Depending on the structure and appearance of the thrombus, white, red, and mixed hyaline thrombi are distinguished.
● White thrombus. Consists of platelets, fibrin and leukocytes, is formed slowly, with rapid blood flow, usually in the arteries, between the trabeculae of the endocardium, on the leaflets of the heart valves in endocarditis.
● Red blood clot. It consists of platelets, fibrin and red blood cells and occurs quickly in vessels with slow blood flow (veins).
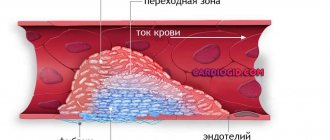
● Mixed thrombus. Includes platelets, fibrin, erythrocytes, leukocytes and is found in any part of the bloodstream and in the cavities of the heart, aneurysms. This thrombus has a small head closely connected to the vascular wall (the structure is a white thrombus), a body (mixed thrombus) and a tail loosely attached to the intima (red thrombus).
Why is a blood clot red?
The tail can break off and become a thromboembolus.
● Hyaline thrombus. Multiple blood clots form only in microcirculatory vessels during shock, burn disease, severe trauma, disseminated intravascular coagulation syndrome, dehydration, severe intoxication, etc. They contain precipitated plasma proteins and agglutinated blood cells, forming a homogeneous, structureless mass with a weakly positive histochemical reaction to fibrin.
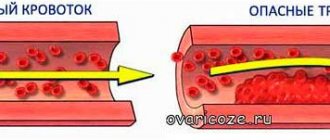
In relation to the lumen of the vessel, thrombi are divided into parietal and occlusive.
● Parietal (white or mixed in structure), for example, a thrombus on atherosclerotic plaques, narrowing the lumen of the vessel.
● Obstructive (usually red), completely closing the lumen of the vessel.
Along the way, blood clots can be localized and progressive (growing along the bloodstream).
In addition to the main types, a number of thrombi are distinguished: arrowroot, tumor, septic, spherical, dilated.
● Maranthic thrombus (from the Greek marasmas - exhaustion, loss of strength). Usually this mixed thrombus occurs in the superficial veins of the lower extremities, the sinuses of the dura mater during exhaustion, dehydration of the body, and sometimes in the elderly.
● Tumor thrombus. It is formed when a malignant neoplasm grows into the lumen of a vein and grows along the bloodstream or when a conglomerate of tumor cells clogs the lumens of microvessels. In polycythemia vera, red blood clots are found in the veins, while in leukemia, leukemic blood clots, consisting of atypical cells and clotted blood, are often found in microvessels.
● Septic thrombus. An infected, mixed thrombus in the veins develops with purulent vasculitis and sepsis.
● Spherical thrombus. Formed when the left atrium of a patient with mitral stenosis is torn from the endocardium. Due to a significant narrowing of the left atrioventricular orifice, thrombotic masses cannot escape and, moving freely in the heart chamber, increase in size, take on the shape of a ball, a smooth surface, as they are polished by the blood flow and friction against the endocardium. This clot can close the valve opening and stop blood flow, causing the patient to faint. After a person falls, the thrombus rolls away and hemodynamics are restored; the patient regains consciousness.
● Dilated thrombus. It develops in aneurysms and can also have a round shape.
Mixed thrombus
Interesting articles:
1) Acute general venous congestion
2) Inflammatory mediators
3) The role of the immune system in regeneration
Classification by morphology
If we consider blood clots from the point of view of appearance and composition, then the classification will consist of four varieties: white, red, mixed (the most common) and hyaline. Depending on the components of the clot, the effect of medicinal substances may vary, therefore, during the diagnosis, the attending physician determines the type.
White clots
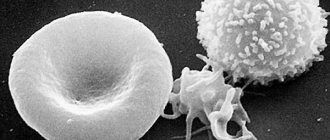
White blood clots are also called gray, agglutination or conglutination. They are formed by platelets - colorless and nuclear-free blood platelets of irregular shape, formed in the red bone marrow. They are directly involved in the coagulation process, and also control blood viscosity, protect vessel walls from damage and promote the dissolution of formed blood clots in healthy people. In some cases, the white clot may be formed by leukocytes (white blood cells) and fibrin (a protein made from fibrinogen synthesized in the liver).
