Causes and methods of eliminating them
Breathing problems, along with a rapid heartbeat, can develop for various reasons.
If shortness of breath occurs, a person will not necessarily begin to choke, because his body can try to eliminate the lack of air by increasing the heart rate. This often happens when working with breathing apparatus, carbon monoxide poisoning and a fairly rapid rise to altitude. Thus, among the most common causes of breathing problems and rapid heartbeat, it is worth highlighting:
- physical stress;
- psycho-emotional stress;
- lack of oxygen due to external factors.
Such problems arise reflexively, do not pose any particular danger and most often go away without medical intervention.
Often, an attack of tachycardia and breathing problems are observed in people who are overweight, as a reaction to physical overexertion.
First aid
With pathological shortness of breath, failure of breathing can overtake a person even at rest, without the influence of any external factors on the body. In this case, the patient usually needs first aid to stabilize breathing.
Standard actions for an attack of tachycardia and shortness of breath include:
- Take a half-sitting body position. The legs should be lowered down.
- Calm down. Panic will only make the situation worse.
- Loosen clothes. Unfasten or remove anything that prevents you from breathing freely.
- Make sure there is sufficient ventilation in the room. If necessary, open windows or use special items such as an oxygen tank.
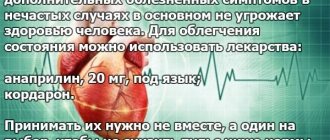
- To take medicine. To eliminate palpitations, you can use nitroglycerin tablets and cardiac glycosides.
Often a person is able to provide such help to himself. In case of particularly severe attacks, you will need to call an ambulance.
Coronary heart disease and heart failure are more often the causes of this condition of the body. In the first case, tachycardia develops due to disruption of the patency of the coronary vessels due to atherosclerosis. In the second case, due to the inability of the heart to maintain the level of blood supply necessary for the body.
Increased heart rate and breathing problems with brain damage are observed due to the localization of control centers of all organs and parts of the body in it. This happens in most cases for the following reasons:
- head injury;
- stroke;
- tumor;
- encephalitis.
Along with tachycardia and heavy breathing, with such problems with the body, neurological symptoms such as dizziness, paralysis, disruptions in the cognitive system, and so on are also noticeable.
The possibility of recovery from such brain disorders depends on the degree of damage to the organ and the effectiveness of the treatment provided.
In this case, therapy depends on the cause of such a disorder. Often, drug treatment is combined with surgical intervention. Problems with the nervous system are relieved with various sedatives.
Breathing problems and rapid heartbeat can also occur for other reasons: vegetative-vascular dystonia, intervertebral hernia, intercostal neuralgia, osteochondrosis.
Quite often, when moving, such problems only get worse. Anti-inflammatory drugs together with therapeutic exercises help well in cases of such diseases.
Due to physical overexertion and stress, disruptions in the functioning of the respiratory system during tachycardia often occur in older people.
Pregnant women also often suffer from similar dysfunctions of the body. This is explained by physiological factors. In this case, in addition to drug intervention, the symptoms that arise can be eliminated through lifestyle correction.
Tachycardia in adolescents
Heart disease, contrary to popular belief, can occur in people of different ages. One can argue for a long time about what caused such a disastrous trend, but the facts do not change. One of the most unpleasant ailments is tachycardia in adolescents. A rapid heartbeat is very harmful to a growing body. Tachycardia can sometimes occur in children. This may be a consequence of excessive physical exertion or extreme anxiety. But if it occurs suddenly at rest, then it is necessary to show the child to the doctor.
Reasons for the development of the disease
Tachycardia is characterized by a rapid heartbeat. It can develop in a teenager due to the influence of various factors. Most often, they are all united by the physical characteristics of the child. In children aged 13-16 years, an increase in heart rate and blood pressure may occur due to rapid growth. As a rule, the heart grows faster with this anomaly. It reaches the size of an adult, but the vascular system remains “childish”. As a result, a slight osmotic imbalance occurs, which leads to increased heart rate.
If a child is externally physically developed, of average or tall height, proportional, then his tachycardia may indicate cardiac hypertrophy. In children of short stature and thin build, the organ may be too small, so it works more actively. This leads to the appearance of tachycardia. In the latter case, attacks of rapid heartbeat will be accompanied by headaches, rapid fatigue and shortness of breath. Also, the reasons for the formation of the disease include:
- great physical activity;
- a state of constant emotional overstrain;
- presence of problems in the functioning of the endocrine system;
- anemia of various types;
- congenital pathologies in the structure of the heart and vascular system.
Separately, doctors consider sinus tachycardia. It develops in children aged 12-16 years for organic and physical reasons. Sinus rhythm in this disease remains normal, but other indicators change. There is a direct connection between the development of this form of the disease, the situation in the family and the child’s lifestyle. Sinus tachycardia is formed for the following reasons:
- severe stress and emotional distress;
- rapid physical development;
- diseases of the endocrine system;
- experiencing emotionally difficult situations;
- excessive physical activity.
Therefore, it is recommended to bring your child to the clinic every year for a full medical examination. In 90% of cases, this type of tachycardia occurs without symptoms. This means that the disease is temporary and is not accompanied by any organic changes. But if tachycardia is not diagnosed in time, it can provoke the development of certain pathological conditions, so parents should periodically measure their child’s pulse. If its frequency is more than 90, then this is a reason to consult a cardiologist.
Some children aged 11-15 years develop paroxysmal tachycardia. With this disease, the heart rate increases to 160 beats. The attack itself lasts only 3 minutes. Doctors associate the development of this disease with disorders in the formation of the nervous system. This is due to problems during pregnancy. Various infections and injuries adversely affect the condition of mother and child. This type of tachycardia manifests itself in withdrawn children living in constant fear. In a state of anger, such a child will not be able to control himself.
Symptoms
Almost all children suffering from one of the types of tachycardia exhibit the following symptoms:
- attacks of rapid heartbeat, accompanied by strong vibrations of the chest;
- rapid fatigue;
- problems with concentration and attention;
- pain in the chest and under the shoulder blade;
- severe shortness of breath and oxygen deficiency after light exercise;
- attacks of darkening in the eyes;
- development of pre-fainting states.
