Author: Tamara Golubeva (education biology and chemistry)
Unfortunately, time does not make people younger. The body ages, and the blood vessels age along with it. Metabolism changes in tissues, blood clotting is disrupted. Chronic diseases accelerate these processes. As a result, blood clots form in the vessels, which can block the blood flow. This disease is called thrombosis.
Depending on the location of the blood clot, a person may develop myocardial infarction, stroke (cerebral infarction) and other equally dangerous complications. Is it possible to help the victim? There is salvation - thrombolysis or thrombolytic therapy (TLT)!
Undoubtedly, timely assistance will not only save a person’s life, but also give hope for complete rehabilitation. Not everyone knows about this, and therefore wastes valuable time. But it is quite logical to assume that blood flow can be restored by removing the unfortunate blood clot in one way or another. This is the essence of TLT.
Thrombolytic drugs are life-saving for a wide variety of vascular diseases, including pulmonary embolism (PE), deep vein thrombosis, cardiac infarction, and ischemic stroke.
Types of TLT:
- Selective thrombolysis. With this method, a drug that dissolves the blood is injected into the reservoir of the damaged artery. This action is possible within six hours after blood flow stops.
- Non-selective thrombolysis – intravenous. This method takes even less time – 3 hours.
Thrombolysis for cerebral infarction (ischemic stroke)
Acute cerebrovascular accidents (ACVA), which provoke severe neurological disorders, are called stroke. The diagnosis of stroke sounds like a death sentence. In Russia. Half of the patients die, most of them within the first month. And you can’t envy the survivors - many remain helpless and disabled until the end of their days.
However, in countries that have been using TLT for many years, the statistics are different: no more than 20% of patients die. Many patients experience complete restoration of neurological function. And this is thanks to thrombolysis, the most effective treatment for ischemic stroke.
The TLT procedure is not very complicated - special enzymes are introduced into the vessel that can dissolve the blood clot. However, there are contraindications:
- Bleeding of various localizations. During TLT, all blood clots are dissolved in the vessels, and those that form as a result of bleeding are not excluded.
- Possible aortic dissection.
- Arterial hypertension.
- Intracranial tumors.
- Hemorrhagic stroke (hemorrhage caused by rupture of the walls of cerebral vessels).
- Liver diseases.
- Pregnancy.
- Brain surgeries.
The patient's age does not prevent thrombolytic therapy!
Among the listed contraindications, some are absolute, others are relative. The most important absolute contraindication is bleeding.
The implementation of thrombolysis may be hampered by the lack of necessary conditions: a computed tomograph, laboratory, neurointensive care unit. And most importantly, there may simply not be enough time. Three (maximum six) hours from the onset of the disease - this period must be met when carrying out thrombolytic therapy. This is the case when time is not money, but life! That’s why it’s so important to pay attention to the first signs of a stroke:
- Unilateral numbness of an arm or leg;
- Incoherent speech;
- Distorted face.
You can ask the person to stretch his arms forward and say something. If such a task turns out to be beyond his strength, immediately call an ambulance. Remember: the countdown has begun, and the patient doesn’t have enough of it!
Thrombolysis before hospitalization
Even a healthy person may show signs of impaired cerebral blood supply:
Decreased vision, cognitive functions;
These symptoms are a sign of the onset of the disease, especially if they occur in older people. In order not to miss fatal changes, you need to conduct the following studies:
Duplex scanning of the carotid arteries;
Ultrasound of cerebral vessels;
Study of coronary vessels;
MRI of the brain (indicated for patients with arterial hypertension, diabetes, obesity, heart failure).
When the first signs of thrombosis appear, it is important to start thrombolysis in a timely manner, without waiting for the onset of a heart attack or stroke. This measure reduces hospital mortality by 17-19%, because “the disease is easier to prevent than to treat.”
If thrombolytic therapy is available before hospitalization, it should be used. This requires qualified health workers and the ability to immediately conduct and interpret a cardiogram. Thrombolysis can be fully carried out within half an hour after examining the patient.
It is important to use thrombolytic therapy no later than 3-6 hours from the onset of the first symptoms. Delay in using TLT will lead to necrosis of myocardial cells and cessation of the functioning of medulla cells.
Author of the article: Volkov Dmitry Sergeevich | Ph.D. surgeon, phlebologist
Education: Moscow State Medical and Dental University (1996). In 2003, he received a diploma from the educational and scientific medical center for the administration of the President of the Russian Federation.
5 most effective homemade hair recipes!
10 natural remedies for arthritis that are scientifically proven to be effective
Heart and TLT
Any vessel in the body can become clogged, including the coronary artery. In this case, myocardial infarction develops. Of course, in a healthy body, the occurrence of a blood clot is unlikely. Usually this process is facilitated by general disorders. Among them: a reduction in the amount of anticoagulant components in the blood: heparin and fibrinolysin, an increase in the content of coagulation components. In addition, local disturbances appear in the vessel: the inner wall becomes rough, atherosclerotic plaques ulcerate, and blood flow slows down.
