Svetlana Shcherbakova
Cardiologist
Higher education:
Cardiologist
Kabardino-Balkarian State University named after. HM. Berbekova, Faculty of Medicine (KBSU) Level of education – Specialist 1994-2000
Additional education:
“Cardiology”
State Educational Institution “Institute for Advanced Training of Physicians” of the Ministry of Health and Social Development of Chuvashia
Contacts
Carrying out an MRI for stroke is practically the only way to detect the disease even in its most acute stage. Of course, not everyone can undergo this procedure. If the patient has metal implants, then it is prohibited, because exposure to a magnetic field causes their movement and temperature changes. A similar ban applies to hearing aids, pacemakers, posts and vinyls. In other cases, MRI is permitted.
Diagnostic approaches
Stroke is one of the most dangerous diseases that leads to death. However, the first signs of stroke can most often be suspected without the participation of a doctor. If you notice strange behavior in a person on the street, do not immediately blame everything on alcohol intoxication. Check if he is conscious. Ask him to smile and raise both hands. Ask his first name, last name, today's date. If the patient does not smell of alcohol, but is confused, finish testing.
Signs of stroke : he has an asymmetrical smile, he cannot raise and hold one of his arms. If you notice these symptoms, call an ambulance immediately. Perhaps it is your immediate reaction that will save a life.
Principles of diagnosis for acute stroke
If a stroke is suspected, doctors conduct a whole range of examinations in the hospital. Of course, the key changes are problems with the brain. They can be detected by MRI or CT scan. It is neuroimaging that should be performed 40 minutes after the arrival of a patient with suspected stroke at the hospital.
However, even this expensive examination is not always effective. In the first hours after an attack, it is rarely possible to detect foci of changes in the brain. An important aspect is dynamic monitoring of the patient.
The second organ that is subject to mandatory testing is the heart. Its work affects the blood supply to the brain. Any organic pathology can disrupt its functions. Therefore, the following set of examinations is carried out: taking a 12-lead electrocardiogram; ECHO-CG with determination of expansion of the heart chambers and the presence of blood clots, if necessary, Holter.
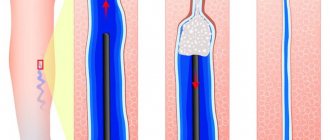
Much attention should be paid to the vessels of the neck and brain. In order to detect critical stenoses and microemboli, the carotid system (external and internal carotid arteries) is examined. It is possible to conduct transcranial Dopplerography, which additionally evaluates the blood flow of the cerebral system.
Blood tests indicate indirect changes due to a stroke. In addition, there are indicators that are important for predicting the outcome of an attack. They also need to be defined. This is a general analysis, hemostasiogram, glucose level, analysis of acid-base balance, homocysteine, etc.
There are also specific markers of stroke and transient ischemic attack. These are neurospecific enolase, brain-derived neurotrophic factor, protein S-100, sialylated carbohydrate antigen KL-6, superoxide dismutase. Unfortunately, due to the high cost of the examination, they have not become widespread in clinical practice.
Imaging for stroke
Why is an MRI or CT scan performed for a stroke? What goals do they pursue? What questions can the attending physician help answer?
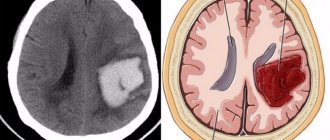
The main goal of imaging is to rule out bleeding, swelling, or other brain damage. This will allow you to quickly change treatment tactics and not harm the patient. Tomography allows you to determine dead tissue and the “penumbra” zone.
The penumbra is the zone of “clinical death” of neurons. Here their metabolism is significantly disrupted by the attack. But they have the potential to recover. Together with the necrosis zone, they form an ischemic focus of the brain.
The last task is to identify stenosis or occlusion of an extra- or intracranial vessel. This will determine the further tactics of patient management (conservatively or surgically).
The hypodense zone is a focus of irreversible necrosis. It is visible on MRI and CT within 6 hours from the onset of the attack. The essence of the phenomenon is that cytotoxic edema forms in dead cells. It is caused by a malfunction of the sodium-potassium pump due to a lack of ATP. Therefore, an increase in the amount of water in a cell by 1% leads to significant changes in the tomogram (reduces brain density by 2.5 Housefield units).
Approaches
So, the main approaches to diagnosing stroke:
- Physical examination;
- Neuroimaging;
- Analyzes;
- Other examination methods.
A physical examination is performed by a neurologist. It tests consciousness, reflexes, memory, and the patient’s ability to navigate the world around him. Even a layman can perform a physical examination. There is a “IMPACT” rule for this.
- U - ask the person to smile . With a stroke, asymmetry of the facial muscles can be observed;
- D – movement . Ask the person to raise their hands and hold them in front of them. During a stroke, the patient cannot move the limb on the affected side;
- A – articulation . Ask the person to give their first name, last name, and home address. With a stroke, speech will be slurred and confused;
- R – solution . If there are positive signs of stroke, call an ambulance.
Approaches used depending on type
Ischemic stroke accounts for 70% of all neurological pathologies. But it also has its own flow characteristics. Let's figure out how approaches to diagnosis differ for different types of stroke.
