Causes of asystole
The website slovmed.com cannot identify clear reasons for the development of asystole. Each case is individual. However, we can identify the factors that occur most often:
- Acute heart failure.
- Myocardial infarction.
- Overdose or abuse of antiarrhythmic drugs.
The main reason often lies in organic changes and decompensation in the myocardium. Conventionally, causes can be divided into primary and secondary. Primary causes include cardiac diseases:
- Ruptured aortic aneurysm.
- Acute myocardial infarction and resulting complications: pulmonary artery thromboembolism, aneurysm rupture, cardiogenic shock.
- Heart disease during decompensation.
- Violation of the rhythm of ventricular contraction: ventricular tachycardia, various ventricular extrasystoles, paroxysm of atrial fibrillation.
- Acute heart failure.
Additional factors contributing to the development of asystole are:
- Excess weight.
- Use of nicotine and alcohol.
- High blood cholesterol levels.
- Male gender.
- Elderly age.
- Diabetes.
Secondary causes include factors that are not cardiac disorders:
- Stroke with brain damage.
- Malignant tumors.
- Damage to internal organs due to renal or liver failure, leukemia, diabetes, anemia.
- Respiratory failure caused by a long-term asthmatic condition.
- Fatigue.
- Choking after a foreign body enters the larynx or bronchi.
- Extensive injuries.
- Poisoning with poisons and chemicals.
- Massive burns.
- Injury after exposure to high voltage current.
- Large blood loss.
go to top
In what cases does asystole most often occur?
Asystole (another clinical name is isoline) is the cessation of synthesis and conduction of electrical impulses in the heart.
The development of pathology is a nonspecific consequence of many conditions. According to the recommendations of the American Society of Cardiology, ventricular asystole develops in the following cases:
hypovolemia (reduced volume of circulating blood due to injury, damage to the integrity of the arteries, redistribution of fluid in the vascular bed);- hypoglycemia is a glucose deficiency that often develops in patients with diabetes after physical activity or when they go to bed without following a diet and insulin use;
- hypoxia is a deficiency of oxygen that is delivered to organs and tissues. The condition develops against the background of cardiac or respiratory pathology, blood diseases;
- disturbances in electrolyte balance, especially potassium metabolism (hypo- and hyperkalemia). Increased ion concentrations accompany injury, metabolic disorders, renal failure and compartment syndrome;
- acidosis – a decrease in blood pH due to the accumulation of under-oxidized products;
- hypothermia is one of the most common causes of death of a child in the first days of life (sudden infant death syndrome) due to exposure to low temperatures, which inhibits the activity of the nervous system and heart rate driver;
- Tension pneumothorax is a pathology characterized by the accumulation of air in the pleural cavity, which compresses the lung tissue;
- thrombosis - blockage of blood vessels in the heart or brain with a blood clot;
- intoxication with toxic substances or medications;
- tamponade - accumulation of blood in the pericardial cavity due to rupture of the heart wall.
These conditions develop with myocardial infarction, traumatic shock, and overdose of pharmacological drugs.
According to Wikipedia, asystole is the resulting condition after ventricular fibrillation, paroxysmal or torsades de pointes, or other hemodynamically compromised arrhythmias.
Symptoms of asystole
How does asystole manifest? This can only be determined by the state in which a person is at the moment of asystole. The main symptom is cardiac arrest (lack of blood circulation), which can be noted if you try to feel the pulse.
In some cases, people note various precursors of asystole:
- 30% of patients felt pain in the chest.
- 32% of patients reported feeling dizzy or losing consciousness.
- 25% of people complained of shortness of breath in the form of difficulty breathing.
- Dyspnea.
- Tachycardia or hypotension.
- Fever.
Ventricular asystole is accompanied by the following set of symptoms:
- Disappearance of pulse, pressure, heart sounds.
- Loss of consciousness.
- Pale skin.
- Lack of breathing.
- Pupil dilation after 45 seconds.
People nearby can observe one of the scenarios:
- Option 1 – a person suddenly falls, loses consciousness, a rare breath escapes, the face and lips turn blue. Attempts to bring the person back to consciousness are unsuccessful.
- Option 2 - a person appears to be asleep if cardiac arrest occurs during sleep. Here it is difficult to detect asystole in time to call for help.