Just as in the case of a stroke with myocardial infarction, it is important to remove the clot in time and restore blood supply to the heart muscle. However, doctors are hesitant to carry out this procedure without a thorough examination of the patient, fearing negative consequences.
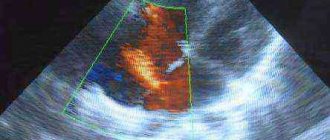
This examination includes duplex scanning, computed tomographic angiography, and Doppler examination. All this allows you to most accurately determine the location of the blood clot and inject the medicine directly into the affected vessel. With this approach, the risk of complications is reduced many times.
But still, sometimes, when the patient has no time left, even emergency doctors perform thrombolysis. Indeed, in such a case, delay is truly like death! Of course, this procedure should be carried out only by qualified specialists - a cardiology team. The duration of thrombolysis can vary from 10 minutes to two hours.
Thrombolytic therapy for myocardial infarction, as well as for stroke, has contraindications. And also the main obstacle is bleeding of any location.
The procedure for dissolving a blood clot is by no means a cheap pleasure. The cost of thrombolytics, especially imported ones, reaches $1000 per injection. But what could be more valuable than life?! Since this procedure is an emergency, the costs for it are included in the compulsory health insurance tariffs for the ambulance team.
Thrombolysis - what is it, types, indications and contraindications
The mysterious word thrombolysis sounds when choosing treatment for pulmonary embolism (PE), heart attack, stroke or some other types of thrombosis. But what kind of procedure is hidden behind this name? In order to understand the importance and necessity of such an intervention, let’s consider what thrombolytic therapy is and who needs it.
CONTENT:
What is this procedure
To understand what thrombolysis treatment is, let’s pay attention to the constituent words. The name stands for thrombus lysis.
In a healthy person, special blood enzymes are involved in the destruction of a blood clot, but in a number of diseases the protective forces fail and artificial or artificial thrombolysis is required.
The need for lysis or dissolution of thrombus formation occurs in the following cases:
- a broken blood clot completely blocks the lumen of the vessel, preventing blood supply to the tissues;
- the accumulation of blood clots impedes vascular blood flow.
Thrombolytic therapy aims to eliminate blood clots using medications. Agents that eliminate platelet aggregation are administered intravenously or inside a thrombosed vessel.
Types of thrombolysis
Depending on the site of administration of the drugs necessary for thrombolysis, doctors distinguish between systemic and local methods. Each method has disadvantages and advantages.
System
Thrombolytic drugs are administered to the patient into a vein in the elbow.
The advantages of the method are as follows:
- general blood thinning;
- the ability to dissolve a blood clot in a hard-to-reach area;
- ease of manipulation (can be performed both in a hospital setting and as first aid for acute thrombosis).
Disadvantages include the need to administer thrombolysis drugs in maximum therapeutic doses. Such medicinal effects negatively affect the general condition of the blood.
Local (selective)
Drugs that eliminate thrombosis are injected into the vessel where the blood clot is located.
Pros of introduction:
- the therapeutic effect is achieved in a short time;
- there is no need to administer large doses of medications;
- drugs have less effect on overall blood clotting;
- effective 6 hours after cessation of blood flow to tissues.
Selective thrombolysis has one drawback - a specially trained specialist is required to carry out the intervention. The procedure is performed by a doctor, inserting a catheter under the control of an ultrasound machine.
Thrombolytic treatment is also divided into types according to the properties of the administered medications:
- generalized (medicines with a broad spectrum of action are used);
- selective (use medications with a narrowly targeted effect).
Which method will be used is selected individually. The choice is influenced by the time elapsed since thrombosis, the nature of vascular disorders and many other factors.
Indications for thrombolysis
Any significant disturbances in blood flow caused by the formation of a blood clot inside a vessel.
Thrombolysis is indicated in the following cases:
- Myocardial infarction (AMI). Thrombolytic therapy for myocardial infarction is carried out to prevent the re-formation of blood clots and increase blood flow. Indications for thrombolysis in myocardial infarction are the first hours after the attack. If AMI occurred 6 or more hours ago, then thrombolytics are not administered, but medications with a blood-thinning effect from other groups are prescribed.
- Stroke. Thrombolysis for ischemic stroke is used relatively often. But for a stroke caused by a ruptured vessel (hemorrhagic), the procedure is not used due to the risk of increased bleeding.
- TELA. Pulmonary thrombosis is a life-threatening condition. With pulmonary embolism, blood circulation in the pulmonary circulation stops and the person dies from lack of oxygen. Indications for thrombolysis for pulmonary embolism are blockage of a pulmonary artery by a thrombus.
- Acute coronary syndrome (ACS). Most people mistakenly consider this term to be synonymous with myocardial infarction. But with ACS, not only the myocardium suffers: rhythm and hemodynamics are disrupted. The cause of coronary syndrome can be acute myocardial ischemia, an attack of unstable angina and some other cardiac disorders. Indications for thrombolysis in patients with ACS are related to the presence of a thrombus in the coronary arteries. A heart attack is considered a form of ACS.