Atherothrombotic
It accounts for about 66% of all seizures. In this case, gross disturbances are formed in the basins of the affected arteries. CT and MRI are used to diagnose the disease. The lesion is visible on the tomogram within 3-6 hours from the onset of the attack.
Cardioembolic
It develops when an embolus enters, which “flies” from plaques of the carotid arteries or from thrombi of the heart chambers during fibrillation. It accounts for about 20% of seizures. Diagnostic approaches: CT or MRI to detect ischemic lesions. Duplex scanning of neck vessels and transcranial Dopplerography to clarify the location of the embolus. In addition, it is necessary to perform an ultrasound of the heart.
Lacunar
When several small vessels are affected, a lesion or lacuna is formed in the brain. It can be detected using CT data. The lacunar lesion has clear contours and is localized in the white matter or basal ganglia.
Other types of strokes
As a rule, they account for about 10% of attacks. Most often, such patients have a history of leukemia, erythremia, coagulopathy, and autoimmune vasculitis. For diagnosis, it is important to conduct brain imaging and profile tests to assess the severity of the underlying disease.
Subarachnoid hemorrhages
This type of lesion can produce a clinical picture similar to that of a stroke. Therefore, it is important to promptly distinguish between ischemic lesions and hemorrhage. Without this, doctors do not have the right to prescribe specific treatment for ischemic stroke.
There is a characteristic picture for subarachnoid hemorrhage, which is noticeable from the first minutes during a CT scan. No specific studies are required, but a few days after SAH, it is more effective to use MRI. The clinic also uses lumbar puncture. Red blood cells are found in it in large quantities. It allows you to identify SAH in the absence of CT data and timely distinguish it from meningitis or encephalitis.
Acute hypertensive encephalopathy
Occurs in less than 1% of cases. It is characterized by neurological syndromes, as in stroke, against the background of a progressive hypertensive crisis. Diagnosis consists of ophthalmoscopy, blood pressure measurement, laboratory and instrumental tests and neuroimaging.
As a rule, in the early stages of OGE there are no signs of brain damage. However, the picture may be nonspecific if “old” ischemic foci are activated against the background of hypertension. In this case, attacks of fresh disorders can only be detected on MRI in diffusion-weighted images.
What is the procedure for suspected stroke?
If a patient is hospitalized with a suspected stroke, no matter what type, then, one way or another, he will be examined using an MRI scanner.
At the same time, it is important that the person’s state is as calm and peaceful as possible, and that no sudden movements or shaking are made. The patient is taken on a gurney to the MRI diagnostic room, changed into comfortable clothes that do not contain metal elements, including fasteners, locks, and buttons.
Then the patient is placed on a retractable horizontal table, the tomograph is closed and the scanners are turned on. During this time, ventilation and fresh air supply are turned on in the MRI machine. The procedure can be interrupted at any time; in this case, the patient has a sensor in his hand, when squeezed, the doctor receives a signal. There is always a nurse nearby, ready to help if the patient vomits or has a nosebleed.
Diagnostics are carried out for a long time - from 40 to 65 minutes. Most often, before an MRI, the patient is injected with a contrast agent, as this improves visualization and gives a chance to see the smallest changes in the brain tissue.
Complete decoding of MRI images takes several hours, but lesions caused by a stroke are immediately visible.
For the patient, MRI of the brain is an absolutely painless procedure. In this case, a stroke produces its own symptoms and the patient may become ill from them. The doctor sees and hears everything that happens in the tomograph.
After a magnetic scan within a few hours, the diagnostician deciphers the images and gives a description of them, after which the attending physician makes an accurate diagnosis, confirms the type of stroke or refutes it, pointing out, for example, developing multiple sclerosis. After clarifying the diagnosis, treatment or surgery is prescribed, after which an MRI may be needed again.
Stroke is one of the most insidious diseases of our time. Its danger lies in its suddenness, however, it is still possible to prevent or predict such a condition, even if you monitor your blood pressure and undergo medical examination and medical examination on time.
Magnetic resonance imaging is not necessary in all clinical cases of pathology. If symptoms are obvious, there are signs of a stroke in one of the cerebral hemispheres, and the patient’s medical history and visual examination data correspond, the diagnosis is established without special primary diagnosis.
However, in some cases, MRI is required. Indications for its implementation are:
- vague symptoms of stroke;
- discrepancy between the patient’s examination data and his medical history;
- suspicion of cerebellar damage or lacunar damage (limited to a small volume of brain tissue located in the deep parts of the hemispheres).
Magnetic resonance imaging is also performed to study the vascular bed of the brain after a stroke, assess the volume of edema or hematoma, and clarify the size of the area of necrosis.
An MRI may be prescribed for the following symptoms:
- Strong headache;
- dizziness, loss of consciousness;
- nausea, vomiting due to pain;
- speech dysfunction;
- numbness and cramps of the limbs, loss of facial sensitivity;
- loss of coordination, spasm or decreased muscle tone;
- noise in ears;
- general weakness, inhibited reaction.
The contrast and visibility of lesions on tomography directly depends on the method of examining the brain. The following MRI techniques are used to obtain images:
- standard (proton-weighted);
- diffusion-weighted;
- perfusion-weighted;
- MR angiography with contrast.