- Option 3 – the patient’s condition is monitored by a monitor in the intensive care unit. Any deviation from the norm in the functioning of the heart is recorded and indicated by an audible signal.
You should be aware that the asystolic state is reversible. The person is at the stage of clinical death, but he can be saved if timely assistance is provided. Here the actions of passers-by or loved ones who happen to be close to a sick person become important.
go to top
Systolic tachycardia in adults: causes
Systolic tachycardia can be caused by other cardiac pathologies.
Quite often it occurs in coronary heart disease. With this disorder, myocardial damage occurs due to insufficient blood circulation. This can seriously affect the functioning of the heart as a whole or individual parts. Systolic tachycardia: other causes
– congenital or acquired heart defects;
- heart failure;
– cardiomyopathy;
– infectious damage to the myocardium.
An important role in the development of systolic tachycardia is played by external influences on the heart. Symptoms of systolic tachycardia may appear as a result of incorrectly selected dosages of medications. Medicines can increase the ejection fraction or, conversely, weaken it.
Systolic tachycardia in adults (a type of arrhythmia) can be caused by electrolyte disturbances. This is due to the fact that the work of the heart directly depends on the amount of elements in the blood such as potassium and magnesium. The activity of the heart can be negatively affected by a lack of these elements or their excess.
Systolic tachycardia symptoms can be very different and treatment should only be prescribed by a doctor after a thorough diagnosis. Systolic tachycardia is characterized by an increase in heart rate greater than 90 beats per minute. There are patients who do not feel much change in the number of strokes, but in older age this is already sensitive. It is because of this that tachycardia is experienced in combination with heart pain and headaches, weakness and high fatigue.
Tachycardia itself is not dangerous, but if combined with other disorders of cardiac origin, it leads to quite serious complications. This is cardiac arrest, stroke, myocardial infarction.
Systolic tachycardia can be caused by overeating. In addition, it is also caused by high physical exertion.
Electrocardiography (ECG) is the main method for diagnosing systolic tachycardia. Echocardiography, cardiac ultrasound, blood biochemistry, urine analysis, and hormonal indicators may be additionally prescribed.
– before each QRS complex, P waves are detected, which indicates sinus rhythm;
– the correct rhythm is observed with tachycardia and bradycardia, as indicated by the same RR interval;
– Heart rate during tachycardia is increased, and during bradycardia it is decreased compared to the age norm.
Electrocardiography is the main method for diagnosing tachycardia, which is available at any level of patient care.
– correct sinus rhythm is maintained;
– Heart rate is more than 90 per minute;
– the P wave is defined as positive in all main leads;
– there is a shorter distance (interval) between the P waves;
– the T wave can be increased or decreased.
With extrasystoles, extraordinary contractions are visible on the ECG, which are divided, depending on the location of the ectopic focus, into atrial or ventricular.
Additional information about the patient’s condition is obtained through ultrasound examination of the heart, stress tests, and daily monitoring. Laboratory tests are also done if hormonal or electrolyte disturbances are suspected.
Emergency care for asystole
Since ordinary passers-by and relatives find themselves next to a person at the moment of asystole, much depends on their actions. You should call an ambulance, and while it arrives, take all necessary actions to restore your heart rhythm.
- Disturb a person, speak loudly, hit him on the cheeks. If he regains consciousness, this is a good sign. You should provide him with access to fresh air and place his head below his shoulders.
- Feel the pulse if the first attempts to restore contact do not work. It is necessary to restore breathing, heart rate and ensure blood circulation in the brain.
In the latter case, the following measures are taken:
- Place the person on a hard surface.
- Throw your head back. Check the patency of the airways so that food debris, dentures and other foreign bodies do not get into them when breathing is restored.
- Blow air into your nose or mouth with your mouth while closing the second hole. The chest should rise when breathing this way.
- Push your chest with both palms between breaths 4-5 times.
These procedures should be performed until a pulse appears or an ambulance arrives.
go to top
Specialized assistance
Emergency care in a medical facility for asystole includes:
- installation of an endotracheal (inside the trachea) endotracheal tube for mechanical ventilation or mechanical ventilation using an Ambu bag;
- catheterization of large vessels with the administration of adrenaline, atropine and other components of infusion therapy, depending on the reasons that caused circulatory arrest;
- conducting electrical pulse cardiac stimulation.
