Intraventricular blockade is a condition in which the ventricular conduction of excitatory impulses slows down or completely stops. The pathology can be caused by damage to one or more branches of the His bundle. It most often develops in older people suffering from other heart diseases. It occurs in young men with a slender build, teenagers, and athletes. In the absence of clinical manifestations, it is considered physiological and does not require drug correction.
Types of intraventricular blocks
VGB can be divided according to the nature of its flow. In accordance with this criterion, the pathology can be persistent (persists constantly), transient (occurs periodically) and alternating (on the ECG there are signs of damage to one or the other leg). In addition, there is a complete and incomplete form of the disease. In the first case, the conduction of the impulse along the affected branch stops completely, in the second it slows down significantly. Classification by type and number of departments that have undergone changes is important:
- Single sided shape:
- monofascicular: isolated blockade of the anterior or posterior branch of the left leg, damage to the right leg;
Types of intraventricular blocks - bifascicular: disruption of the conductivity of both strands of the LPN.
- Bilateral form or combined blockade:
- right and anterior left legs of the PG;
- right and posterior left legs of the PG.
- Three-bundle form: blockade of intraventricular conduction, affecting all parts of the His system.
Please note: Focal intraventricular heart block in the proximal region, before division into the anterior and posterior branches, is not considered a true bifascicular form of pathology. However, this issue is of academic rather than clinical significance.
Causes of the disease
In general, the causes of VZhB do not differ from those of other conduction disorders (atrioventricular, synatrial block). All etiological factors are divided into organic and functional. The former include congenital and acquired heart defects, valvular calcification, ischemic disease, idiopathic fibrosis in Lenegra and Lev's disease, myocardial tumors.
The most common cause of blockades is post-infarction cardiosclerosis with subsequent proliferation of connective tissue in the necrosis zone. Such forms of pathology are considered irreversible.

A common functional factor in the occurrence of pathology is the use of high doses of antiarrhythmic drugs of class 1C, 1A. Representatives of these groups are “Propafenone”, “Amiodarone”. Intraventricular blockades develop with hyperkalemia, acidosis, and insufficient oxygen in the blood. Sometimes it is not possible to determine the cause of the disease. In this case, they speak of the idiopathic form. It is important to remember that dysfunction of the autonomic nervous system, leading to the formation of AV blockade, does not affect intraventricular conduction.
Visit to the doctor
After a heart attack or other serious cardiac pathology, it is necessary to regularly visit a cardiologist, at least in the first six months. This will allow you to record your condition, identify complications, if any, and promptly eliminate them.
Separately, it is worth noting that any type of this blockade at the initial stage requires increased attention and mandatory consultation with your doctor.
First of all, you should go to a therapist or cardiologist, who can guide you on whether you really should be afraid of this disease, what examinations to undergo, and how to structure your therapy. After all, as we have already noted in this article, this disease can be either completely harmless or seriously threaten your life and health. In the latter case, hospital treatment, possibly surgical intervention, will be required.
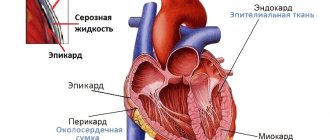
Pathogenesis of VGB
Disruption of impulse conduction processes in most cases is caused by mechanical compression of transport pathways. Similar phenomena occur as a result of swelling of the heart tissue, necrosis with transition to fibrosis, and tumor pressure. Functional causes of the disease lead to changes in excitability and the duration of the refractory period, and a decrease in membrane potential. In this case, reversible blockades develop, which go away on their own after the action of the etiological factor is eliminated.
Complete blockade of one of the branches of the His bundle leads to the fact that the corresponding ventricle and part of the septum begin to be excited in a special way. The impulse is carried out from the other half, which significantly slows down the contraction process and discoordinates the work of the heart. With an incomplete type of pathology, significant changes in the functioning of the main organ do not occur. There is a moderate weakening of conductivity.
Symptoms of the disease
With intraventricular blockades, there are no changes in the frequency or rhythm of the heart. Therefore, specific clinical symptoms are usually absent. Auscultation may reveal a pathological splitting of the first and second sounds (complete cessation of impulse transport along the PNPG) or a paradoxical splitting of the second sound (blockade of the LPNG).
In the presence of combined heart lesions, the disease can manifest itself in the form of vague or squeezing pain localized in the left half of the chest, burning sensation, shortness of breath, swelling of the legs, and decreased tolerance to physical activity. However, all these symptoms are usually caused by concomitant pathological processes, in the presence of which one can assume blockade of intraventricular conduction.
Additional examinations
When diagnosing a blockade, the patient usually requires additional examinations. For accurate and correct diagnosis, cardiologists are recommended to use one or all three of these methods.