The diffusion-weighted tomography method is based on the study of metabolism (movement of matter) in areas of brain tissue. By clearly delineating areas of reduced metabolism, it allows you to identify areas of irreversible tissue damage and areas that are subject to restoration with intensive therapy (penumbra zones).
The perfusion-weighted technique involves studying the blood supply in various areas of the brain. Deviation from the norm in the direction of decreased blood supply is a diagnostic criterion for stroke.
Magnetic resonance angiography is a study aimed at visualizing cerebral vascular pathologies.
Stages of stroke by time
Temporal classification is based on the speed of biochemical reactions that occur in the cell of dead neurons. It is this that guides clinicians in choosing possible diagnostic methods.
The most acute period
This period lasts from the onset of the attack and during the first 6 hours. It is suitable for initiating thrombolysis and other interventional techniques. To determine the lesion, diffusion-weighted modes are used on MRI, MR angiography, and CTA. These studies make it possible to determine the presence of a lesion, the localization of a blood clot in the artery, and the possibilities of interventional therapy.
Acute phase
Lasts at least 24 hours from the moment of the attack. During this phase, a CT examination is performed to exclude hemorrhagic stroke. An ischemic lesion may not be visible on neuroimaging.
Given the late delivery and the impossibility of performing interventional techniques, other extensive examinations are not performed. Recommended MRI over time after 12-24 hours, monitoring of laboratory blood parameters, acid-base balance. The heart is examined to identify arrhythmias, fibrillation, and other cardiogenic complications
Subacute phase
Lasts from the first day to the first 6 weeks from the attack. Stroke can be detected by MRI. After 5 days, the lesion is visible in almost any scanning mode. Examination of brachiocephalic vessels, pressure monitoring, ECG, and general clinical examinations are required.
Chronic phase
At this stage, the focus of necrosis is replaced by connective tissue. Changes will be noticeable on CT and MRI. During this phase, the patient has already been discharged from the hospital and is undergoing rehabilitation. Changes in the visualization picture remain forever. It is important to distinguish them from “fresh” lesions during new attacks.
Does an MRI always show a stroke?
Magnetic resonance imaging performed on modern equipment will show a stroke even in the first 1-2 hours after its occurrence. The diffusion-weighted imaging technique is particularly effective in diagnosing the disease. With its help, you can notice changes in the brain that occur 5 minutes after a circulatory disorder.
The accuracy of the tomography result depends on the stage of the stroke, its type and the chosen research technique.
Due to its low sensitivity, MRI is an auxiliary method in the diagnosis of hemorrhages, which account for up to 20% of all stroke cases. In addition, to study brain tissue in the most acute stage of pathology, it is necessary to use a strictly diffusion-weighted technique, because Standard MRI fails to detect up to 30% of ischemic cases.
CT or MRI: what to choose
The decision to conduct a specific study is made by the attending physician. It is based on clinical protocols, hospital capabilities, patient condition and other points. If a stroke patient is not taken to the hospital, there is a direct threat to his life. You should remember this when scheduling your own examinations.
| CT | MRI | |
| Accuracy | Allows you to diagnose hemorrhagic changes in the brain | Makes it possible to determine the focus of ischemia in DWI mode on the first day after the attack. Effective in brain research. |
| Price | 2-3,000 rubles | 3-4,000 rubles (price without contrast) |
| Duration | 10-20 minutes | Up to 30 minutes |
| Applicability | Radiation exposure | Virtually no restrictions in use |
| Contraindications | Relative | Presence of foreign metal parts (implants, prostheses) |
Changes on MRI in the early and late recovery period
During the recovery period, the dead area of tissue is organized with the formation of cystic or glial degeneration. Partial restoration of functions is ensured by the development of alternative neural networks; cells located in the nuclear zone do not recover after a stroke. MRI of the brain is performed in case of sudden deterioration of the condition or to predict rehabilitation potential.
In the early recovery period, MRI scans show gradually decreasing areas of ischemia; changes associated with tissue edema disappear along the periphery of the area. By the beginning of the late recovery period, a cystic cavity, glial or mixed foci may form in the stroke area. If the lesion proceeded as a minor stroke and by 21 days after the onset of the disease there was complete recovery, changes on MRI after the stroke are weakly expressed or may be completely absent.
MRI after stroke
The main task of MRI after an attack is to confirm or refute the presence of a stroke and exclude other pathologies (tumor, inflammatory process, hematoma). It is also important to identify the hemorrhagic process in a timely manner. It radically changes the tactics of patient management (thrombolysis is contraindicated for them).
MRI techniques:
- Diffusion-weighted images (used for early detection of ischemia);
- T1 and T2 weighted images (used to diagnose chronic and subacute hemorrhages);
- MR angiography is performed in patients with regressing neurological pathology. It is necessary to identify urgent indications for surgical intervention.
What is DWI?
The MRI image reflects the distribution of hydrogen atoms in tissues and their magnetic environment in the layer. MRI can create a functional or anatomical image. In the first case, the process of tissue change is visualized. The second is the exact location of structures and organs.
Diffusion-weighted images reflect the process of diffusion of liquid molecules in cells and intercellular space.
Interesting! By diffusion, scientists mean the passive movement of molecules along a concentration gradient.
When damage occurs in the brain tissue, cytostatic edema forms in the first minutes. The level of ATP, the energy component of the cell, decreases. Sodium-potassium channels on the neuron membrane stop working.