It is not necessary for a child to exhibit all of these symptoms at once. The appearance of rapid heartbeat and chest pain is enough to contact a cardiologist. You should not delay your visit to the doctor, because... in addition to the reasons listed above, tachycardia may be a symptom of a tumor or other ailment.
Diagnostics
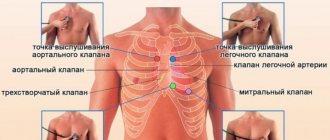
You should visit a cardiologist immediately after you notice a rapid heartbeat in your child. In guys, the appearance of this disease may be associated with the physiological characteristics of the development of the body, but you still need to undergo an examination. The following methods are used to diagnose the disease:
- Ultrasound;
- echocardiography;
- ECG;
- electrocardiography;
- electrophysiological study.
The patient will need to describe in detail the symptoms he experienced and the time when they appeared. If the child has suffered from any disease before the onset of tachycardia, additional diagnostic methods are used to exclude complications. Echocardiography of the heart is considered the most accurate. It allows you to detect hidden pathologies in the structure of the organ.
Treatment
The doctor’s recommendations depend on the type of tachycardia and the reason that triggered its development. If the illness occurs after the flu or another infection, a course of antibiotics and vitamins is prescribed to finally rid the patient of the pathogen. In case of problems with the functioning of the endocrine system, the patient may be prescribed a course of hormonal medications. You cannot prescribe medications to your child yourself. Valerian, motherwort, validol and other “harmless” medications can cause other problems.
In 86% of cases, tachycardia does not require any drug treatment. It is enough to adjust the work and rest schedule, balance the diet, and introduce physical exercise into daily practice. If a child is exposed to severe emotional stress at school due to the behavior of classmates, he should consult a psychologist or change educational institution. You should temporarily reduce the time spent on the computer, TV and smartphone. Leisure time should be spent calmly, devoting it to reading, playing musical instruments, etc.
Dyspnea in heart failure, the treatment of which is complicated by the underlying disease
If the heart cannot cope with the load, shortness of breath occurs. In the vessels of the lungs, blood flow slows down and pressure in the arteries increases, resulting in spasm of the arterioles. Naturally, gas exchange is disrupted.
You can describe in more detail the pattern of development of shortness of breath in heart disease:
- If the left parts of the heart are affected, then the volume of cardiac output decreases and blood stasis forms in the lung area.
- Congestive manifestations disrupt the gas exchange of the respiratory tract, which causes a failure in their ventilation.
- To normalize breathing, the body increases the depth and frequency of breaths. This is how shortness of breath develops.
Almost all cardiovascular pathologies are accompanied by shortness of breath of various types:
- In older people, lack of air occurs due to ischemia and arterial hypertension.
And since there is a correlation between hypertension and excess weight, in obese patients with constantly high blood pressure, shortness of breath is present not only during exercise, but also at rest, and even at night.The sleep of such people is disturbing and is often interrupted by apnea.
- Myocardial infarction and its asthmatic variant have all the signs of left ventricular failure. There is hoarse breathing with shortness of breath and even suffocation.
- All chronic heart lesions are accompanied by nocturnal shortness of breath.
- Cardiac asthma causes a lot of suffering.
- Pulmonary edema is very dangerous and can be fatal.
- Thromboembolism, which causes respiratory failure, generally cannot exist without shortness of breath and suffocation.
How to determine that shortness of breath is cardiac? This shortness of breath has specific symptoms that you need to know:
- Inhalation is very difficult.
- Occurs and intensifies under any load.
- Occurs in a lying position. The horizontal position forces the heart to work harder. If you sit down, your breathing will normalize.
How to relieve attacks and how to treat shortness of breath in heart failure, what pills are prescribed by specialists for this? To eliminate it, you should act on the cause, which is heart failure.
It is imperative to conduct a thorough diagnosis to help find the root cause of the disease - high blood pressure, coronary artery disease or congenital heart disease.
Tachycardia, the symptoms of which are varied, affects a person’s overall health. The disease must be monitored and consulted with a doctor. Not only an increased pulse is a sign of tachycardia. What are the main symptoms of this type of disease?
- Feeling of pain and heaviness in the area of the heart muscle.
- Lack of air, weakness and shortness of breath, frequent dizziness.
- Fatigue, loss of appetite, insomnia and high body temperature.
- Tachycardia is manifested by decreased performance and deterioration of health.
- Increased heart rate along with angina attacks, worsening heart failure.
- Disorders of the blood supply to organs and tissues.
- Focal disorders of the nervous system, seizures.
- Decreased blood pressure, decreased diuresis.
- The patient may experience cold extremities.
We suggest you read: Sinus tachycardia description of ECG - All about hypertension
The symptoms should alert anyone who develops them. If not only your pulse has increased, but also your temperature, and you also feel unwell, you will need to call an ambulance to get qualified specialist help. You need to try to remove all the symptoms of the disease in order to feel good and not aggravate your condition.
Stressful situations
A condition called shortness of breath is characterized, first of all, by a violation of the normal depth and frequency of breathing - a person has a feeling of severe lack of oxygen. Some people in this state begin to panic and try to find a way out of the current situation as quickly as possible. And there is only one solution - you just need to calm down and understand that stress with almost 100% probability cannot lead to a person suffocating.
Feeling short of air
The mechanism for the development of the problem in such situations is as follows: under the influence of a stress factor or strong emotional shock, a large amount of adrenaline is released into the blood. This leads to overstrain of the respiratory system, which provokes a decrease in the efficiency of breathing, but does not cause it to stop completely.
In a state of panic, when a lack of air is felt, a person begins to literally “swallow” it, directing it not into the lungs, but into the stomach. Many people also forget to exhale, which only makes matters worse and increases panic.
State of panic, palpitations, shortness of breath
Another reason for shortness of breath in stressful situations and severe emotional states is muscle spasm. Under the conditions being studied, the brain gives the muscle system a command to prepare for possible danger. The muscles of the pharynx become tense, among other things. Because of this, the feeling known to every person as “a lump in the throat” arises.
