The minute volume of blood, like the systolic volume, can be different for each person; this value is not constant and can change depending on the state of the body and its activity.
These parameters are the main indicators characterizing the contractile functions of the myocardium. Minute blood volume is abbreviated as MOC and is one of the most important parameters for determining the amount of this fluid that is ejected by the heart ventricle within 1 minute. Using this parameter, you can diagnose various heart diseases.
Since the human heart has two ventricles, despite the fact that their pumping levels are approximately the same, studies are carried out by calculating the total amount of blood, and not separately from each ventricle within a minute. The result obtained has a physical value of liters per minute.
In order to remove anthropometric differences and their influence on IOC, it is expressed as a cardiac index. IOC is a cardiac index, which is the value of the volume of blood flow passing per minute divided by the total body area. The physical dimension of such an index is expressed in liters per square meter per minute. General designations for the parameters of normal blood circulation were also adopted.
If measurements are taken from a young person who is healthy, calm and in a supine position, then the normal IOC will be in the range of 4.5-6 l per minute, the cardiac index values will fluctuate within 2-4 l/sq.m*min.
In total, the body of an adult human contains approximately 5 liters of blood, that is, in a healthy state, the body distills all the blood in just a minute.
To provide sufficient nutrition and improve gas exchange in tissues during hard work or active training, the IOC can increase to 30 l/min.
Since transporting oxygen throughout the body is one of the main functions performed by blood cells, studying the IOC at maximum voltage is also an important procedure. It shows what functional reserve the heart has, based on its hemodynamic functions.
If a person is healthy, then his hemodynamic reserve of the heart will be in the region of 300-400%. But this is not the limit: if a person plays sports for a long time or leads an active lifestyle, this parameter can be 6 times higher than resting IOC, that is, 600%.
Systolic indicator
Systolic blood volume is a parameter that directly depends on cardiac output; to calculate it, you will need to divide the IOC value by the sum of heartbeats for the same minute. This value shows how much blood is pumped into each ventricle and released into the great vessel, which is often the pulmonary artery. That is, this is the stroke volume of blood that is ejected by the heart in one contraction.
Systolic volume is very dependent on heart rate. The greatest amount of release is observed at 130-170 heartbeats per minute. If this parameter becomes larger, then the required amount of blood simply does not have time to collect in the ventricles, and the systolic indicator drops significantly.
In the same person who is at rest, the heart contracts approximately 75 times per minute, and the systolic volume is 70-90 ml, which are approximate indicators of normal functioning of the cardiovascular system.
If the body is completely calm, then all the blood does not leave the ventricle; at the end of systole, a reserve amount remains in it, which the body may require in the event of a sudden change in condition, for example, severe fright, stress, or the start of training.
The residual reserve can reach 50% of the total volume accumulated in the ventricles. How much can be stored as a reserve is also a very important parameter of the heart. So, if the formed reserve increases, then the maximum systolic volume increases, which the body can quickly begin to throw out if necessary.
Adaptation of the entire circulatory apparatus associated with changes in systolic volume occurs due to various self-regulation mechanisms caused by the influence of extracardiac nerve mechanisms. Regulation occurs due to changes in the force of myocardial contraction. As contraction force decreases, systolic volume also decreases.
Stroke volume in heart failure
The heart muscle contracts up to 4 billion times throughout a person’s life, providing up to 200 million liters of blood into tissues and organs. The so-called cardiac output under physiological conditions ranges from 3.2 to 30 l/minute. Blood flow in organs changes, doubling, depending on the strength of their functioning, which is determined and characterized by several hemodynamic indicators.
Stroke (systolic) blood volume (SV) is the amount of biological fluid that the heart ejects in one contraction. This indicator is interconnected with a number of others. These include minute blood volume (MBV) - the amount ejected by one ventricle in 1 minute, as well as the number of heart contractions (HR) - this is the sum of heart compressions per unit of time.
The formula for calculating the IOC is as follows:
IOC = SV * HR
For example, SV is 60 ml, and heart rate in 1 minute is 70, then IOC is 60 * 70 = 4200 ml.
To determine the stroke volume of the heart, you need to divide the IOC by the heart rate.
Other hemodynamic parameters include end-diastolic and systolic volume. In the first case (ECD) is the amount of blood filling the ventricle at the end of diastole (depending on gender and age - in the range from 90 to 150 ml).
End systolic volume (ESV) is the amount remaining after systole. At rest, it is less than 50% of diastolic, approximately 55-65 ml.
Ejection fraction (EF) is a measure of how efficiently the heart pumps with each beat. The percentage of blood volume that enters the aorta from the ventricle during contraction. In a healthy person, this figure is normal and at rest is 55-75%, and during physical activity reaches 80%.
