How to stop an attack of tachycardia during stress?
Tachycardia - increased heart rate. A person’s pulse under natural conditions does not exceed 60 beats/min, and when excited, the rapid heart rate reaches 100. There are the following main signs of a rapid heart rate from stress:
- constant feeling of anxiety and fear;
- rapid breathing;
- weakness;
- compression in the chest area;
- tingling in the heart;
- a person feels a pulsation in the veins in the neck, and beats in the head.
Nervous tachycardia has a physiological basis. A person experiences rapid heartbeat due to constant nerve strain or physical overload. Anxiety increases during stressful situations. Young people who are constantly on edge are more likely to experience depression than adults.
Enter your pressure
Move the sliders
Tachycardia due to stress requires rest. Therefore, the patient must be put to bed, high pillows placed under his head, and all irritants removed. To relieve anxiety, the patient is given medications - Corvalol, Valocordin or Barboval. While waiting for medical help if you have severe stress, it is recommended to get a light relaxing massage.
Against the backdrop of strong excitement, a person may develop a fever.
- frequent shallow breathing;
- inability to take a full breath;
- rush of blood to the cheeks (feeling of heat);
- chest tightness;
- headache;
- anxiety and fear;
- increased sweating;
- palpable pulsation in the neck area.
First aid
If there is severe tension on the nerves that causes tachycardia, you should proceed as follows:
- Sit or lay the patient down so that the head is elevated.
- Unbutton the collar and remove all accessories from the neck.
- Provide access to fresh air or turn on a fan.
- Give a sedative - Corvalol, Barboval, Valocordin.
If palpitations are not treated, a heart attack may occur, in which necrosis of the heart tissue occurs due to the interruption of blood supply. Tachycardia is also dangerous for the development of a stroke, when cerebral circulation is sharply disrupted. The condition is fraught with complete or partial paralysis of the limbs, speech impairment, coordination of movements, and blurred vision. Such consequences lead to severe disability or death.
Tachycardia in neurosis is accompanied by painful sensations in the chest in the presence of normal physical indicators. Only the heart rate increases. The problem appears when a person exposes himself to excessive emotional stress. The disease is called heart neurosis.
Deviation is accompanied by external and internal manifestations. Signs of pathology occur when a person experiences conflict, stress, or expects bad or good news.
Painful sensations in the heart can last for several days or even a month. They have varying degrees of severity:
- With cardialgia, a person is bothered by dull, pressing or sharp pain in the chest area. They can spread to other parts of the body, for example, the arm, shoulder blade, neck. These manifestations are accompanied by anxiety and fear of death. If you undergo an electrocardiogram, you may not notice any symptoms. But sometimes neurogenic cardialgia leads to spasm of the coronary arteries, which can cause circulatory problems.
- Panic attacks are observed, during which strong impulses of fear roll in, and hot and cold flashes disturb. There is a feeling of hiding and running away. The heart rate increases to critical levels.
- An increase in heart rate always accompanies panic attacks. It can also occur for other reasons: during severe physical exertion or as a result of early awakening. Tachycardia can become permanent.
- Patients report a feeling of heart sinking. This is how extrasystoles appear that occur in the morning. The heart may freeze for seconds, and after that the heartbeat returns to normal. If you change the situation or calm down, the symptom disappears.
- A feeling of shortness of breath, fever or chills indicate an incorrect reaction of the body to neurosis.
People suffering from neuroses are often diagnosed with vegetative-vascular dystonia, which occurs when the functions of the nervous system are impaired. Manifestations of rapid heartbeat can also be noticed after eating food. This is due to the rush of blood to the gastrointestinal tract.
These conditions also include a feeling of dizziness, trembling, swelling or paleness of the skin.
In hypertension, the presence of cardiac neurosis is accompanied by increased blood pressure, pain in the heart and headaches.
In such situations, treatment difficulties arise, since each patient complains of a large number of different symptoms.
It is important to be able to distinguish heart pain associated with neurosis from angina pectoris. If there are problems with the main muscle, any physical activity causes attacks of pain. You can improve your well-being only with the help of Nitroglycerin.
With neurosis, heart medications do not bring relief, so patients usually ask the doctor to prescribe something more effective.