As a rule, this type of clot forms in vessels with good blood flow, mainly in the arteries and cavities of the heart. White blood clots form slowly, perpendicular to the direction of movement of rapidly circulating blood; gradually the growth becomes voluminous and resembles coral. In appearance it is a light gray or white substance, and its surface is embossed. The structure of the clot is crumbling, that is, if it separates from the wall of the vessel, it will disintegrate into small particles.
Red clots
Red blood clots (coagulation) are formed for exactly the opposite reasons - in vessels with slow blood circulation, which at the same time has a high degree of coagulation. The color of clots is determined by the high content of red blood cells, of which in most cases they are composed.
Erythrocytes (red blood cells) are disc-shaped biconcave cells that are saturated with oxygen in the lungs and then carry it to all cells of the body. The red color of these elements is due to the fact that their cytoplasm contains large quantities of hemoglobin, a pigment containing an iron atom. It not only determines the red color of the entire cell, but is also directly involved in the delivery of oxygen, since it is able to bind it.
In appearance, a thrombus of this type is in most cases smooth, but there may also be raised areas. The clot is usually loosely connected to the wall of the vessel, and, unlike white blood clots, it does not form large coral-like formations. Most often, red blood clots affect the veins.
Mixed clots
Mixed blood clots are formed by the fusion of white and red blood clots, so we can say that they are mainly composed of platelets and red blood cells. In this case, such a clot can form in an artery, a vein, or in the cavity of the heart. Mixed thrombi differ in structure from white and red ones; they have three anatomical parts - a conical or flat head, a body (directly mixed thrombus) and a tail. In this case, the head, which is a white blood clot, is attached to the wall of the vessel, and the tail, which is a red blood clot, is freely located in the lumen of the vein or artery and has a loose structure.
Since the head of a mixed thrombus is attached to the vessel wall, the tail poses the greatest danger. It is always localized against the blood circulation, so it can easily come off, clogging the vessel, this process is called thromboembolism.
In rare cases, when the tail reaches a significant size, it can provoke the detachment of the entire blood clot, which can even lead to death if the clot blocks the lumen of vital organs.
It happens that different parts of a mixed thrombus are located in different veins, for example, the head is in the femoral vein, the body is in the external iliac vein, and the tail is in the inferior vena cava.
Hyaline clots
Hyaline blood clots are currently considered the most mysterious by the nature of their occurrence, since researchers do not have a consensus on the mechanism of their formation. They appear predominantly in small vessels of the microcirculatory system and are mostly multiple in nature. Hyaline clots can occur after shocks, burns, disseminated intravascular coagulation (blood clotting disorders due to the release of thromboplastic substances from tissues), electric shocks, extensive skin injuries, etc.
Hyaline blood clots mostly consist of red blood cells, white blood cells, and precipitated plasma proteins glued together or destroyed. Also, the clot may contain a small amount of fibrin protein, but it is not constant, and sometimes the component may disappear completely. The prerequisite for the formation of a hyaline thrombus is often a significant slowdown or complete cessation of blood flow in the vessel.
Treatment methods
Treatment of thrombosis of the lower extremities of the ileofemoral type is carried out in a hospital setting. Conservative therapy is most often used, and surgery is used in rare cases.
Once such a diagnosis is made, therapy may include:
- Use of medications.
- Thrombolysis procedure. The essence of the method is to restore blood supply in a blood vessel by dissolving the blood clot.
- If the doctor suspects a high risk of blood clot detachment (which can lead to life-threatening blockage of the vessel), then special filters are used. Their purpose is to “catch” a detached blood clot. But such therapy is not completely safe and its appropriateness should be determined by the attending physician after a visual examination of the patient.
When making a diagnosis confirming the disease, the following groups of medications can be used:
- Anticoagulants. This group is designed to inhibit the blood coagulation system. They are prescribed for both indoor and outdoor use.
- Pharmacological group of blood thinning medications.
- Anti-inflammatory. The process of inflammation is often accompanied by severe pain.
- If the disease has recently arisen, then methods can be used to dissolve thrombotic formations.
Prescription of radical therapy
In some cases, radical therapy is carried out. It involves the removal of thrombotic fractions. Such operations are prescribed in cases where:
- There is a high probability of venous gangrene.