The minute volume of blood without tension is 4.5-5 liters. When moving to intense physical exercise, the rate increases to 15 l/minute or more. Thus, the cardiac system satisfies the needs of tissues and organs for nutrients and oxygen to maintain metabolism.
Hemodynamic blood parameters depend on training. The value of a person's systolic and cardiac output increases over time with a slight increase in the number of heartbeats. In untrained people, heart rate increases and systolic output remains almost unchanged. An increase in SV depends on an increase in blood flow to the heart, after which the SV also changes.
The amount of blood ejected by the ventricle of the heart into the arteries per minute is an important indicator of the functional state of the cardiovascular system (CVS) and is called minute volume
blood (IOC). It is the same for both ventricles and at rest is 4.5–5 liters.
Stroke volume provides an important characteristic of the pumping function of the heart.
, also called
systolic volume
or
systolic ejection
.
Stroke volume is the amount of blood ejected by the ventricle of the heart into the arterial system in one systole. (If you divide the IOC by the heart rate per minute, we get the systolic
volume (SV) of blood flow.) With a heart contraction of 75 beats per minute, it is 65–70 ml; during work it increases to 125 ml. In athletes at rest it is 100 ml, during work it increases to 180 ml. The determination of MOC and CO is widely used in the clinic.
Ejection fraction (EF)
– expressed as a percentage, the ratio of the stroke volume of the heart to the end-diastolic volume of the ventricle. EF at rest in a healthy person is 50-75%, and during physical activity it can reach 80%.
The volume of blood in the ventricular cavity that it occupies before its systole is end-diastolic
volume (120–130 ml).
End-systolic volume
(ECO) is the amount of blood remaining in the ventricle immediately after systole.
At rest, it is less than 50% of the EDV, or 50-60 ml. Part of this blood volume is reserve volume.
The reserve volume is realized when CO increases under load. Normally, it is 15–20% of the end-diastolic value.
The volume of blood in the cavities of the heart remaining when the reserve volume is fully realized at maximum systole is the residual
volume. CO and IOC values are not constant. During muscular activity, IOC increases to 30–38 l due to increased heart rate and increased CO2.
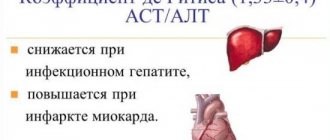
A number of indicators are used to assess the contractility of the heart muscle. These include: ejection fraction, rate of blood expulsion during the rapid filling phase, rate of increase in pressure in the ventricle during the period of stress (measured by probing the ventricle)/
Blood expulsion rate
changes using Doppler ultrasound of the heart.
Pressure rise rate
in the cavities of the ventricles is considered one of the most reliable indicators of myocardial contractility. For the left ventricle, the normal value of this indicator is 2000-2500 mmHg/s.
A decrease in the ejection fraction below 50%, a decrease in the rate of blood expulsion, and the rate of pressure increase indicate a decrease in myocardial contractility and the possibility of developing insufficiency of the pumping function of the heart.
The value of the IOC divided by the body surface area in m 2 is determined as the cardiac index
(l/min/m2).
SI = MOK/S (l/min×m 2)
It is an indicator of the pumping function of the heart. Normally, the cardiac index is 3–4 l/min×m2.
IOC, SV and CI are united by the common concept of cardiac output.
If the IOC and blood pressure in the aorta (or pulmonary artery) are known, the external work of the heart can be determined
P is the work of the heart in minutes in kilograms (kg/m).
MOC—minute blood volume (l).
Blood pressure is pressure in meters of water column.
At physical rest, the external work of the heart is 70–110 J; during work it increases to 800 J, for each ventricle separately.
Thus, the work of the heart is determined by 2 factors:
1. The amount of blood flowing to it.
2. Vascular resistance during the expulsion of blood into the arteries (aorta and pulmonary artery). When the heart cannot pump all the blood into the arteries at a given vascular resistance, heart failure occurs.
There are 3 types of heart failure:
1. Insufficiency from overload, when excessive demands are placed on the heart with normal contractility due to defects, hypertension.
2. Heart failure due to myocardial damage: infections, intoxications, vitamin deficiencies, impaired coronary circulation. At the same time, the contractile function of the heart decreases.
3. Mixed form of failure - with rheumatism, dystrophic changes in the myocardium, etc.
The entire complex of manifestations of cardiac activity is recorded using various physiological techniques - cardiography:
ECG, electrokymography, ballistocardiography, dynamocardiography, apical cardiography, ultrasound cardiography, etc.
The diagnostic method for the clinic is the electrical recording of the movement of the contour of the heart shadow on the screen of the X-ray machine. A photocell connected to an oscilloscope is applied to the screen at the edges of the heart contour. As the heart moves, the illumination of the photocell changes. This is recorded by an oscilloscope in the form of a curve of contraction and relaxation of the heart. This technique is called electrokymography.
.