Tachycardia due to nerves is treated depending on the cause. If the provoking factors are not eliminated, the problem will persist for a long time.
Before prescribing medications, in order to improve your health, it is necessary to undergo an examination and reduce the negative impact of provoking factors.
During treatment, certain difficulties may arise. This is due to the fact that many patients with this diagnosis refuse to visit psychotherapists and do not want to follow the doctor’s recommendations, considering their disorder as something shameful.
Therefore, it is important to explain to the patient what his problem means and persuade him to visit other highly specialized specialists. For some patients, recovery occurs immediately after visiting a doctor and having a detailed conversation.
It is impossible to determine exactly which drugs to prescribe. The course of treatment depends on the symptoms and general condition of the body. First of all, tachycardia in depression and neurosis is eliminated by methods of getting rid of anxiety and psychological discomfort:
- A calming, encouraging and reassuring conversation is held with the patient. The patient should talk to the psychotherapist, who deals with such problems.
- They recommend streamlining your routine, getting more rest and eating right, avoiding stress and normalizing relationships in the family and at work.
- If the patient complains of feeling unwell, he is first prescribed mild sedatives based on medicinal plants and the cause of the disorder is eliminated.
There are neurological clinics that treat people with similar problems. Typically, such establishments house patients suffering from panic attacks, migraines and other nervous disorders.
In case of frequent attacks of neurosis, they can be stopped with the help of:
- light antidepressants in the form of Amitriptyline, Grandaxin, Azafen;
- beta blockers. If you are worried about tachycardia against the background of hypertension, then your well-being is improved with the help of Anaprilin and Trazicor;
- mild sleeping pills if a person suffers from insomnia. But he should use them no longer than a few weeks, since they quickly get used to them and cannot sleep without them;
- physiotherapeutic procedures. The condition is improved by using electrophoresis, pine and pearl baths, and electrosleep. Increased excitability can be eliminated with a Charcot shower and a circular shower;
- autogenic training and mental relaxation.
For any form of neurosis, it is useful to undergo sanatorium-resort treatment in institutions of the neurosomatic type.
Very often it is enough to change the environment, the regime, tune in to a positive mood, undergo balneological therapy and stop using any medications.
Rapid heartbeat due to nervousness is treated mainly with traditional methods. Feeling better is achieved with the help of tinctures and decoctions. The most commonly used root is valerian root. Thanks to medications based on it, you can quickly calm the nervous system. Hop cones, calamus rhizomes, and motherwort have a positive effect.
If disorders of the central nervous system are accompanied by dizziness and attacks of suffocation, then to alleviate the condition, collections of caraway, motherwort, chamomile, cudweed, and hawthorn help.
Peony tincture is used as a sedative.
You can enhance the beneficial properties of plants by drinking a glass of warm water with the addition of a spoon of honey at night. This will relieve nervous tension and make it easier to fall asleep.
Regardless of the cause, nutrition plays an important role in recovery. It helps restore heart function. First of all, it is recommended to eat more nuts. They contain magnesium, which is necessary for the functioning of the nervous system. It increases the resistance of nerve fibers to impulses.
If treatment is not started in a timely manner, a neurotic personality type develops. This fact should be especially taken into account if signs of a problem have arisen in a child.
Tachycardia is not considered a separate disease, but exclusively one of the components of the disease. An increased heart rate during stress indicates that a malfunction is occurring in the human body. Therefore, an attack of tachycardia indicates disturbances in the functioning of the heart or other internal organs. The outbreak must be stopped quickly, because the consequences can be tragic.
Treatment of attacks
If a stressful situation is out of a person’s control, only a doctor will prescribe adequate treatment.
In case of nervous disorders, it is advised to seek help from a psychologist or psychotherapist. The doctor will help you cope with depression, eliminate anxiety, and keep your nerves in order. The doctor will teach you how to control yourself and relieve the constant feeling of anxiety. The general practitioner will prescribe an ECG and a general blood test to find out the cause of the tachycardia.
Signs and treatment of cardiac neurosis
The main cause of the development of heart neurosis (cardioneurosis) is stress. The process of the onset of the disease is simple: stress provokes a sharp release of adrenaline, which harms the heart and blood vessels. People of all ages are at risk for developing this disease.