It must be remembered that the time allotted for resuscitation is 30 minutes. The sooner the provision of first aid begins, the greater the chance of a victim or patient having a favorable outcome.
European countries and the United States have put into practice training the population in CPR skills, including the use of stationary street defibrillators.
These devices, which are a good aid for resuscitation, make it possible to determine the need for their use. Thanks to software voice prompts, anyone can understand whether cardiac defibrillation is required or not.
Treatment of asystole
Asystole begins its treatment in the ambulance and continues in the intensive care unit. Doctors continue to perform chest compressions, maintain ventilation with a special mask, administer intravenous adrenaline and use a defibrillator.
Upon arrival at the intensive care unit, intensive care continues, which takes at least 30 minutes. The patient is connected to mechanical breathing. Various medications are injected into the subclavian vein to support brain function, which is reversible within the first 8 minutes after breathing stops. The following drugs are used here:
- Dopamine.
- Sodium hydroxybutyrate.
- Alkaline solution.
- Reopoliglyukin.
- Glucose.
- Panangin.
- Sodium bicarbonate.
- Insulin.
The effectiveness of the drugs is observed on cardiac monitors.
Specialized treatment is carried out in the form of artificial ventilation of the lungs and administration of Atropine and Adrenaline hydrochloride into the veins. If there is no effect from adrenaline, the drug is administered in a stream every 5 minutes or every 3 minutes, increasing the dose to 5 mg.
The administration of drugs into peripheral veins occurs when they are diluted with saline solutions. If there is no access to the veins, Adrenaline, Atropine, Lidocaine are injected into the trachea with a dosage increased by 2 times. And intracardiac administration of drugs occurs in the absence of other administration options.
There are also accompanying symptoms that can be eliminated using available methods:
- Hypovolemia is eliminated by restoring blood volume.
- Pneumothorax is treated with a catheter, which is left open and then replaced with a drain.
- Cardiac tamponade is treated with pericardiocentesis, pericardiotomy, and catheter drainage.
- Intracardiac thrombosis and myxoma are treated with surgery.
- Hypoxia eliminates mechanical ventilation.
go to top
How does cardiac arrest develop?
In general, preventive measures for extrasystole prevent various pathologies and diseases that are at the basis of its development. These are ischemic heart disease, cardiomyoptitis, myocarditis, and so on. In addition, as part of prevention, their exacerbations are prevented. Therefore, it is recommended to exclude drug, food, and chemical intoxication (so as not to provoke the disease).
Patients who have ventricular extrasystole without symptoms (without other problems with cardiology) should follow a diet that contains a lot of magnesium and potassium salts. In addition, they should stop smoking, drinking alcohol and drinking a lot of caffeine. You can't overexert yourself.
Kogol also provoke the development of a disease that causes serious discomfort. Keep an eye on the load...
The causes of asystole are usually divided into cardiac and extracardiac. The first category of etiological factors consists of:
- cardiac ischemia;
- acute coronary syndrome, myocardial infarction;
- myocarditis;
- pericarditis with cardiac tamponade (the result of treatment is visible immediately after the evacuation of accumulated fluid);
- congenital and acquired heart defects (including aortic stenosis, damage to the valve apparatus);
- cardiomyopathy;
- heart injuries;
- carrying out invasive medical procedures (coronary angiography, catheterization of the cavities of the heart and large vessels), performing direct cardiac stimulation.
Stopping the heart rhythm is a possible complication of these measures.
The development of asystole can be provoked by disturbances of homeostatic constants. What are extracardiac factors?
1) Various disorders of vascular tone during shock.
2) Significant reduction in circulating blood volume.
3) Thrombosis in the area of large branches of the pulmonary trunk.
4) Reflex arrest of cardiac activity due to irritation of the vagus nerve due to blunt trauma to the abdomen.
5) Accumulation of air in the pleural cavity (pneumothorax).
6) Blood gas disorders (O2 deficiency and/or CO2 predominance).
7) Pronounced electrolyte changes: low blood pH, sharp increase in potassium and calcium, nitrogen compounds. Increased production of stress hormones.
