Anaphylactic shock is a common emergency condition that can be fatal if treated incorrectly or delayed. This condition is accompanied by a large number of negative symptoms; if these occur, it is recommended to immediately call an ambulance and provide first aid yourself before it arrives. There are measures to prevent anaphylactic shock that will help prevent the condition from recurring.
What is anaphylactic shock?
Anaphylactic shock (anaphylaxis) is an acute, rapidly developing and deadly allergic reaction of the body to an allergen.
Anaphylactic shock is an immediate allergic reaction, most often manifested when the allergen re-enters the body. The development of anaphylaxis is so rapid (from a few seconds to 5 hours from the beginning of contact with the allergen) that if the emergency care algorithm is incorrect, death can occur literally within 1 hour!
As we have already noted, anaphylactic shock, in fact, is a super-strong (hyperergic) response of the body to the entry of a foreign substance into it. When an allergen comes into contact with antibodies, which have the functions of protecting the body, special substances are produced - bradykinin, histamine and serotonin, which contribute to the disruption of blood circulation, disruption of the muscular, respiratory, digestive and other systems of the body. Due to disruption of normal blood flow, organs throughout the body do not receive the necessary nutrition - oxygen, glucose, nutrients, starvation occurs, incl. brain. At the same time, blood pressure drops, dizziness appears, and loss of consciousness may occur.
Of course, the manifestations described above are not a normal reaction of the body to an allergen. What is observed with anaphylaxis indicates a malfunction in the immune system, therefore, after providing emergency care for anaphylactic shock, therapy is also aimed at normalizing the functioning of the immune system.
According to statistics, anaphylaxis is fatal in 10-20% of cases if it is caused by the administration of a drug (drug allergy). In addition, from year to year, the number of manifestations of anaphylactic shock is growing. This is due, first of all, to the deterioration of the general health of a large number of people, the low quality of modern food products and the frivolous use of medications without consulting doctors. Statisticians also note that the manifestation of anaphylaxis is more noticeable in women and young people.
For the first time, the term “Anaphylactic shock” appeared in the scientific world at the beginning of the 20th century, when it was introduced into use by 2 people - Alexander Bezredka and Charles Richet.
Anaphylactic shock. ICD
ICD-10: T78.2, T78.0, T80.5, T88.6; ICD-9: 995.0.
How to recognize cardiogenic shock
To provide first aid, you need to know how this condition manifests itself.
- A sharp decrease in blood pressure (systolic (upper) below 90 mm Hg).
- Pale skin, possible cyanosis, “marbled” spotting.
- Increased sweating.
- Cold extremities.
- Confusion.
- Accelerated heartbeat, weak pulse, difficult to palpate.
- Pulmonary edema (manifested by suffocation, rapid breathing, wheezing, and sometimes foamy sputum).
- Possible loss of consciousness.
If you find similar symptoms in any of your relatives or others, immediately call an ambulance.
For emergency cardiogenic shock, the algorithm is as follows:
- Call an ambulance.
- Place the patient on his back. Raise your legs slightly (this is necessary in order to improve blood flow to the brain and heart).
The most important thing is to call an ambulance in time, since only emergency resuscitation measures performed by specialists can help the patient.
Causes of anaphylactic shock
The cause of anaphylactic shock can be an incredible number of different allergens, so we will note the most common of them:
Insect bites
From year to year, an increasing number of insect bites are observed. Accordingly, the percentage of not only anaphylaxis, but also deaths is increasing. The most common species that bite humans are wasps, bees, and hornets. Moreover, the simultaneous bite of several insects in most cases provokes the development of anaphylactic shock. Moreover, it was noticed that if a person was bitten by a wasp, and everything passed, i.e. nothing happened beyond local edema, then the next bite is accompanied by more severe manifestations, even if this next time will be in a year or two. I recommend that you, dear readers, read the article - what to do if you are bitten by a wasp, bee or bumblebee.