Ultrasound of the heart or echocardioscopy. This procedure is prescribed if there is a suspicion of myocarditis, heart disease, or myocardial infarction. If the patient denies the fact of hospital treatment, an Echo-CS is considered mandatory, since otherwise the patient may suffer a heart attack on his legs, which will have a fatal impact on his health.
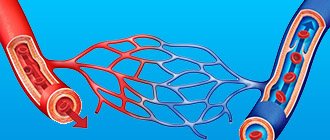
Another method is coronary angiography. It is done to evaluate in detail the patency of the coronary arteries, and also to determine whether there is a need for bypass surgery or stenting.
Finally, 24-hour Holter ECG monitoring is often prescribed. It is especially useful in case of unstable blockade. This may be due to tachydependent blockade, that is, tachycardia, which manifests itself and worsens during physical activity.
Diagnosis of intraventricular blockades
The basis of diagnosis is a 12-lead electrocardiogram. Local intraventricular block on the ECG manifests itself as follows:
- Complete blockade of the right leg. In the right precordial leads, the QRS complexes are M-shaped. The S wave in V1, V2, aVL is widened and jagged. The duration of the ventricular complex is more than 0.12 seconds. A negative or biphasic T wave may occur in lead 3.
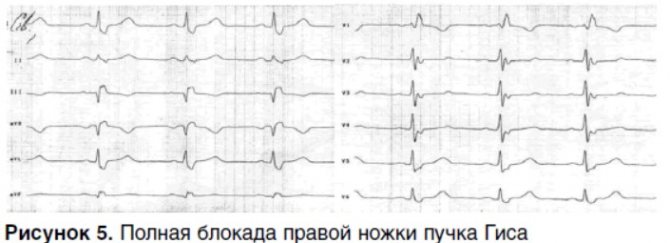
- Partial blockade of the right leg. The duration of the ventricular complex is 0.09-0.11 seconds, they are of the rSR' type, in leads I and V6 the S wave is slightly widened.
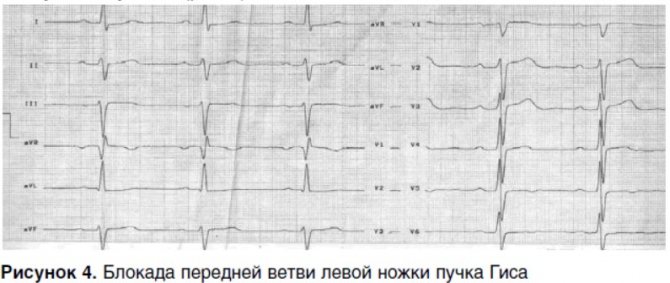
- Blockade of the left anterior branch. Marked deviation of the EOS to the left, QRS duration - 0.08-0.11 seconds, qS type in leads I and aVL.
- Blockade of the left posterior branch. Deviation of the EOS to the right, QRS I and aVL leads type rS, in leads III and aVF - qR.
- Complete blockade of LBP. Deformed, widened R wave with a wide split apex in V5, V6, I, aVL. In V1, V2, III, aVF, the S wave is subject to deformation. In some cases, T wave inversion and a shift of the electrical axis to the left are determined.
In bi- and trifascicular types of the disease, the film reveals signs of all available options for damage to the conductive tracts. Nonspecific intraventricular block is characterized by the appearance of a picture that does not fit into the framework of damage exclusively to the His apparatus.
If a ventricular conduction disorder is detected, both an adult patient and a child may be assigned an additional examination. If organic pathology of the myocardium and valvular apparatus is suspected, ultrasound examination of the heart is used. It allows you to visualize the organ. 24-hour Holter monitoring is recommended for people with variable blockades. Patients who have had a myocardial infarction or suffer from angina, especially unstable angina, need coronary angiography to assess the patency of the heart vessels.
Laboratory examination does not have sufficient information content. A person may be prescribed a number of clinical tests, however, their diagnostic value is minimal. With concomitant cardiac injuries, elevated troponin levels may be observed. Prolonged course of the disease sometimes leads to an increase in blood viscosity.
Please note: In most cases, intracardiac blockages are detected by chance, during a routine ECG or examination for another disease. It is almost impossible to suspect the presence of the disease without the results of electrocardiography.
Symptoms
Often this disease is asymptomatic. If any signs of intraventricular block occur, they are due to the underlying pathology that led to this block. For example, with myocardial ischemia, headaches appear, usually in the back of the head, and chest pain. Myocarditis is manifested by shortness of breath and chest discomfort.
If a patient exhibits intraventricular block on the ECG, which is accompanied by certain suspicious complaints, the patient should be urgently examined for cardiac pathologies.
