At certain intervals, people undergo a general blood test . The results of this clinical study show how well the body functions.
If any organs or systems fail, this almost always affects the quality of the blood. Today, patients present with microcytosis . Many people are frightened by such a diagnosis, without even understanding what it is. In fact, such a violation in itself is not dangerous. It only indicates that certain problems are occurring in the body.
Microcytosis: normal or pathological?
Blood consists of four main elements: plasma, platelets, leukocytes and red blood cells. In microcytosis, red blood cells are affected . Red blood cells decrease significantly in size. Most often, this is not considered the norm. Identification of such a violation indicates problems in the body. The size of a red blood cell in a healthy person is 7.5 micrometers. If the red blood cells are smaller in size, they are called microcytes, and if they are larger, they are called macrocytes.
When a small amount (up to 30%) of cells of the wrong size is present in the blood, this can be considered normal . However, if there are more pathologically altered blood cells than normal ones, then the patient is sent for additional examinations.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
Microcytosis is a type of anisocytosis . At the same time, platelets and red blood cells of different sizes are present in the blood: small, normal and large. If there are more than 30% microcytes in the blood, then this is dangerous to health .
The fact is that red blood cells perform an important function. They move through the vessels and supply all organs with oxygen. If their size is smaller than required, then they cannot carry a sufficient amount of oxygen. The organs are not sufficiently nourished with blood, and additional diseases develop. In this regard, a decrease in hemoglobin levels, iron deficiency or anemia is also noted.
This condition requires immediate action. The doctor must refer the patient for a comprehensive diagnosis and prescribe therapy.
What is blood macrocytosis in a general analysis?
An increase in the average volume of red blood cells of more than 100 fL (femtoliters) occurs in 3% of the general population. According to the study, 7% of patients had a mean red blood cell volume greater than 96 fL, and 1.7% had a mean red blood cell volume greater than 100 fL. With the increasing use of automatic blood analyzers and the prescription of certain medications, this pathology will occur more often in general practice.
Hypothyroidism (in combination with anemia) is the most common cause of macrocytosis in older people compared to other age groups.
The results of the New York study indicate that AIDS drugs now emerge as the most common cause of macrocytosis.
In some patient populations, 80% of cases of macrocytosis are due to alcoholism. Recently, a connection has been identified between Helicobacter pylori and vitamin B12 deficiency.
Pathophysiology of macrocytosis
Etiological factors of macrocytosis are divided into two groups: megaloblastic and non-megaloblastic. With megaloblastic factors, macroovalocytes and supersegmental neutrophils are detected in a peripheral blood smear (Fig.
1), and in non-megaloblastic ones - round macrocytes or macroreticulocytes (Fig. 2).
Since the mechanisms of macrocytosis are not completely clear, the division into megaloblastic and non-megaloblastic factors is somewhat relative.
Rice. 1. Megaloblastic anemia with macroovalocytes (thin arrows) and supersegmental neutrophils (thick arrow). Fig. 2. Microangiopathic hemolytic anemia (non-megaloblastic) with polychromatophilic macrocytes (thin arrows) and neutrophils with normal segmentation (thick arrow). Short arrows indicate schistocytes—cells characteristic of this pathology.
Differential diagnosis of macrocytosis
Megaloblastic factors (including vitamin B12 and/or folic acid deficiency) Non-megaloblastic factors False macrocytosis
|
|
|
In megaloblastic processes, the precursors are larger in size than mature red blood cells, since deficiency of folic acid and vitamin B12 impairs the synthesis of RNA and DNA and leads to increased levels of homocysteine and methylmalonic acid in the blood serum. These markers can be used to determine the etiology of megaloblastic anemia, although appropriate tests are not yet very common in routine clinical practice.
In non-megaloblastic processes, macrocytosis occurs due to increased red blood cell synthesis through hemolysis or loss of red blood cells (bleeding). Reticulocytes are immature red blood cells, so they are larger in size than mature red blood cells. The pathophysiological mechanisms by which other diseases cause macrocytosis are not clearly understood.