Apical cardiogram
recorded by any system that detects small local movements. The sensor is fixed in the 5th intercostal space above the site of the cardiac impulse. Characterizes all phases of the cardiac cycle. But it is not always possible to register all phases: the cardiac impulse is projected differently, and part of the force is applied to the ribs. The recording may differ from person to person and from one person to another, depending on the degree of development of the fat layer, etc.
The clinic also uses research methods based on the use of ultrasound - ultrasound cardiography.
Ultrasonic vibrations at a frequency of 500 kHz and higher penetrate deeply through tissues being generated by ultrasound emitters applied to the surface of the chest. Ultrasound is reflected from tissues of various densities - from the outer and inner surface of the heart, from blood vessels, from valves. The time it takes for the reflected ultrasound to reach the capturing device is determined.
If the reflective surface moves, the return time of the ultrasonic vibrations changes. This method can be used to record changes in the configuration of heart structures during its activity in the form of curves recorded from the screen of a cathode ray tube. These techniques are called non-invasive.
Invasive techniques include:
Catheterization of the heart cavities
. An elastic catheter probe is inserted into the central end of the opened brachial vein and pushed towards the heart (into its right half). A probe is inserted into the aorta or left ventricle through the brachial artery.
Ultrasound scanning
- the ultrasound source is inserted into the heart using a catheter.
Angiography
is a study of heart movements in a field of X-rays, etc.
Mechanical and sound manifestations of cardiac activity. Heart sounds, their genesis. Polycardiography. Comparison in time of periods and phases of the cardiac cycle of ECG and FCG and mechanical manifestations of cardiac activity.
Heart beat.
During diastole, the heart takes the shape of an ellipsoid.
During systole, it takes on the shape of a ball, its longitudinal diameter decreases, and its transverse diameter increases. During systole, the apex rises and presses against the anterior chest wall. A cardiac impulse occurs in the 5th intercostal space, which can be recorded ( apical cardiography
).
The expulsion of blood from the ventricles and its movement through the vessels, due to reactive recoil, causes vibrations of the entire body. Recording these vibrations is called ballistocardiography
. The work of the heart is also accompanied by sound phenomena.
Heart sounds.
When listening to the heart, two sounds are detected: the first is systolic, the second is diastolic.
Systolic
the tone is low, drawn-out (0.12 s). Several overlapping components are involved in its genesis:
1. Mitral valve closure component.
2. Closure of the tricuspid valve.
3. Pulmonary tone of blood expulsion.
4. Aortic tone of blood expulsion.
The characteristic of the first tone is determined by the tension of the leaflet valves, the tension of the tendon threads, papillary muscles, and the walls of the ventricular myocardium.
Components of blood expulsion occur when the walls of the great vessels are tense. The first sound is clearly audible in the 5th left intercostal space. In pathology, the genesis of the first tone involves:
1. Aortic valve opening component.
2. Opening of the pulmonary valve.
3. Tone of pulmonary artery distension.
4. Aortic stretch tone.
Strengthening of the first tone can occur with:
1. Hyperdynamics: physical activity, emotions.
When there is a violation of the time relationship between the systole of the atria and ventricles.
With poor filling of the left ventricle (especially with mitral stenosis, when the valves do not open completely). The third option of amplifying the first tone has significant diagnostic value.
Weakening of the first sound is possible with mitral valve insufficiency, when the valves do not close tightly, with myocardial damage, etc.
In the first part of the article, I showed the work of the heart, blood vessels and the phases of the cardiac cycle. In the second part we will consider the stroke volume of the heart, the work of the heart at an increased heart rate.
With each contraction of the heart in an adult (at rest), 50-70 ml of blood is released into the aorta and pulmonary trunk, 4-5 liters per minute. With great physical stress, minute volume can reach 30–40 liters. In other words, the athlete’s heart stretches to such a size that it can pump more than 200 ml of blood in one contraction. For example, the heart of a professional track and field athlete works for a minute at a pulse of 180 beats/min. can pump 36 l. blood. This is the 4th bucket of 10 liters!
Each person’s SV is individual, depending on hereditary data and training. In women, for example, SV is 10-15% less than in men.
A person with an athletic heart (having a larger stroke volume) has a higher level of endurance, especially for prolonged physical activity (marathon, cycling, long-distance swimming).
What effect does physical activity have on the heart?
- Heart rate (HR) increases
- Stroke volume (SV) increases
- Systolic pressure increases
- Diastolic pressure and peripheral vascular resistance decrease
- Respiration rate increases
- Coronary blood flow increases
- Blood redistribution occurs (blood will be in the working muscle)
Effect of aerobic exercise (long-term)
- Athletic heart (increased size and strength of contraction)
- Decreased heart rate
- Increased number of capillaries in muscles
Stroke volume during physical activity.