The liquid enters the cytoplasm without resistance, leading to an increase in volume and further death of the structure. Since the MRI machine in DWI mode is capable of recording the flow of liquid (after all, water contains hydrogen atoms that are registered in a magnetic field), after scanning the brain, you can get a picture of the initial ischemic focus.
Thus, the device registers changes in cells at the biochemical level. As a result, it is possible to assess cerebral ischemia within a few minutes from the onset of clinical symptoms. Cytostatic edema persists for 5-7 hours. Further, its interpretation is impossible, because a zone of necrosis is formed.
So, the DWI mode is used to assess acute cerebral ischemia in the first 5-7 hours from the start of the neurological clinic. It is ineffective in the late period of stroke.
T1-weighted images
They are obtained using a standard tissue relaxation sequence. This is the ability of hydrogen's magnetic field to return from one direction to another.
Because different tissues in the brain have different densities, they will appear differently on T1. So, fat has a denser structure compared to liquid. The fat in such pictures looks bright, and the liquid looks dark. Blood deserves special attention.
Methemoglobin (subacute hemorrhage after 3 days) has a bright color and a hyperintense signal, in contrast to the acute hemorrhagic process. Thus, diagnosis between fresh and old hematoma can be based on comparison of T1 and T2 weighted images. This interpretation of MRI significantly influences the tactics of the attending physician.
T2-weighted images
Another type of image is called T2. Its peculiarity is that the picture is obtained by recording transverse or spin-spin relaxation. Their physical characteristics are different from T1. Distinctive features of T2 images: fluids are bright, adipose tissue is intermediately bright. The white matter of the brain is dark gray, and the gray matter is light gray.
Flair
To clarify the nature of the pathology, sequences are used in which a certain component is suppressed. For example, Flair sequence or fluid attenuation inversion recover allows you to eliminate the influence of fluid on the image. The signal is fixed in such a way that the visualization from the liquid component of the tissue is erased and not recorded. In this case, dense pathology will be visible better.
The Flair sequence is used to detect infarction, meningitis, subarachnoid hemorrhage, multiple sclerosis, and traumatic brain injury.
SWI
The technique uses the difference in sensitivity between tissues. Thanks to gradient echo scanning, images are obtained with increased contrast and high sensitivity to venous blood. Hemorrhages and areas of iron accumulation are clearly visible on them.
Use of SWI: search for small pinpoint bleeding, diagnosis of tumors, vascular diseases. For example, accurate scanning for Alzheimer's disease, minor strokes or heart attacks, multiple sclerosis.
IDK cards
The measured diffusion coefficient is a quantitative indicator that characterizes the movement of water molecules in tissue. It is calculated from diffuse-weighted images. For calculations, a special computer application is used, which presents the image in the form of a map.
Main areas of application: research of the central nervous system. In particular, diagnosis of acute ischemic stroke, differential diagnosis of brain tumors, infectious processes.
Can an MRI fail to show a stroke?
A stroke is accompanied by toxic swelling of cells. Diffusion-weighted images are more sensitive to it. IDC maps may show a hypointense signal after a few minutes of stroke. They are more specific to the diffusion of hydrogen protons into cells. Therefore, a typical ischemic, hemorrhagic and cardioembolic attack is visible on MRI in more than 95% of cases.
However, in the history of magnetic resonance imaging there are several documented cases of stroke that were not visible on the machine. We were talking about lacunar strokes, ischemic processes in the vertebrobasilar region and the brain stem. The reason for this has not been established. But the first changes in the tomograms appeared only 24 hours after the attack.
T1, T2 and Flair sequences are used as aids for diagnosing stroke. In them, in the first minutes after symptoms, the picture of stroke is invisible. Therefore, if the study was performed using these sequences, acute stroke may not have been detected.
Preparation and procedure
No special preparation is required to perform an MRI of the brain. The patient is often admitted to the hospital in serious condition and the study is carried out for emergency reasons. It is important that the attending physician clarifies the following points before starting the procedure:
- Does the patient have metal products in his organs and tissues (hemostatic clips, joint prostheses, staples). They are a relative contraindication to the study and degrade image quality;
- MRI is also contraindicated for patients with electrical stimulators, valve prostheses, and drug pumps;
- Does the patient suffer from claustrophobia? If the answer is positive, the patient is sedated;
- The patient's high weight may be a contraindication. The “old” model tomographs are designed for patients up to 125 kg, while the “new” devices have a maximum weight of up to 200 kg.
How is the procedure performed?
Before the procedure, it is recommended to remove all items containing metal (glasses, watches, chains). The procedure takes 40-60 minutes. Before the examination, you should visit the toilet.
The doctor will warn you that you must lie still in the MRI machine. Any fluctuations will degrade the quality of the pictures. In addition, a constant “knocking” sound is heard in the pipe. For labile patients, it may cause premature completion of the examination. Therefore, relaxing music is often played in patient rooms, headphones are used, and light sedatives are used.
What does it look like?
The initial manifestations of a stroke are clearly visible on IDK maps and DWI images. In the first case, after the first minutes of the attack, a hypointense signal appears on the maps. On DWI, cytotoxic edema is indicated by high signal intensity.