False macrocytosis
In addition, it is necessary to exclude false macrocytosis (occurs infrequently), which can be caused by cold agglutinins, hyperglycemia, or leukocytosis. Through cold agglutinins, red blood cells stick together, so the automatic analyzer shows a larger volume.
Against the background of hyperglycemia, the blood is more concentrated, so when it is diluted to determine the average volume of red blood cells, the cells swell more than usual - an error occurs.
With severe leukocytosis, the transparency of the blood sample decreases, so the automatic analyzer overestimates the size of the cells.
Macrocytosis in general blood test
Once macrocytosis is detected, the differential diagnosis can be narrowed based on history and physical examination. Attention should be paid to the presence of anemia, the degree of increase in the average volume of red blood cells and the general health of the patient.
A thorough examination is indicated when the diagnosis is unclear or there is anemia (according to WHO criteria, anemia is diagnosed based on a decrease in hemoglobin levels below 130 g / l in men and 120 g / l in women).
Diagnosis of macrocytosis
Diagnosis should begin with an extensive complete blood count (including reticulocytes) and determination of serum vitamin B12 levels. If the number of reticulocytes is increased, bleeding or hemolysis should be suspected, although reticulocytosis also occurs in the recovery period after anemia.
It is very important to begin testing for vitamin B12 levels because if vitamin B12 deficiency remains undiagnosed, megaloblastic anemia can be corrected with folic acid replacement therapy, but the patient will not get rid of the neurological symptoms caused by vitamin B12 deficiency.
If an accurate diagnosis cannot be established based on the history and physical examination, complete blood count, vitamin B12 level and reticulocyte count, metabolic tests should be performed to exclude liver and kidney diseases, thyroid hormone levels to exclude thyroid pathology, homocysteine and methylmalonic acid levels to rule out vitamin B12 deficiency despite normal serum vitamin B12 levels.
If the cause of macrocytosis still cannot be determined, the severity of the anemia and the patient's general health should be used to determine the indication for referral to a hematologist for a bone marrow biopsy or to rule out a rare etiology. After a thorough examination, an accurate diagnosis can be made in 90% of patients.
Vitamin B12 deficiency
Vitamin B12 is absorbed in the ileum only in a bound state with intrinsic factor, which is synthesized in the parietal cells of the gastric mucosa.
In pernicious anemia, a lack of parietal cells leads to insufficient absorption of vitamin B12, and over time, a deficiency of this vitamin occurs.
Most often, pernicious anemia is caused by autoimmune atrophic gastritis, in which antibodies are synthesized against parietal cells and intrinsic factor. Less commonly, pernicious anemia is caused by gastritis caused by H. pylori and Zollinger-Ellison syndrome.
Patients with vitamin B12 deficiency may complain of: paresthesias associated with peripheral neuropathy, poor nutrition or vegetarianism, socioeconomic problems, bowel dysfunction (including diarrhea), bowel surgery. During a physical examination, neurological symptoms are revealed: ataxia, decreased proprioceptive and vibration sensitivity. In addition, dental problems or nonspecific stomatitis or glossitis occur.
Because women routinely take folic acid as part of their perinatal vitamins, anemia is much less common during pregnancy.
In individuals at risk, nitric oxide abuse should be avoided as it inactivates vitamin B12 through oxidation.
Other rare etiologies include infection with Diphyllobothrium latum (broad tapeworm) or congenital disorders of cobalamin metabolism, including Imerslund syndrome (congenital malabsorption of vitamin B12 combined with proteinuria).
Only 10% of patients with vitamin B 12 deficiency have anemia.
If the serum vitamin B12 level is below the lower limit of normal (100-400 pg/ml [74-295 pmol/l]), the level of methylmalonic acid and homocysteine should be determined and, if these markers are elevated, the patient is diagnosed with vitamin B12 deficiency . The Schilling test (measuring the level of absorption of vitamin B12 in the intestine) is now rarely performed.
The effectiveness of oral vitamin B12 therapy is the same as intramuscular administration. Relapse of pernicious therapy occurs on average 65 months after completion of treatment.