Read also Adnexitis - symptoms, causes, types and treatment of adnexitis
Animal bites
The development of anaphylactic shock can also be triggered by bites of various animals, for example, snakes, spiders, various centipedes, exotic frogs, etc. In fact, the reaction can be caused by any representative of the animal kingdom that releases poison when biting its victim. It will be very useful to read the article - what to do if you are bitten by a snake.
Food
Due to the fact that the body, due to various GMO products, does not receive the required amount of vitamins and microelements, as well as many people replacing normal food with fast food products and other unhealthy foods, many people experience various disturbances in the functioning of the body. In addition, allergies to various products are increasingly observed, with about 30% of allergy sufferers susceptible to anaphylaxis.
Highly allergenic food products include:
- nuts and their derivatives - peanuts and peanut butter, almonds, hazelnuts, walnuts, etc.;
- seafood - shellfish, crabs, some types of fish;
- dairy products, eggs;
- berries and fruits - citrus fruits, strawberries, grapes, bananas, pineapples, pomegranate, raspberries, apricots, mangoes;
- other products: tomatoes, chocolate, green peas, honey.
Medicines
Due to the rapid development of the media, many people, without consulting their doctor, often unwisely use certain drugs that can not only cure, but also significantly worsen a person’s health condition. You need to understand that some drugs are prescribed only in combination with other drugs, but all the details are usually outlined by the doctor based on an examination and thorough diagnosis of the patient.
Let's look at medications that carry a risk of developing anaphylaxis:
Antibiotics , especially penicillin (“Ampicillin”, “Bicillin”, “Penicillin”) and tetracycline series, sulfonamides, “Levomycetin”, “Streptomycin”, etc. The statistics of cases of anaphylaxis is 1 in 5000.
Nonsteroidal anti-inflammatory drugs (NSAIDs) - Aspirin, Ketoprofen, Paracetamol, etc. The statistics of cases of anaphylaxis is 1 in 1500.
Angiotensin-converting enzyme (ACE) inhibitors used in the treatment of hypertension - “Captopril”, “Enalopril”, etc. The statistics of cases of anaphylaxis is 1 in 3000.
Anesthetics used for various surgical interventions - Ketamine, Propofol, Thiopental, Halothane, Sevovluran, etc. The statistics of cases of anaphylaxis is 1 in 10,000.
Other medications: vaccines, serums.
Contrast agents
Contrast agents are injected into a person's body intravenously to perform a series of radiological health tests - computed tomography (CT), angiography and fluoroscopy. Contrast agents literally highlight various organs for more detailed diagnostics. The incidence rate of anaphylaxis is 1 in 10,000.
Other reasons
Other causes of anaphylaxis include household chemicals (direct contact and inhalation of vapors), animal hair, inhalation of vapors (perfumes, deodorants, varnishes, paints, house dust), cosmetics (hair dyes, mascara, lipstick, powder), vitamin B1 (Thiamin), artificial materials (latex), etc.
Diagnostic methods
Cardiogenic shock is diagnosed in severe situations. Doctors will check for signs and symptoms of shock and then perform additional tests to determine what is causing this serious condition. Diagnosis of cardiogenic shock includes:
Blood pressure measurement.
The main symptom of cardiogenic shock is a drop in blood pressure. If a patient is in shock and is taken to the hospital by ambulance, blood pressure will be measured before arriving at the hospital.
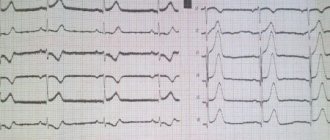
Electrocardiogram (ECG).
This is the first test that must be performed to diagnose myocardial infarction. The essence of this method is to record electrical potentials that arise during the work of the heart and to display them graphically on paper or a monitor. The electrical activity of the heart is recorded using electrodes attached to the skin.
Chest X-ray.
X-rays will allow your doctor to determine the size and shape of your heart and blood vessels.
Blood tests.
Laboratory research methods are necessary to clarify the degree of damage to the kidneys and liver, determine infectious damage to the heart and diagnose myocardial infarction. Another type of blood test (arterial blood gases) can determine how much oxygen is in the blood.