Signs of ischemic stroke (acute period)
| T1 | Isointense signal (no focus detected) |
| T2 | Isointense signal (only large lesions are visible) |
| Flair | Signal intensity varies |
| DWI | High signal intensity |
| IDK cards | Low signal intensity |
Hemorrhagic stroke
| Can be recognized on MRI within the first 12 hours after an attack |
| Signal hyperintensity noted on Flair images |
Cardioembolic stroke
Has symptoms similar to ischemic stroke. When performing angiocontrast, you can see the cause of acute stenosis of the vessel - embolus.
Lacunar stroke
| T1 | Hypointense signal |
| T2 | Hyperintense signal |
| Flair | Hyperintense signal |
| DWI | Diffusion limitation |
Stages of stroke
- Early acute stroke (0 to 6 hours)
Optimal detection modes are IDK and DWI cards. With the first option, the signal intensity decreases, and with the second, it increases. Flair mode usually has high signal intensity.
- Late acute (6 to 24 hours)
| T1 | Low signal intensity 16 hours after stroke onset |
| T2 | High signal intensity 8 hours after stroke onset |
| Flair | High signal intensity |
| DWI | High signal intensity |
| IDK cards | Low signal intensity |
At this stage, the stroke may not be visible on CT/MRI.
- Early subacute period (from 24 hours to 1 week)
| T1 | Low signal intensity, hyperintensity with cortical necrosis |
| T2 | High signal intensity |
| Flair | Normal signal intensity |
| DWI | High signal intensity |
| IDK cards | Low signal intensity |
This is the stage of contrast accumulation and the formation of a fogging effect.
- Chronic (phase begins after 3 weeks)
It is characterized by resorption (resorption) and scarring (replacement of a focus of connective tissue).
| T1 | Low signal intensity |
| T2 | High signal intensity |
| Flair | The signal is decreasing |
MR angiography
In rare cases, for ischemic stroke and transient attack, MRI with angiography and contrast is used. The purpose of the study is to clarify the nature and localization of vessel occlusion for further surgical treatment. This may be intracranial thrombus extraction or other techniques.
MR angiography uses a bolus of intravenous contrast. When filling the vessel with the drug, a series of photographs are taken. An image is obtained that allows you to create a 3D reconstruction of the circle of Willis, intracranial veins, and carotid basin. The tomogram will show where the blood flow is disrupted.
Pathogenesis: description of cerebral infarction
Extensive neuronal ischemia rapidly depletes intracellular adenosine triphosphate (ATP), leading to the destruction of membrane-bound ionic polypeptides responsible for neuronal membrane activity and the generation of electrical impulses. This metabolic aberration leads to the accumulation of intracellular ions, creating cytotoxic edema.
Endothelial cells in the head are more resistant to ischemia than nerve and neuroglial cells. Approximately 3-4 hours after the onset of a heart attack, the integrity of the biological barrier is disrupted, and plasma proteins penetrate into the extracellular space. Vasogenic edema occurs, this process begins 8 hours after the onset of a heart attack and reaches a maximum 1-2 days after the onset of apoplexy. Reperfusion can also cause a hemorrhagic complication of cerebral infarction.
Important! MRI scan changes in ischemic apoplexy and cyst can be very similar. Therefore, it is definitely recommended to conduct a repeat MRI or additional examinations for differential diagnosis. If the diagnosis is incorrect, the doctor will not be able to treat the patient correctly.
Computed tomography in the diagnosis of ischemic stroke
In case of stroke of ischemic type, CT plays a supporting role and allows to exclude hemorrhagic conditions, trauma and subarachnoid bleeding. The ischemic zone is not visible in the first hours and weeks after the attack. CT also makes it possible to differentiate between “old” focal brain lesions and new ones (when compared with the MRI picture).
Will it show?
If acute stroke is suspected, CT is performed to exclude hemorrhage and if MRI is unavailable. Early signs of ischemia appear as:
- Obscuration of lenticular nuclei;
- Pointed increase in MCA density;
- Hyperdense SMA;
- Reduced differentiation of the insular cortex.
Late signs of ischemia (after 1 month):
- Zone of hypodensity in the parenchyma of the brain.
These signs are indirect and can only suggest a diagnosis of ischemic stroke. An objective picture appears after a few weeks.
Comparison of different types of stroke
| Type of stroke | Signs on CT |
| Ischemic | There is no clear picture of ischemic damage in the acute period of the disease. The presence of a stroke can be judged only by indirect signs. Should be performed to exclude intracranial hemorrhages. |
| Hemorrhagic | CT is used to diagnose hemorrhages. It represents an area of increased density on the tomogram. It is usually surrounded by perifocal changes of low density, which are formed due to edema. |
| Cardioembolic | Not visible on CT in the early stages |
| Lacunar | The most acute period is characterized by the formation of a hypodensity zone without even boundaries. The usual localization is in the zone of perforating vessels of the distal parts of the brain. In the late period, a clear hypodense focus with cerebrospinal fluid density is visible. |
Preparation and procedure
No preliminary preparation is required to perform a CT scan of the brain. The only negative point: during a CT scan the patient is exposed to radiation. However, modern spiral computed tomographs make it possible to monitor it. Single or double scanning does not lead to consequences for the patient’s body.