Treatment of the disease
There is no need to treat stable, persistent ventricular block. The patient is indicated for dynamic observation due to the risk of atrioventricular node dysfunction. This is especially true for multi-beam types of pathology. Treatment of the underlying disease should be prescribed:
| Main disease | Treatment |
| IHD | Antiplatelet agents, statins, beta blockers, nitrates for attacks. |
| congenital heart disease, tumors | Operational correction. |
| Intoxication with antiarrhythmics | Symptomatic therapy. |
| Acidosis | Introduction of buffer solutions, eliminating the cause of increased acidity. |
| Hyperkalemia | Calcium chloride, diuretics, laxatives, infusion therapy. |
| Hypoxia | Oxygen therapy, mechanical ventilation if necessary. |
If there is a high risk of progression of the pathology and damage to the AV conduction system, the patient is given a pacemaker that resynchronizes and restores proper functioning of the ventricles.
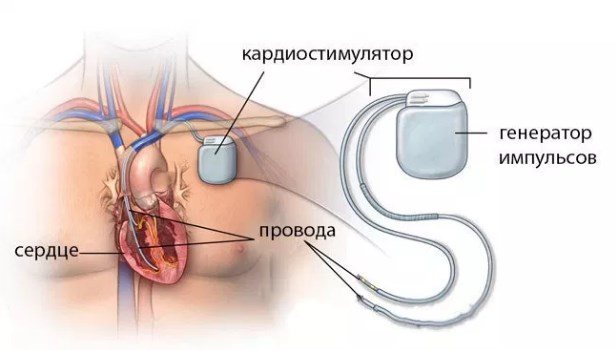
The procedure is carried out if the following phenomena were discovered during the diagnosis:
- two- or three-bundle lesions with intermittent atrioventricular block of any degree;
- history of fainting of cardiac origin;
- prolongation of the QT interval more than 100 ms.
Danger and prognosis
Local stable blockades of intraventricular conduction are not dangerous and do not lead to the development of complications. They can exist for a long time or go away independently with age. In the presence of bilateral lesions, especially affecting the posteroinferior branch of the His bundle, the risk of complete transient AV block with the appearance of Morgagni-Adams-Stokes attacks increases. This probability is 6%.
Emerging risks are determined by the severity of the underlying disease. Thus, acute myocardial infarction accompanied by LBBB has an in-hospital mortality rate of about 40%. Limited blockades of the intraventricular type, especially those occurring at a young age, rarely lead to serious consequences and have a favorable prognosis. The reason for deferment from the army for young people with a similar diagnosis is only a complete form of conduction disorder. Conscripts with an incomplete variety are considered fit for service with minor restrictions.
Did you like the article? Save it!
Still have questions? Ask them in the comments! Cardiologist Mariam Harutyunyan will answer them.
Mikhail Astakhov
Graduated from Ryazan State Medical University with a degree in General Medicine. Anesthesiologist-resuscitator
Why does ventricular block develop?
Intraventricular block can be registered in an absolutely healthy person without causing him any discomfort. But this applies only to conduction disturbances along the right branch.
If a left hemiblock (especially a complete one) is recorded, as well as in the case of a two-, three-fascicular block or block of terminal branches, it is always necessary to think about the presence of some kind of cardiac pathology.
Most pathological intraventricular blocks are based on organic damage to the myocardium due to various reasons
Causes of pathological blockades that develop in childhood:
- Myocarditis,
- Myocardial dystrophy (cardiomyopathy),
- Cardiosclerosis after inflammatory diseases of the heart tissue,
- Violations of the architectonics of the heart due to congenital or acquired defects,
- Heart tumors.
These diseases can cause the occurrence of both left and right hemiblock, as well as blockade of the terminal branches.
However, it should be remembered that in children and adolescents, incomplete or even complete blockade of the right leg is often a normal condition and can occur in a child against the background of complete health.
Causes of intraventricular blockades that first appear in adulthood and old age:
- 40% of all blockades are caused by atherosclerotic damage to the artery supplying the myocardium in the area of the conduction bundle, and the resulting myocardial ischemia in coronary artery disease. In addition to chronic ischemia, acute myocardial infarction can lead to the occurrence of intraventricular block (in 8-13% of cases of AMI, complete left block is diagnosed).
- 30-40% of all cases of intraventricular block are caused by arterial hypertension, especially with the formation of compensatory hypertrophy of the heart muscle (hypertrophic cardiomyopathy).
- 20% is due to rheumatism and congenital heart defects (CHD). In addition, blockades are often observed after surgical correction of congenital heart disease (in 40% of people operated on for heart defects).
This is interesting: The essence of the DOT rejuvenation procedure
Regardless of age, blockades can be caused by alcohol poisoning and its surrogates, chest injuries, hyperkalemia, for example, due to renal failure or excessive use of certain drugs. Thus, intraventricular blockade develops in case of poisoning with potassium-sparing diuretics (spironolactone, veroshpiron), potassium-containing drugs (panangin, asparkam), as well as some psychotropic drugs (amitriptyline, sertraline, etc.).