Therefore, it is important for patients to agree to a long course of treatment, since vitamin deficiency will reoccur if treatment is stopped, unless the etiology of vitamin B12 deficiency has been diagnosed and corrected.
Folate deficiency
The etiology of folic acid deficiency may resemble that of vitamin B12 deficiency due to malnutrition or malabsorption.
In addition, 35% of alcoholic patients with macrocytic anemia have folate deficiency due to an unbalanced diet, malabsorption, digestive dysfunction, and possibly increased folate catabolism.
Folate deficiency is caused by some medications used to treat seizures, cancer, and autoimmune diseases. For example, methotrexate directly inhibits dihydrofolate reductase, which leads to functional folic acid deficiency.
The following drugs affect the metabolism of folic acid: 5-fluorouracil, pyrimethamine, trimetroprim/sulfamethoxazole (Biseptol), pentamidine and diphenine. Metformin and cholestyramine have a negative effect on the absorption of folic acid. Therefore, patients taking such medications should take additional folic acid.
It is not advisable to determine the level of folic acid in blood serum, since this indicator increases sharply with food intake and therefore such a test is not economically justified.
If folic acid deficiency is suspected, its level in red blood cells should be determined, since this indicator more accurately correlates with the level of folic acid reserves in the body.
During the differential diagnosis of the etiology of megaloblastic anemia, it must be taken into account that a normal level of methylmalonic acid indicates folic acid deficiency, especially if the level of vitamin B12 is within the normal range.
It should be remembered that with a deficiency of vitamin B 12 and folic acid, homocysteine levels will be increased.
Effect of drugs to treat HIV
Macrocytosis occurs during HIV treatment with reverse transcriptase inhibitors (eg, stavudine [ZERIT], lamivudine [Epivir], zidovudine [Retrovir]) because these drugs affect DNA synthesis, which can lead to megaloblastic changes. The majority of patients receiving drugs in this group have macrocytosis without anemia. This indicates patient compliance and does not require treatment.
Medicines that can cause macrocytosis:
- Treatment of HIV infection: reverse transcriptase inhibitors (eg, stavudine [ZERIT], lamivudine [Epivir], zidovudine [Retrovir])
- Anticonvulsants (eg valproic acid, diphenine)
- Folic acid antagonists (eg methotrexate)
- Chemotherapy medications (eg, alkylating agents, pyrimidine, purine inhibitors)
- Trimetroprim/sulfamethoxazole (Biseptol)
- Biguanides (eg metformin, cholestyramine)
Reticulocytosis (hemolysis or bleeding)
Reticulocytosis can be explained by the mention of bleeding (chronic or acute) in the patient's history. When collecting a family history, attention should be paid to the presence of relevant hematological syndromes, including sickle cell anemia, congenital spherocytosis and glucose-6-phosphate dehydrogenase deficiency.
Macrocytosis occurs infrequently in long-distance runners as a result of chronic trauma to the feet.
During physical examination, hepatosplenomegaly or other signs of bleeding (eg, pallor of the conjunctiva or mucous membranes) are present in hemolysis. A peripheral blood smear may show signs of red blood cell hemolysis.
Macrocytosis occurs due to the bone marrow's response to increased cell destruction or bleeding, resulting in the release of reticulocytes into the bloodstream.
Alcoholism
The most sensitive tests for diagnosing alcoholism in patients with macrocytosis are the Michigan Alcoholism Screening Test and the determination of γ-glutamate transferase levels.
During the physical examination of alcoholism, signs such as gynecomastia, caput medusae (jellyfish head) and jaundice are indicated. Alcohol is more likely to cause macrocytosis due to direct toxic effects than folic acid deficiency.
In chronic alcohol abuse, the average red blood cell volume is usually less than 110 fL. When you abstain from drinking alcohol, the average volume of red blood cells increases rapidly.
Bone marrow dysfunction
Myeloproliferative diseases (sometimes called refractory anemia) are much more common among older people than among younger people. Although the diagnosis may be suspected based on a peripheral blood smear, a bone marrow biopsy is necessary to confirm it.