There are no absolute contraindications for the examination. Particular caution should be exercised when referring pregnant women and young children for CT scanning. The potential benefits and risks of this procedure should be assessed.
The examination itself lasts several minutes. The patient lies down on a table that moves towards the tomograph frame. During the examination, the patient does not experience claustrophobia. After all, there is enough free space inside the frame.
CT with angiocontrast provides more information for the treating physician. However, contrast agents contain iodine. As a result of their administration, allergic reactions, including anaphylactic shock, are not uncommon. The patient is obliged to warn the attending physician in advance about an allergic reaction to contrast, if it has happened before. In the case of initial administration, the treatment room is equipped with a special anti-shock arrangement. It will help medical personnel cope with any type of allergic reaction.
What does the disease look like on a CT scan?
| Type of stroke | |
| Ischemic | Not visualized in the acute period |
| Hemorrhagic | An area of increased density with perifocal edema, without edema in the chronic phase |
| Cardioembolic | Not visualized in the acute period |
| Lacunar | Hypodense zone without boundaries |
CT and angiography
CT angiography (CTA) allows you to evaluate the condition of not only the soft tissues of the brain, but also the bloodstream. The study accurately determines the location of vascular thrombosis, aneurysmal changes, and vascular malformations. All these pathologies are indications for CTA. In case of stroke, it is performed before a planned invasive intervention or before thrombolysis.
The patient may have contraindications for CTA:
- This is an allergic reaction to iodinated contrast agents;
- Kidney failure;
- Diabetes mellitus with decompensation;
- Pregnancy;
- Multiple myeloma;
- Acute heart failure.
To conduct the study, contrast is administered intravenously. After this, the usual scanning procedure is carried out. The images are processed with a special program that allows you to create a three-dimensional image of the blood vessels of the brain.
Contraindications to MRI in neurology
Contraindications for MRI:
- Metal implants,
- Claustrophobia,
- Pacemakers, although new protocols allow imaging in selected cases,
- MR-incompatible prosthetic heart valves,
- Allergy to contrast agent,
- Severe obesity.
Patients with metal implants may experience many potential complications, such as pacemaker failure and related consequences. For patients with a metal prosthesis, it is recommended to check its compatibility with MRI.
Cliustrophobic patients are unable to complete an MRI scan. In selected patients, gentle sedation or imaging in an open MRI system may be attempted. However, most open MRI scanners provide lower quality images.
In rare cases, patients may be allergic to a special substance (such as gadolinium) used in MRI. If any of these contraindications are present for stroke, a computed tomography (CT) scan of the brain is prescribed.
Analyzes
Imaging techniques play a major role in diagnosis. But they are of no value without a clinical picture of the disease and tests. What laboratory parameters indicate the presence of a stroke? What markers are needed to monitor the life activity of a sick person?
Laboratory examination of blood: general analysis, biochemical
In the first minutes after arrival at the hospital, it is important to perform laboratory diagnostics of the following indicators:
| General blood analysis | Platelet level |
| Blood for sugar | General glycemia |
| Hemostasiogram | Activated partial thromboplastin time (aPTT) indicates defects in the coagulation system; International normalized ratio (INR). |
After this, laboratory monitoring of indicators is carried out daily. Basic tests:
| General blood test with formula and ESR |
| General urine analysis |
| Detailed hemostasiogram (aPTT, INR, D-dimers, prothrombin index, thrombin) |
| Biochemical analysis (total protein, alate, asate, urea, creatinine, sodium, chlorine, potassium, C-reactive protein and homocysteine) |
| Determination of acid-base status |
| Determination of oxygenation (pulse oximetry) |
ECG
An important diagnostic factor is a 12-lead ECG. Any cardiac pathology can cause a stroke or aggravate the course of this disease. Main problems:
- Decrease in the ST segment as an indicator of myocardial ischemia;
- Heart rhythm disturbances in the form of arrhythmias and blockades;
- Detection of atrial fibrillation (severe chronic form of arrhythmia).
Lumbar puncture
Spinal puncture is rarely used to diagnose ischemic stroke. It was used quite widely in the past, when MRI and CT machines were not available. Therefore, its use in modern medicine is limited.
The puncture is carried out:
- If you suspect meningitis or encephalitis;
- For diagnosing stroke in the absence of neuroimaging. The presence of blood in the punctate indicates a hemorrhagic process, subarachnoid hemorrhage, or injury.
Ultrasound scanning with Doppler
This study assesses blood flow through the carotid system. Often the source of cardioembolic stroke is an atherosclerotic plaque. It can be detected by performing ultrasound with Doppler ultrasound. Scanning of the brachiocephalic vessels allows us to find critical stenosis, which can also provoke cerebral ischemia.
Arterial pressure
Blood pressure monitoring is performed in all patients with suspected stroke. The numbers should not exceed 140/90-150/100 mmHg. Pressure is determined constantly in intensive care conditions. When transferred to the general ward, diagnostics are carried out 2-3 times a day. If the numbers are consistently high, a consultation with a cardiologist is required to change the treatment regimen for hypertension.
Chest X-ray
A chest x-ray is performed upon admission to the hospital of any patient. This procedure allows you to exclude severe respiratory pathology. And also to identify advanced foci of the tuberculosis process. This test has no clinical significance for diagnosing stroke.