Feeling of a lump in the throat
This phenomenon does not pose a serious danger - the human body cannot suffocate itself.
Associated symptoms
Dyspnea after tachycardia has certain accompanying symptoms. The most common ones include:
- weakness;
- increased sweating;
- swelling of the legs;
- blue skin;
- dizziness;
- chest pain;
- sense of anxiety.
With severe heart failure, pulmonary edema may develop, which is characterized by its own symptoms:
- increase in the size of neck vessels;
- increased breathing;
- blue face;
- cough that produces frothy sputum.
Coronary heart disease as one of the causes of shortness of breath and excessive sweating
This disease is quite widespread among older people. The pathology has a number of characteristic symptoms. Among them the following can be noted:
- Dyspnea;
- Weakness;
- Pain in the heart of an angina nature;
- Increased sweating;
- Labored breathing;
- Nausea without vomiting.
Pathology can be suspected by the presence of angina pectoris. It is considered one of the earliest symptoms of this disease. This disease requires immediate treatment.
Tachycardia: occurring in the morning
When a person wakes up or gets out of bed after sleep, his pulse may increase sharply and very mild nausea may appear. This occurs due to the fact that the position of the body changes, the heart begins to work actively after a state of maximum rest.
To avoid tachycardia in the morning, do not immediately get out of bed. After waking up, lie in bed for a while so that your heart does not get a lot of work right away. Treatment for this type of arrhythmia is not required, just watch your rhythm of life.
What diagnostics are needed?
When, after tachycardia, it becomes difficult for a person to breathe, this is a reason to go to the hospital. After the examination, the attending physician may prescribe a series of examinations to identify the cause of the problem. The main ones include:
- general blood and urine analysis;
- electrocardiogram;
- radiography;
- ultrasound examination of the heart;
- magnetic resonance and computed tomography.
Based on the results of the examinations completed, the doctor makes a diagnosis and prescribes treatment or, if necessary, redirects to the appropriate specialist.
Rapid heartbeat with high blood pressure: what to do and take
It is not surprising that the heart rate also increases with high physical activity. Tachycardia associated with high activity is also directly intertwined with breathing.
If you like to do various exercises and train, you need to learn all the nuances of proper breathing techniques. When you exercise, inhale and exhale according to the rules.
When exercising, your breathing must be fine, otherwise your pulse will constantly fluctuate and your body temperature will rise. Of course, such tachycardia is not particularly dangerous for your health, but during physical activity you need to control the training process so as not to aggravate the situation.
Treatment of tachycardia directly depends on the cause of its immediate occurrence. Any therapy should be carried out by an experienced specialist. First you need to remove all the factors that provoke the pulse to rise:
- Drinks that contain caffeine.
- Nicotine and alcohol, spicy foods, chocolate.
- Protect the patient from unnecessary physical activity.
Treatment will require consultation with a neurologist. You will be prescribed sedatives and psychotherapy. If you do not follow all the recommendations, your heart rate will not stabilize and will cause other heart diseases.
Symptoms of tachycardia are individual, therefore their treatment should be selected so as to fully correspond to the characteristics of the patient’s body. The disease is unpleasant, since an increased pulse causes discomfort in every person. If treatment is timely and effective, the disease will not worsen, and its symptoms will leave you.
Of course, there is also an alternative treatment for tachycardia, but it is appropriate only after consultation with your doctor. Sometimes all sorts of different herbs and infusions harm the heart, disrupting its rhythm and activity even more. You should not engage in active self-medication, since proper consultation and treatment methods are the key to successful recovery from the disease.
The heart is the leading organ in the human circulatory system. The health of the latter depends on its uninterrupted and coordinated work.
This organ works throughout life. It can contract and expand 50 to 150 times per minute. During contraction, blood flows in and out. A healthy organ contracts exactly the same number of times per minute.
During contraction, blood enriched with nutrients and oxygen flows to other organs. The contraction process is the heart rate.
If a malfunction occurs in the heart, this will indicate that there are some problems in the organ. Therefore, it is important to prevent such failures. Identify and treat them in a timely manner.
The heart of a healthy person can beat 60 to 80 times per minute. If the contraction frequency is more than 90 times per minute, this will indicate tachycardia.
In this case, contractions and heart function will be normal, but the rhythm will be rapid. Tachycardia can come and go suddenly. Attacks can last from several minutes to several hours or days.
Typically, heart problems occur in the fairer sex, as they are more emotional and temperamental. Also, such symptoms can appear in those who often have mood changes, are active, and are prone to anxiety and depression.
Experts note that palpitations are not a disease in themselves. It only indicates that a person has some kind of disease.
Causes of tachycardia
There can be many of them. Here it is important to learn to separate tachycardia, which can appear from physical stress on the body, fear or stress, from pathological one.
The first is considered a normal reaction of the body to stress. The second can also manifest itself when a person is in a calm state.
The last manifestation already indicates that the body has a disease of some systems or organs. Also, a rapid heartbeat can appear when a person leads an unhealthy lifestyle and does not give the heart regular exercise for a long time. The latter can cause heart failure.
Internal and external factors of tachycardia:
- Using drugs that stimulate the nervous system.
- Abuse of coffee.
- Insomnia.
- Constant stress.
- Drinking alcohol in large quantities.
- Overwork of the body.
- Heavy weight.
- Indiscriminate use of certain types of medications.
- Large overloads of the body physically.
- High blood pressure.
- Diseases, for example, ARVI.
If there is an insufficient amount of magnesium or calcium in the body, this can also cause tachycardia.
When you are sick and have a high body temperature, a rapid heartbeat may also occur. Each degree above normal increases the heart rate by 10 beats per minute.
We suggest you read: Is ginger useful or not for hypertension • How to cure hypertension
The mechanism of cardiac activity is also negatively affected by those professions where you have to work hard physically, where there are emotional problems, frequent stress and other typical situations.
Eating large amounts of chocolate will also have a negative effect on the body.
Experts identify the following causes of tachycardia:
- Appeared as a result of the presence of other diseases (coronary heart disease, heart disease, myocarditis, cardiomyopathy).