Other etiology
The effects of medications, hypothyroidism, liver and kidney diseases, and COPD cause a less pronounced increase in the average volume of red blood cells. A significant percentage of macrocytosis is due to liver disease and hypothyroidism. Therefore, during the history taking and physical examination, these diseases must be excluded. Macrocytosis also occurs after splenectomy.
Down syndrome may be accompanied by reticulocytosis or myeloproliferative diseases. Treatment, if indicated, consists of correcting the primary pathology.
Source: https://www.eskulap.top/terapija/chto-jeto-takoe-makrocitoz-krovi-v-obshhem-analize/
Reasons for violation
There are three main stages of microcytosis. At the first stage, only 40% of red blood cells are isolated in a general blood test, whose sizes are smaller than normal. At the second stage, there are 50-60% of pathological cells. In this case, the person feels weakness, headache, and fatigue.
The most severe stage of microcytosis is the third. At the same time, microcytes account for more than 70%. A patient with a similar diagnosis must be hospitalized and undergo additional examinations in a hospital setting. Otherwise, nausea, vomiting, or even loss of consciousness may occur. The following causes of blood microcytosis are distinguished:
- weakened immunity due to colds and viral diseases;
- problems with the thyroid gland;
- liver dysfunction;
- lack of vitamins A, B12 in the body;
- anemia;
- iron deficiency;
- oncological pathologies;
- congenital blood abnormalities;
- genetic pathologies;
- seasonal and daily fluctuations in the functioning of the circulatory system;
- nervous fatigue;
- severe stress, etc.
Expert opinion
Kovaleva Elena Anatolyevna
Doctor-Laboratory Assistant. 14 years of experience in clinical diagnostic services.
Ask a question to an expert
The above factors are the main ones. However, in addition to this, the doctor can identify other diseases that cause a similar change in the chemical composition of the blood .
Microcytosis will not cause harm to health if the cause of its development is eliminated in time.
To do this, the patient must undergo all examinations prescribed by the doctor. In addition, if a course of treatment , it must be completed without fail. If no measures are taken for a long time, microcytosis will lead to the development of other, more serious pathologies.
Macrocytosis: symptoms, causes, treatment and prevention
Macrocytes in a blood smear
Macrocytes are abnormally large cellular components of blood. The presence of such elements in the bloodstream is called macrocytosis.
This condition is a consequence of a disruption in the process of hematopoiesis at the stage of cell generation.
Incorrectly formed red blood cells are not able to perform their functions properly, that is, they cannot deliver hemoglobin through the capillaries, participate in the creation of immunity and metabolic processes.
In infants, macrocytosis is normal. And for pregnant women, it is a frequent companion throughout the entire period of bearing a baby, which is associated with the restructuring of processes in the bloodstream. Correcting nutrition and taking vitamins helps pregnant women cope with this disorder. For other groups of the population, this is a dangerous symptom.
In most cases, an unnatural increase in blood cells is accompanied by anemia - a low level of hemoglobin in the bloodstream. Anemia is a common symptom that reflects a number of diseases and is characterized by a lack of oxygen in the tissues of the body. An in-depth study of the causes and extent of macrocytosis allows us to determine the type of anemia and its treatment regimen.
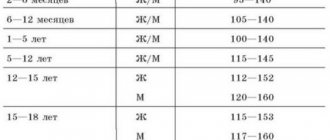
Macrocytosis in a blood test. Deviations in macrocytosis
Determining red blood cell parameters is an important diagnostic step
Comprehensive laboratory diagnostics allows you to determine the size of blood cells and their characteristics with high accuracy. To identify macrocytosis and the degree of its development, the following indicators are used.
- MCV—mean erythrocyte volume. It is measured in both femtoliters (fl) and micrometers (µm).
- RDW—red blood cell distribution width.
- MCH is the average hemoglobin content in a red blood cell.
- MCHC is the average concentration of hemoglobin in an erythrocyte.
- HGB is the hemoglobin content in the bloodstream.