- Acute forms of thrombophlebitis. In patients with acute venous thrombosis, thrombolysis can reduce the severity of the condition and improve blood flow in the extremities.
For thrombolytic therapy, indications relate to obstruction of veins or arteries due to blood clots. In addition to the listed conditions, it is possible to use thrombolytics for other diseases accompanied by the appearance of intravascular blood clots.
Contraindications to thrombolysis
When prescribing thrombolysis, the doctor takes into account indications and contraindications. Thrombolytic therapy is prohibited in the following cases:
- hypertensive crisis;
- recent operations (risk of internal bleeding at the surgical site);
- blood diseases;
- age over 70 years (vessels become fragile and hemorrhages may develop);
- the presence of benign or malignant neoplasms;
- tendency to bleeding (low blood clotting);
- diabetes;
- recent TBI (up to 2 weeks from the date of receipt);
- pregnancy;
- breast-feeding;
- ulcerative lesions of the digestive tract mucosa;
- aneurysm of any location;
- liver or kidney failure;
- individual intolerance to medications.
Even if the above contraindications are not identified, there are the following prohibitions for carrying out the procedure in acute conditions:
- With AMI. Conditional contraindications to thrombolysis for myocardial infarction are the presence of atherosclerosis in the patient or more than 6 hours have passed since the attack. Thrombolysis for a heart attack in these cases will be poorly effective.
- With ACS. Acute coronary syndrome occurs for various reasons, and a contraindication to thrombolytic therapy in patients with ACS is the absence of thrombosis.
- For a stroke. Thrombolysis therapy is not always necessary for patients with stroke. If it is undesirable to perform a procedure during an ischemic stroke, if a lot of time has passed since the attack, then thrombolysis for a hemorrhagic stroke is dangerous due to increased intracranial hemorrhage.
- With pulmonary embolism. There are no contraindications. With this pathology, there is a pronounced disturbance or complete cessation of pulmonary blood flow, and without medical assistance, pulmonary thromboembolism ends in death. Thrombolysis helps save lives.
But all contraindications are relative. Often, in severe cases, doctors use thrombolysis for pulmonary embolism or large heart attacks without specifying the list of prohibitions. This is due to the fact that the patient’s vital signs sharply deteriorate, and the administration of thrombolytics helps to avoid death.
Treatment methods
As mentioned earlier, there are systemic and selective methods of administering medications. Let's find out which method is better, taking into account the nature of the pathology that has arisen and how it is carried out.
System
They are considered universal. Systemic thrombolysis is done by administering lysing agents through a vein. Indicated in the following cases:
- for stroke;
- with a heart attack;
- with pulmonary embolism.
The convenience lies in the fact that assistance can be provided both in the hospital and at the pre-hospital stage. Clinical recommendations for therapy include monitoring ECG and blood clotting.
Selective
Another name is catheter thrombolysis. In this case, the doctor places a catheter in the vein or artery affected by thrombosis.
How the procedure is performed depends on the location of the blood clot:
- Local thrombolysis for a heart attack is done in the cardiac intensive care unit with an intravenous catheter. The method serves as an alternative to coronary bypass surgery.
- Selective thrombolysis for stroke is rarely performed due to the difficulty of accessing the cerebral arteries. Thrombolytic therapy for ischemic stroke using catheterization is possible only in clinics specializing in helping stroke patients.
- Vein thrombosis. With this pathology, lysis of blood clots is considered one of the simplest. The doctor injects the selected medication into a vein of the limb.
Which method to use is decided individually.
Catheterization of a thrombosed vessel makes it possible to more effectively eliminate the problem, and intravenous infusion of thrombolytics makes it possible to provide assistance more quickly and prevent complications.
Drugs for thrombolysis
Thrombolytic therapy for myocardial infarction, stroke or pulmonary embolism is carried out with various medications. Thrombolytic drugs are selected taking into account the nature of the pathology, but sometimes it is possible to use those drugs that are in the first aid kit (in the ambulance the list of drugs is limited). Let's consider popular drugs for thrombolysis:
- Streptokinase. A classic drug for dissolving blood clots, it is used for myocardial infarction or pulmonary embolism, and less commonly as thrombolytic therapy for ischemic stroke. In case of thrombosis, the medicine has a powerful lysing effect, but greatly thins the blood and increases the permeability of the vascular wall. Streptokinase is considered a thrombolytic with many side effects. Most often used for myocardial infarction and pulmonary embolism.
- Actilyse. Mechanism of action: thrombolytics and fibrinolytics. The components of the drug, reacting with fibrinogen, provoke lysis of the blood clot. Despite the fact that Actilyse is a second-generation thrombolytic drug, the drug produces few side effects and is often used in hospitals. Actilyse and other new generation drugs are considered the most popular products.
- Urokinase. In the 4th generation classification, it is considered a convenient drug for lysing blood clots. When used, it has few side effects, but is expensive.
- Fortelysin. Like Actilyse, it belongs to the second generation (this list of drugs is most popular for the treatment of thrombosis). Fortelysin is considered one of the best drugs for thrombolysis with a small number of adverse reactions.