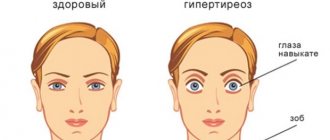
- Hormonal and endocrine disorders in the body (thyroid diseases, menopause in women, benign and malignant tumors).
The heartbeat may become faster when there is high blood pressure. We must also remember that the body reacts in this way to various disorders. In this case, only a specialist can determine the disease after an examination.
If attacks are accompanied by:
- chest pain
- darkening in the eyes,
- dizziness,
- loss of consciousness
- weakness,
- shortness of breath,
this indicates that paroxysmal tachycardia is occurring. Such symptoms are explained by the lifestyle that a person leads (drinking alcohol, smoking, taking drugs, etc.).
Another cause of tachycardia is arrhythmia. There are many types of it. The most common is atrial fibrillation. In this case, the heart will contract frequently, but irregularly.
This disease occurs more often in elderly people with coronary heart disease. But if there is a congenital predisposition to arrhythmia, then it can occur in anyone and at any age.
In order to accurately make a diagnosis in a particular case, it is necessary to conduct many additional examinations of the person, as well as to be constantly observed by a doctor.
If there is tachycardia:
- dizziness,
- weakness,
- dry and pale skin,
- fast fatiguability,
Anemia may be the cause. This is characterized by a decrease in the level of hemoglobin in the blood. This can often be found during pregnancy or after childbirth.
Another cause of anemia can be leukemia. In this case, you need to do a blood test, which will immediately confirm the diagnosis.
Before making a residual diagnosis, it is necessary to determine what type of tachycardia the patient has. She may be:
- Chronic.
- Paroxysmal.
In the first case, characteristic symptoms in a person will be observed constantly or appear after a certain, uniform period of time. The second type can appear only once, unexpectedly.
When tachycardia appears, the patient will either have a strong heartbeat, when it will seem that the heart is audible, or it will beat very quietly. At this time, the person will find it difficult to breathe, he will panic, his vision will darken, he will become scared and hot.
You may feel a tingling sensation in your body, heart pain, trembling in the body, it will be painful to strain and laugh. Your head will start to hurt and feel dizzy. Insomnia will occur. All these are signs of tachycardia.
Signs:
- Cramps.
- Loss of consciousness.
- Pain in the chest area.
- Low pressure.
- Shortness of breath and suffocation.
During treatment, an important role will be played by the environment in which the person is located, the absence of stress, loud sounds, stress on the body, a certain daily routine and nutrition.
Diagnostics
Basic methods:
- Holter ECG monitoring.
- Electrocardiogram.
- Electrophysiological study.
- Echocardiography.
Sometimes your doctor may prescribe bicycle ergometry. At this time, the patient is observed while on an exercise bike.
Additionally, blood pressure may be measured, the thyroid gland will be examined for hormones, and general urine and blood tests may be taken.
In the event that a person feels that his heart is beating too strongly or weakly, he should observe himself and the behavior of his body. This must be done in order to collect the maximum amount of information required by the doctor to make a diagnosis.
Attention must be paid to:
- Frequency of attacks.
- Their duration.
- Time of manifestation.
During an attack, you should measure your pulse. You also need to think about what could lead to the symptoms. Perhaps it was some situation in life or taking certain foods/drinks or medications.
When you need to urgently call a doctor for help:
- The heart suddenly began to beat strongly, the blood pressure rose, there was fear, a headache, etc.
- The attack happened for the first time.
- There are heart diseases, thyroid diseases, diabetes, chronic diseases, during pregnancy, if close relatives have had such problems, during recovery from some illness.
After the diagnosis, the specialist will be able to make the correct diagnosis and prescribe treatment.
It happens that neither tests nor other examinations can show any signs of disruption of the heart, but palpitations are still present.
In this case, you need to pay close attention to your previous lifestyle and change it, try to avoid stress, and not eat foods that can provoke the appearance of tachycardia.
The question of what to do with rapid heartbeat and high blood pressure is of interest to many who suffer from these symptoms. To determine the most optimal treatment method, you need to consult a specialist, take tests and undergo all the required procedures. If the tests are negative, this indicates that the rapid heartbeat and high blood pressure are due to secondary tachycardia.
Causes of tachycardia
What does the heart lack?
Chronic heart failure is a common disease in people over 60 years of age. It is fraught with a fatal risk, so the problem of its diagnosis and treatment deserves the closest attention. The doctor is always faced with the task of figuring out why a person has such an illness.
Three symptoms: shortness of breath, weakness and fatigue
Recently I accidentally met a friend of mine who suffered a myocardial infarction six months ago. I knew that she had a heart attack suddenly, at work, from where she was hospitalized by ambulance straight to the intensive care unit of the hospital. Before the heart attack, the woman did not suffer from angina, did not consult a cardiologist, and always considered herself healthy. In the hospital, she underwent coronary angiography and, having discovered pronounced changes in one of the coronary arteries, was offered stenting - widening the narrowed artery using a special device that is inserted into it through a vascular catheter. But the woman categorically refused surgical treatment.
When we met, I noticed her shortness of breath. In addition, she complained to me about swelling of her legs, weakness, fatigue and frequent attacks of palpitations. It became clear to me that there was chronic heart failure, which developed in a woman after a myocardial infarction in the absence of the necessary treatment.
Chronic heart failure is not an independent disease, but a sad result of many other serious illnesses: heart attack, hypertension, myocarditis, cardiopathy, valvular heart disease, thyroid diseases and a number of others. Congestive heart failure means that the heart cannot pump the full volume of blood to meet the body's vital needs.
There are three main signs of heart failure: shortness of breath, weakness and fatigue. These are the complaints that patients most often present with. Along with this, they may be bothered by rapid heartbeat, interruptions in heart function, swelling of the legs and feet, and heaviness in the right hypochondrium. Meanwhile
None of these symptoms is 100% proof of heart failure. Therefore, when making a diagnosis, cardiologists never rely only on patient complaints or even clinical data.