- NBT is the ratio of red blood cells to its total volume.
Standard indicators of red blood cells:
- MCV = 6.2 - 8.2 µm;
- MCV = 80 – 94 fl;
- RDW = 11.5 - 14.5%;
- MCH = 27 - 35 pg;
- MCHC = 310 - 360 g/l;
- HGB = 120 - 140 g/l for women, 130 - 160 g/l for men;
- NCT = 0.36 - 0.46 l/l for women, 0.41 - 0.52 for men.
Based on the degree of deviation of the data obtained in the analysis, the stage of development of macrocytosis is determined. An additional study may include taking a bone marrow sample, which will help determine the cause of the pathology.
Symptoms of macrocytosis
Visual impairment is a possible sign of macrocytosis
At an early stage, symptoms may not appear. Changes in the size of blood cells are often discovered by chance during a routine blood test. Later stages are characterized by the following symptoms:
- fatigue, weakness;
- sudden weight loss;
- varnish tongue (with a smooth, shiny surface);
- pallor or yellowness of the skin;
- fainting;
- dyspnea;
- cardiopalmus;
- tingling in the limbs;
- brittleness of hair and nails;
- flashing “flies” before the eyes;
- dizziness.
All these symptoms are characteristic of the state of anemia, and each symptom separately helps to determine what exactly the body lacks at the moment to restore oxygen metabolism. Brittle nails and hair indicate a lack of iron, a varnished tongue indicates a lack of vitamin B 12.
Symptoms of macrocytosis appear cyclically, that is, the patient notices them periodically, and not constantly. This often leads to the fact that a person simply gets used to it and does not pay attention to changes in his body. Meanwhile, any of these symptoms is a reason to consult a doctor.
Causes of macrocytosis
Pathology of the thyroid gland can cause macrocytosis
A detailed examination of the body allows us to determine the cause of the pathology.
The main reasons are:
- Lack of cyanocobalamin (vitamin B 12),
- lack of folic acid (vitamin B 9),
- dysfunction of the thyroid gland,
- hepatitis,
- intestinal diseases,
- damage to liver tissue,
- bone marrow pathologies,
- spleen diseases,
- some forms of leukemia,
- use of medications (Chloridine, Allopurinol).
Macrocytosis can also be caused by congenital anomalies. But often it is poor nutrition or alcohol abuse that becomes hostage to disorders.
Treatment of macrocytosis
The cause of macrocytosis must be identified
Abnormally large blood cells are an indicator of the presence of the disease. Therefore, it is necessary to treat the root cause, and not the consequence of the development of the disease.
The basis for restoring natural processes in the bloodstream is good nutrition, as well as giving up alcohol and smoking.
A diet poor in vitamins provokes disturbances in blood formation, and alcohol-containing drinks lead to impaired liver function. Cigarettes contain poisons that contribute to intoxication of the entire body.
Additionally, depending on the disease, the following may be prescribed:
- course of vitamins,
- immunoglobulins,
- iron-containing preparations,
- blood transfusion,
- therapy with glucocorticoid drugs.
Severe forms of disease require mandatory hospitalization of the patient.
Prognosis and possible complications
Macrocytosis in childhood is also unsafe
Macrocytosis is a dangerous sign of a number of diseases characterized by a lack of oxygen in the body.
Immune suppression is one of the first consequences of this disorder, which leads to frequent infectious diseases and their complications.
In order to speed up the delivery of hemoglobin to the organs, the heart muscle begins to contract more often. The result is heart failure and tissue wear.
One of the common complications is a disorder of the central nervous system, which is manifested by impaired concentration and memory.
Lack of oxygen also leads to deformation of the structures of the mucous membranes and skin.
In childhood, the impact is on mental and physical development.
A condition in which tissues are not fully saturated with oxygen over a long period gradually leads to their degeneration. Severe forms of the disease lead to heart attacks, cardiogenic shock, and acute renal failure.
Timely treatment and dietary correction allow you to restore the natural circulation of red blood cells. However, in the future you should regularly monitor your health and undergo examinations.