The names of drugs from the group of 5th generation thrombolytics are not worth listing. These modern drugs have a minimum of contraindications, are well tolerated, but are expensive and are used only in large clinics.
There are no oral agents for thrombolysis - drugs are used only in injection solutions. But some patients mistakenly confuse thrombolytics and anticoagulants (Warfarin), which are available in tablets and are indicated for long-term use.
Ambulance with thrombolysis for emergencies
The system of emergency measures for ambulance workers contains the following clinical recommendations:
- TELA. If this condition occurs, therapy with thrombolysis agents is indicated, regardless of possible contraindications.
- Stroke. If there is no certainty about the nature of stroke lesions, then the administration of thrombolytics is undesirable. Recommendations for doctors and paramedics indicate that it is better to carry out supportive therapy to eliminate the risk of intracranial bleeding in hemorrhagic stroke.
- AMI. Thrombolysis for myocardial infarction at the prehospital stage will help in the first hours. If more than 6 hours have passed since the attack, then only the administration of narcotic analgesics and delivery of the patient to the hospital is recommended.
All appointments are made by a doctor, and, in some cases, by a paramedic. Before using thrombolysis at the prehospital stage, the possible benefits and harms to the patient are taken into account.
What are the complications?
Thrombolytics are considered “heavy” drugs for the human body. Let's consider common complications of thrombolytic therapy:
- fever up to 38° and above;
- acute failure of cardiac function;
- cerebral hemorrhagic hemorrhages (with ischemic stroke);
- heart rhythm disturbances;
- drug-induced hypotension;
- internal and external bleeding.
To avoid unwanted reactions, thrombolysis is carried out under the control of electrocardiography and blood clotting.
How is effectiveness assessed?
How much the procedure helps is assessed using MRI or Doppler ultrasound. Let's consider the main criteria for the effectiveness of thrombolysis:
- Zero. The drugs do not affect the blood clot.
- First. There is a slight lysis of the thrombus structure.
- Second. Blood flow appears, but the bloodstream is partially freed.
- Third. Maximum therapeutic effect - the bloodstream is fully functioning.
Whether thrombolysis is needed or not is decided individually. But if the procedure is necessary, then you should not refuse - resorption (lysis) of the blood clot will improve blood circulation and prevent complications of the disease.
: use of thrombolytic therapy by emergency doctors
Source: https://sosudyinfo.ru/bolezni/trombolizis.html
Methods of performing thrombolysis
Thrombolysis is carried out by two main methods:
- Systemic;
- Local.
The first method is advantageous in that the medicine can be injected into a vein without having any idea where the blood clot is hidden. With the bloodstream, the drug is carried throughout the entire blood circulation, where on its way it encounters an obstacle in the form of a blood clot and dissolves it. But systemic thrombolysis has a significant drawback: an increased dose of medication is required, and this is an additional burden on the entire circulatory system.
When performing local thrombolysis, the drug is injected directly into the location of the thrombus. The drug is supplied through a catheter, which is why the method is called catheter thrombolysis. However, this method is more difficult to implement than the first and is associated with a certain danger. During the procedure, the doctor monitors the movement of the catheter using x-rays. The advantage of this method is its low invasiveness. It is used even if the patient has a large number of chronic diseases.
What dissolves blood clots?
The main thrombolytics used when indications for thrombolysis are:
- Streptokinase. This medicine is the cheapest among thrombolytic drugs. A significant disadvantage of streptokinase is its incompatibility with the human body, which causes numerous allergic reactions. Also, a relatively short half-life suggests its long-term administration (60 minutes). And most importantly, when using streptokinase, numerous hemorrhagic side effects develop. All this served as a reason for the development of more modern thrombolytics.
- Urokinase. It is much more expensive, but its advantage over streptokinase has not yet been proven. Requires the administration of heparin into a vein. This protein was first discovered in human urine. But later it was isolated from other tissues and organs.
- Anistreplase. Expensive drug. It can be administered as a jet, which greatly facilitates its prehospital use. Injection of heparin into a vein is not required.
- Alteplase. Expensive medicine. With timely administration of the drug, patient survival is higher than in the case of streptokinase. Heparin therapy is required for a week. High risk of cerebral hemorrhage.
Indications for use
Indications for thrombolysis in myocardial infarction are:
- Prolonged (more than 20 minutes) anginal attack in the first 12 hours from its onset;
- ST segment elevation of 0.1 mV or more in two adjacent standard or 0.2 mV in adjacent pericardial ECG leads;
- Complete block of the left bundle branch, which occurred for the first time in the presence of pain.
TLT is indicated in conditions where it is not possible to conduct PCV within 90-120 minutes from the moment of first contact with the patient.
Thrombolysis in case of myocardial infarction has the right to be performed by a specialized cardiological ambulance team equipped with everything necessary to relieve possible complications.
Complications of TLT
- Bleeding. Both minor and very dangerous are possible.
- The contractile function of the heart muscle is impaired, which manifests itself as signs of heart failure.
- Hemorrhagic stroke. This complication may occur in elderly patients as a result of streptokinase use.