Overdose of medications, individual reaction to barbiturates, narcotic drugs, adrenergic blockers, quinidine, cardiac glycosides.
9) All conditions leading to the inability of oxygen to enter the lungs (drowning, suffocation, aspiration of foreign bodies).
10) Electric shock and lightning.
The pathogenetic process of asystole depends on the initial state of the myocardium, the quality, as well as the severity of the etiotropic factor. Cardiac arrest may develop at the level of the main pacemaker (sinus node), blockade at the AV junction, or primary ventricular asystole.
Treatment of asystole begins regardless of the availability of specialized care. Each person should be trained in primary resuscitation measures.
To perform CPR at the level of an ordinary citizen, you must be able to perform artificial ventilation and closed heart massage.
Mechanical ventilation is carried out “mouth-to-mouth” and “mouth-to-nose”; in children, a mixed version is possible with simultaneous blowing of air into the nasal and oral cavities. They first check the patency of the airways, clear them as much as possible from mucus, vomit, and in case of drowning, from water and mud. Air is exhaled through a handkerchief into the victim’s mouth or nose, blocking the return flow of air (the mouth-to-mouth technique requires covering the nose and vice versa).
Effectiveness is assessed by chest movements.
Closed heart massage is performed just above the xiphoid process above the projection of the heart (landmark - the lower third of the sternum), with the hands in a cross-shaped position and the arms straightened at the elbow joints. Compressions are carried out to a depth of up to ¾ of the thickness of the chest. The presence of a pulse wave from the vessels of the neck at this moment indicates the correctness of the measures.
Under ideal conditions, resuscitation is carried out by two people, trying to achieve a heart massage rate of up to 100 per minute, for every 30 compressions there are 2 injections into the lungs.
How long do people live with asystole?
There is no need to talk about favorable prognosis for asystole, since in rare cases a person receives sufficient help. How long do people live with asystole? The minutes count when the basic functions of the body stop: heartbeat, breathing and brain function.
In most cases, death occurs. Even with timely delivery of the patient to the hospital, only 15% of cases can be saved from death.
How often does asystole occur? In newborns it occurs with a frequency of 72.1 per 100,000, in childhood – 3.73, in adolescents – 7.37, in adults – 126.5.
Ventricular fibrillation gives a more favorable prognosis (4 times more) than asystole. However, death is observed in both variations. If destruction of brain cells or other organs occurs, then the prognosis becomes even more unfavorable.
Clinical manifestations
Acutely developed ventricular asystole is manifested by a lack of consciousness, dilated pupils, the inability to determine the pulse in the great vessels and listen to the heartbeat.
At the same time or a little later, the respiratory movements of the chest stop. The condition requires urgent cardiopulmonary resuscitation (CPR).
Cardiac arrest may occur gradually. The gradual development of atrioventricular block with subsequent asystole is characterized by Morgagni-Adams-Stokes attacks.
The patient's consciousness becomes clouded, the patient is excited, then clonic-tonic convulsions occur, and heartbeats are interrupted.
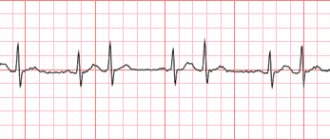
Asystole on the ECG is recorded as a straight line. When recording a cardiogram before a complete cardiac arrest, various types of chaotic oscillations, ventricular fibrillation are often detected, or blockades are previously present.
Algorithm for providing assistance
Treatment of cardiac asystole according to approved clinical protocols involves carrying out resuscitation measures in the presence of signs of circulatory arrest. At the pre-hospital stage (before the arrival of the ambulance, which must be called by witnesses), it is necessary:
straightening and clearing the airways (unfasten the narrow collar, remove foreign objects from the oral cavity).
- mouth-to-mouth breathing;
- indirect cardiac massage (at least 100 compressions per minute) - this method of artificial contraction of the myocardium contributes to minimal hemodynamic recovery. The effectiveness of the event is ensured by the activation of the nervous system and sinus node.
Emergency doctors use intravenous injections of adrenaline, which helps activate the autonomic nervous system and start cardiac activity.