Prevention
A balanced diet is a good way to prevent macrocytosis
Preventive measures are aimed at optimizing nutrition and giving up bad habits.
- Food must contain a sufficient amount of vitamins.
However, you should not prescribe vitamin therapy yourself. An excess of vitamins and their incorrect combination lead to negative consequences, including macrocytosis. - Smoking, in addition to intoxicating the body, poses a risk of developing macrocytosis due to the fact that cigarette smoke contains carbon monoxide.
This component instantly combines with hemoglobin. As a result, hemoglobin molecules are no longer able to deliver oxygen to the tissues. - Alcohol interferes with the absorption of microelements, including iron and vitamins, and also destroys hemoglobin molecules.
Alcohol has a particularly negative effect on the liver, which leads to the accumulation of toxic substances in it and subsequent disruption of the kidneys, heart and brain. - Active pastime in the fresh air will bring great benefits. This is the most effective way to saturate the body with oxygen.
Macrocytosis is not uncommon and is treatable in most cases. A healthy lifestyle and nutritious nutrition is a chance to forever get rid of the risk of a recurrence of pathology.
Source: https://gidanaliz.ru/analiz/oak/makrocitoz-v-analize-krovi.html
Microcytosis in a child
In childhood, deviations from the norm in the results of a general blood test are possible. This does not necessarily indicate a deviation. Microcytosis of the first degree is not dangerous. However, if the pediatrician insists on additional examination, then all diagnostic procedures must be completed. Microcytosis of the second and third degrees is already a serious disorder.
In childhood, such indicators may be a sign of leukemia . As medical practice shows, if the number of microcytes in a child exceeds 70%, then urgent hospitalization is necessary. In the hospital, the baby will be given an accurate diagnosis, referred to the necessary specialists and prescribed competent and effective treatment. However, in most cases, children exhibit microcytosis at the initial stage , which indicates a malfunction of the immune system. In this case, it is enough to normalize your diet and daily routine. And the red blood cells will return to normal on their own.
How does hypochromic anemia develop?
The participation of iron in the development of hypochromic anemia is expressed in different ways:
- lack of iron intake from food;
- violation of hemoglobin synthesis (combination of protein with heme);
- instability of the resulting molecule, loss of the ability to retain oxygen.
Accordingly, in the clinical course of chronic and acute anemia the following conditions are distinguished:
- with quantitatively confirmed low iron levels;
- with poor saturation of red blood cells, when there is enough iron in the body;
- when there is more iron than necessary, the excess is formed from the massive breakdown of red blood cells, but the body cannot redistribute it and hemoglobin is not synthesized;
- mixed form.
Deviation in pregnant women
When carrying a child, a woman is required to detect deviations from the norm in a general blood test. Sometimes the level of white blood cells increases, sometimes the shape of platelets changes, but most often microcytes are found in the blood. If their number does not exceed 40%, then there is no reason to worry . However, if there are too many microcytes (more than 40%), there is cause for alarm. This may signal fetal rejection, incompatibility of biological materials between mother and child, or severe stress on the body.
In such a situation, the gynecologist performs a number of additional procedures to find out the cause of this disorder. Depending on the diagnosis and individual characteristics of the patient, a course of treatment is prescribed, and then relapse is prevented.
How it manifests itself
People with elevated levels of microcytes in the blood do not have specific symptoms. When feeling unwell, weak and decreased in performance, not everyone even goes to the doctor. But the severity of microcytosis depends not on its degree, but on its duration.
Attention: without timely treatment, symptoms will only get worse. Changes in blood composition greatly affect a person’s health.
Oxygen starvation and impaired blood composition are manifested by the following external signs:
- weakness, drowsiness;
- disturbance of taste sensations;
- dry mouth, seizure formation;
- atrophy of the papillae of the tongue, tingling, change in its color;
- frequent nausea, urge to vomit;
- sensation of a lump in the throat, difficulty swallowing;
- pale and dry skin;
- dry and brittle hair and nails;
- shortness of breath, tachycardia;
- itching of the external genitalia.