- The lesion began to spread to the inferior vena cava region.
If necessary, the surgeon recommends retrograde elimination of thrombosis.
In this case, a hole is made in the thigh. Often such treatment is impossible due to the enormous pressure in the right iliac vein. Another contraindication to this method is the presence of adhesions in the lumen of the vein. Patients, as a rule, are not recommended to delay therapy due to the high risk of complications with the pulmonary arteries.
Preventive measures designed to strengthen the walls of blood vessels also play an important role. The use of funds aimed at the general improvement of the body also helps to stop the development of a dangerous process.
Classification by localization in the vessel
In addition to the fact that thrombosis can occur in any part of the human circulatory system, that is, in the area of any internal organ, blood clots also differ in that they can be located differently in the vessel itself. This applies to blood clots of any structure and appearance.
Parietal variety
Parietal clots are quite common; they partially cover the lumen of the vessel. The parietal variety is characteristic of large vessels, as well as elements of the heart - chambers and valves. Often the parietal variety occurs as a result of inflammatory processes, for example thrombophlebitis, which is one of the complications of the last stages of varicose veins.
At first, such clots are not dangerous, since they block the blood flow only partially, but they have the characteristic feature of layering on each other, forming group accumulations. If therapeutic measures are not taken, the formed blood clot will subsequently completely block the blood vessel, which can be fatal.
Obstructive variety
Obstructing, or, in other words, clogging blood clots prevent blood circulation across the entire width of the affected vessel. Moreover, such clots, as opposed to parietal clots, are formed mainly in small blood vessels. The greatest diagnostic difficulty in this case is mixed thrombi, since it becomes difficult to determine where they begin and attach to the vascular wall, and where their tail ends.
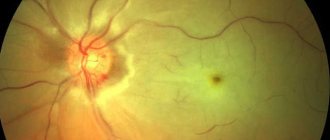
Despite the fact that occlusive clots affect small blood vessels, they pose a significant threat to human health and life. If such a phenomenon occurs in the vessel of the spleen, there will be an increase in its size and a partial loss of efficiency; location in the renal branch of the circulatory network will lead to renal infarction, and in the intestine - to gangrene. When an occlusive thrombus is localized in a heart vessel, death is inevitable.
Axial variety
Axial thrombi can be called a kind of middle type between parietal and occlusive.
Thrombotic synthesis process
The pattern of thrombus formation is not simple and consists of many reactions occurring sequentially. They use microelements, enzymes and proteins. Only a hemostasiologist can describe all these processes. Even for an ordinary general practitioner, this is quite difficult to do.
Thrombosis, depending on the type of vessels, is classified into arterial and venous. At the same time, the properties of the clots themselves (rate of formation, appearance) differ. But the mechanism of thrombus formation remains similar.
In the general case, the formation of a blood clot includes a number of successive stages, where each previous one triggers the next one:
- Agglutination is a reaction to changes in the vascular wall. In this case, accumulation and adhesion of blood platelets occurs in the damaged area.
- Fibrin synthesis.
- Adhesion to the created clot of red blood cells with leukocytes.
- Sedimentation of blood plasma proteins on the formed clot, which begins to thicken.
- The resulting blood clot is fixed on the damaged area. In some cases, the entire blood clot or its fractions can break off and enter third-party tissues of the body, causing blood flow disorders.
This phenomenon, in which the thrombotic fraction comes off, is called thromboembolism. This condition is dangerous because it can lead to a heart attack - necrosis in the tissue.
Other types
In addition to the main classifications of blood clots, there are several separate types that are specific to certain groups of patients. These varieties include the following types:
- Mirantic. It occurs in weakened elderly people with long-term dehydration. The thrombus is localized mainly in the superficial veins.
- Tumorous. Formed as a result of metastasis, that is, the formation of secondary foci of a malignant tumor. Often such a clot gradually grows towards the right lobes of the heart.
- Septic. Occurs as a result of a local inflammatory process caused by infection. Localized in the veins and on the valve flaps of the heart.
Thus, there are several types of blood clots, each of which will require a specific approach during treatment. The type of blood clot is determined by the doctor during diagnosis.
- Thrombosis of mesenteric vessels: symptoms, treatment
- Features and causes Not everyone knows what mesothrombosis is, until...
