest on the arm where it is higher (usually the left arm).
In order to prevent surges in blood pressure, in addition to acetylsalicylic acid and statins, systematic use of antihypertensive drugs is required. Most often, beta blockers are prescribed for this purpose. Research results confirm that drugs from this pharmaceutical group reduce the mortality of patients in the post-infarction period, reduce the risk of recurrent heart attacks, and help increase life expectancy.
In some patients, blood pressure levels after a heart attack are pathologically low. This phenomenon is often observed in the postoperative period. The reason lies in:
- impaired blood circulation in the coronary arteries;
- loss of elasticity of vascular walls;
- insufficient blood supply to a certain area of the heart muscle.
Against the background of low pressure and irreversible changes in the myocardium, the patient experiences: weakness, dizziness, yawning, slow heart rate, constant feeling of cold in the arms and legs.
In such cases, it is advisable to take hypertensive medications or revise the treatment regimen: it is possible that previously prescribed medications cause an excessive decrease in pressure.
Critically low pressure after myocardial infarction (below 60 mm Hg) may indicate a recurrent attack and requires immediate medical attention.
Another phenomenon, called decapitated hypertension, is observed in some patients who have had a heart attack. Normal or slightly elevated systolic (upper) pressure is combined with high diastolic (lower) pressure, and ranges from 130-140/90-100 mm Hg. Pathology indicates low contractile activity of the myocardium and high tone of peripheral vessels.
Changes in blood pressure after a heart attack
During a heart attack, the increase in pressure occurs gradually and rarely reaches critical values. It is not advisable to rely on tonometer readings to diagnose a heart attack - high blood pressure does not always indicate the development of this dangerous condition, and at the same time, a heart attack is not always accompanied by a noticeable increase in blood pressure.
If the increase in blood pressure during a heart attack is not critical, then pressure after a myocardial infarction requires qualified care and observation in a hospital, especially in patients with hypertension. This is due to the fact that after a heart attack the pressure always decreases. In this case, the decrease can occur either gradually or sharply. Low blood pressure persists for a long time; this indicator will not return to normal on its own, so drug therapy is used to normalize blood pressure, but only in a hospital and under the supervision of medical personnel.
The drop in pressure after a heart attack is caused by two factors - disruption of the heart muscle and changes in vascular tone. At the same time, against the background of a decrease in pressure, the pulse rises to values close to normal. In some cases, in men who have suffered from hypertension for a long time, the pressure after a heart attack remains within normal limits, without sudden jumps. If, after suffering an attack, the pressure stabilizes a few days later, this is considered a positive change and gives a good chance for a quick restoration of the functioning of the cardiovascular system.
The danger of low blood pressure is characterized by risks of loss of consciousness, lack of oxygen, and migraines.
What is the pressure during a heart attack?
Pressure during a heart attack is an important diagnostic criterion. However, it is impossible to give an unambiguous answer to the question of what pressure and pulse during a heart attack without taking into account the phase of the disease and the patient’s initial, i.e., blood pressure preceding the attack.
Myocardial infarction is the formation of a necrosis focus in the area of the heart muscle, the development of which is associated with relative or absolute insufficiency of coronary blood flow. This is a very serious, life-threatening disease. Up to 50 years of age, a heart attack affects men several times more often, and at an older age it can occur with equal frequency in both men and women.
Its prognosis largely depends on the timeliness of medical care provided. Therefore, every person should know the first signs of myocardial infarction, including whether there can be normal blood pressure (blood pressure) with this cardiovascular pathology.
Differences in symptoms between men and women
Symptoms of an attack vary between men and women. Despite the fact that women are less likely to experience a heart attack, more often the attack ends in death. In approximately half of heart attacks in women, the patient dies. This is due, first of all, to the late diagnosis of the attack. Unlike men, heart attacks among women are in most cases characterized by nonspecific symptoms. As a result, the patient does not see a doctor and death occurs a few hours later.
Women are less likely to have heart attacks, but they have a higher mortality rate
Men recover better and faster after an attack. Specific symptoms of a heart attack in this case allow you to promptly suspect a dangerous disorder and call an ambulance.
It is important to remember the symptoms of an attack that are typical for women:
- dyspnea;
- lack of oxygen;
- pain in the upper abdomen;
- neuralgic pain around the chest;
- disorientation and dizziness.
To accurately diagnose a heart attack in women, a thorough examination is necessary. The risk group includes patients with cardiovascular pathologies, as well as obese women. The average age of patients who have suffered a myocardial infarction is 60-67 years.
What is the pressure during a heart attack and what does it depend on?
Hypertension, i.e. a pathological condition in which the patient often or constantly has arterial hypertension, is a risk factor for the development of myocardial infarction. Of particular danger is a sharp decrease in significantly elevated blood pressure (for example, during a hypertensive crisis). However, during myocardial infarction, pressure fluctuations are also observed in patients who have not previously suffered from arterial hypertension.
Normally, blood pressure in adults (men and women) should not exceed 140/90 mm. rt. pillar With a sharp and significant increase in it, a spasm of blood vessels occurs and the blood flow through them significantly worsens.