There is no prevention of cardioneurosis. To reduce the likelihood of the disease occurring, it is necessary to avoid stressful conditions and periodically take sedatives.
Especially if you have heart defects and heart diseases, such as myocarditis, rheumatic carditis and others. Also at risk are people who often suffer from acute respiratory infections and sore throats, are subject to frequent mood swings, depression, smokers and drink alcohol, and have had pneumonia.
Let's look at the signs and treatment of heart neurosis.
Signs of cardiac neurosis.
A person suffering from cardioneurosis often experiences such signs of the disease as attacks of dizziness, insomnia, pain in the heart, shortness of breath, tachycardia (accelerated pulse) and arrhythmia. During physical exertion and nervous tension, I experience discomfort in the heart area and dark vision.
A strong sound is enough - and the patient is covered in perspiration, his heart is tormented, and he may even faint in severe cases. Patients with cardiac neurosis are very excitable.
Despite all the external signs of abnormal heart function, medical tests such as echography and ECG do not reveal heart disease. Therefore, it is very difficult for a doctor to make a diagnosis, because all tests are normal, but the patient feels unwell, he may find signs of hypertension, ischemia and other heart diseases.
How can you identify heart neurosis?
The disease heart neurosis can easily be mistaken for another disease of the cardiovascular system, for example, ischemia or angina. Therefore, you need to pay attention to the following signs of the disease.
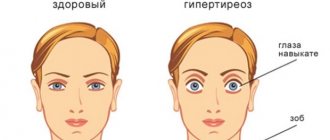
Why does tachycardia appear with VSD?
With vegetative-vascular dystonia, the pulse often increases. For the development of the pathology in question, certain conditions are necessary. This usually happens when:
- chronic fatigue;
- working at night, insufficient sleep;
- nervous overstrain, neuroses;
- depression;
- smoking, poor diet and alcohol abuse;
- general exhaustion of the body;
- hormonal imbalance.
Scientists believe that most pathologies of the heart and blood vessels arise under the influence of psycho-emotional factors. Increased heart rate is a concern with low levels of physical activity. Under such conditions, thinning of the myocardium occurs.
The development of tachycardia is observed when the sympathetic department of the autonomic nervous system predominates over the parasympathetic.
This failure does not allow the ventricles to fill with blood in a timely manner, and organs and tissues do not receive it in sufficient quantities. Therefore, the heart begins to contract more often to make up for the blood deficiency.
Prevention of tachycardia
Prevention of tachycardia includes compliance with the following recommendations:
- Minimize the consumption of coffee, strong tea, alcohol, chocolate;
- Avoid overeating, try to give preference to vegetables and fruits that contain large amounts of vitamins and microelements, especially pay attention to replenishing the body with magnesium and potassium;
- Maintain a work/rest/sleep schedule;
- Avoid working with a lot of stress;
- Avoid taking medications without consulting your doctor;
- Try to move more, but at the same time do not overstrain your body with excessive physical activity;
- Spend more time in nature.
For what reasons does tachycardia occur in neurosis?
This disorder can occur under the influence of many factors. It's connected with:
- features of the development of the nervous system. Usually with asthenic type;
- vegetative-vascular dystonia;
- high blood pressure;
- hormonal changes in the body;
- poor environmental situation;
- working in hazardous industries;
- chronic infectious diseases.
But the main factors causing cardioneurosis are considered to be mental trauma and high blood pressure.
Tachycardia with neurosis occurs if:
- Vegetative dystonia.
- Hypertension.
- Hormonal changes in the body.
The impetus for cardialgia of nervous disorders can also be:
- bad ecology.
- bad habits.
- chronic infections.
Doctors often find it difficult to distinguish cardialgia of nervous disorders from angina pectoris. A characteristic sign of the first case is the behavior of people; with severe heart pain, patients try to move less so as not to aggravate it. And with cardioneurosis, the pain does not hamper movement, the person is able to walk, run and gesticulate briskly.
Symptoms of cardiac tachycardia:
- Feeling of heat in the body.
- The skin becomes pale or very red.
- Hands and feet get cold.
- Body temperature rises.
Symptoms of tachycardia in neurosis:
- Heart pain can last from a few minutes to a couple of months. It radiates under the shoulder blade or into the neck area.
