Why does a pathological process develop?
For a major stroke, the reasons are the same as for smaller cerebral disorders:
- blockage of the vascular bed by a thrombus or atherosclerotic plaque;
- vessel damage.
Factors that provoke extensive cerebral infarction will be as follows:
- Atherosclerosis. Intravascular cholesterol deposits impede blood circulation, and a detached plaque can completely block the vessel.
- Thrombosis. Blood clots form on the walls of arteries in people with high blood viscosity. Separation of a blood clot and blocking of a vascular lumen by a clot is the cause of an acute ischemic attack. This pathology does not depend on age - it can develop at both 60 and 90 years.
- Hypertensive crises. Increases in pressure provoke vascular spasm, which does not always disappear after a decrease in blood pressure. Blood flow in a spasmodic cerebral vessel partially or completely stops.
Hemorrhage is provoked by other factors:
- weakness of the vascular wall;
- congenital vascular anomalies (pathological narrowings, kinks);
- aneurysm;
- head injuries.
The negative impact of provoking causes is enhanced by excess weight, endocrine pathologies and bad habits (smoking, alcohol).
Relatives who stand under the doors of the intensive care unit when their mother had a massive stroke at the age of 70 can hope for a more favorable ischemic form.
What to be prepared for after a cerebral hemorrhage
The consequences of a cerebral infarction can be expressed as follows:
- Partial or complete paralysis of the body;
- Paresis (numbness) of the limbs;
- The patient may lose the ability to walk and navigate in space;
- Impaired speech communication;
- Inability to swallow;
- Deafness, complete or partial;
- Changes in mental state;
- Inability to control urination and bowel movements;
- The need for constant care.
No doctor can answer the question about the patient’s further condition after a stroke; everything is very individual. But there are several signs that suggest the development of an unfavorable prognosis in an elderly person:
- Location of the lesion in the brain. If its most important centers are affected, the outcome will be fatal.
- The area of spread of hemorrhage, affecting the loss of many body functions.
- The most severe consequences are observed in patients with hypertension and atherosclerotic plaques on the vessels of the brain.
- A coma caused by cerebral edema sharply worsens the prognosis.
- A recurrent stroke usually ends in the death of the patient.
Factors that can lead to rehabilitation and recovery of an elderly patient:
- The hematoma is small in size, as confirmed by laboratory tests;
- The patient does not lose consciousness;
- Absence of heart disease, atherosclerosis of the head and neck vessels;
- Normal blood pressure.
Calling a doctor in a timely manner is of great importance. When admitted to the hospital within the first 6 hours, the likelihood of a favorable outcome of the disease increases significantly. The life of an elderly patient often depends on the experience and skillful actions of the specialist who comes to the call.
Typically, ischemic stroke is preceded by transient attacks. It is the recognition of the signs of these disorders and their treatment that will prevent the development of severe pathology of the cerebral blood supply. Prolonged post-stroke coma often leads to the death of the patient.
For patients over 80 years of age, the prognosis after a stroke is usually poor. This is primarily due to the presence of concomitant diseases and lack of support from a weakened immune system.
Often the likelihood of a cure is reduced due to the provision of unqualified care and the lack of opportunity to buy expensive medicines and pay for doctors’ services.
A patient over 80 years of age, more often than a young person, finds himself after a stroke in a state of coma, characterized by a loss of the body’s response to external impulses and an unconscious state.
The main signs of coma are that the patient cannot breathe on his own, blood circulation is impaired due to a drop in pressure in the vessels, and a constant state of fever. In most patients, if the coma lasts more than 7 days, death occurs.
When a stroke occurs in the left hemisphere, there is complete or partial paralysis of the right side of the body. The patient loses the ability to pronounce long phrases, understanding speech, he can only answer in monosyllables or in separate words.
When the right hemisphere is damaged, the motor function of the limbs on the left side is impaired. An elderly patient loses memory for immediate events, clearly remembering his past, his facial expression changes, as paralysis of his half occurs, and coordination of movements is impaired.
It is impossible to give a favorable prognosis after a stroke in elderly patients even if all recommendations are followed. However, you can significantly reduce the risk of a recurrent attack by changing your lifestyle for the next year allocated for rehabilitation:
- For elderly patients, proper nutrition is of particular importance: cereals, whole grain bread, vegetables and fruits. Even if there is no appetite, you still need to eat food, since the body needs support during the recovery period.
- Often, older patients experience complete or partial paralysis of the body. An anti-decubitus mattress will help prevent the development of skin infections. The patient needs to regularly change body position.
