Etiology of the disease
The thickening of the walls of the aorta of the heart occurs as a result of certain processes in the human body.
The main reasons for thickening of the aortic walls:
- Development of hypertension.
- Vascular atherosclerosis.
- Previous diseases that are transmitted through unprotected sexual intercourse.
- Past scarlet fever, measles.
- Smoking abuse.
- Foods with high cholesterol levels.
- Excessive consumption of alcoholic beverages.
- Viral infections.
- Genetic predisposition.
With the development of hypertension, when there is a constant increase in blood pressure, the vessels of the circulatory system experience excessive stress during blood flow, since blood passes through them under very high pressure.
The aorta, in turn, being the main conductor of blood, experiences pressure, which in case of hypertension unimaginably exceeds permissible norms.
With this constant state of affairs, the walls of the vessel begin to stretch and lose their former elasticity. Fibrous growths begin to form on the walls of the aorta, leading to their thickening, and, as a result, the entire aorta becomes thicker.
Another reason why the walls of the aorta and the aortic valve on the heart thicken is the physical changes in the human body caused by gradual aging. Patients age 55 years and older. Atherosclerosis, as a provoking factor in the development of this pathology, leads to the formation of cholesterol plaques, which lead to a gradual narrowing of the aortic walls.
Cholesterol plaques are one of the causes of aortic thickening
In children, this disease is caused by a genetic predisposition. There are cases when, as the child grew older, the pathology stopped its development, and a new round of the disease was observed in old age.
Aortic insufficiency
The frequency of detection of heart defects largely depends on the research methods used for diagnosis. The overall prevalence of aortic regurgitation was 4.9% in the Framingham Study and 10% in the Rigorous Heart Study, of which moderate to severe aortic regurgitation was 0.5 and 2.7%, respectively.
The most common cause recently is associated with disease (aneurysm) of the ascending aorta and bicuspid aortic valve, in 50% of cases the cause is degenerative changes in the aortic valve. Rarer causes may be rheumatism (15%), atherosclerosis, infective endocarditis (8%).
According to the severity, initial aortic insufficiency is distinguished (regurgitation volume 60 ml per contraction, regurgitation fraction
Degenerative changes in the walls of the aorta, leading to their expansion, are dangerous due to sudden rupture of the aorta and severe bleeding with the possibility of death.
Aortic aneurysm is degenerative changes in the walls of the aorta, leading to their expansion. The prevalence of the disease is higher in men.
Types of Aortic Aneurysm
- Thoracic aneurysm;
- arch aneurysm;
- abdominal aneurysm.
Groups and risk factors for aortic aneurysm
- Male gender;
- age over 40 years;
- hereditary predisposition;
- sedentary lifestyle;
- smoking.
Causes of aortic aneurysm
- Hereditary predisposition;
- hypertension;
- arteriosclerosis;
- late stage syphilis;
- vascular injuries;
- blood clots in blood vessels.
Symptoms of aortic aneurysm
At first, the disease is asymptomatic, but in the later stages pressing pain may be detected in different parts of the body.
For thoracic aortic aneurysm:
- pain in the heart area;
- dyspnea;
- hoarseness of voice.
For an abdominal aortic aneurysm:
- pain in the abdomen and lower back;
- feeling of heart pulsation in the stomach.
Symptoms of a ruptured aneurysm:
Diagnosis of aortic aneurysm
- Radiography;
- ultrasonography;
- Magnetic resonance imaging;
- angiography (vascular examination).
Treatment of aortic aneurysm If the aneurysm reaches a large size or grows rapidly, surgical intervention is indicated: the damaged section of the vessel is removed and replaced with an artificial canal or vessel from another part of the body.
Prognosis The danger of the disease lies in the possibility of sudden rupture of the aorta and severe bleeding with a high probability of death. Death can occur within minutes. The probability of aortic rupture directly depends on the size of the aneurysm: with an aneurysm diameter greater than 6 cm, the probability of its rupture within 10 years reaches 50%. When emergency medical measures are taken in the event of a ruptured aneurysm, 50% of patients survive.