- Allergic reactions.
- Reperfusion arrhythmias. It is observed in almost half of patients.
- Reocclusion of the coronary artery. Occurs in 19% of patients.
- Arterial hypotension. Its connection with bleeding cannot be ruled out.
- Fever, rash, chills.
TLT at the prehospital stage
What signs suggest disorders in the blood vessels of the brain:
- Pain in the head;
- Dizziness;
- Decreased attention, vision, memory.
Who doesn't know these symptoms? At certain periods of life they can appear in completely healthy people. However, these same signs are observed at an early stage of cerebrovascular accident. To exclude this possibility and not miss strokes, every person in their fifties should undergo an annual ultrasound of the cerebral vessels, as well as duplex scanning of the carotid arteries.
In addition, it is a good idea to undergo an MRI of the brain - the most informative study. It is especially indicated for patients at risk: those suffering from diabetes, hypertension, atherosclerosis, obesity, and heart problems. A serious factor is physical inactivity and heredity (especially maternal). It is also useful to conduct a study of the coronary vessels.
If during the examination thrombosis of certain vessels is detected, the most correct solution would be thrombolysis. Stubborn statistics prove the effectiveness of this method. It has become an axiom that it is easier to prevent any disease than to treat it. Prehospital thrombolysis reduces mortality from strokes and heart attacks by up to 17%.
Thrombolytic therapy is preferable at the prehospital stage, subject to the availability of trained medical personnel, ambulance personnel, and the ability to interpret the ECG on site. In this case, TLT can begin within 30 minutes after meeting the patient.
Heart and thrombolysis
As a result of blockage of a coronary vessel by a thrombus, the patient experiences a myocardial infarction.
This process does not occur spontaneously; it is preceded by general disorders:
Slowing blood flow;
Reduction in the blood levels of heparin and fibrinolysin, which have an anticoagulant effect;
Increased content of blood clotting components;
Ulceration of atherosclerotic plaques;
Roughness of the inner wall of the vessel;
Slowing down blood flow, thickening it.
In case of myocardial infarction, in order to restore blood supply to the heart muscle, it is necessary to promptly remove the blood clot that has blocked the coronary vessel. If you do not conduct a thorough examination of the patient first, the procedure is fraught with complications.
Necessary studies to determine the location of the blood clot and specify the site for drug administration:
CT (computed tomography);
Ultrasound with Doppler study.
A comprehensive study helps to significantly reduce the risk of complications.
In urgent cases, the emergency cardiology team can perform thrombolysis on an emergency basis to save the patient’s life. The procedure takes from 10 minutes to 2 hours. Just as when relieving the consequences of a stroke, bleeding is the most important contraindication.
The cost of a set of drugs for thrombolytic therapy can reach up to 50-60 thousand rubles, but these costs are included in health insurance rates.
Panacea?
An impressive list of contraindications and complications of thrombolytic therapy indicates its careful use. This method should only be used in the most exceptional cases, when a person's life is at stake.
Important! Only early application of the method is effective: within 3 (maximum 6 hours) from the first “bells” of the disease.
Subsequently, the heart muscle or brain cells die. The use of thrombolysis in this case is not only useless, but even more extremely dangerous!
9.5. Thrombolytic drugs. Treatment regimens
Streptokinase, recombinant tissue plasminogen activator (alteplase) and its modification - tenecteplase, modified (recombinant) prourokinase (purolase®) are used as thrombolytic drugs.
Streptokinase
is administered intravenously at a dose of 1,500,000 IU over 30-60 minutes in a small amount of 0.9% sodium chloride solution. Coronary blood flow can be restored on average in 55% of cases.
When using streptokinase, especially insufficiently purified drugs, a decrease in blood pressure, bradycardia, anaphylactic reaction, even shock can be observed. Streptokinase is a protein foreign to the body; its administration causes the production of antibodies. This makes its repeated use after 5 days and in subsequent years ineffective and even dangerous. Streptokinase belongs to the so-called non-fibrin-specific thrombolytics. It leads to a more pronounced decrease in the level of fibrinogen in the general bloodstream than fibrin-specific (having an affinity for thrombus fibrin) drugs.
The advantage of recombinant tissue plasminogen activator and its derivatives, as well as Purolase, is the lack of antigenicity, which allows the drugs to be re-administered at any time as soon as the need arises, and the tropism towards thrombus fibrin, which increases the frequency of restoration of coronary blood flow when used before 70%. Recombinant tissue plasminogen activator (alteplase)
is administered intravenously (the drug is first dissolved in 100-200 ml of distilled water or 0.9% sodium chloride solution) according to the “bolus + infusion” scheme. The dose of the drug is 1 mg/kg BW (but not more than 100 mg). The bolus is 15 mg; subsequent infusion of 0.75 mg/kg MT over 30 minutes (but not more than 50 mg), then 0.5 mg/kg (but not more than 35 mg) over 60 minutes (total infusion duration 1.5 hours).