In a hospital setting, the patient is treated for the resulting consequences of resuscitation (“post-resuscitation illness”) and the primary cause of circulatory arrest, which implies:
- adequate ventilation (using a machine or oxygen therapy);
- surgical interventions for injuries;
- correction of metabolic processes;
- use of antidotes;
- administration of intravenous glucose solution;
- replacement therapy with blood products after significant loss and hypovolemia.
There are no traditional methods for treating or preventing asystole; cardiac arrest is one of the signs of death, which requires emergency resuscitation.
What is the prognosis for diagnosing this disease?
The development of ventricular asystole is accompanied by classic symptoms of clinical death:
unconscious state (with sudden development, the person falls);
- absence of pulsation in the carotid arteries;
- reaction of the pupil to light (pathological dilation).
- lack of breathing;
- decreased muscle tone;
The pathophysiological mechanisms of the development of symptoms are based on the absence of an electrical impulse, which causes a contraction of the myocardial muscle mass. Stopping blood circulation leads to disruption of the transport of glucose and oxygen to vital organs: lungs, brain and heart.
Due to metabolic changes, the control of the nervous system (central and autonomic) over conscious activity, involuntary breathing and heartbeat is disrupted.
The diagnostic algorithm for suspected asystole includes:
- checking the patient’s response to voice and visual images;
- measurement of pulse on the carotid arteries;
- checking for breathing;
- reaction of the pupil to light (at night a special flashlight is used).
The diagnosis of “asystole” is made according to electrocardiography data, which determines the isoline (a flat line, without teeth or other signs of activity of the conduction system of the heart).
The prognosis for this disease depends on two circumstances: whether there is organic damage to the organ, and what is the level of destruction of the ventricles. The most serious diseases are those that appear after acute MI, as well as diseases such as cardiomyopathy and myocarditis. If the morphological changes are pronounced, fibrillation of both the atria and ventricles is possible. If the heart is not completely affected, this condition does not have a serious impact on the prognosis.
If supraventricular extrasystoles occur in a malignant form, atrial fibrillation may develop. If these are ventricular extrasystoles, persistent ventricular tachycardia may occur and death may occur. Functional type extrasystoles, as a rule, are benign.
Prevention
To avoid the development of primary asystole caused by damage to myocardial structures, it is necessary to implant a pacemaker in such a patient.
To prevent secondary asystole, somatic diseases should be identified and treated in a timely manner. There are no preventive measures that would be 100% guaranteed to prevent sudden cardiac arrest. Everyone is at risk - even healthy people.
General rules that minimize the risk of injury boil down to following the principles of a healthy lifestyle:
- Fight against bad habits - smoking, alcohol abuse, drug use.
- Full physical activity - walking, feasible sports, swimming, cycling.
- Proper nutrition - enriching the diet with vitamins and minerals, avoiding fast food, processed foods, and canned food.
- Optimal work and rest regime, eight hours of sleep at night.
- Timely treatment of existing diseases, sanitation of foci of infection.
- Self-monitoring of blood pressure and heart rate.
- Annual visit to a cardiologist for preventive purposes.
Asystole is a deadly condition that requires urgent hospitalization and emergency medical care. Even timely treatment measures do not always save the lives of patients.
Symptoms
Before the development of asystole, a prodromal period is observed, during which a general deterioration of the patient’s condition occurs. The patient experiences various symptoms indicating the onset of pathological processes in the cardiovascular system. This:
- general weakness;
- shallow breathing and shortness of breath;
- strong heartbeat;
- discomfort in the chest area.
The above symptoms occur in approximately two thirds of patients with asystole. The remaining group of patients does not feel any changes as the attack approaches. In them, the disease is detected suddenly, accompanied by the following symptoms:
- ari src=”https://mirkardio.ru/wp-content/uploads/2017/10/asistoliya-serdca-chto-ehto-takoe5.png” class=”aligncenter” width=”791″ height=”445″[ /img]
- decreased blood pressure;
- breathing problems.
After a few minutes, the patient’s well-being worsens, the heart stops working, which leads to poor circulation, loss of consciousness and respiratory arrest. This condition is considered clinical death. The patient can be brought back to life only if first aid is provided in a timely manner.
During cardiac arrest, some patients continue to breathe for several minutes. However, their low frequency and superficiality do not allow them to adequately saturate the body with oxygen.