I remember one of my patients, Marina. This 50-year-old woman experienced shortness of breath when walking up a short flight of stairs. She quickly got tired, felt weakness, heaviness in the right hypochondrium. Such symptoms did not arise by chance - for many years the patient suffered from severe hypertension and varicose veins. In addition, she was experiencing menopause and at the same time continued to work hard. In a word, even without heart failure she had reasons to feel unwell.
While examining the patient, I noticed the blueness of her lips and swelling of her legs and feet, and noted an increase in the size of her liver. And she suggested that she go to the cardiology department for an examination to confirm that her health problems were related specifically to heart disease.
Four stages and four classes
In clinical practice, heart failure is often characterized according to the severity of clinical symptoms. According to the domestic classification of circulatory failure, developed in 1935 by cardiologists V.Kh. Vasilenko, G.F. Lang and N.D. Strazhesko distinguishes acute and chronic heart failure and three stages of chronic circulatory failure.
Stage I – shortness of breath and fatigue appear only with significant physical exertion.
Stage II A – signs of circulatory failure occur during normal physical activity.
Stage II B – pronounced signs of heart failure appear at rest.
Stage III is a dystrophic stage with severe hemodynamic disturbances, metabolic disorders and irreversible changes in the structure of organs and tissues.
In specialized hospitals, the New York classification is also widely used, which distinguishes four functional classes of circulatory failure according to severity:
1st class – no subjective complaints;
2nd class – complaints during significant physical exertion;
3rd class – complaints with minor physical activity;
4th grade – the appearance of complaints at rest.
Correct diagnosis
To determine what stage of chronic circulatory failure is and what class it belongs to, it is necessary to perform a set of examinations: first of all, do a biochemical blood test, ECG and chest x-ray. But to accurately diagnose heart failure itself, you need to do echocardiography. It is a mainstream method and has been called the “Queen of Evidence” for its ease of implementation, safety, and ubiquity.
Echocardiography (ECHOCG) - ultrasound examination of the heart - makes it possible to clarify the very fact of cardiac dysfunction, its nature and hemodynamic state. It allows you to look inside the heart and major vessels and see how efficiently the heart works. The main indicator of heart failure according to echocardiography is the ejection fraction, which reflects the pumping function of the left ventricle. Normally, this figure should be 50% or more, that is, at least 50% of the blood in the left ventricle should enter the aorta during its contraction.
In my patient Marina, an echocardiographic study revealed a significant increase in the size of the left ventricle of the heart. And the ejection fraction was only 40%, which confirmed the presence of chronic heart failure due to hypertension.
Having assessed the severity of the disease using correct diagnosis, we were ready to carry out adequate treatment, which had two main goals: reducing the severity of the clinical manifestations of heart failure and ultimately increasing the patient’s life expectancy.
By reducing the severity of the manifestations of the disease, experts mean the elimination or reduction of influences that contribute to its progression, and the possible elimination of the cause of heart failure. To do this, it is necessary to treat arrhythmias, inflammatory diseases, and chronic diseases of internal organs. For patients with angina pectoris and post-infarction cardiosclerosis, restoration of coronary blood flow is indicated by bypass surgery or stenting of the coronary arteries.
Adequate treatment
Therapeutic treatment of patients with chronic heart failure includes non-drug therapy and drug interventions. Non-drug treatment is the normalization of body weight, proper nutrition aimed at reducing elevated blood lipid levels, avoiding alcohol, limiting the consumption of table salt and liquid, and also moderate and dosed physical activity under the supervision and supervision of a doctor.
Drug therapy, which is preferably selected in a hospital, should be aimed primarily at the successful treatment of arterial hypertension. It has been proven that this is the most effective prevention of the development of chronic heart failure. By the way, it was with drug therapy that Marina’s treatment began. In particular, she was prescribed angiotensin-converting enzyme inhibitors (ACEIs), beta-blockers, veroshpiron and other diuretics. They also offered to carry out a full range of non-drug methods. Judging by her condition, I see that such treatment will definitely help her.
How can we help people who have already tried all therapeutic agents, but their stage of heart failure is still high? In Russia, approximately 8.5 million people suffer from heart failure, with 3.5 million having the disease at a severity level where pills are not effective. Swelling, shortness of breath, and fatigue occur in them at rest. Several times a year they are forced to undergo treatment in hospitals, but without much success.
Previously, the only method of saving lives and restoring the health of such patients was a heart transplant operation. Today, the main alternative to cardiac transplantation may be the use of circulatory support devices, called artificial ventricles. Miniature electromechanical pumps are completely implanted into the patient’s body and pump blood along with or instead of a diseased heart, helping the person live and lead an active lifestyle.
In its effectiveness, this method surpasses all therapeutic methods of treatment. Special studies have proven that placement of an artificial left ventricle improves the prognosis of patients even with critical chronic heart failure.
I told all this to a friend I met by chance. She paid attention to my recommendations to undergo examination at the cardiology department. She is now in the clinic, where she is undergoing correction with drug therapy, after which she will be transferred to cardiac surgery to resolve the issue of stenting the coronary arteries.
Larisa GENYA, Candidate of Medical Sciences Magazine “60 years is not age”
YOUR HEART SHOULD BE CHECKED AFTER 50 YEARS OLD
Heart disease has long ceased to be a problem for older people, but age still plays an important role. Our heart ages, like the rest of our body. The number of elastic fibers in vascular and cardiac tissue decreases, and collagen fibers increase. Figuratively speaking, if a young man’s blood vessels are a rubber tube, with age they become like old rubber: they bend reluctantly, crack in places, and after 60 years they turn into a hard metal pipe.
The ability of the heart to stretch decreases, and it itself decreases in size. This leads to increased systolic (upper) pressure in the blood vessels and increased diastolic pressure inside the heart. The heart has difficulty filling with blood and can only compensate for this in one way - by contracting faster. And this contributes to the occurrence of arrhythmia and heart failure. Therefore, the older a person is, the more he needs control over the cardiovascular system, even if he does not feel any reason to worry.
If there are problems, a full set of tests and tests to find out what condition the heart is in looks like this: general and biochemical blood tests, urine tests (heart function is closely related to kidney function), ECG, echocardiography, ultrasound of the thyroid gland and carotid artery and Holter monitoring (ECG is taken for 24 hours or longer). All this together will give a complete picture of what is happening.