Tenecteplase difference
from alteplase in that a longer half-life from the body allows the drug to be used in the form of a single bolus, which is especially convenient for pre-hospital treatment. The dosage is determined by the patient’s BW: 30 mg for BW<60 kg, 35 mg for 60-70 kg, 40 mg for 70-80 kg; 45 mg at 80-90 kg and 50 mg at BW>90 kg.
Purolaza®4
is administered intravenously (the drug is first dissolved in 100-200 ml of distilled water or 0.9% sodium chloride solution) according to the “bolus + infusion” scheme. The bolus is 2,000,000 IU; subsequent infusion of 6,000,000 IU over 30-60 minutes.
Source: studfile.net
Methods of performing thrombolysis
Thrombolytic therapy (TLT, thrombolysis) is a type of pharmacological therapy aimed at restoring normal blood flow due to the dissolution (liquefaction) of a blood clot inside the vascular bed.
To find out how thrombolysis is performed, you need to know about TLT therapy methods:
- non-selective method - intravenous thrombolysis is carried out within 3 hours after hemodynamic slowdown by introducing blood-dissolving drugs into the damaged artery basin;
- selective - performed in the first 6 hours.
Depending on the location, there are different types of therapy for TLH:
- systemic - when thrombolytics are administered into a vein “blindly”, without having a real idea of the location of the thrombus;
- local - drugs are administered directly to the location of the blood clot.
Examples of stories about the use of thrombolysis therapy by emergency physicians are shown in Video 1 and Video 2.
Contraindications to thrombus lysis
Local and systemic thrombolysis is carried out with the use of thrombolytics: streptokinase, urokinase, anistreplase, alteplase.
In this case, thrombolytics dissolve blood clots in the vessels, converting plasminogen into active plasmin. This enzyme breaks down fibrin (the clotting component of a blood clot).
The main contraindications for thrombolytic therapy are an increased risk of bleeding of a traumatic or pathological nature in the six-month period preceding lysis of blood clots.
This is explained by the fact that during thrombolysis (thrombolytic therapy), a reaction occurs that dissolves blood clots in the body.
Often their liquefaction leads to the resumption of acute internal (gastrointestinal, pulmonary, uterine) bleeding, hematuria, as well as bleeding:
- due to surgery and injuries (including post-resuscitation) with damage to internal organs;
- in the presence of other conditions, the danger of which is associated with the development of hemorrhagic complications (acute pericarditis, pancreatitis, dissecting aortic aneurysm, history of intracranial tumors);
- with pathologies of blood clotting (thrombocytopenia, hemorrhagic diathesis);
- due to severe (chronic) arterial hypertension (BP > 200/120 mm);
- due to taking indirect anticoagulants.
This means that thrombolytics can also be used at older ages, if there are no contraindications to thrombolytic therapy in the medical history.
What dissolves blood clots?
The main indications for thrombolysis are cardiovascular diseases (stroke, heart attack, pulmonary thromboembolism, blockage of deep veins, peripheral artery or shunt, thrombolysis for ischemic stroke).
At the prehospital stage, indications for thrombolytic therapy include long-term transportation (more than half an hour) of the patient to the hospital or a forced delay in thrombolysis for more than 1 hour.
Indications for thrombolysis in a hospital setting:
- depression of the ST segment in leads V1-V2 with an increase (jump) in the amplitude of the R waves, which indicates tissue death in the region of the posterior wall of the left ventricle of the heart;
- rise of the ST segment above the level of 0.1 and 0.2 mV in at least 2 ECG leads;
- complete blockade of the His bundle (his left bundle branch), if 12 hours have not passed since the formation of the blood clot; unstable hemodynamics with maintaining the rate of ST rise on the ECG.
It is known that a blood clot is easy to dissolve if it is still fresh, therefore, in case of sudden blockage of blood vessels, thrombolysis drugs must be administered within the first 2 hours.
Thrombolytics significantly improve the prognosis if they are administered within the next 6 hours after the onset of the first symptoms (tingling, nagging pain in the chest, numbness, swelling of the lower extremities, as well as the appearance of sudden weakness, accompanied by difficulty speaking, impaired visual acuity).
In addition, survival may increase when thrombolytic drugs are administered at a later date (up to 24 hours).
Contraindications to TLT with them
Thrombolysis
Indications for thrombolysis ( elderly age is not a contraindication ) • ECG reveals a rise in the ST interval of more than 1 mm in two or more adjacent leads (if anterior MI is suspected) or in 2 of 3 limb leads II, III, avF (if anterior MI is suspected) to inferior MI), or the presence of LBBB (probably when subtotal coronary artery occlusion progresses to total), or idioventricular rhythm,
• first 6 hours of myocardial infarction. But if pain persists, ST segment elevation and the absence of the Q wave (when the myocardium is still alive), the first 12 hours are also “suitable”, if the MI has not ended and there is a “mosaic” clinical picture. The decision to perform thrombolysis after 12 hours is made on the basis of clinical pictures, anamnesis and ECG
Complications of TLH and taking neutralizing drugs
In medical practice, various types of complications are recorded during TLT. This:
- severe (gastrointestinal, intracranial, abdominal) - until the results of a blood test for hemoglobin and hematocrit, platelet level, etc. are obtained, it is urgent to stop administering thrombolytics and heparin, and stop taking aspirin. Test for thrombophilia.