At the beginning of an acute heart attack, blood pressure usually rises, but after 20-30 minutes it drops, sometimes very strongly, to the point of developing vascular collapse and cardiogenic shock.
Why does blood pressure rise and fall during a heart attack?
High blood pressure is one of the common causative factors underlying impaired blood flow in the coronary artery system. But even if the patient did not have arterial hypertension, elevated blood pressure is characteristic of the onset of a heart attack and persists in the first minutes after a heart attack. This is due to significant irritation of pain receptors, the release of so-called stress hormones (adrenaline, norepinephrine) into the blood, which have a vasopressor effect, that is, an increase in blood pressure.
However, the high blood pressure begins to decrease quite quickly. This is due to the fact that as a result of the resulting focus of necrosis, the contractility of the heart muscle is impaired to one degree or another and cardiac output decreases. In turn, due to a decrease in cardiac output, a whole group of endogenous substances enters the patient’s blood:
- myocardial inhibitory factor;
- lactic acid;
- leukotrienes;
- cytokines;
- thromboxane;
- bradykinin;
- histamine.
Of particular danger is a sharp decrease in significantly elevated blood pressure (for example, during a hypertensive crisis).
These substances further reduce the contractile function of the heart, which becomes the main cause of the development of cardiogenic shock - a dangerous complication of myocardial infarction. Its main features:
- arterial hypotension (systolic blood pressure equal to or less than 80 mm Hg);
- decrease in pulse pressure to 20 mm Hg. Art. or less;
- rapid pulse of weak filling;
- lethargy up to complete loss of consciousness;
- impaired peripheral circulation (pallor and/or marbling of the skin, decreased skin temperature, acrocyanosis);
- oligoanuria (decrease in diuresis to 20 ml/h or less).
It should be understood that high or low blood pressure in itself is not a sign of myocardial infarction. Also, labile pressure (“jumps” in blood pressure) cannot be considered as a symptom of this disease.
A significant drop in blood pressure during a heart attack in women and men is an unfavorable prognostic sign and indicates an extensive focus of necrosis and the development of cardiogenic shock.
How does blood pressure change during a heart attack?
The likelihood of developing a myocardial infarction increases in old age, but an attack can also occur in young men and women. If physical activity is accompanied by discomfort in the heart area, you should consult a doctor, as this indicates angina pectoris preceding a heart attack.
The first manifestation of an attack is hypertension. A decrease in pressure is observed after severe chest pain. In this case, you should call an ambulance and monitor your blood pressure.
During a heart attack, a lack of contraction of the left and right ventricles develops. This condition is accompanied by pressure surges. It starts to fall, then quickly normalizes and rises. The pressure decreases during myocardial infarction after a small jump upward.
To assess the patient's condition, the doctor needs information about the patient's performance under normal conditions. The development of an attack is indicated by symptoms in the form of:
- blanching of the skin;
- decrease in body temperature;
- nausea and vomiting;
- cold sweat;
- involuntary bowel movements;
- cold sweat.
The main sign of a heart attack is severe chest pain, radiating to the arm, shoulder, neck, and jaw.
The more the patient knows about the pressure and pulse during a heart attack, the greater his chance of saving his life by promptly informing doctors about the cause of his illness. It happens that people with a very high pain threshold died from a heart attack right in the process of their daily activities, which were not interrupted until the last moment.
If you suspect a heart attack, it is more important not so much to detect the indicators as to track the dynamics of rise and fall. In most cases, blood pressure readings during a heart attack look like a sharp jump up without any reason. Then, when the patient experiences an attack, the pressure begins to drop rapidly, which is no more beneficial for the body.
How does myocardial infarction develop?
Myocardial infarction is one of the most severe acute forms of coronary heart disease (CHD).
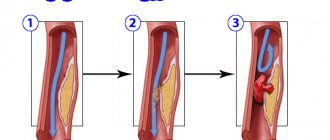
In the vast majority of cases, the direct cause of myocardial infarction is atherosclerosis of the coronary arteries - the vessels through which blood flows to the heart muscle. With atherosclerosis, lipid metabolism is disrupted in the patient's body. This leads to the deposition of cholesterol in the form of plaques on the walls of the arteries. Gradually, cholesterol deposits are saturated with calcium salts and increase, creating an obstacle to blood flow. In addition, platelets attach to the surface of atherosclerotic plaques, leading to the gradual formation of blood clots.
During myocardial infarction, pressure fluctuations are also observed in patients who have not previously suffered from arterial hypertension.
Atherosclerosis is a systemic disease, that is, it affects all blood arterial vessels. However, in different people, different vessels are susceptible to it to a greater or lesser extent. Myocardial infarction is usually preceded by atherosclerosis of the coronary vessels, and stroke is preceded by atherosclerotic lesions of the cerebral vessels.