- The symptom disappears if the patient begins to move.
- Fear of death and anxiety arise.
- Panic attacks. The pulse becomes very rapid.
- Heavy loads.
- Dyspnea.
- Vegetovascular dystonia.
- Dizziness.
A stressful situation provokes in a person a sharp increase in the production of the hormones adrenaline and norepinephrine. Under the influence of these biologically active substances, vasospasm occurs, which impedes blood flow. This leads to increased heart function and an increase in heart rate. Nervous tachycardia occurs due to the following reasons:
- conflict situations in the workplace and within the family;
- a constant feeling of anxiety when loved ones are sick or in an unfavorable environment;
- death of a relative;
- reading books or watching programs with negative content;
- long-term depression;
- severe anxiety before responsible public speaking;
- melancholic temperament.
Heart neurosis: why does it occur and how to treat?
Heart neurosis is a functional pathology of the main organ.
Treatment of cardiac neurosis is carried out by a general practitioner. Another name for this phenomenon is cardioneurosis. It appears due to severe stress, excessive stress or emotional shock.
Due to the above reasons, cardiac activity accelerates, which leads to disruption of the natural rhythm of work. It's not fatal or dangerous, but it does cause problems.
According to statistics, about 10% of the population are susceptible to cardioneurosis.
Symptoms
general information

Myocarditis is a disease of the heart muscle in which it becomes inflamed and the heart loses the ability to perform its main functions: excitability, contractility, conduction.
What is the danger?
Tachycardia, especially persistent, can worsen the patient's condition.
Severe tachycardia, which tends to recur periodically, is very dangerous for humans. The consequence may be the development of heart attacks and strokes. Of the 72% relapses, every fifth patient is susceptible to death. Therefore, people suffering from tachycardia are at risk of sudden death. Compared to people who do not have a rapid heart rate, the risk is doubled and sometimes 10-fold.
If you do not deal with tachycardia during VSD, the consequences can be quite serious. An increased heart rate negatively affects a person’s quality of life, causing shortness of breath and dizziness. Lack of treatment will lead to hypertrophic changes in the myocardium. Over time, the heart wears out, its contractility decreases, and heart failure occurs.
Tachycardia accompanying vegetative-vascular dystonia is dangerous due to the development of:
- insufficient blood supply to the brain;
- cardiac asthma or pulmonary edema, which is associated with left ventricular failure;
- arrhythmic shock.
That's why it's so important to fix the problem in a timely manner.
How to determine the presence of unnoticed chronic tachycardia yourself?

In order to independently determine the presence of tachycardia during VSD, you need to be at rest, it is better in the morning after waking up to lie in bed for a few minutes, and then count the pulse on your wrist.
The algorithm of actions looks like this:
- First, you need to examine both hands to determine which of them has a more distinct pulse;
- Place a stopwatch in front of you (every phone now has one);
- Place your index and middle finger on the radial artery (the place on the wrist under the thumb) and press lightly;
- Looking at a stopwatch, count the number of beats within 30 seconds. Multiply the resulting number by 2, this will be the number of heartbeats per minute at rest, at low loads.
If there is a need (on the recommendation of a doctor) to monitor your heart rate regularly, it makes sense to purchase a portable heart rate monitor or electronic blood pressure monitor at the pharmacy. All tonometers of the latest generation are equipped with pulse sensors.
Classification of pathology
VSD can manifest itself not only as tachycardia. Pulse disturbances in this condition occur in the form of:
- Supraventricular tachycardia. At the same time, the heart contracts at a speed of more than two hundred beats per minute. The attacks occur suddenly and last from a few seconds to 2-3 days. The pathology differs in its supraventricular origin. The ectopic focus can also be located in the atria or atrioventricular node. This phenomenon does not pose a health hazard, but is accompanied by nervous tension, which causes significant discomfort to the person.
- Persistent tachycardia. The pulse does not exceed 120 beats per minute. The patient may not notice the problem for a long time, since it is characterized by slow development and gradual completion. In this case, disturbances in heart rhythm and increased pressure in the arteries are observed;
- Sinus tachycardia. The generation of the impulse occurs in the sinus node. The number of heart contractions is no more than 135 per minute. Most often it affects people at a young age. If the patient tolerates the attacks well, then this situation can be regarded as a normal condition.