Treatment and prevention of arterial thrombosis
- Arterial thrombosis is a disease characterized by the formation of a blood clot in…
- To whom and when is thrombolytic treatment prescribed?
- What are they? Trobolytic (fibrinolytic) drugs are medications that can...
Cardiovascular system >>>> Mechanism of blood clot formation and causes of thromboembolism
The mechanism of blood clot formation and the causes of thromboembolism.
The mechanism of thrombus formation was created by nature itself to “repair” damaged vessels. The process of blood clot formation is called thrombosis . The meaning of this process is to carry out irreversible denaturation of proteins and blood cells (platelets and red blood cells) in order to hermetically seal the site of damage. A distinctive feature of blood clots is the fact that they are attached to the wall of a blood vessel and have a layered, crumbly structure and a rough surface. The entire design of the thrombus is designed to maintain blood flow, and its strong adhesion to the vessel under normal conditions does not provide for its separation.
The mechanism of thrombus formation.
When a blood vessel is damaged, substances begin to be released from its wall that inhibit antiaggregation processes (that is, processes that prevent blood clotting) in this place of the bloodstream. At the same time, platelets begin to change and disintegrate, and procoagulants (thrombin and thromboplastin) are released into the blood - substances that promote blood clotting.
How blood clots form
The formation of a blood clot is a complex process. Physiological clots form as a result of damage to the vessel. At the same time, substances (thrombin and thromboplastin) are released into the bloodstream, which activate coagulation processes. This occurs as a result of the breakdown of platelets. The following phases of clot formation are distinguished:
Upon activation, the formation of prothrombinase occurs. With its help, the protein thrombin appears. Next comes the coagulation phase. Under the influence of the protein thrombin, fibrinogen is converted into fibrin. The latter is the basis of the resulting blood clot. A mesh is formed in the damaged area, which receives red blood cells, white blood cells and platelets.
This is how a dense fibrin clot is formed. This is the retraction phase. When hemodynamic parameters stabilize, the thrombus resolves. This is a normal blood clotting process in any person. The formation of blood clots, which cause blockage of blood vessels, is no different. Subsequently, such blood clots do not resolve on their own and cause thrombosis.
In the first days, the clots are still poorly fixed. They may break off and enter the main arteries or veins with the development of thromboembolism. This is an even more dangerous condition. The following factors play an important role in the development of thrombosis:
- decrease in circulating blood volume;
- increased blood viscosity;
- valve dysfunction;
- slowing blood flow;
- platelet tendency to aggregation;
- mechanical damage to the walls of blood vessels.
There are people whose blood clotting process is impaired as a result of a lack of special factors. They practically do not form blood clots, which is fraught with large blood loss at the slightest damage. An example would be hemophilia.
Why is a blood clot dangerous?
Under the influence of thrombin, febrinogen (a protein that affects the erythrocyte sedimentation rate) is converted into fibrin, which in the form of a mesh of threads forms the basis of a blood clot. Blood cells collect in the cells of this network: aggregated platelets, leukocytes and erythrocytes. The structure becomes denser over time. The process of thrombosis is completed and the “leakage” of blood is eliminated.
The causes of thrombosis can be varied.
Consequences of thrombosis.
The uncontrolled process of thrombus formation causes the development of many diseases:
Factors contributing to the detachment of a blood clot from the vessel wall.
Violation of the elastic properties of blood vessels leads to the development of their fragility, which means that the vessel wall will not be able to hold the blood clot tightly enough. The integrity of the vascular wall may occur at the site of attachment of the blood clot.
Since the thrombus is constantly washed by the blood and, being held on the wall of the vessel, experiences continuous resistance to the blood flow, the qualitative characteristics of the blood that put pressure on the thrombus - the fluidity and viscosity of the blood - are of particular importance. The higher the fluidity of the blood, the easier it is for it to wash the blood clot, going around it. The higher the viscosity of the blood, the more difficult it is for the clot to withstand the blood pressure in the vessel.
There is such a thing as a “floating” blood clot . Such a thrombus is connected to the wall of the vessel pointwise and constantly sways in the blood flow. Any sudden movement: coughing, deep breath, laughter, muscle tension when lifting weights can tear it from its place and throw it into the bloodstream. There are special hardware research methods to determine which of the blood clots can be dangerous - coagulogram , ultrasound angiology, sonoelastography.