Normally, blood pressure in adults (men and women) should not exceed 140/90 mm. rt. pillar With a sharp and significant increase in it, a spasm of blood vessels occurs and the blood flow through them significantly worsens. And if the lumen is blocked by an atherosclerotic plaque, then blood flow can completely stop. As a result, the area of the heart muscle supplied by this vessel ceases to receive nutrients and oxygen along with the blood. Clinically, this is manifested by the patient experiencing an acute attack of pain in the chest area, i.e., an attack of angina. If coronary blood flow is not restored within 30 minutes from its onset, irreversible processes begin in the affected area of the myocardium, leading to its necrosis.
Symptoms of myocardial infarction
Myocardial infarction often occurs in the morning. This is due to the fact that at this time there is an increase in the secretion of catecholamines (hormones of the adrenal cortex), which increase blood pressure. The patient suddenly develops unbearable pressing pain in the left half of the chest or in the chest area, lasting over 25-30 minutes and not relieved by taking nitroglycerin. The pain may radiate to the left arm, throat, lower jaw, back or epigastric region. Characteristic signs of the disease are anxiety, restlessness and fear of death.
It should be understood that high or low blood pressure in itself is not a sign of myocardial infarction. Also, labile blood pressure cannot be considered a symptom of this disease.
Myocardial infarction is often accompanied by the development of shortness of breath, profuse sweating, and severe pallor of the skin. In almost all cases, certain heart rhythm disturbances are noted (bradycardia, extrasystole, tachycardia), some of which are described by patients as an attack of strong heartbeat.
First aid for myocardial infarction
If a person suddenly experiences severe heart pain, he should immediately receive first aid. The algorithm of actions in this situation is as follows:
- call an emergency medical team;
- lay the patient down (if he loses consciousness, turn his head to the side);
- give him a Nitroglycerin tablet under the tongue if the pain does not go away and the systolic blood pressure exceeds 100 mm Hg. Art., then after 15-20 minutes you can give the medicine again;
- ensure a flow of fresh air (open the window, unbutton the collar);
- try to calm the patient;
- before the arrival of doctors, monitor basic vital functions (pulse rate, breathing);
- in the event of clinical death, immediately begin resuscitation measures (indirect cardiac massage, mouth-to-mouth artificial respiration), which should be carried out either until the patient regains spontaneous breathing and heart rate, or until the ambulance arrives and the doctor declares biological death.
According to medical statistics, about 10% of patients with myocardial infarction die in the prehospital stage. At the same time, correctly provided first aid can save a person’s life.
First aid
If signs appear that resemble a heart attack, the victim needs to remove his belt and unfasten his collar to make it easier for him to breathe. If the patient is indoors, open a window and immediately call emergency services.
To prevent a person from experiencing the fear of death that arises during an attack, he is calmed down and given nitroglycerin under the tongue. After 10 minutes, the medication is repeated. To prevent the blood from thickening, the patient needs to take Acetylsalicylic acid; any analgesic that is at hand is suitable to reduce pain.
Valerian or Corvalol drops help reduce the heart rate and eliminate fear. Before the ambulance arrives, you need to measure your blood pressure. No other actions can be performed until the doctor arrives.
Prevention
Myocardial infarction is a very serious disease, from which it is no longer possible to fully recover, since part of the cardiac function is irretrievably lost with the death of a section of muscle. Therefore, it is very important to try to prevent its occurrence.
Myocardial infarction often occurs in the morning. This is due to the fact that at this time there is an increase in the secretion of catecholamines, which increase blood pressure.
In fact, preventing cardiovascular diseases is quite simple and consists of maintaining a healthy lifestyle. This concept includes a number of measures.
- Rejection of bad habits. It has long been proven and there is no doubt that alcohol and nicotine have a negative effect on the condition of the heart and blood vessels and worsen their functions.
- Proper nutrition. The diet should limit the content of fats (especially animal origin) and light carbohydrates. You should consume enough vegetables and fruits daily. Properly organized nutrition allows you to normalize metabolism, therefore reducing the risk of developing atherosclerosis, type II diabetes, and obesity.
- Monitoring blood pressure levels. If a patient suffers from arterial hypertension, it is necessary to regularly measure blood pressure levels and carefully take antihypertensive drugs prescribed by a therapist or cardiologist. In addition, fatty, hot, spicy and salty foods should be completely excluded from the diet, or at least sharply limited.
- Fighting physical inactivity. This includes daily walks, morning exercises, and physical therapy classes.
- Complete rest. Both physical and psycho-emotional overload should be avoided. A good night's sleep is very important. An annual wellness holiday in a sanatorium or dispensary is recommended.
Prevention of recurrent disease
It is easier to prevent a disease than to treat it – this axiom directly applies to heart diseases. To prevent anything irreparable from happening, you should:
- quit smoking and alcohol;
- actively spend your free time (fitness, swimming, hiking);
- eat foods rich in vitamins;
- exclude fatty, salty, sweet, smoked, fried, and semi-finished products from the diet;
- get rid of excess weight;
- control chronic diseases;
- Visit a cardiologist regularly.
Maintaining the correct principle of life will relieve problems with the heart and blood vessels. Timely medical assistance during an attack will save health and life.