- minor (from the puncture site, from the mouth or nasal) - if this occurs, it is necessary to apply pressure to the bleeding areas, and to prevent such bleeding, the number of invasive procedures should be reduced;
- bleeding:
- fever - according to statistics, occurs in 5% of patients taking thrombolytics; neutralizing drugs - aspirin or paracetamol;
- arterial hypotension (not to be confused with an allergic reaction!) - observed in 10-15% of patients taking streptokinase or anistreplase, therefore, as treatment, the doctor chooses infusion therapy with simultaneous cessation of thrombolytic drugs that cause complications;
- rash - can be observed in a third of patients taking streptokinase or anistreplase, therefore, as treatment, it is necessary to stop taking these thrombolytics, prescribe diphenhydramine and corticosteroids (in severe cases).
- chills - may occur as a reaction to the breakdown of the enzyme plasminogen; treatment with pethidine.
Source: medicinka.online
The essence of TLT is the drug destruction of the blood clot. It is ensured by the administration of drugs that activate endogenous fibrinolysis, which leads to the splitting of fibrin threads (fibrino- or thrombolytics). In the absence of contraindications, TLT should be performed in patients with STEMI, if the time from the onset of an anginal attack does not exceed 12 hours, and the ECG shows ST segment elevation >0.1 mV, in at least 2 consecutive chest leads or 2 consecutive limb leads, or LBP blockade appears. The administration of thrombolytics is justified at the same time with ECG signs of true posterior MI (high R waves in the right precordial leads and ST segment depression in leads V1-V4 with an upward T wave).
TLT reduces in-hospital mortality by an average of 21% compared with patients who did not receive it. The use of TLT allows saving an additional 30 lives for every 1 thousand patients treated in the first 6 hours of the disease, and 20 for every 1 thousand in the interval 7-12 hours *. The beneficial effects of TLT persist for at least the next 20 years.
If the EMS team has the ability to monitor the heart rhythm and perform electrical cardioversion, TLT should begin at the prehospital stage in the EMS car. At the same time, reducing the delay time before the start of treatment by an average of 1 hour can further reduce the probability of death in the next month by 17%.
Absolute contraindications to TLT:
• previous hemorrhagic stroke or cerebrovascular accident of unknown etiology;
• ischemic stroke suffered within the last 3 months;
• brain tumor, primary and metastases;
• suspicion of aortic dissection;
• presence of signs of bleeding or hemorrhagic diathesis (except for menstruation);
• significant closed head injuries in the last 3 months;
• changes in the structure of cerebral vessels, for example, arteriovenous malformation, arterial aneurysms.
Relative contraindications to TLT:
• history of persistent, high, poorly controlled hypertension;
the presence of poorly controlled hypertension (at the time of hospitalization - SBP >180 mm Hg, DBP >110 mm Hg);
• ischemic stroke >3 months old;
• dementia or intracranial pathology not listed in the “Absolute contraindications”;
• traumatic or prolonged (>10 min), cardiopulmonary resuscitation or major surgery suffered within the last 3 weeks;
• recent (within the previous 2-4 weeks) internal bleeding;
• puncture of a vessel that cannot be pressed;
• for streptokinase - administration of streptokinase, incl. modified, more than 5 days ago or known allergy to it;
• pregnancy;
• exacerbation of peptic ulcer;
• taking indirect anticoagulants (the higher the MHO, the higher the risk of bleeding).
TLT gives a beneficial effect regardless of the gender of the patient, concomitant diabetes, blood pressure (if SBP
Source: zakon.today
Thrombolysis for acute myocardial infarction
Cardiovascular diseases occupy first place in the general structure of pathology and are the cause of premature death among the population in more than 60% of cases.
Cardiovascular accidents (unstable angina, myocardial infarction) are especially dangerous due to their sudden onset, which is often accompanied by the development of life-threatening complications.
Therefore, it is worth starting highly qualified treatment as soon as possible, since the greatest losses occur in the first 2 hours of the disease.
The development of AMI (acute myocardial infarction) is based on intracoronary thrombosis at the site of a destabilized atherosclerotic plaque, which leads to cessation of blood supply and the development of necrosis of a portion of the heart muscle. This is a very fleeting process: within 60 minutes from the onset of ischemia, about 50% of cardiomyocytes in the affected area die.
Emergency care for AMI at the prehospital stage should be aimed at:
- adequate pain relief;
- resumption of patency of the damaged vessel, prevention of reocclusion (repeated cessation of blood circulation);
- maintaining the patency of the coronary arteries, reducing platelet aggregation;
- limiting the ischemic zone, preventing or eliminating complications.
What is thrombolysis and how is it performed?
Thrombolysis (TLT) is the process of dissolving a blood clot under the influence of an enzyme introduced into the systemic circulation, which causes destruction of the basis of the blood clot.