Symptoms of manifestation
Symptoms of thickening of the aortic walls of the aortic valve leaflets are manifested in the following:
- Disorders of the central nervous system.
- Digestive disorders.
- Dizziness.
- Headache.
- Decreased concentration.
- Problems with mental functioning.
- Memory impairment.
- Pain in lower extremities.
- Sudden lameness in one leg.
- Pain when walking.
- Chronic fatigue.
- Increased irritation.
- Chest pain.
- Combat syndrome in the abdominal area.
- Rapid weight loss.
- There are leg cramps.
Symptoms of aortic disease are not pronounced in the initial stages of the process of wall thickening. The patient begins to notice some changes in the functioning of his body only when the pathology has already started irreversible processes and led to disruption of the functioning of internal organs. Signs will depend on the location of the aorta that has been damaged.
Compaction of the walls of the aorta at the root of the blood vessel leads to angina pectoris and myocardial infarction. In case of insufficient blood circulation through the circulatory system of the brain, it leads to disturbances in the functioning of the central nervous system, the patient begins to experience severe headaches, dizziness, and character changes. The person becomes extremely irritable and gets tired quickly.
Pathologies of the heart muscle in young people are becoming more common, which is explained by smoking and drinking alcoholic beverages.
If you have bad habits, the thickening of the aortic wall with their further peeling is provoked by harmful tars that are contained in nicotine smoke.
The aorta in the abdomen, through which blood flows to the legs, causes intermittent claudication. As a rule, a person begins to limp on the left or right leg. The symptom is accompanied by sudden convulsive muscle contractions, the process of walking becomes painful.
For the gastrointestinal tract, compaction of the aorta manifests itself in the form of pain in the thoracic region, disruption of the digestion process, and a rapid decrease in body weight. In especially severe cases, peritonitis begins to develop.
Anatomical compaction of the walls of the aorta of the heart
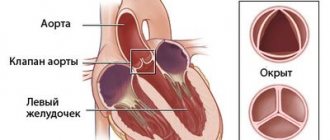
Causes of formation, symptoms and methods of treating aortic stenosis
Aortic stenosis is a reduction in the valve opening. Against the background of this narrowing, the flow of blood from the left ventricle to the heart is significantly limited. This disease is the most common heart defect.
Often the disease progresses in patients who have crossed the sixty-year threshold.
Deformations of the aortic valve leaflets can provoke the appearance of pathology. This happens eighty-five percent of the time. And only in ten percent of cases the root cause of the disease is the process of rheumatization.
general information
Aortic stenosis that has not been acquired is considered separately by doctors. The presence of a congenital anomaly leads to an increase in the load on the left ventricle.
Provoking factors
There are a considerable number of reasons that provoke the development of aortic stenosis. The most common reasons for which the disease develops include:
- Congenital cardiac anomaly.
- Deposition of calcium salts on the aortic valve.
- Rheumatic process.
Features of congenital anomaly
Congenital aortic stenosis should be considered a pathology when a baby is born with a pre-existing abnormal process in the actual valve. This is a fairly rare pathology. A bicuspid valve is no less rare. When a person is in childhood, the anomaly has no consequences. A completely different picture is observed in adult patients. Due to the narrowing of the valve, a person often needs to have it replaced.
When is calcium deposited?
Over time, calcium salts are deposited on the walls of the heart valves. This element is found in human blood, being dissolved. As a person ages, salts deposit on the valves.
In this case, the manifestations of a serious disease do not make themselves felt until the person reaches the age of seventy.
Diagnostic examination
Considering the fact that the symptoms of thickened aortic walls do not appear immediately, the patient begins to notice the first signs when the disease has already progressed. In some cases, pathology is detected during a routine medical examination, using fluorography.