Surely some have noticed, you run and run for 20-30 minutes, the pulse is high, and then from 150-155 beats/min. it drops to 135 bpm. at the same intensity. This is an indicator that the heart has returned to its normal volume, the blood vessels and capillaries of the body have started working.
With prolonged physical activity of 40-60% of the maximum (or 120-150 beats/min when running), the chamber of the left/right ventricle is stretched, since the maximum amount of blood enters in this mode. If the ventricular chamber is stretched (diastole phase), then, accordingly, it must further contract as much as possible (systole phase) in order to push out blood.
Heart function at elevated heart rate.
When the load increases, when working in the 4-5th pulse zone (PZ), the heartbeat increases, and so does the pulse. The systole and diastole (contraction and relaxation) phases become more frequent. Why can't we run at a heart rate of 170 -180 beats/min for as long as we can at a heart rate of 150 beats/min? The point is this...
SV with an increased heart rate will decrease, oxygen exchange between muscle tissues (upper/lower limbs) will be disrupted, which will limit the performance of work.
Accordingly, in this mode (anaerobic glycolysis), the athlete will not be able to show high results for a long time. With a decrease in nutrients and oxygen supplied to the muscles, as we know, the body begins to use glucose in anaerobic mode, muscle glycogen, releasing pyruvate, lactate, which enters the blood. Together with lactate, the amount of hydrogen ions (H+) increases. And then excess H+ destroys protein and myofibrils. In small quantities it helps to increase strength, but in excess, with strong acidification, it only harms the body. If there is a lot of H+ and they remain in the blood for a long time, then this also reduces the athlete’s aerobic capabilities and endurance, as it destroys mitochondria.
But the good news is that with the help of competent interval training and tempo training, we can increase the body’s buffering capabilities, increasing VO2 max and pushing back the threshold.
Interval training, especially among professional athletes and even amateurs who work for results, is associated with large intervals of 1000 m and above, and these workouts are very exhausting not only for the physical condition, but also for the nervous system. If you do them often, it can lead to overtraining, inflammation, illness, and injury. In my opinion, depending on the athlete’s training period and the athlete’s level, 1-2 varied interval training sessions per week or even once every 2 weeks are sufficient.
The faster the heart rate, the more the biochemistry shifts towards anaerobic metabolism, the less time we can do this or that work. The higher the heart rate, the more oxygen and energy the muscles need to consume. As a result, the heart muscle will not receive enough nutrition, which will lead to ischemia (impaired cardiac circulation) of the heart.
In order to increase endurance, it is not enough just to increase the stroke volume of the heart (SV). The condition of the muscles, capillarization and development of the circulatory system also matter here. These qualities develop during training.
Interval training is also different: short intense and long (not at full strength). The first can last 10-20 minutes, and the second 40-60 minutes or more. The more intense the interval, the higher the heart rate (pulse), the more the heart muscle is pumped, and the elasticity decreases.
You need to understand that interval training at maximum heart rate is acceptable if you are a professional athlete and are preparing for competitions. Prolonged exercise in this mode is undesirable for health, as it leads to acidification of not only the muscles, but also the heart.
Exercising with too high a heart rate leads to hypertrophy of the heart muscle and a decrease in stroke volume, and as a result can lead to heart failure and even death. Therefore, competently drawing up a training plan and understanding the specifics of training exercises allows you to consistently and evenly develop body functions without harm to health.
What is the threat to an athlete’s health when running for a long time at a high heart rate or how does the body protect us from sad consequences?
1) First, the body becomes fatigued, then the working muscles (arms, legs) become clogged and become weak.
2) Gag reflex, nausea, as a reaction to acidification of the body.
3) Disabling the central nervous system, loss of consciousness.
4) Cardiac arrest.
You and I are smart now and we won’t bring ourselves to the point of point 4.
Heart failure in old age
In old age, if a person has moved little throughout his life, the walls of his heart become thinner, and the systolic volume does not exceed 20 ml. This is very little. The heart is not used to completely emptying the chambers, it weakens.
As a result, older people develop heart failure. When the valves are damaged, the heart cannot work at full strength, and then cardio training is dangerous.
It is necessary to lead a healthy lifestyle and walk outdoors more often. Hypokinesia (immobility) contributes to aging of the body, loss of strength and heart failure.
But the situation will be different if a person tries not to be lazy and goes to the gym. Training triggers a certain mechanism - an increase in negative pressure in the chest. This results in increased venous return to the heart.
Systolic volume and minute volume of blood. Effect of training
To characterize the hemodynamics of the heart, indicators such as heart rate (HR), stroke and minute blood volumes, ejection fraction and others are used. Let us consider separately such an indicator as systolic volume (SV) and how it affects other functions of the body.
For people involved in sports, it is extremely important to monitor the hemodynamics of their heart. What is CO? Systole is the contraction phase of the heart, and diastole is the relaxation phase of the chambers.