- Swelling of the legs develops gradually. To prevent it, diuretics are prescribed.
- Treatment of concomitant diseases is necessary.
Modern medicine believes that taking maintenance medications for older patients helps reduce the rate of ischemic attack and expand the “therapeutic window” (the period immediately after hemorrhage).
Constant use of such medications should be under medical supervision.
Thus, stroke is especially dangerous for older patients. The main consequence of an attack can be partial or complete paralysis of the body, leading to the inability of the patient to self-care. Visual and auditory dysfunctions are also common.
The patient’s psyche may change, he becomes whiny or, conversely, aggressive. The main goal of treatment and recovery after a stroke is to prevent another attack, which often ends in the death of the patient.
Source: stopinsult.ru
Types of major stroke
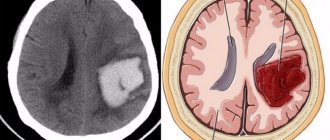
Acute cerebrovascular accidents are divided into ischemic and hemorrhagic. In the first case, the lumen of the artery closes, in the second, blood escapes from the damaged vessel. Various reasons lead to the development of these types of stroke. In addition, they differ in pathogenetic mechanisms and clinical presentation. Extensive stroke is divided into the following types:
- Hemodynamic. Vasospasm provokes a decrease in the amount of oxygen that reaches the brain tissue. The cause of this condition is often hypotension.
- Microocclusion. A stroke develops due to a local disturbance in blood flow.
- Lacunar. In the brain, due to increased pressure in the vessel, a cavity is formed. It is filled with liquid.
- Cardioembolic. Arrhythmias lead to the detachment of a blood clot. As a result of uneven contraction of the myocardium, blood turbulence occurs. The detached blood clot enters the brain vessel, causing the development of a stroke.
- Atherothrombotic. The cause of acute cerebrovascular accident is the blocking of the artery lumen by an atherosclerotic plaque. Atherosclerosis is formed due to changes in the lipid composition of the blood.
Although there are many types of stroke, a major one occurs when there is hemorrhage or ischemia. They have similar symptoms and progression rates, but the consequences will be different, as will the type of treatment. If with an extensive ischemic stroke the patient has a chance of full recovery, then with a large hemorrhagic stroke it is unlikely, and often people remain disabled due to hemorrhage.
An extensive ischemic stroke occurs due to blockage and thrombosis of blood vessels, as a result of which cells begin to starve without oxygen and die. In this case, lacunar, atherothrombotic, hemodynamic stroke, and micro-occlusion may develop. They are characterized by a sudden onset or a long period of development, so symptoms will appear gradually.
The main difference between a hemorrhagic extensive stroke is the rupture of blood vessels or aneurysms, hemorrhage in the brain, and the penetration of red blood cells through the walls of the heart. This happens suddenly and takes no more than four hours, during which all functions of the human body suffer. Often the process is painful, the patient may experience breathing and heart problems, speech impairment and even paralysis. Surviving this type of stroke is extremely difficult, especially after 50 years.
Diagnostic and treatment methods
Treatment tactics depend on the type of major stroke, the patient’s age, concomitant diseases and other factors. With the hemorrhagic type, it is important to eliminate the source of bleeding, and some patients may require surgery to remove the hematoma or aneurysm. For ischemic stroke, therapy is carried out in several directions:
- correction of breathing and heartbeat;
- elimination and prevention of brain swelling;
- thinning the blood and preventing the formation of blood clots;
- symptomatic treatment aimed at relieving seizures, fever and other clinical signs.
The Clinical Institute of the Brain has all the necessary conditions for the treatment and rehabilitation of patients with strokes. At the first stage, all procedures must be carried out in a hospital, under round-the-clock supervision of doctors. In addition, in the first weeks the likelihood of a second attack is increased, and it is important not to miss its first symptoms. After complete stabilization, treatment continues at home, with mandatory examinations and constant monitoring of the patient’s condition.
At-risk groups
Stroke is a pathology that can occur in people of any age group. But this is especially dangerous for people who fall into the following risk factors:
- People under 40 years of age who smoke a lot, abuse alcohol and take drugs;
- People from 40 to 60, and men after 50 years are more susceptible to this disease than women, but after 60 years the rates level out;
- People over 60 years old - at this age, as a rule, there are already plaques on the vessels, which significantly increase the risk of pathology. In addition, older people often suffer from hypertension, which leads to rupture of the vascular wall.