Ultrasound of the heart
To clarify the diagnosis, ultrasound of the heart muscle, circulatory system and contrast angiography of blood vessels are performed. For people who have a genetic predisposition to diseases of the cardiovascular system, heart diagnostics should be carried out once a year.
Causes
Its reasons may be:
- congenital valve changes;
- fusion of the valves as a result of an inflammatory process (rheumatic fever, infective endocarditis, syphilis, etc.);
- additional formations on the valves that limit their mobility (usually these are calcifications, less often - healed vegetation).
Short description
Aortic valve stenosis is a heart defect in the form of narrowing of the aortic opening due to pathology of the aortic valve and perivalvular structures.
Frequency • Isolated aortic valve stenosis - 1.5–2% of acquired valve defects; Aortic valve stenosis in combination with other defects - 23% • Congenital aortic stenosis - 3–5.5% of all congenital heart defects; in combination with other congenital disorders - 13% • The predominant gender is male.
Treatment methods
If it is possible to identify the disease at the initial stage of development, the method of continuous monitoring over time is used. The patient needs to go on a diet, reduce the amount of foods that contain cholesterol, and stop smoking and drinking alcoholic beverages.
Cholesterol-free foods
The diet should not include fatty and smoked foods, too hot or peppery; it is not recommended to eat sweets and flour products. It is prohibited to consume carbonated drinks.
Moderate exercise and long walks are recommended. Before choosing a type of physical activity, you should consult with your doctor to determine whether it is permissible to engage in certain physical activities.
The patient is highly recommended to avoid exciting and stressful situations. If necessary, a course of specialized medications is prescribed. This type of therapy is applicable only in the absence of disease progression.
If the disease develops rapidly, surgery is necessary. If the heart valves are severely damaged, it is necessary to replace them with a prosthesis or perform plastic correction of the thickened walls. If the heart muscle is damaged due to circulatory problems, it is replaced with a donor organ.
Folk remedies
The use of traditional medicine methods can only be used after consultation with your doctor. Quite often, a raw food diet or vegetarianism is practiced, herbal medicine, massage and the use of freshly squeezed juices are used, which will help lower blood cholesterol levels.
Refusing to eat meat products in favor of a raw food diet or vegetarianism is only possible on the advice of a nutritionist and your doctor. If you have problems with the gastrointestinal tract, it is strictly prohibited to engage in a raw food diet.
The patient is prescribed medications to relieve the root cause of the pathological phenomenon. If the thickening of the walls of the heart was caused by hypertension, it is necessary to constantly monitor blood pressure and, if necessary, correct it with medications, reducing the pressure on the walls of the main blood vessel.
Treatment of hardening of the aortic walls of the heart can give the desired effect only with an integrated approach and the patient observing a healthy lifestyle and giving up all bad habits.
The aorta is the largest vessel in the human body, through which oxygenated blood is distributed to smaller arteries. It is directly connected to the left ventricle of the heart, and the flow of arterial blood into it is controlled by the operation of the muscular valve. The compaction of the walls of the aorta and the cusps of the aortic valve impedes the flow of blood, which causes rapid wear and tear of the heart and insufficient blood supply to all organs and systems.
Arterial hypertension
Chronic increase in pressure leads to loss of elasticity of the vascular walls. Compensatoryly, the vascular endothelium becomes rigid and thickens due to fibrous growths.
Aortocardiosclerosis
Provoking environmental factors (poor nutrition, obesity, physical inactivity) lead to an increase in cholesterol levels in the blood. It can deposit on the wall of the aorta and heart valves. Over time, portal plaques thicken and significantly narrow the space for blood circulation.
Acute rheumatic fever has many manifestations, one of which is bacterial carditis and valvulitis with subsequent thickening of the mitral or aortic valve.
Endocarditis and myocarditis
Inflammation of the muscular or inner epithelial layer of the heart also leads to scarring at the level of the valves and aortic ring.