The result of a blood clot detaching from a vessel is an embolism - blockage of the lumen of the vessel. If a small vessel is blocked, then in the worst case it will end in gangrene of the limb, in the blood vessel of which a thromboembolism , but if a blood vessel that supplies blood to the heart or brain is blocked, then the end result will be necrosis and death of the entire organism.
Announcement
Allergy to tobacco
An allergy to tobacco is nothing more than an allergy to the alkaloid nicotine, but it is often mistaken for an allergic reaction...
Fighting bacteria - new methods
Bacteria have learned to resist antibiotics, and scientists are taking a closer look at lantibiotics. Lantibiotics are promising research because they represent...
Spa manicure – procedure and relaxation
Beauty salons today offer an expanded nail care program - the so-called “spa manicure”. What is a spa manicure?..
Pectins - what is it?
Pectins are substances of plant origin that have the properties of water sorbents and mucous substances. Pectins are especially useful for people who have...
Thrombosis. Definition.
Thrombosis (from the Greek “thrombos” - lump) is a complex intravital process of formation in the blood vessels or cavities of the heart of dense masses consisting of stabilized fibrin and blood cells that can, to one degree or another, interfere with the activity of the heart and/or the movement of blood through the vessels .
When analyzing this definition, you need to pay attention to the following points. First, thrombosis is a lifetime phenomenon
, thereby differing from post-mortem blood coagulation.
In thrombosis, the thrombus is fixed to the vascular wall, and the post-mortem blood clot lies free in the lumen of the vessel and can easily be removed from it. This circumstance is important in forensic medical practice, when it is necessary to establish the cause of death and the time of its occurrence. Secondly, thrombosis is the intravascular formation of dense masses that, to one degree or another, impede the movement of blood through the vessels.
The formation of a blood clot is a protective reaction of the body to damage (alteration) of the vascular wall, preventing bleeding.
However, the resulting thrombus cannot also interfere with normal laminar blood flow, and, in some cases, contribute to additional thrombus formation, an increase in the mass of the thrombus and complete obstruction of the blood vessel. Thrombosis of microcirculatory networks is the main pathogenetic mechanism of shock and DIC syndrome. In addition, it is well known that blood clots formed in the vessels or cavities of the heart, in cases of their separation from the vascular wall, become emboli, which, obstructing the corresponding vascular networks, can cause serious circulatory disorders. When we talk about thrombosis, we mean intravascular blood coagulation and the formation of dense masses. Blood clots can also form outside of blood vessels, due to physical, chemical or other types of trauma to body tissues, but in this case we are talking only about the formation of a blood clot, and not about thrombosis. The mechanism of the so-called “external blood coagulation pathway” will be discussed in more detail below. Thirdly, thrombosis is a complex process
that includes a number of stages and leads to the formation of dense masses consisting of stabilized fibrin and blood cells. Indeed, thrombosis is a multistage and multicomponent process in which both cellular and plasma coagulation factors are involved. Pathology of any link in this complex process can have very serious consequences for the body.
Classification by morphology
If we consider blood clots from the point of view of appearance and composition, then the classification will consist of four varieties: white, red, mixed (the most common) and hyaline. Depending on the components of the clot, the effect of medicinal substances may vary, therefore, during the diagnosis, the attending physician determines the type.
White clots
White blood clots are also called gray, agglutination or conglutination. They are formed by platelets - colorless and nuclear-free blood platelets of irregular shape, formed in the red bone marrow. They are directly involved in the coagulation process, and also control blood viscosity, protect vessel walls from damage and promote the dissolution of formed blood clots in healthy people. In some cases, the white clot may be formed by leukocytes (white blood cells) and fibrin (a protein made from fibrinogen synthesized in the liver).
As a rule, this type of clot forms in vessels with good blood flow, mainly in the arteries and cavities of the heart. White blood clots form slowly, perpendicular to the direction of movement of rapidly circulating blood; gradually the growth becomes voluminous and resembles coral. In appearance it is a light gray or white substance, and its surface is embossed. The structure of the clot is crumbling, that is, if it separates from the wall of the vessel, it will disintegrate into small particles.