Thus, provoking factors can be combined into the following subgroups:
- advanced age;
- arterial hypertension;
- heart diseases;
- stress;
- bad habits;
- cholesterol imbalance;
- excess weight;
- hereditary predisposition;
- diabetes.
Description of the disease
An extensive cerebral stroke is a sudden disruption of blood circulation in the patient’s brain, which occurs against the background of a critical narrowing of large and small vessels. With a major stroke, a large area of the vascular bed suffers from vasospasm. However, the pathology can also be deep-seated. That is, in this case, large left or right carotid arteries are affected. But both hemispheres can be affected at once. With a larger number of dead neurons, the patient’s chance of survival and/or complete rehabilitation is significantly reduced. After suffering a pathology, the patient may experience complications, from partial impairment of motor activity of the muscles of the face and body to complete paralysis of the entire body.
Important!
The pathology mainly affects elderly people or people who have previously experienced ischemic attacks.
Other complications after an attack
Literacy and the quality of rehabilitation undoubtedly play a huge role in the rate of recovery. The chances of surviving the consequences of a major stroke in this context will depend on the patience, effort and care of the patient's family members. But no matter how hard friends and relatives try, cerebrovascular accidents can have an extremely negative impact on the brain centers, as a result of which the patient’s quality of life will leave much to be desired.
In addition to the above problems encountered during a stroke, other complications can negatively affect the patient’s recovery:
- Digestive disorders - they are caused by the patient’s bedridden state, as well as non-compliance with the diet. Constipation is especially dangerous - because of it, acts of defecation are accompanied by an increase in pressure.
- Atrophy of cartilage and muscle tissue - occurs against the background of prolonged lack of physical activity.
- Bedsores are ulcerative formations on the skin that can cause an inflammatory process if the necessary hygiene procedures are not followed.
- Pneumonia is a consequence of weakened immunity and insufficient ventilation in the premises.
Often, with an extensive cerebral infarction, complications begin to develop. It could be:
- swelling of the brain - most often diagnosed;
- weakening of the immune system and the development of congestive pneumonia against this background;
- the development of inflammatory processes in the urinary tract, which is explained by the emergence of difficulties with self-care in patients;
- problems with joint mobility, which is explained by prolonged periods of lying down;
- the appearance of bedsores against the background of constant lying, which provokes a serious disruption of blood flow with subsequent death of individual sections of tissue;
- deterioration of blood circulation and, as a consequence, the development of thrombosis;
- decreased tone in the intestinal walls, which results in a problem such as constipation.
Almost all people who have experienced a massive cerebral infarction/hemorrhage experience persistent impairment of motor, sensory, cognitive, and speech functions.
| Type of neurological deficit | Possible consequences of a major stroke |
| Paresis, paralysis of arms, legs, lower face |
|
| Impaired coordination, balance deficit |
|
| Visual impairment |
|
| Loss of sensation |
|
| Decrease in intelligence |
|
| Memory disorders |
|
| Speech disorders |
|
With a major stroke, it is quite difficult to eliminate the consequences of the stroke. Few people achieve full recovery. Rehabilitation helps many people achieve good results: the ability to take care of themselves independently or with minimal assistance, communicate, and lead a moderately active life. Without it, a person is often doomed to remain deeply disabled.
Restoring function after a major stroke takes a long time. Motor disorders can be eliminated in six months, memory and thought processes can be improved in a year. It takes the longest to restore speech – 2-3 years.
The rehabilitation program may include:
- kinesiotherapy;
- massages;
- physiotherapy;
- classes with a speech therapist-aphasiologist, neurologist, psychologist;
- special exercises for eyes, articulation;
- gaming techniques to improve coordination, memory, thinking;
- communication;
- learning memory techniques.
Features of left-sided and right-sided lesions
The symptoms of a dangerous disease and the rehabilitation period directly depend on which hemisphere was affected.
Left-sided lesions are characterized by the following symptoms:
- the patient loses sensation on the right side of the body, paralysis or paresis may occur;
- the patient practically loses vision in the right eye;
- speech becomes slurred and incoherent, and may be completely absent;
- the patient does not perceive other people’s speech, cannot think logically, read or write;
- the patient suffers from memory loss, forgets letters or numbers, and gets confused in performing simple actions.
Right-sided lesions are characterized by the following disorders:
- there is a loss of sensitivity on the right side of the body, a high probability of paralysis;
- the patient ceases to recognize close people;
- the patient develops an inadequate emotional state, he is unable to recognize human emotions, orient himself in time and space;
- the patient develops memory problems.
With left-sided brain damage, there is a greater chance of full recovery, and rehabilitation is faster than with damage to the right hemisphere.