Narrowing of the lumen between the left ventricle and the aorta leads to the following clinical picture:
- attacks of dizziness, even fainting, associated with minor physical activity;
- shortness of breath, attacks of suffocation;
- fast fatiguability,
- attacks of angina pectoris (pain behind the sternum of aching or burning nature).
For a long time, aortic stenosis is asymptomatic; severe symptoms appear when the opening narrows by more than 70%.
Symptoms of the disease are associated with the localization of the pathological process:
- when the lumen of the aortic root narrows, insufficient blood supply to the heart muscle occurs, this is manifested by the development of typical angina pectoris, including acute myocardial infarction;
- if the ascending part and arch of the aorta are compacted, neurological symptoms appear (headache, dizziness, weakness, fatigue, etc.);
- thickening of the descending aorta leads to malnutrition of the lower body and the development of intermittent claudication, acute abdominal pain, etc.
Stenosis of the aortic mouth (aortic stenosis) and all its features
general information
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Aortic stenosis (aortic stenosis) is one of the most common heart defects in modern society. It is diagnosed in every fifth patient over the age of 55, and 80% of patients are men.
In patients with this diagnosis, there is a narrowing of the aortic valve opening, which leads to disruption of blood flow into the aorta from the left ventricle. As a result, the heart has to make significant efforts to pump blood into the aorta through the reduced opening, which causes serious problems in its functioning.
Causes and risk factors
Aortic stenosis can be congenital (occurs as a result of intrauterine developmental anomalies), but more often it develops during a person’s life. The causes of the disease include:
- heart disease of a rheumatoid nature, which usually occurs as a consequence of acute rheumatic fever due to infections caused by a certain group of viruses (group A hemolytic streptococci);
- atherosclerosis of the aorta and valve - a disorder that is associated with lipid metabolism disorders and cholesterol deposition in the vessels and valve leaflets;
- degenerative changes in heart valves;
- infective endocarditis.
Classification and stages
Aortic stenosis has several forms, which are distinguished according to different criteria (localization, degree of blood flow compensation, degree of narrowing of the aortic opening).
- according to the location of the narrowing, aortic stenosis can be valvular, supravalvular or subvalvular;
- by the degree of blood flow compensation (by how much the heart can cope with the increased load) - compensated and decompensated;
- According to the degree of narrowing of the aorta, moderate, severe and critical forms are distinguished.
The course of aortic stenosis is characterized by five stages:
- Stage I (full compensation). There are no complaints or manifestations; the defect can only be determined through special studies.
- Stage II (hidden insufficiency of blood flow). The patient is concerned about mild malaise and increased fatigue, and signs of left ventricular hypertrophy are determined by x-ray and ECG.
- Stage III (relative coronary insufficiency). Chest pain, fainting and other clinical manifestations appear, the heart increases in size due to the left ventricle, and the ECG shows its hypertrophy, accompanied by signs of coronary insufficiency.
- Stage IV (severe left ventricular failure). Complaints of severe malaise, congestion in the lungs and a significant enlargement of the left heart.
- Stage V, or terminal. Patients experience progressive failure of both the left and right ventricles.
See more about the disease in this animation:
Is this scary? Danger and complications
The quality and life expectancy of a patient with aortic stenosis depends on the stage of the disease and the severity of clinical signs. People with a compensated form without severe symptoms do not have a direct threat to life, but the symptoms of left ventricular hypertrophy are considered prognostically unfavorable.
In patients with the “classic triad” (angina, syncope, heart failure), life expectancy rarely exceeds five years. In addition, in the later stages of the disease there is a high risk of sudden death - approximately 25% of patients diagnosed with aortic stenosis die suddenly from fatal ventricular arrhythmias (usually these include people with severe symptoms).