Depending on where the pathological focus is located, generating incorrect impulses, tachycardia can be:
- ventricular or atrial;
- sinus.
Classification based on the cause of the deviation identifies pathologies:
- Extracardiac, when a rhythm disturbance occurred under the influence of external factors.
- Intracardiac. Heart rate increases as a result of organic damage to the heart and blood vessels.
Therapy is prescribed depending on the type of pathology.
How not to miss the first symptoms?

Paroxysmal tachycardia, manifested by a sudden attack of rapid heartbeat during neurotic processes, is accompanied by signs of disorders in other organ systems. In addition to abnormal heart rhythm, stabbing chest pain and dizziness, nausea and vomiting, shortness of breath with pronounced tachypnea, irritability, panic attacks and insomnia are also observed. Sometimes cardioneurosis is accompanied by an obsessive fear of cardiac arrest, which is called cardiophobia. If the work of the parasympathetic nervous system predominates, then neurosis, on the contrary, is manifested by attacks of slow cardiac activity, increased sweating and redness of the skin of the face or limbs.
How to stop an attack of tachycardia during stress?
Nervous tachycardia can cause serious disturbances in the functioning of the heart. Therefore, in case of prolonged attacks, it is necessary to take measures.

The following measures are used as first aid:
- The patient needs to be provided with fresh air. Therefore, you need to open a window indoors or take it outside.
- Put a person to bed.
- They calm and distract the patient from problems.
- They give sedatives in the form of Valerian, Validol or Corvalol.
- If you have a tonometer, measure your blood pressure and pulse.
First aid should be provided without noise and fuss. The patient's condition should be monitored by a doctor. Therefore, if there is a noticeable increase in the pulse and the appearance of weakness, it is necessary to call an ambulance or send the person to a medical facility in other ways.
The use of sedatives is indicated throughout the day from the onset of the attack. The breaks between taking medications should be several hours. When the symptoms disappear, the person is recommended to undergo testing.
Treatment of attacks
During treatment or remission, heart attacks may occur. Although they do not pose a threat to life, they cannot be ignored. First aid recommendations:
- Lay the patient down and provide air access.
- Measure blood pressure and pulse.
- Distract with conversation on neutral or interesting topics.
- Offer a mild sedative: valerian, motherwort, Corvalol.
If the pulse rate increases, dizziness occurs, you need to call an ambulance.
How to get rid of the disease 7 ways
Everyone who is familiar with the diagnosis of vegetative-vascular dystonia knows the concept of tachycardia. Why tachycardia occurs during VSD should be examined in more detail.
Need to know! The very concept of “tachycardia,” translated from medical language, means “rapid heartbeat.” Normally, in a middle-aged adult at rest, the number of heart beats per minute should correspond to an average of 72 beats. These parameters differ slightly between women and men (from 65 to 90 and from 60 to 80, respectively).
In children under 2 years of age and elderly people, heart rate is increased to 100-140 beats per minute. This means that if a thirty-five-year-old woman sitting quietly in front of the TV has a pulse exceeding 90 beats per minute, we can detect an attack of tachycardia during VSD.
It is completely impossible to recover from tachycardia with VSD. In order for the tachycardia caused by VSD to disappear, the disease of vascular dystonia itself must be cured. There is a separate article on how to treat VSD, so it is worth considering ways to eliminate pulse instability in the presence of VSD.
You can stop an attack of tachycardia during VSD (with a heart rate of more than 160 beats per minute) by observing the following measures:
- Take a reclining position to ensure a state of rest;
- Release your neck and chest if you have tight underwear (open your shirt collar, loosen your tie, unfasten your bra);
- Rinse your face with cold water, place a damp, cool cloth or towel on your forehead;
- Try to cough or induce vomiting (if an attack of tachycardia during VSD is accompanied by nausea);
- Provide fresh air access to the room and use classical breathing techniques. For five minutes, inhale deeply and exhale quickly;
- Take from 15 to 30 drops of Corvalol, Valoserdin or Valerian tincture;
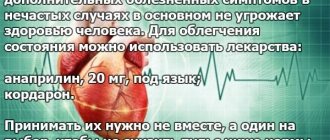
- If an attack of tachycardia during VSD caused a violent emotional outburst, accompanied by an increased release of adrenaline into the blood, beta-blockers will help calm the heart. The simplest and most accessible among them is “Anaprilin” at the time of tachycardia during VSD. Taking one tablet under the tongue blocks the release of adrenaline, slightly lowers blood pressure, and reduces heart rate. The effect of “anaprilin” is symptomatic and short-term. Taking it as a therapeutic agent at the time of tachycardia with VSD does not make sense. Another important note: if two sublingual Anaprilin tablets did not have the desired effect, ten will not help, and an overdose will lead to serious complications.