How patients are treated
The therapy selected for the patient is influenced by whether a large stroke is bilateral or unilateral, as well as on which side the pathological focus is localized. Treatment is selected individually, but there are general rules:
- Improving blood supply to the brain. For this purpose, vasodilators and nootropics are used.
- Blood pressure control. Crises will negatively affect cerebral blood flow, so antihypertensive medications are selected.
- Prevention of thrombosis. They give it in tablets or give injections of blood-thinning medications.
How does treatment occur if vital functions are impaired or the patient is in a coma? These patients are connected to artificial life support, which means that a machine breathes for the person, and nutrition is given through a tube or administered by drip.
Coma as a consequence of a stroke
Coma is a borderline state when a person loses all vital functions. It often occurs in patients who have suffered a major stroke.
Identified by symptoms such as:
- lack of pupil reaction to light;
- loss of sensitivity of soft tissues;
- falling into deep sleep;
- inability to control vital processes.
In most cases, a comatose state does not bode well, since it is impossible to trace the dynamics of treatment and recovery, since brain activity is reduced to zero.
The gradual death of brain cells and the inability to regenerate them leads to the fact that a person loses the ability to live independently.
Almost all cases of coma in the post-stroke state are fatal.
Mechanism of violation
Another name for ischemia is cerebral infarction. As a result of a sharp restriction of blood supply, brain tissue dies. This condition often occurs due to rupture of an atherosclerotic plaque, blockage of the lumen of a vessel by an embolus or thrombus.
The cause of atherosclerosis is the deposition of cholesterol in the inner layer of the artery. A blood clot forms due to increased blood viscosity. This condition often occurs against the background of concomitant diabetes mellitus and tumor formations. A cerebral infarction develops due to a sudden cessation of blood flow to the brain tissue.
With the development of ischemic stroke of the left hemisphere, sensory disturbances and motor disorders appear on the right. Damage to the right hemisphere is accompanied by speech disorders. General cerebral symptoms include dizziness, nausea, loss of consciousness, and in rare cases, coma. Specific signs of ischemic stroke are considered to be a decrease or complete loss of sensitivity in the right half of the body, limited or absent movements in the limbs, problems with swallowing, and drooping of the corner of the mouth.
Among the main causes of hemorrhagic stroke are:
- uncontrolled arterial hypertension;
- excessively thin blood;
- congenital deformations of the vascular wall.
Rupture of blood vessels with subsequent leakage of blood into the brain cavity most often provokes a sharp rise in blood pressure. In addition to the listed etiological factors, aneurysm, traumatic brain injury, physical or emotional stress can cause hemorrhagic stroke.
Hemorrhagic stroke is characterized by a sudden and rapid onset. Symptoms include severe headache, rapid breathing, confusion, and possible development of coma. The skin becomes cold to the touch, the corner of the mouth droops, and blood pressure rises. Against the background of hemorrhage in the brain, the tone of the muscles of the limbs decreases, strabismus may appear, the pupils dilate, and swallowing is impaired. Hemorrhagic stroke has a less favorable course and is often accompanied by complications.
An extensive stroke differs from a localized form of the disease. They consist in the fact that other types of strokes are characterized by blockage of blood vessels in the brain (ischemic type of disorder) or hemorrhage (hemorrhagic), in which large vessels are damaged, and with an extensive stroke, the lesions are localized in several parts of the brain.
Because of the extensive damage to the brain, patients with a major stroke have little chance of survival, and survivors have little chance of regaining lost function.
First aid to the victim
In case of a major stroke, you should urgently call an ambulance. But there is no time to waste before she arrives.
First aid to a patient includes the following actions:
- First, the person should be placed in a horizontal position, with the head and upper torso positioned slightly above the general level of the body (it should be raised by 20-30 cm). This will slow down the development of cerebral edema.
- Provide maximum fresh air flow. To do this, you need to remove all restrictive clothing, belts, and ties from the patient. The windows in the room where it is located must be open (you must ensure that there is no draft).
- The respiratory tract should be cleared of mucus and vomit. It is important to ensure that the person’s tongue does not sink in, as it can block the airway. Be sure to turn your head to the side and remove the removable dentures.
- If the patient cannot breathe on his own, resuscitation must be carried out until the ambulance arrives.
About the correct algorithm for performing cardiopulmonary resuscitation:
- You should not give a person food, medications or water - this will only cause harm.
- If the victim's limbs are paralyzed, then they need to be rubbed.