Echocardiogram. (EchoCG).
This method is based on the ability of ultrasound to be reflected from tissues, perceived by the device and converted into an electrical signal, transmitting an image of the heart muscle to the monitor. EchoCG allows you to determine the contractility of the myocardium, the size of the heart cavities, the condition of the valves, their functioning, the thickness of the walls of the heart, atria, ventricle, identify cicatricial changes in the heart, and the presence of intracardiac blood clots.
Coronary angiography
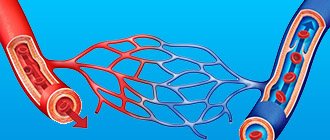
Coronary angiography (angiography).
This method identifies narrowed or closed (occluded) coronary arteries. Liquid contrast is injected into the arteries of the heart, through a special device (catheter), which is brought to the arteries, through a puncture (puncture) in the femoral artery. The contrast agent fills the arteries, the arteries become visible on x-rays and this allows you to accurately determine the nature, degree and location of narrowing of the coronary arteries.
In addition, through a catheter, the doctor can eliminate stenosis in the coronary artery by performing angioplasty. Angioplasty is performed using a small balloon that is inserted into the affected area of the coronary artery, where it is inflated and thereby eliminates the narrowing in the artery. In most cases, the use of intravascular stents is necessary. This reduces the incidence of re-narrowing in the coronary artery.
Symptoms of anaphylactic shock
Signs of anaphylactic shock can appear within a few seconds after contact with the allergen.
The first symptoms of anaphylactic shock:
- general weakness;
- dizziness, clouding of consciousness;
- feeling of heat in the body;
- convulsions;
- drop in blood pressure;
- cardiopalmus;
- involuntary urination, defecation;
- strong fear, panic;
- headache;
- chest pain;
- hyperemia, as well as blanching of the skin;
- increased sweating.
Other symptoms of anaphylactic shock include:
- changes in the skin - hyperemia, urticaria, severe itching, Quincke's edema;
- disorders of the respiratory system - shortness of breath, suffocation, swelling of the mucous membranes of the respiratory system and spasms in the upper respiratory tract, a feeling of a lump in the throat;
- swelling of the facial part - eyes, lips, tongue;
- dilated pupils;
- stuffy ears
- taste disturbances;
- nausea, vomiting;
- increased tactile sensitivity;
- blueness of fingers and toes;
- myocarditis, myocardial infarction.
Read also Abscess - symptoms, causes and treatment of abscess
Clinical symptoms and diagnosis
With cardiogenic shock, almost all patients experience the following symptoms:
- severe pallor of the skin, blue lips and fingers;
- confusion or loss of consciousness;
- sticky and cold sweat;
- rapid breathing;
- frequent, but barely palpable pulse (so-called threadlike).
In addition, most patients complain of severe chest pain - a sign of myocardial ischemia. These symptoms may also be present in other diseases, so it is impossible to make diagnoses on your own, much less give any cardiac medications to the patient; doctors will carry out an accurate diagnosis. They will measure blood pressure, do an ECG and perform other tests to determine the severity of the patient’s condition.
Types of anaphylactic shock
Anaphylactic shock is classified as follows:
With the flow:
- Mild flow;
- Moderate course;
- Heavy current.
According to clinical manifestations:
Typical option. General symptoms.
Hemodynamic option. Anaphylaxis is accompanied by disturbances in the functioning of primarily the cardiovascular system - pain in the heart, a drop in blood pressure, disturbances in the rhythm of the heart, disturbances in blood flow. The hemodynamic variant of anaphylaxis has 4 degrees of severity.
Asphyxial option. Anaphylaxis is accompanied by disturbances in the functioning of primarily the respiratory system - breathing problems, swelling of the respiratory tract (throat, bronchi, lungs), shortness of breath.
Cerebral option. Anaphylaxis is accompanied by disturbances in the functioning of mainly the central nervous system (CNS) - fears, cerebral edema, dizziness, convulsions, loss of consciousness, cardiac and respiratory arrest.