The most common complications of the disease include:
- chronic and acute left ventricular failure;
- myocardial infarction;
- atrioventcular block (comparatively rare, but can also lead to sudden death);
- swelling and congestion in the lungs;
- systemic emboli caused by calcium particles from the valve can cause strokes and visual impairment.
Symptoms
Often, signs of aortic stenosis do not appear for a long time. Among the symptoms that are characteristic of this disease are:
- Shortness of breath. Initially, it appears only after physical exertion and is completely absent at rest. Over time, shortness of breath occurs in a calm state and intensifies in stressful situations.
- Chest pain. Often they do not have an exact localization and appear mainly in the heart area. The sensations can be pressing or stabbing in nature, last no more than 5 minutes and intensify with physical activity and stress. Angina pain (acute, radiating to the arm, shoulder, under the shoulder blade) can be observed even before the appearance of pronounced symptoms and is the first signal of the development of the disease.
- Fainting. Usually observed during physical activity, less often - in a calm state.
- Rapid heartbeat and dizziness.
- Severe fatigue, decreased performance, weakness.
- A feeling of suffocation, which may become worse when lying down.
When should you see a doctor?
Often the disease is diagnosed accidentally (during preventive examinations) or in the later stages due to the fact that patients attribute symptoms to overwork, stress or adolescence.
Diagnostics
Diagnosis of stenosis of the defect is complex and includes the following methods:
- Anamnesis collection. Analysis of patient complaints, past illnesses and family history (cases of heart disease or sudden death in close relatives).
- External inspection. Patients have pallor and cyanosis of the skin, heart murmurs and wheezing in the lungs, and the peripheral pulse in the radial arteries is weak and rare.
- Auscultation of aortic stenosis. The method involves listening to the sounds and rhythms of the heart - with aortic stenosis, the second sound is usually weakened or completely absent, and systolic and diastolic murmurs are also noted.
- General blood analysis. It is carried out to determine the level of red blood cells, platelets, leukocytes, as well as the level of hemoglobin.
- General urine analysis. Makes it possible to identify disorders that may affect the course of the disease.
- Electrocardiography. A method for assessing the electrical activity of the heart, allowing to identify disturbances in its functioning.
- Echocardiography. An ultrasound examination that determines the degree of narrowing of the aorta and the most significant indicators of heart function.
- Coronary angiography with aortography. An invasive procedure that involves penetrating the vessels of the arms and legs to examine the vessels of the heart and aorta.
- Exercise tests. Exercise tests include walking, exercise bike and treadmill tests.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
Treatment methods
There is no specific therapy for aortic stenosis, so treatment tactics are selected based on the stage of the disease and the severity of symptoms. In any case, the patient must register with a cardiologist and be under strict supervision. It is recommended to undergo an ECG every six months, give up bad habits, diet and a strict daily routine.
Patients with stages I and II of the disease are prescribed drug therapy aimed at normalizing blood pressure, eliminating arrhythmia and slowing the progression of stenosis. It usually includes taking diuretics, cardiac glycosides, and drugs that lower blood pressure and heart rate.
Radical methods for the initial stages of aortic stenosis include cardiac surgery. Balloon valvuloplasty (a special balloon is inserted into the aortic opening, after which it is inflated mechanically) is considered a temporary and ineffective procedure, after which in most cases a relapse occurs.
In childhood, doctors usually resort to valvuloplasty (surgical valve repair) or Ross operation (transplantation of the pulmonary valve to the position of the aorta).
At stages III and IV of aortic stenosis, conservative drug treatment does not give the desired effect, so patients undergo aortic valve replacement. After surgery, the patient must take blood thinners for the rest of his life, which prevent the formation of blood clots.
Prevention
There are no methods to prevent congenital aortic stenosis or to diagnose it in utero.
Preventive measures for acquired defects include a healthy lifestyle, moderate physical activity and timely treatment of diseases that can provoke narrowing of the aorta (rheumatic heart disease, acute rheumatic fever).