Source: "Interlocutor"
Comments on the article
Add a comment
July 12, 2020
How is this condition treated?
To relieve shortness of breath during tachycardia at home, taking Valocordin or a sedative, like tincture of hawthorn and motherwort, can help.
For such problems, it is necessary not to treat increased heart rate and shortness of breath, but to treat the reasons that cause these symptoms. The treatment regimen is drawn up depending on the underlying pathological process. Medications, physical therapy, and surgery may be required. It is necessary to combine the main course of treatment with lifestyle corrections and avoidance of irritating factors.
Medicines can reduce nervous excitability, restore the usual heart rhythm, reduce myocardial oxygen demand and stabilize blood pressure. They should be used strictly according to the scheme drawn up by the attending physician.
Treatment of tachycardia
The essence of tachycardia therapy is to eliminate the causative factor, relieve the load on the heart muscle and stabilize its rhythm. The following medications are usually prescribed for long-term use:
- adrenaline blockers;
- cardiac glycosides;
- diuretics;
- angiotensin-converting enzyme inhibitors.
We suggest you read: Sinus tachycardia after chemotherapy
The course of treatment for shortness of breath is compiled depending on the causative factor:
- If a foreign body enters the respiratory tract, the patient must be given first aid in order to quickly remove this irritant.
- Allergic pulmonary edema is eliminated by the use of glucocorticosteroids, antihistamines and adrenaline.
- They save from asphyxia by performing tracheotomy and conicotomy.
- For asthma, you should take drugs representing the groups of beta-adrenergic agonists, glucocorticosteroids and anticholinergics.
- Inflammatory processes are eliminated using antibacterial and detoxification treatment.
- Tumors, pneumothorax and hydrothorax are treated with surgery.
Folk remedies
To normalize the heartbeat, the following recommendations are considered the most popular among traditional methods:
- An infusion of blue cornflower flowers will regulate your heart rhythm. Drink it 100 ml three times a day for 3 months.
- Oat juice from the greens of the plant is useful for this problem. It is taken 50 ml three times a day. This remedy is most effective if increased heart rate occurs along with hypertension.
- Brewing mint or lemon balm for a month and drinking it, like tea, helps with attacks of tachycardia - they will become less frequent and will be noticeably easier to tolerate. This tea is especially suitable for the female half of the population, because men may experience problems with potency when using it.
- Replace your usual cup of coffee or tea with a medicinal mixture of rose hips and hawthorn, motherwort leaves, and green tea. You need to take half a teaspoon of all ingredients.
- Adonis infusion. It is consumed in a course of two to three weeks, one tablespoon three times a day.
- Hawthorn infusion. 1 tablespoon of hawthorn flowers is poured into a glass of boiling water, and then infused for 20 minutes. You need to take the infusion half an hour before meals, 3 times a day, half a glass.
- Infusion of adonis. 1 teaspoon of adonis herb is poured into a glass of boiling water, then the infusion must be boiled again for 5 minutes. After this, the broth is infused for 2 hours. It should be strained and taken a tablespoon 3 times a day.
Which doctor should I contact?
Since shortness of breath can be associated with a variety of diseases, it is first appropriate to consult a general practitioner or pediatrician if the problem occurs in a child. Based on the medical history, description of the problem, and physical examination, the doctor will be able to make an assumption about why shortness of breath occurred and refer the patient to specialized specialists - a pulmonologist, cardiologist, hematologist, psychiatrist and others. Depending on what disease is detected, the doctor prescribes a treatment regimen.
References
- Martynenko T.I. et al. Optimization of early nosological verification of shortness of breath of pulmonary or cardiac origin // Pulmonology - 2014. - No. 1. - P. 27-31.
- Shortness of breath. Mayo clinic (date of access: 07/16/2019). URL: https://www.mayoclinic.org/symptoms/shortness-of-breath/basics/definition/sym-20050890.
- Princely N.P. Bronchial asthma: difficulties of diagnosis // Practical Pulmonology - 2011. - No. 1.
- Chikina S. Yu. Principles of assessing shortness of breath in the practice of a pulmonologist // Practical Pulmonology - 2006. - No. 2.
- Tatochenko V.K. et al. Pneumonia //Pediatric pharmacology – 2006. – T. 3. – No. 4.
- Poltavskaya M. G. et al. Chronic shortness of breath in cardiac patients: prevalence and etiology // Clinical Medicine - 2007. - T. 85. - No. 6. - P. 37-42.
- Polozova E.V., Shilov V.V., Kuznetsov O.A. The main clinical manifestations of damage to the respiratory system in acute severe carbon monoxide poisoning, complicated by thermochemical damage to the respiratory tract //Efferent Therapy - 2009. - T. 15. - No. 3 -4. – pp. 35-39.
- Avdeev S. N. Thromboembolism of the pulmonary arteries // Practical Pulmonology - 2009. - No. 3.
- Savenko I. A. et al. Clinical pharmacology of drugs for the treatment of anemia in the educational process // International Journal of Experimental Education - 2013. - No. 8. - P. 132-134.
- Nemerov E.V. et al. Analysis of clinical cases with shortness of breath syndrome //Siberian Medical Journal (Tomsk) – 2013. – T. 28. – No. 2.
- Mravyan S. R., Protopopova T. A. Diagnosis and treatment of cardiovascular diseases during pregnancy - 2010.
GZEA.PD.18.09.0435j
After tachycardia, it is difficult to breathe during pregnancy
Why does tachycardia occur after eating? What are the causes of such manifestations of arrhythmia? Your heart rate may increase after eating because you have heart disease:
- ischemic acute disease;
- cardiac chronic and acute failure;
- anomalies of various cardiac pathways;
- aortic insufficiency;
- rhythm disturbances;
- VSD;
- arterial hypertension.
If after eating you experience tachycardia and nausea, you need to be more careful about your health. Contact your physician and cardiologist, he will be able to determine why you have irregular heartbeat after eating. Your heart rate needs to be stabilized as much as possible so that breakfast, lunch and dinner do not affect your heart.