Abdominal option. Disturbances occur mainly in the abdominal region - abdominal pain, nausea, vomiting, spontaneous urination and defecation, swelling of the gastrointestinal tract.
According to the nature of the flow
- Acute malignant
- Benign
- Zyatyazhnoe
- Recurrent
- Abortive.
How to recognize cardiogenic shock
To provide first aid, you need to know how this condition manifests itself.
- A sharp decrease in blood pressure (systolic (upper) below 90 mm Hg).
- Pale skin, possible cyanosis, “marbled” spotting.
- Increased sweating.
- Cold extremities.
- Confusion.
- Accelerated heartbeat, weak pulse, difficult to palpate.
- Pulmonary edema (manifested by suffocation, rapid breathing, wheezing, and sometimes foamy sputum).
- Possible loss of consciousness.
If you find similar symptoms in any of your relatives or others, immediately call an ambulance.
For emergency cardiogenic shock, the algorithm is as follows:
- Call an ambulance.
- Place the patient on his back. Raise your legs slightly (this is necessary in order to improve blood flow to the brain and heart).
- Provide the victim with complete rest until paramedics arrive.
- Unfasten or loosen all clothing, especially tight clothing (tie, belt, bra, etc.).
- Open a window to get more fresh air.
- If a person loses consciousness, perform cardiopulmonary resuscitation (chest compressions, artificial respiration). Perform these steps only if you have the appropriate skills. If you don't know how to do this, you can only do harm.
- When the doctors have already arrived, clearly describe to them all the patient’s symptoms and all the actions you performed. If you have such information, then tell the doctors what medications the victim took, what cardiovascular and other chronic diseases he suffered from. This will help them make a diagnosis.
The most important thing is to call an ambulance in time, since only emergency resuscitation measures performed by specialists can help the patient.
Diagnosis of anaphylactic shock
Diagnosis of anaphylactic shock is usually determined by the clinical picture. A full diagnosis is carried out after first aid, because Literally every second counts. Of course, if an allergic reaction begins, it is advisable to tell the doctor when it appeared, as well as how much time has passed since contact with the allergen.
After emergency care, a detailed diagnosis of the patient includes the following studies:
- allergy history;
- skin and patch tests (Patch test);
- blood test for total immunoglobulin (IgE);
- provocative tests.
The purpose of the research is to determine the causative agent of the allergic reaction.
Complications and prognosis for the patient
Cardiogenic shock is a deadly condition. The main role in reducing the mortality rate is played by the time of emergency care. If the necessary measures were taken within the first 30 minutes after the development of the first symptoms, the mortality rate does not exceed 30-40%. Relief of shock at a later date leads to a progressive increase in the percentage of deaths.
Further prognosis depends on the etiology of cardiogenic shock, the degree of damage to the heart muscle and the severity of multiple organ failure.
Emergency care for anaphylactic shock
The algorithm of actions for anaphylactic shock includes the following points of first emergency aid (pre-hospital):
1. It is necessary to immediately stop contact with the allergen.
2. Lay the victim, if possible, so that his head is below the level of his feet; for this, you can put something under his feet. Turn your head to the side so that if vomiting occurs, the person does not choke on the vomit. If the person has dentures, remove them.
3. Remove tight clothing from the person and provide free access to air.
4. If an allergic substance was injected into a limb, apply a tourniquet above the injection site (for 25 minutes), which will prevent the rapid spread of the antigen throughout the body.
5. If blood pressure does not drop, give the victim an antihistamine to drink: Suprastin, Tavegil. If possible, administer them intramuscularly, which will speed up their action.
6. Inject a 0.1% solution of adrenaline into the frenulum of the tongue (sublingually) or intramuscularly. The dose for adults is 0.3-0.5 ml, for children - 0.05-0.1 ml/year of life. To administer adrenaline intravenously, it must be diluted with saline in a ratio of 1:10 to obtain a solution of 0.01% adrenaline.