Ultrasound of the heart
For a deeper diagnosis of cardiac pathology (presence of dilatation of the heart chambers, intracavitary blood clots), a cardiac ECHO is performed. It allows for a more thorough and in-depth study of cardiogenic pathology. After all, it is often she who provokes stroke.
Specific tests for stroke
Homocysteine is an important indicator for predicting the severity of stroke. Homocysteinemia indicates occlusive damage to the blood vessels of the brain and is a more important marker than cholesterol. The analysis is necessarily carried out in case of ischemic stroke. Homocysteine levels can also be used to monitor the patient’s condition after a TIA.
Features of MRI data in acute cerebral circulatory disorders
All information received by medical personnel during the study differs depending on the period of illness. It is presented in the most understandable form in the table below.
| Data from the hyperacute period (up to 24 hours from the moment of attack) | The scans clearly show ischemic changes in the tissues. Allows you to estimate the size of the area deprived of blood supply. |
| Acute phase data (up to 7 days) | Scans can reveal increasing tissue swelling. The attending physician will be able to assess the mass effect. |
| Subacute period data (up to 21 days) | Scans can reveal a decrease in tissue swelling and mass effect. |
| Chronic phase data (after 21 days) | The scans reveal a decrease in tissue swelling. It is possible to determine the degree of damage to brain cells and use the information obtained to make a preliminary prognosis for the restoration of functions. |
Before performing the procedure, the doctor must find out about the patient whether he has metal implants and various electrical devices. The procedure cannot be performed after thrombolysis, because During MRI, doctors will not be able to monitor the clinical condition of patients.
Checking for stroke
Symptoms of stroke are quite specific. And when they appear, you need to immediately go to the hospital. But how to recognize a stroke without special sophisticated equipment? The task of the average person is not to establish an accurate topical diagnosis. A person without medical education should simply be able to distinguish dangerous signs that require immediate medical attention. There are several simple tests for this. Let's tell you more about them.
FAST test for stroke
In English it sounds like Face-Arm-Speech Test . Or face-hand-speech test. The name makes clear the main signs that you should pay attention to.
Face . With a stroke, asymmetry of the facial muscles is revealed. When the patient smiles, the corner of his mouth droops.
Hand . The patient is asked to raise both upper limbs upward. On the side opposite to the lesion, movement is weakened or impossible.
Speech . The patient has slurred, unclear speech. To do this, ask them to say a simple phrase.
If you identify at least one symptom from the list, you should immediately call an ambulance.
other methods
In addition to the above symptoms, the patient may experience the following changes:
- Impaired consciousness. The patient falls, while breathing and blood circulation are normal;
- Difficulties with orientation in space;
- Memory loss. He forgets everything that happened to him in the next few hours;
- Sharp headache. Does not respond to pills and leads to vomiting;
- Loss of sensation in half of the body;
- Loss of muscle strength in the limbs.
Differential diagnosis of stroke
- The patient is admitted to the hospital with focal neurological symptoms;
- A neurologist examines him and collects anamnesis.
| Anamnesis | Ischemic stroke | Hemorrhagic stroke |
| The ischemic type includes lacunar and cardioembolic | And also SAC | |
| The onset of the disease is gradual, symptoms appear at night and in the morning | Acute onset after physical or emotional stress |
There is a history of ischemic stroke and changes in the blood vessels of the brain. A typical picture is a man or woman over 60 years of age suffering from hypertension and/or diabetes. There is a high level of cholesterol and atherosclerotic damage to the brachiocephalic vessels, as well as concomitant cardiac pathology. There is usually no history of hemorrhagic stroke. The patient is young.
Next, the doctor conducts an objective examination.
| Objectively | Ischemic | Hemorrhagic |
| Appearance | Without features. Lethargy and pallor of the skin. | Increased sweating, facial flushing, redness of the sclera. |
| Headache, nausea, vomiting | Rarely | Often |
| Focal symptoms | Expressed | Absent in SAH |
| Impaired consciousness | Slow shutdown | Sudden fainting, stupor, coma |
| HELL | High numbers | Rarely |
| Hemiparesis | Often from the onset of an attack | Rarely |
| Rigid neck muscles, meningeal signs | No | Often |
| Speech Impairment | Often | Rarely |
- After the examination, the patient is sent for a CT/MRI to clarify the diagnosis. At the same time, the characteristic signs of stroke, which were mentioned above, are revealed. The issue of patient management tactics should be decided immediately: conservatively, thrombolysis, surgery. In the latter case, MR (CT) angiography is additionally required to clarify the location and degree of vessel stenosis.
- Laboratory and instrumental diagnostics are of auxiliary importance.
Formulation of diagnosis
The diagnosis of acute stroke reflects the following criteria:
- Type of stroke (stroke of ischemic type);
- Arterial basin or topical localization (in the MCA basin);
- Type of stroke (lacunar, cardioembolic);
- From what date (date);
- Primary or repeated.
Additionally, complications (cerebral edema) and underlying diseases (coronary artery disease, hypertension) are indicated.
What is the procedure for suspected stroke?
Diagnosis of stroke using MRI is performed in the following sequence:
- After the patient arrives at the hospital, the doctor differentiates the symptoms of a stroke from similar signs of other pathologies (for example, hypoglycemia).