Diagnosis of a major stroke involves an MRI or CT scan of the brain. These studies will determine the severity of the disease, the size of the affected areas, and their location.
Prevalence and development
According to statistics, more than 400 thousand patients with this diagnosis are registered in Russia every year, and 35% of them die. Around the world, there are approximately 12 million people affected by this disease every year.
A major stroke develops due to the formation of blood clots in large vessels. They cause either narrowing of the lumen or rupture of the vessel. In both cases, the disease develops.
The disease is dangerous for any age category (except children), but the causes of its occurrence and risk factors vary slightly.
- Young people (up to 40 years old). At this age, hemorrhagic major stroke is more common. Young people who abuse drugs and cigarettes are at risk.
- Middle-aged people (40-60 years old).
Men aged 40-50 years are more susceptible to this disease than women, but by the age of 60 the rates level out. The thing is that men aged 40-50 years are 19% more susceptible to atherosclerosis than women. By age 60, this percentage drops to almost zero. - Elderly people (over 60 years old).
At this age, the risk of occurrence is very high (increases almost 18 times). In people over 60 years of age, plaque forms on the inner surface of blood vessels, which leads to blockage or rupture and subsequent bleeding. Heart disease leads to the formation of blood clots. In older people, blood pressure can be high for a long time, which eventually leads to rupture of blood vessels.
People with diabetes and heart disease are more likely to have a stroke. Any vascular pathologies and heart diseases (blood flow disorders) also increase the risk of developing the disease.
First aid for stroke and heart attack
Signs of stroke and heart attack develop suddenly, rapidly and can take you by surprise at home, at work or on vacation. Providing first aid for a heart attack and stroke begins with calling an ambulance.
At home in case of a heart attack you need to:
- calm down;
- provide access to fresh air;
- give a comfortable position with the head end of the bed raised;
- let chew 300 mg. aspirin (“aspirin cardio”, “magnicor”).
If the patient loses consciousness, it is necessary to assess the presence of spontaneous breathing and pulse. If breathing and pulse in the carotid artery are not detected, begin a set of resuscitation measures, according to the algorithm, as in the video in this article:
With a stroke, everything is more complicated. Without knowing the mechanism of development of the disease, you should not start any measures. Medicines for stroke and heart attack are different. Using the same medications at home can be dangerous.
A patient with stroke symptoms must be provided with complete rest, access to fresh air, and high blood pressure reduced, but not more than 10% of the initial level (tissue hypoperfusion can lead to a worsening of the condition).
Patients in a coma need to ensure airway patency. You can place the patient on his side in a stable position, and if the tongue is retracted, perform the Safar maneuver, as in the photo:
Reception of Safar
If convulsions develop, you need to lay the patient on a flat surface and place a pillow under the head or roll up a blanket so that the patient does not get injured.
Rehabilitation and prevention of complications
Full recovery after a major stroke is only possible if the patient is young, does not have serious illnesses, and important centers are not affected. This happens in 3-5% of victims.
Rehabilitation after a major stroke has the following goals:
- if possible, restore impaired functions (whether the brain is restored depends on the severity of the pathological process);
- provide the patient with adequate care (prevention of bedsores, prevention of diseases caused by a sedentary lifestyle);
- social adaptation (it is necessary to teach a person to live with the disorders that have arisen, to find something to do to prevent depression)
- the work of exercise therapy doctors, speech therapists and other specialists.
Whether it is possible to recover from an attack or whether a person will remain disabled forever depends on many factors. And in most cases, with large cerebral injuries, even with good care and competent actions of doctors, recovery is impossible.
Survival prognosis
It is quite difficult to make a prognosis for any type of stroke, since everything depends on the degree of damage to brain tissue. However, extensive organ damage does not provide a chance of survival. In addition, the patient may soon experience another stroke. The chances of survival depend on several factors:
- Age. It is easier for a young body to cope with the consequences of pathology, since regeneration processes occur faster. In older age, the patient's incapacity is guaranteed.
- State of health at the time of hemorrhage. This is especially true for the cardiovascular system.
Report by neurologist Mikhail Moiseevich Shperling on the care of patients who have suffered a stroke:
- Bad habits. It is more difficult for an organism affected by nicotine and alcohol to fight the consequences of the disease. In such patients, the mortality rate is very high.
- Speed of emergency care.
- Patient care. Those people who are surrounded by the care and love of loved ones, receive positive emotions and support from them, and recover faster.
If the patient is bedridden, then it will be more difficult to cope with the disease. It is important to ensure cleanliness and comfort for the person and to prevent bedsores. Proper nutrition is also necessary.