If, 10 minutes after the onset of an attack of tachycardia during VSD, at the time of applying the above measures, the heart rate does not fall below 150 beats per minute, you should urgently call an ambulance. Since the development of complications such as myocardial infarction, stroke, and clinical death is possible.
Tachycardia with VSD manifests itself constantly. The pulse rate at rest may be 30 beats per minute higher than normal. Sometimes a person does not even feel this state, because he is used to it. Such tachycardia with VSD leads to serious problems in the functioning of the heart and to dangerous disorders.
To avoid the development of negative consequences of tachycardia during VSD, you should undergo a thorough examination of the body. The cause of chronic tachycardia may not be VSD at all, but more serious health problems.
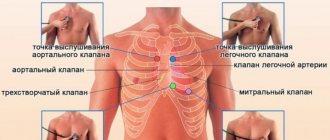
Diagnostics
In order to accurately establish the diagnosis and ensure the normal functioning of the heart, procedures are prescribed that make it possible to determine the nature of tachycardia, its causes, type, and formulate a possible prognosis.
- Electrocardiogram. Electrical impulses from the heart are measured.
- Daily monitoring. Recording heart function for one day.
- Event recorder. A device that records signals when the patient experiences characteristic symptoms. Helps examine rhythm disturbances at selected time intervals.
- Electrophysiological studies. A special catheter is inserted into the vein and advanced towards the heart, controlling the process. Having reached the goal, the device begins to stimulate contractions, and heart rate indicators are recorded.
- Table tilt test. Helps determine how the nervous and cardiovascular systems respond to changes in posture. The patient is injected with a drug that provokes arrhythmia, and then placed on a table that rhythmically changes position.
The main method of treating cardiac neurosis is psychotherapy. Sessions help to find out the cause of the nervous condition, in most cases it is dissatisfaction with work, problems in personal life. An excited state undermines the immune system and causes fatigue. Sessions are more effective when combined with medications selected by the doctor. They start with light sedatives on a homeopathic basis.
Neurotic attacks can be treated with stronger medications:
- Antidepressants: azaphene, amitriptyline, nialamide.
- Beta-blockers: Trazicor, anaprilin. Prescribed when tachycardia and hypertension reach a borderline state.
- Sleeping pills to improve sleep. Selected individually. It is recommended to take the medicine for no more than three weeks to avoid addiction.
Complex prescriptions give a good effect:
- Electrosleep.
- Electrophoresis.
- Pearl and pine baths.
- Sharko's shower.
Folk remedies
Traditional methods are widely used to treat tachycardia in neurosis. The most popular recipes are tinctures of valerian and peony. Collecting hop cones or calamus rhizomes is effective. Disorders accompanied by dizziness and attacks of suffocation can be relieved by a collection of cumin, motherwort, chamomile, cudweed and hawthorn.
A frequent pulse with VSD can be detected at home. It is necessary to count the number of contractions while in a calm state. If nothing worries you, then the diagnosis is made by chance during a routine examination. To normalize the condition, it is necessary to identify what caused the violation and eliminate the cause. In this case, the following diagnostic methods are used:
- electrocardiogram;
- echocardiography;
- magnetic resonance imaging.
A conversation is held with the patient, during which the doctor collects anamnesis and identifies factors contributing to the development of hypertension. If there are organic or psychological causes, they are treated. The International Classification of Diseases identifies VSD as one of the types of neurosis. Therefore, the patient must undergo a course of restoration and strengthening of the nervous system.
Treatment of tachycardia with folk remedies
Important!