- All metal structures are removed from the patient. The presence of non-removable steel objects and devices in the patient’s body may be a contraindication to the procedure.
- If there are no contraindications to MRI, the patient is placed on the tomograph table, his head is fixed during the procedure, and he is pushed into the tunnel. To perform MR angiography, the patient is first injected with contrast agents – gadolinium preparations.
- Using high and ultra-high fields, we study and obtain images of the brain in various projections.
After the procedure, a diagnostician analyzes the images obtained and describes pathological changes for further treatment of the patient in intensive care units.
The area of study for various tomography techniques is: the structure, metabolism and blood supply of brain tissue or the lumen of blood vessels supplying nutrients to the probable affected area.
To prescribe and conduct a magnetic scan, the patient must have certain complaints and symptoms. There are cases when it is possible to determine a stroke without diagnostic methods, for example, all the obvious signs are present, however, there are diseases that occur with symptoms similar to a stroke, which can mislead the doctor.
Indications for diagnostics using a tomograph are:
- severe headaches;
- nausea, vomiting due to migraines;
- severe dizziness;
- memory impairment;
- speech dysfunctions;
- numbness of body parts;
- noise in ears;
- spasms of the body or limbs;
- lethargy, weakness;
- loss of consciousness;
- coma.
MRI of the brain in case of stroke is necessarily performed using contrast.
Like any procedure, magnetic resonance imaging has its contraindications. But it is worth understanding that in each specific case they are individual and there are many conditions under which it is still possible to perform an MRI.
Diagnostics will be contraindicated in the following cases:
- when there are metal objects in the body, and there is no way to remove them during the procedure (implants, clips, prostheses, clamps, pins);
- the subject has installed electronic mechanisms that cannot be removed (pacemaker, insulin pump, ventilator, neurostimulator, artificial kidney, implanted hearing aid);
- the patient is unable to hold himself still for a long time (convulsions, panic attacks, epilepsy, nervous conditions);
- pronounced claustrophobia (fear of being in a confined space);
- the patient is overweight (over 125 kg);
- allergic reactions to the components of the drug (with contrast-enhanced tomography);
- acute cardiac and acute renal failure.
Under some conditions, MRI can be performed with the patient under anesthesia; this eliminates a number of contraindications. In addition, modern medicine offers scanning options using advanced devices, such as vertical and open tomographs. This contributes to an increase in permitted examination cases.
Topical diagnosis of stroke
| Arterial pool | Clinic | Localization |
| Anterior cerebral artery (ACA) | Leg-predominant hemiparesis, urinary incontinence, confusion | Hemiparesis on the right with lesions of the LPMA, on the left with lesions of the PPMA |
| Middle cerebral artery (MCA) | Weakness and disturbance of all kinds of sensation, more pronounced in the arm than in the leg. Hyperreflexia. | If PSMA is affected, the clinic is on the left; if the left is affected, the clinic is on the right |
| Posterior cerebral artery (PCA) | Loss of half the visual field on the opposite side, amnesia, paresis of 3 pairs of cranial nerves (CN) | If there is a lesion on the left, the clinic is on the right |
| Stroke in the trunk area | The arm is bent, the leg is extended. Oculomotor nerve palsy. | Clinic on the limbs on the opposite side, lesion of the 3rd pair of cranial nerves on the side of the stroke |
Topical diagnosis of stroke without CT or MRI imaging is difficult. It can only be carried out by professionals. Sometimes the clinical picture and neuroimaging picture are different. This suggests that the processes of neuron death and restoration are not fully understood by modern medicine.
Hemorrhagic transformation of ischemic stroke
Hemorrhagic transformation is an effusion of hemorrhagic contents into the brain tissue against the background of a picture of a true ischemic stroke. It occurs with extensive, large and medium lesions. May appear during thrombolytic therapy. Hemorrhagic transformation has virtually no effect on mortality. But it leads to diagnostic difficulties.
For example, this phenomenon occurs in the acute, acute and early subacute periods (up to 5 days after the onset of stroke). Visible on SWI or gradient echo sequences on MRI. Requires restrictions in anticoagulant therapy.
Diagnosing a stroke is a complex, step-by-step process. It requires modern equipment and physician experience. Therefore, if you suspect a disease, you should call an ambulance and take the patient to the hospital. Attempts to act independently can lead to death.
Is tomography effective?
Almost the only diagnostic method for accurately determining a stroke and its severity is magnetic resonance scanning. The procedure shows a disease, the attack of which occurred just a couple of hours ago, even when it is difficult to say anything or make any predictions based on the general condition of a person admitted to intensive care.
With special examination protocols using diffusion-weighted imaging techniques, magnetic resonance imaging will show changes in the brain that are characteristic of patients who have had an ischemic stroke. MRI detects circulatory disorders faster than any other diagnostic methods.
It is important that the diagnostician is literate and competent, and if a stroke is suspected, he carries out the diagnosis from the necessary perspective, visualizing specific areas of the brain. In this case, the attending physician will not only prescribe effective drug treatment and rehabilitation, but will also be able to predict the patient’s future condition.
Tomography allows you to diagnose stroke with high accuracy even in the early stages or immediately after an attack