In this case, nausea after eating is an integral sign of tachycardia. Your heart muscle begins to work more actively, almost to the limit of its capabilities. If you have VSD, nausea after eating manifests itself more strongly, which prevents you from actively going about your business and working.
Also, after eating, there are periods of dizziness up to the point of loss of consciousness - be careful. If your head starts to spin, be sure to sit down and rest for a while.
In this case, tachycardia and shortness of breath also appear together. The pulse rises, breathing becomes much more difficult, so the patient may begin to choke when walking quickly or climbing steep stairs.
You may also experience severe chest pain, weakness, frequent yawning and anxiety immediately after eating. Remember that patients may even experience a fever as their heart rate increases and blood circulates faster. All these reasons should force you to definitely consult your doctor.
Weakness and tachycardia can occur after eating and due to other factors:
- obesity;
- diabetes;
- stomach diseases, which are especially aggravated after eating;
- pathologies of the nervous system;
- thyroid disease.
During pregnancy, tachycardia and breathing problems occur quite often. From a medical point of view, this phenomenon is explained by natural disturbances in the functioning of the cardiovascular system due to an increase in the load on it - in a woman in this position, the uterus requires more blood supply. Symptoms in the early stages of pregnancy are hardly noticeable, but by the third trimester they become quite noticeable.
Also, many doctors cite reasons such as:
- anemia;
- weight gain;
- malfunction of the thyroid gland;
- allergic reactions;
- bronchial asthma;
- stress;
- overvoltage.
To eliminate such symptoms, the doctor’s first recommendation is usually lifestyle modification. A special diet, gymnastics, walks in the fresh air, calmness - all this may well improve a woman’s well-being. If there is no effect from such changes in life, the doctor prescribes drug therapy depending on the characteristics of the person’s condition.
How much does pressure increase during exercise?
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Sport is a positive stress for the body. Changes in human pressure during physical activity are very common, due to the characteristics of the body and the preferred sport. Performing exercises stimulates the release of adrenaline, which plays an important role in a person’s adaptation to environmental factors. Systematic exercise helps strengthen the vascular wall, stabilize breathing, and also increase the degree of saturation of tissues with useful substances and oxygen.
Causes of increased blood pressure during exercise
An increase in the concentration of adrenaline in the blood is associated with activation of the sympathetic part of the nervous system. During physical exercise, breathing becomes more frequent and fluid circulation in the body improves. This requires additional costs from the body. Blood pressure often increases in everyday life - during heavy lifting, during long walking, and also in cases of nervous tension.
The following body systems are involved in increasing blood pressure:
- cardiovascular – blood moves faster, saturating tissues with useful substances, improving the tone of arteries and veins;
- respiratory - the lungs expand and fill with air, the internal organs receive more oxygen;
- humoral – metabolism in the body accelerates, the synthesis of certain hormones increases, muscle mass increases.
In trained people whose activities involve playing sports or other types of physical activity, changes in hemodynamic parameters during and after exercise may not be observed at all. The important thing is how long it takes for the increased levels to return to normal. If they persist for several hours, it may indicate hypertension.
Why does blood pressure increase after exercise?
A physically weak body reacts to new exercises with a short-term increase in blood pressure. Increase by 15–20 mm Hg. Art. within an hour is normal. Long-term maintenance of high levels indicates hidden problems of the vascular system. Arterial hypertension at the initial stage is observed only in stressful situations, without manifesting itself in a calm environment.
If high blood pressure occurs during exercise, and within an hour the blood pressure readings have not returned to normal, a person may experience:
- dizziness, accompanied by redness of the eyes, flickering spots in the field of vision, nausea and vomiting;
- pain in the heart of an aching, squeezing nature, up to an attack of angina pectoris due to spasm of the coronary vessels;
- lethargy and lethargy, numbness of the limbs, as well as impaired diction may indicate ischemia of brain tissue;
- external signs are facial redness, excessive sweating, constant shortness of breath, sudden coughing attacks.
Dealing with hypertension caused by one of the types of physical labor is more difficult than with the usual increase in blood pressure. Stabilization of hemodynamic parameters depends on the individual characteristics of the body. People prone to vascular diseases should carry a blood pressure-normalizing pill with them and carefully monitor how they feel when performing new exercises.
Reasons for decreased blood pressure during exercise
Regulation of vascular tone is carried out using the sympathetic and parasympathetic parts of the nervous system. In people with sympathicotonia, blood pressure increases in stressful situations. The predominance of the parasympathetic nervous system is one of the factors in the development of hypotension, which is worth remembering when performing sports exercises.
The following causes a decrease in blood pressure:
- vegetative-vascular dystonia of the hypotensive type;
- inconsistency of the selected set of exercises with the physical capabilities of a person;
- depletion of body resources (vitaminosis, overwork);
- heart defects, mitral valve prolapse;
- history of angina attacks.
If blood pressure decreases only during physical activity and quickly returns to normal levels within an hour after exercise, this may indicate asthenia. Poor nutrition, a sedentary lifestyle, excess weight and a history of lack of exercise make the body especially vulnerable. Thoughtful training with a predominance of the dynamic component will help the body strengthen.
Why does blood pressure drop after exercise?
Many people complain of weakness and dizziness after exercise. If proper rest is provided, their condition quickly returns to normal. If low blood pressure persists for a long time after exercise, this may indicate a decrease in vascular tone, which leads to VSD and persistent hypotension.
Decrease in values by 10–20 mmHg. Art. characterized by:
- dizziness, drowsiness;
- severe weakness;
- blurred vision, blurred vision;
- pain behind the sternum;
- feeling of lack of oxygen.
Blood pressure drops to 90 to 60 mmHg. Art. and below can lead to sudden loss of consciousness. To prevent the development of collapse, you need to be careful about your condition during training. Hypotonic people are best suited for walking, exercise therapy and swimming, which help strengthen the vascular system.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
Monitoring hemodynamic parameters
Even experienced athletes with high endurance must monitor their condition during training. Before the first lesson, it is recommended to visit a doctor, who should assess the level of blood pressure, pulse intensity, breathing rate and then give recommendations regarding the desired sport.