Before using folk remedies against tachycardia, be sure to consult your doctor! Herbs, fruits, lemon and honey. Peel 4 lemons and squeeze out the juice, which should be mixed with 250 g of honey. Next, grind 16 leaves of indoor geranium (kalachik) and 18 almonds through a meat grinder, then mix this mixture with 10 g of valerian tincture and 10 g of hawthorn tincture. Mix all the prepared ingredients thoroughly and add 6 whole camphor grains to the mixture. The resulting folk remedy for tachycardia should be taken 1 tbsp. spoon in the morning, on an empty stomach, 30 minutes before meals, and store in the refrigerator.
Garlic and lemon. Add 10 medium chopped garlic cloves, juice from 10 lemons and 1 liter of honey to a 3-liter jar. Mix all the ingredients thoroughly, cover the jar tightly with plastic and set aside to infuse for 7 days. You need to take the resulting product 2 tbsp. spoons, 1 time per day, until complete recovery.
Adonis. Boil 250 ml of water in a small saucepan, then turn the heat to low and add 1 teaspoon of adonis herb to the water. Boil the product for no more than 3 minutes, then remove from heat, cover with a lid and set aside to infuse for 30 minutes. Next, you need to strain the broth and take 1 tbsp. spoon 3 times a day.
To achieve the maximum effect from Adonis, take the following remedy throughout the day: peel and cut 500 g of lemons, to which add a couple of tablespoons of honey and 20 crushed apricot kernels. Mix the weight thoroughly and take this mixture 1 tbsp. spoon morning and evening. By the way, apricot kernels contain vitamin B17, which also has an antitumor effect.
Adonis. Pour 1 teaspoon of adonis herb with a glass of boiling water and put the product on low heat for 5 minutes, then remove it from the heat, cover and let it brew for 2 hours. Next, you need to strain the product and take 1 tbsp. spoon 3 times a day, 30 minutes before meals.
Hawthorn. Pour 1 tbsp. spoon of hawthorn flowers with a glass of boiling water, cover the product with a lid, let it brew for about 30 minutes, then strain and take the prepared remedy for tachycardia, 100 ml 3 times a day, 30 minutes before meals. The course of treatment is until complete recovery.
Causes
The body's normal reaction to life
Tachycardia with neurosis, VSD, panic disorder occurs at the same time as in all other people on the globe. Another thing is that an anxious neurotic, concentrated on the work of his body in general and the heart in particular, interprets these normal physiological reactions as symptoms of an impending serious illness and even death.
The following can provoke an increase in heart rate both in neurosis and in good health:
- insomnia;
- alcohol consumption;
- caffeine;
- increased body temperature (both in the heat and during acute respiratory infections);
- changes in hormonal levels (primarily in women);
- a drop in blood sugar during hunger (the hunger itself may go unnoticed);
- smoking, etc.
And, of course, the heart rate always increases during physical activity. This is the norm. But suspicious, anxious people sometimes become so afraid of this norm that they notice a terrible heartbeat even when getting out of bed and walking across the room.
In fact, when rising from a horizontal to a vertical position, all people's heart rate increases. But not everyone thinks to count it.
Also, all people normally have an increase in heart rate after eating. But only anxious patients with VSD notice some kind of special tachycardia after eating, which often provokes the development of panic after eating.
Preparing for fight and flight
If you have generalized anxiety or panic disorder, or you believe that you suffer from vegetative-vascular dystonia, you are constantly worried. Even when you don't notice it. That is, your body is constantly preparing to run or fight. And it certainly increases your heart rate. That's how it should be.
In this case, palpitations are associated with an increase in the level of stress hormones, and with increased breathing, often leading to hyperventilation, and with the redistribution of blood in the body, and with the transition of muscles into a painful state.
All these reactions of preparation for active actions should increase the heart rate. And they do. And this indicates health, not illness.
Obsession with counting pulse
It has already been said above that patients with neurosis, VSD, etc. may notice tachycardia not only when it is present, but also in its absence. The heart rate will be a maximum of 90 beats, or even 72, the heart will beat perfectly evenly, but the neurotic will constantly complain about the palpitations and be sure that he is dying.
What can we say about the horror that covers a suspicious person at the moment when his heart actually beats at a frequency of 140 or more beats per minute. Patients with panic disorder interpret this behavior of their heart as the inevitable approach of death.