7. Also inject the injection site with a solution of adrenaline, in dosages for adults - 0.3-0.5 ml, children - 0.1 ml/year of life, diluted with 4.5 ml of saline.
8. If you know the place where the allergen got in (insect bite, injection, etc.), apply something cold there. Ice or a chilled bottle of water is a great option. This will slow down the process of absorption of the allergic substance by the body.
9. Call a doctor immediately. It would be great if someone called a doctor at the very beginning, during an emergency.
Important! When providing first aid for anaphylactic shock, do not forget to monitor your blood pressure.
10. In case of cardiac arrest, begin artificial ventilation and chest compressions.
First medical aid for anaphylactic shock
The following measures are taken if the victim’s condition does not improve, but rather worsens.
Read also Sphenoiditis. Symptoms, causes, types and treatment of sphenoiditis
1. Adrenaline solution is continued to be administered intramuscularly and intravenously, in dosages for adults - 0.3-0.5 ml, for children - 0.05-0.1 ml/year of life. The frequency of injections is 5-10 minutes. The dose may be increased if blood pressure continues to fall and clinical manifestations worsen. A single dose of 0.1% adrenaline solution should not exceed 2 ml.
2. If the blood pressure level does not normalize, it is necessary to start intravenous drip administration of 0.2% norepinephrine (Dopamine, Mezaton), at a dose of 1.0-2.0 ml per 500 ml of 5% glucose solution. Instead of glucose, you can use saline solution.
3. Glucocorticosteroids are administered intravenously:
- "Dexamethasone": adults - 8-20 mg, children - 0.3-0.6 mg/kg;
- "Prednisolone": adults - 60-180 mg, children - 5 mg/kg.
Hormones are administered over 4-6 days.
4. After normalizing blood pressure, an antihistamine is administered intramuscularly:
- "Suprastin" (2% solution): adults - 2.0 ml, children - 0.1-0.15 ml/year of life;
- "Tavegil" (0.1% solution): adults - 2.0 ml, children - 0.1-0.15 ml/year of life;
Symptomatic treatment
With bronchospasm. A 2.4% solution of aminophylline in saline is administered intravenously, in a dose for adults - 10.0 ml, for children - 1 ml/year of life. Additionally, respiratory analeptics and cardiac glycosides (Digoxin, Strophanthin) can be administered.
If vomit enters the respiratory tract, suction is started and oxygen therapy is used.
For anaphylaxis from penicillin antibiotics, 1670 IU of penicillinase diluted with 2 ml of saline is administered intramuscularly.
After providing emergency medical care for anaphylactic shock, the patient must be hospitalized for a minimum period of 10 days. During inpatient observation and symptomatic treatment, the patient may still experience late allergic reactions after anaphylactic shock. At this time, it is very important to receive qualified medical care.
How to recognize cardiogenic shock
To provide first aid, you need to know how this condition manifests itself.
- A sharp decrease in blood pressure (systolic (upper) below 90 mm Hg).
- Pale skin, possible cyanosis, “marbled” spotting.
- Increased sweating.
- Cold extremities.
- Confusion.
- Accelerated heartbeat, weak pulse, difficult to palpate.
- Pulmonary edema (manifested by suffocation, rapid breathing, wheezing, and sometimes foamy sputum).
- Possible loss of consciousness.
If you find similar symptoms in any of your relatives or others, immediately call an ambulance.
For emergency cardiogenic shock, the algorithm is as follows:
- Call an ambulance.
- Place the patient on his back. Raise your legs slightly (this is necessary in order to improve blood flow to the brain and heart).
The most important thing is to call an ambulance in time, since only emergency resuscitation measures performed by specialists can help the patient.
Treatment of anaphylactic shock
After anaphylactic shock, symptomatic treatment of the patient is continued, which includes:
Taking antihistamines , which are used for outbreaks of an allergic reaction - Loratadine, Claritin, Suprastin.
Taking decongestants , which are used for allergic reactions in the respiratory system - “Xylometazoline”, “Oxymetazoline”. Contraindications: nursing mothers, children under 12 years of age, hypertension.