Any heart disease, including aortic stenosis, is potentially life-threatening. To prevent the development of heart pathologies and defects, it is very important to take a responsible attitude towards your health and lifestyle, as well as regularly undergo preventive examinations, which can detect diseases at the initial stages of their development.
Diagnostics
If one or more of the complaints listed above occur, you should consult a doctor for further examination.
Visual inspection
During inspection, pay attention to the following:
- characteristic pallor (also called “aortic”): due to a decrease in cardiac output, peripheral capillaries narrow to redistribute blood to the central channel;
- shortness of breath with minimal physical activity – with severe disruption of blood flow;
- acrocyanosis (blueness of the tip of the nose, lips) - not always;
- rarely swelling of the lower extremities.
Physical examination methods
Additionally, the doctor assesses the state of the cardiovascular system using the following diagnostic measures:
- palpation – intensification and displacement of the apex impulse down and to the left (V-Vl intercostal space along the midclavicular line);
- percussion – displacement of the relative dullness of the heart to the left;
- Auscultation – the appearance of a rough noise in the systole phase, weakening of the ll tone over the aorta, moist rales are possible over the surface of the lungs due to left ventricular failure;
- blood pressure measurement - hypotension.
Development of atherosclerosis of the aorta
The first reason for the development of atherosclerosis, including aortic one, is a violation of lipid metabolism in the body, when low-density lipoproteins predominate over high-density lipoproteins, and a large amount of triglycerides in the cholesterol molecule.
Low molecular weight lipids penetrate into the choroid, and a lipid (cholesterol) spot appears in it, which has a viscous and elastic shape. At this stage of development of atherosclerosis, it is possible to completely dissolve these plaques with the help of a therapeutic process without damaging the bloodstream system.
Next, the lipid plaque thickens, and calcium molecules attach to it, and a dense atherosclerotic plaque begins to form on the aorta.
The vessel loses its elasticity, and the plaque closes the lumen of the vascular bed for the normal passage of blood through it.
The danger of lipid plaques lies not only in the fact that they can completely close the lumen of the aorta and cause occlusion, but also in the fact that they have the ability to peel off from the choroid and cause clogging of the arteries, leading to ischemia of the organ whose artery is affected by thrombosis.
Aortic dissection
Development of aortic valve calcification
Calcification of the heart valves is a precursor to diseases such as heart failure, generalized atherosclerosis, stroke, heart attack, etc. Typically, calcification of the aortic valve develops against the background of degenerative processes occurring in its tissues, caused by rheumatic valvulitis. On the wrinkled, welded edges of the valve leaflets, shapeless calcareous growths form, blocking the mouth of the aorta. In some cases, calcification can involve the wall of the left ventricle, the anterior valvular leaflet, and the septum between the ventricles located in close proximity.
The disease has several stages:
- At the initial stage, hyperfunction of the left ventricle is noted. It promotes complete emptying. Therefore, dilatation (stretching) of its cavity does not occur. This condition can last for quite a long time. But the possibilities of hyperfunction are not limitless and the next stage begins.
- Each time more and more blood remains in the LV cavity. Due to this, its diastolic (during the period of excitation) filling requires a larger volume. And the ventricle begins to expand, that is, its tonogenic dilatation occurs. This in turn causes increased contraction of the LV.
- The next stage is myogenic dilatation, caused by weakening of the myocardium, which is the cause of aortic insufficiency (stenosis).
senile (top) and bicuspid stenosis (bottom) of the aortic valve due to calcification
Calcification of the AC is detected during radiography. It is clearly visible on an oblique projection. On echocardiography, calcification is recorded in the form of a huge number of high-intensity echo signals.
Since aortic circulatory insufficiency is compensated for a long time, the person feels completely healthy. He has no clinical manifestations of the disease. Heart failure occurs unexpectedly (for the patient) and begins to progress rapidly. Death occurs on average 6 and a half years from the onset of severe symptoms. The only effective treatment for this defect is surgery.