Drugs for TLT (tissue plasminogen activators) are divided into direct (Streptokinase) and indirect (Alteplase, Actilyse, Tenecteplase).
The mechanism of action of tPA is conventionally divided into 3 stages:
- Binding of the enzyme to plasminogen, which is located on fibrin (formation of a ternary complex);
- tPA promotes the penetration of plasminogen into fibrin, converting it into plasmin;
- The resulting plasmin breaks down fibrin into small fragments (destroys the blood clot).
There is a direct relationship between the time of initiation of TLT and the prognosis for the patient. The guidelines of the European Association of Cardiology indicate that thrombolysis should be performed up to 12 hours from the onset of the disease (further administration of the drug is not advisable).
The TLT procedure causes platelet activation and increases the concentration of free small blood clots. Therefore, TLT must be performed together with adjuvant antiplatelet therapy.
Tenecteplase is used for TLT at the prehospital stage. It is administered intravenously as a bolus (intravenous bolus, using a syringe) over 10 seconds. This is a third-generation tPA, which has a high safety profile (low risk of hemorrhagic and hemodynamic complications, allergic reactions), does not require specific storage conditions and is easy to use.
Alteplase is administered in a hospital setting. After administering 5 000 ml of heparin, 15 mg of the drug is administered as a bolus. Next, they switch to drip administration of 0.75 mg/kg over 30 minutes and 0.5 mg/kg over 60 minutes. The total dose is 100 mg. The entire procedure is carried out against the background of continuous heparin infusion.
Streptokinase is administered intravenously in a dosage of 1.5 million OD diluted in 100 ml of saline over 30-60 minutes. Before using the drug, a bolus of 5 thousand OD of heparin is administered, followed by resuming the infusion no earlier than 4 hours after the end of the administration of Streptokinase.
According to the order of the ministry, after TLT, the patient must be taken to a specialized hospital with the possibility of balloon angioplasty or stenting no later than 12 hours.
Indications for use
Indications for thrombolysis in myocardial infarction are:
- Prolonged (more than 20 minutes) anginal attack in the first 12 hours from its onset;
- ST segment elevation of 0.1 mV or more in two adjacent standard or 0.2 mV in adjacent pericardial ECG leads;
- Complete block of the left bundle branch, which occurred for the first time in the presence of pain.
TLT is indicated in conditions where it is not possible to conduct PCV within 90-120 minutes from the moment of first contact with the patient.
Thrombolysis in case of myocardial infarction has the right to be performed by a specialized cardiological ambulance team equipped with everything necessary to relieve possible complications.
Contraindications
Absolute contraindications to thrombolysis for myocardial infarction:
- Hemorrhagic stroke less than 6 months ago;
- History of TBI, surgery within 3 weeks;
- Gastrointestinal bleeding less than 1 month ago;
- Disorders of the blood coagulation system;
- Dissecting aortic aneurysm;
- Refractory arterial hypertension (SAT more than 200 mmHg, DAP more than 110 mmHg).
Relative contraindications:
- TIA less than 6 months ago;
- Systematic use of direct anticoagulants;
- Pregnancy, first 28 days after birth;
- Punctured vessels of large diameter inaccessible for compression;
- Long-term traumatic cardiopulmonary resuscitation;
- Recent laser therapy for fundus retinal diseases;
- Liver failure;
- Gastric ulcer in the acute stage;
- Infective endocarditis;
- Diabetic hemorrhagic retinopathy and other retinal hemorrhages.
The doctor is obliged to warn the patient about all possible contraindications and complications of the procedure. The patient confirms consent to TLT in writing in the thrombolysis protocol.
https://www.youtube.com/watch?v=7ghXSVoBLoE
Possible complications of thrombolytic therapy (occur in no more than 0.7% of cases):
- Parenchymal hemorrhages, bleeding at the injection site;
- Acute rhythm disturbances - atrial fibrillation is considered as an indicator of recanalization (restoration of blood circulation) of the vessel;
- Allergic reaction, fever.
Clinical criteria for successful reperfusion (resumption of oxygen supply) of the myocardium:
- Rapid regression of pain syndrome;
- Manifestations of reperfusion arrhythmias during thrombolytic administration;
- Involution of ECG changes (approximation of the ST segment to the isoline;
- Decrease in the level of cardiac-specific biochemical markers of necrosis.
The effectiveness of TLT is also affected by the time of day - recanalization occurs worse in the morning. At this time, platelet activity, coagulation processes, blood viscosity, vasomotor tone and natural inhibition of fibrinolysis have maximum daily indicators.
conclusions
Thrombolytic therapy is included in the list of standard measures when providing care to patients with acute coronary syndrome at the prehospital stage.
The use of TLT in the first hours from the onset of AMI symptoms can save patients with potentially necrotic myocardium, improve left ventricular function and reduce the mortality rate from AMI.
The risk of rethrombosis (re-occlusion) is reduced by the combination of thrombolysis with heparin therapy and long-term use of Aspirin.
The following sources of information were used to prepare the material.
Source: https://cardiograf.com/terapiya/medicamentoznoe/trombolizis-pri-infarkte-miocarda.html