The use of leukotriene inhibitors , which relieve swelling of the respiratory system and eliminate bronchospasms - Montelukast, Singulair.
Hyposensitization. This method involves the systematic gradual introduction of small doses of a large number of allergens, which is aimed at developing the body's resistance to allergens, and accordingly minimizing repeated attacks of acute allergic reactions, including anaphylactic shock.
Mechanism of disease development
The pathogenesis of the disease is as follows: when the left ventricular myocardium, conduction system or valvular apparatus of the heart is damaged, cardiac output decreases. This leads to a persistent drop in systolic blood pressure, provoking inadequate and insufficient blood circulation in the central nervous system and other organs and systems.
Multiple organ failure is formed, which has the following manifestations:
- Kidneys. A decrease in blood flow in the renal arteries leads to disruption of the organ, which is expressed by a decrease (oliguria) or complete absence (anuria) of urine excretion, as well as the accumulation in the blood of toxic products of nitrogen metabolism - residual nitrogen and urea.
Decreased blood flow in the renal arteries
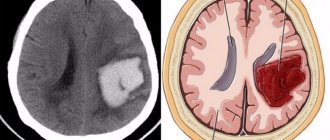
- CNS. Oxygen starvation of the brain leads to psychomotor agitation, which later gives way to depression of consciousness. The functioning of the vascular and respiratory centers is disrupted, which aggravates the course of cardiogenic shock.
- Heart and blood vessels. In conditions of insufficient oxygen supply in the tissues, the process of anaerobic glycolysis starts, which leads to the accumulation of lactate (metabolic acidosis). The permeability of the walls of blood vessels through which blood plasma exits increases, its thickening and intravascular coagulation develop. Central venous pressure drops, exacerbating damage to the heart muscle.
- Lungs. With insufficient contractile function of the left ventricle, its diastolic volume increases, which leads to an increase in pressure in the pulmonary circulation, up to the capillary bed. Plasma leaks through the walls of blood vessels into the lung tissue, and pulmonary edema develops.
Prevention of anaphylactic shock
Prevention of anaphylactic shock includes the following rules and recommendations:
— storage of a medical card indicating all information about allergic reactions to a particular substance;
- if you are allergic, always carry with you an allergy passport and a set of emergency medications: antihistamines (Suprastin, Tavegil), a tourniquet, a solution of adrenaline with saline, cardiac glycosides (Digoxin, Strophanthin).
- do not use medications without consulting a doctor, especially injections;
- use traditional methods of treating diseases only after consulting a doctor;
- try to wear clothes mainly made from natural fabrics;
— use household cleaning products with gloves;
— use chemicals (varnishes, paints, deodorants, etc.) only in well-ventilated areas;
- exclude immunotherapy for uncontrolled bronchial asthma;
- avoid contact with stinging insects - wasps, bees, hornets, bumblebees, as well as other animals - snakes, spiders, exotic frogs and other representatives of exotic fauna;
- if an allergy occurs, consult your doctor, do not leave the course of the disease to chance.
Prehospital diagnostics
In a condition such as cardiogenic shock, diagnosis is based on identifying myocardial infarction or a factor that could provoke a drop in systolic function of the heart: hemodynamically significant arrhythmia, poisoning with cardiotropic poisons, cardiac injury and tamponade, pulmonary embolism, myocarditis, rupture of the papillary muscles of the left ventricle, destruction of the mitral valve or aortic valve with endocarditis.
These studies are appropriate at the prehospital stage and represent the minimum set of measures that will make it possible to clarify the cause of shock and act etiotropically. In particular, an ECG in 100% of cases will reveal a hemodynamically significant arrhythmia and in 98-100% will show the presence of transmural myocardial infarction.
Although in such a condition as cardiogenic shock, emergency care is provided at the stage of syndromic diagnosis (shock of unspecified etiology). Then an infusion of cardiotonic is established, oxygen therapy, narcotic pain relief, anticoagulant treatment, and hemodynamic unloading of the pulmonary circulation are performed.