Red clots
Red blood clots (coagulation) are formed for exactly the opposite reasons - in vessels with slow blood circulation, which at the same time has a high degree of coagulation. The color of clots is determined by the high content of red blood cells, of which in most cases they are composed.
Erythrocytes (red blood cells) are disc-shaped biconcave cells that are saturated with oxygen in the lungs and then carry it to all cells of the body.
Diagram of thrombus formation. Briefly about an important natural mechanism
The human body is a rather fragile system. Damage to the skin or internal organs causes bleeding. To save lives, nature has invented a mechanism called thrombosis.
The essence of this physiological reaction is the irreversible denaturation of blood proteins to seal the damaged vessel. Under normal conditions, the resulting clot does not separate from the site of damage to the vessel wall. At the same time, blood flow is maintained.
Diagram of blood clot formation
Classification by localization in the vessel
In addition to the fact that thrombosis can occur in any part of the human circulatory system, that is, in the area of any internal organ, blood clots also differ in that they can be located differently in the vessel itself. This applies to blood clots of any structure and appearance.
Parietal variety
Parietal clots are quite common; they partially cover the lumen of the vessel. The parietal variety is characteristic of large vessels, as well as elements of the heart - chambers and valves. Often the parietal variety occurs as a result of inflammatory processes, for example thrombophlebitis, which is one of the complications of the last stages of varicose veins.
At first, such clots are not dangerous, since they block the blood flow only partially, but they have the characteristic feature of layering on each other, forming group accumulations. If therapeutic measures are not taken, the formed blood clot will subsequently completely block the blood vessel, which can be fatal.
Obstructive variety
Obstructing, or, in other words, clogging blood clots prevent blood circulation across the entire width of the affected vessel. Moreover, such clots, as opposed to parietal clots, are formed mainly in small blood vessels. The greatest diagnostic difficulty in this case is mixed thrombi, since it becomes difficult to determine where they begin and attach to the vascular wall, and where their tail ends.
Despite the fact that occlusive clots affect small blood vessels, they pose a significant threat to human health and life. If such a phenomenon occurs in the vessel of the spleen, there will be an increase in its size and a partial loss of efficiency; location in the renal branch of the circulatory network will lead to renal infarction, and in the intestine - to gangrene. When an occlusive thrombus is localized in a heart vessel, death is inevitable.
Axial variety
Axial thrombi can be called a kind of middle type between parietal and occlusive. Such clots are attached to the vascular wall in only one anatomical area - the head or part of the body, partially obstructing blood flow. Moreover, if a blood clot comes off, under the influence of blood circulation it can still remain in a suspended state for some time, “collapsing” into a spherical shape.
How does pathology manifest itself?
Thrombosis of the lower extremities is characterized by impaired blood flow , which leads to the following manifestations:
- Pain in the calf muscles, groin or inner thigh.
- An increase in the size of the legs as a result of the appearance of edema. The latter develop in the direction from the feet to the groin, and in some cases reach the gluteal muscles.
- Change in color of legs. In this case, the lower limbs acquire a color from pale to blue.
- Pain increases during palpation of the problematic venous area in the leg area.
It happens that ileofemoral thrombosis leads to loss of sensation in the toes due to its rapid development. The pain is sharp and throbbing in nature. Often the patient experiences coldness in the lower extremities. This condition is typical for acute ileofemoral phlebothrombosis on the left or right .
After a few days from the onset of the disease, the swelling that appears may become smaller. And on the affected leg it will be possible to observe the vascular pattern.
Other types
In addition to the main classifications of blood clots, there are several separate types that are specific to certain groups of patients. These varieties include the following types:
- Mirantic. It occurs in weakened elderly people with long-term dehydration. The thrombus is localized mainly in the superficial veins.
- Tumorous. Formed as a result of metastasis, that is, the formation of secondary foci of a malignant tumor. Often such a clot gradually grows towards the right lobes of the heart.
- Septic. Occurs as a result of a local inflammatory process caused by infection. Localized in the veins and on the valve flaps of the heart.
Thus, there are several types of blood clots, each of which will require a specific approach during treatment. The type of blood clot is determined by the doctor during diagnosis.
- Treatment and prevention of arterial thrombosis
- Arterial thrombosis is a disease characterized by the formation of a blood clot in…