To improve the condition of the circulatory system during training you need:
- ensure sufficient heat transfer through high-quality clothing (the correct size, appropriate for the season);
- measure blood pressure 20 minutes before exercise and 10 minutes after each exercise session;
- choose professionally equipped premises with good ventilation and no proximity to production facilities;
- drink enough clean water (not less than 2 liters daily).
Those who want to exercise should remember to eat properly. A love of fatty and fried foods, as well as alcohol abuse, negatively affects the condition of blood vessels. It is worth limiting the amount of coffee and black tea you drink. To improve vascular tone, you need to include more foods containing K and Mg in your diet.
Pressure standards during and after loads
In medical practice for many centuries, the value of normal blood pressure was set at 120/80 mmHg. Art. Sports exercises, which are positive stress for the body, can lead to a slight increase in blood pressure. The indicators that are optimal for a particular person are called “working” indicators. If a person feels well, having indicators of 100/70, this is not a cause for concern.
Normal blood pressure depends on a person’s gender:
- for men 18–50 years old – 120-130/80–85 mmHg. Art.;
- for women 18–50 years old – 110-120/80–85 mm Hg. Art.;
- the figure is 140/90 mmHg. Art. is the limit indicating the development of arterial hypertension.
During intense exercise, the pressure of a previously untrained person during exercise can increase by 15–25 mm Hg. Art. Normally, the indicators should return to “working” levels after half an hour. Elevated blood pressure persisting for several hours indicates hypertension. The first stage of hypertension implies indicators of 140–159/90–99 mmHg. Art. and allows light loads if the recommendations are followed. The transition of the disease to the second and third stages is a serious obstacle to playing sports.
Contraindications for physical activity
It is better to refrain from intense exercise during periods of exacerbation of chronic diseases, with severe heart pathologies, as well as in the case of an expected pregnancy.
People suffering from:
- frequent sudden changes in pressure in everyday life;
- thrombosis of blood vessels of the lower extremities;
- cerebrovascular accident.
If your blood pressure still hasn’t returned to normal after half an hour, you should think about other types of physical activity. If there is a sharp deterioration in the condition that occurs against the background of physical activity, sports should be stopped for a while.
Is there any danger?
Normal physiological tachycardia and rapid breathing caused by overexertion are completely normal and should not cause concern.
Pathological tachycardia can have quite serious consequences, because in this case the heart does more work, which leads to faster wear and tear. Tachycardia is especially dangerous in its paroxysmal form, in which the heart rate reaches three hundred per minute. It can lead to ventricular fibrillation, which can be fatal.
If breathing problems appear without obvious reasons, you should suspect some kind of malfunction in the functioning of the human body. Considering the tachycardia in this case, the disorders relate to the cardiovascular system. But only a specialized doctor can make a final diagnosis, so if such problems arise, you must immediately seek medical help.
When a rapid rhythm is combined with a lack of air, you need to analyze the physical stress to which the body has recently been subjected. If there were enough of them, then to improve well-being and avoid similar health problems in the future, the physiological factor should be reduced.
Tags: happen, shortness of breath, tachycardia
About the author: admin4ik
« Previous entry
Side effects of beta blockers
Taking beta blockers can cause hypotension, an excessive decrease in blood pressure, and bradycardia, a decrease in heart rate. The patient should quickly seek medical help if the systolic pressure is less than 100 mmHg and the pulse is less than 50 beats per minute. Beta blockers should not be taken during pregnancy as they may cause fetal growth retardation.
- The best way to recover from hypertension (quickly, easily, healthy, without “chemical” drugs and dietary supplements)
- Hypertension is a popular way to cure it at stages 1 and 2
- Causes of hypertension and how to eliminate them. Tests for hypertension
- Effective treatment of hypertension without drugs
Beta blockers have numerous side effects. Here are the most serious of them.
- Increased fatigue: This may be the result of decreased blood flow to the brain as blood pressure drops.
- Slow heart rate: a sign of general weakness.
- Heart blocks: If there is a problem with the conduction system of the heart, taking beta blockers may be harmful.
- Exercise intolerance: Not the best choice of drug for an active athlete.
- Exacerbation of asthma: drugs in this group can worsen the condition of patients with bronchial asthma.
- Reducing levels of LDL cholesterol, or low-density lipids in the blood: Some beta blockers reduce levels of “good” cholesterol.
- Toxicity: If you have liver disease or kidney failure, beta blockers can accumulate in the body as they are cleared from the body through the liver, kidneys, or both.
- Possibility of increased blood pressure if you stop taking the drug: If you suddenly stop taking the drug, your blood pressure may rise even higher than before you started treatment. These medications should be stopped gradually over several weeks.
- Lower blood sugar levels: Diabetics taking this class of drugs may have a reduced response to low sugar levels because the hormones that raise blood sugar levels are dependent on nerves blocked by beta blockers.
- The most dangerous side effect of stopping beta blockers: heart attacks. Beta blockers should be stopped gradually to avoid heart pain and heart attacks.
Conditions requiring special caution when using beta blockers:
- Diabetes mellitus (especially patients receiving insulin);
- Chronic obstructive pulmonary disease without bronchial obstruction;
- Peripheral arterial disease with mild to moderate intermittent claudication;
- Depression;
- Dyslipidemia (problems with cholesterol and triglyceride levels in the blood);
- Asymptomatic sinus node dysfunction, 1st degree atrioventricular block.
In these conditions you should:
- choose cardioselective beta blockers;
- start with a very low dose;
- increase it more gradually than usual;
- for patients with diabetes - carefully monitor blood glucose levels.
Absolute contraindications to the use of beta blockers:
- Individual hypersensitivity;
- Bronchial asthma and chronic obstructive pulmonary diseases with bronchial obstruction (or requiring the use of bronchodilators);
- Atrioventricular block of 2-3 degrees, in the absence of an artificial pacemaker;
- Bradycardia with clinical manifestations;
- Sick sinus syndrome;
- Cardiogenic shock;
- Severe damage to peripheral arteries;
- Low blood pressure with clinical manifestations.