Aggregation or gluing of red blood cells: what is it, treatment
Red blood cell aggregation is the process of connecting blood cells into one system. As a result of this phenomenon, specific columns of different sizes and densities are formed in the blood. The process can be observed through a microscope if you examine a fresh drop of blood. Over time, the density of the columns increases, and the density of individual cells decreases, and the boundaries begin to blur.
Process Basis
Agglutination or aggregation is the process of blood cells sticking to each other. After some time, the compounds precipitate into a homogeneous precipitate. The entire process is directly influenced by antibodies, which help the body fight negative factors. It is these antibodies that are the factor that encourages the body to stick together red blood cells.
Antibodies that trigger a process called aggregation appear in a person’s blood when pathogenic microflora enters the body and a disease begins to develop.
Children do not have such cells if the child is completely healthy. If antibodies are detected in the blood, the specialist must prescribe special treatment, since this condition is considered a deviation from the norm.
An adult may have agglutinins, even if the body is completely healthy. This phenomenon does not require special treatment or observation by specialists.
The presence of antibodies in the body of an adult is an indicator that the immune system has already fought such a disease and has remembered it.
The presence of antibodies to many diseases is an indicator that a person cannot become infected again. In addition, antibodies can form after taking certain medications.
Agglutinins found in the human body without pathologies do not require any therapeutic intervention and are a normal indicator.
Laboratory testing for the presence of such antibodies is carried out in the following cases:
- To detect antibodies to a specific disease.
- If necessary, determine the causative agent of the disease.
- In case of determining the patient's blood type.
Red blood cell aggregation is an important indicator that can tell a lot about the condition of the patient’s body. The gluing of red blood cells is a process that does not require treatment or special medical supervision. Only in children, the presence of some agglutinins is not considered normal and requires therapeutic measures.
If red blood cells in the body begin to actively stick together, then this condition may indicate the development of the following pathological processes:
- shock from the injury;
- condition after a heart attack;
- peritonitis;
- severe burns;
- acute form of pancreatitis;
- intestinal obstruction.
Adhesion can occur at the epicenter of injury or throughout the entire bloodstream. It all depends on the form and type of disease.
If the red blood cells are strongly glued together, then this condition can lead to serious consequences, including:
- disruption of blood circulation;
- metabolic disorder;
- dysfunction of internal organs.
To normalize the condition, treatment is required, since in such a case there is an increase in blood acidity, which in turn leads to hypoxia.
If red blood cells clump together, this condition can cause blood flow to slow down or stop in the capillaries. This condition is dangerous to human life and health.
So, the aggregation process can be triggered by diseases that are actively developing in the patient’s body. This condition is dangerous to health and requires immediate treatment, which will protect the person from serious consequences and death.
Diagnosis and treatment
The process of red blood cell clumping is detected during laboratory testing, which is carried out for the purpose of prevention or detection of diseases. Modern methods make it possible to identify this process by hemoscanning or by studying a drop of blood.
The first research option is the most common, since studying a drop of blood requires the most modern laboratory equipment and the presence of a specialist.
With the help of laboratory blood tests, dangerous diseases can be detected in a timely manner and treatment can be started in the early stages. If deviations from the norm were found during the study, then this condition requires treatment.
As therapy, a specialist may prescribe drugs that:
- Improves blood properties.
- Promote the bending of blood cells.
- Improves the penetration of blood cells through capillaries.
- Makes the blood less thick.
As a preventive measure, it is necessary to regularly donate blood for this indicator in order to identify deviations in time. It is especially important to get tested for people over 50 years of age.
In addition, you must:
- Avoid stress.
- To live an active lifestyle.
- Don't forget about proper nutrition.
- Do not take medications without a doctor's prescription.
If you follow all preventive measures, you can maintain your health. Be sure to donate blood for preventive purposes.
What is agglutination?
The term "Agglutination" is translated from the Latin "agglutinatio" meaning "sticking". In biological systems or laboratory analysis, this is the gluing and aggregation of organic particles (bacteria, sperm, blood cells) having agglutinogen antigens on their surface when interacting with specific agglutinin antibodies. The resulting agglomerate is called agglutinate.
Even normally, antibodies and antigens may be present in human blood that do not cause adhesion. These are components of the ABO antigen system, which correspond to the blood group, antibodies that appear as an immune response when certain bacteria or other pathogens of infectious diseases (dysentery, typhoid fever) enter the body.
Red blood cell agglutination
The agglutination reaction mechanism can be direct (active) or indirect (passive). The effect of direct agglutination occurs in an organism or sample when the structural membrane antigens of red blood cells begin to interact with the plasma's own antibodies or components of bacterial cells.
Direct agglutination is used in clinical studies, determining blood type or the presence of the Rh factor. The effect of passive adhesion is widely used to make a diagnosis of infectious diseases (bacterial, viral).
What is red blood cell aggregation and how is it treated. The process of red blood cell gluing is called
Agglutination or aggregation is the process of blood cells sticking to each other. After some time, the compounds precipitate into a homogeneous precipitate. The entire process is directly influenced by antibodies, which help the body fight negative factors. It is these antibodies that are the factor that encourages the body to stick together red blood cells.
Antibodies that trigger a process called aggregation appear in a person’s blood when pathogenic microflora enters the body and a disease begins to develop.
Children do not have such cells if the child is completely healthy. If antibodies are detected in the blood, the specialist must prescribe special treatment, since this condition is considered a deviation from the norm.
An adult may have agglutinins, even if the body is completely healthy. This phenomenon does not require special treatment or observation by specialists.
The presence of antibodies in the body of an adult is an indicator that the immune system has already fought such a disease and has remembered it.
The presence of antibodies to many diseases is an indicator that a person cannot become infected again. In addition, antibodies can form after taking certain medications.
Agglutinins found in the human body without pathologies do not require any therapeutic intervention and are a normal indicator.
Laboratory testing for the presence of such antibodies is carried out in the following cases:
- To detect antibodies to a specific disease.
- If necessary, determine the causative agent of the disease.
- In case of determining the patient's blood type.
Red blood cell aggregation is an important indicator that can tell a lot about the condition of the patient’s body. The gluing of red blood cells is a process that does not require treatment or special medical supervision. Only in children, the presence of some agglutinins is not considered normal and requires therapeutic measures.
What can trigger this process?
If red blood cells in the body begin to actively stick together, then this condition may indicate the development of the following pathological processes:
- shock from the injury;
- condition after a heart attack;
- peritonitis;
- severe burns;
- acute form of pancreatitis;
- intestinal obstruction.
Adhesion can occur at the epicenter of injury or throughout the entire bloodstream. It all depends on the form and type of disease.
If the red blood cells are strongly glued together, then this condition can lead to serious consequences, including:
- disruption of blood circulation;
- metabolic disorder;
- dysfunction of internal organs.
To normalize the condition, treatment is required, since in such a case there is an increase in blood acidity, which in turn leads to hypoxia.
If red blood cells clump together, this condition can cause blood flow to slow down or stop in the capillaries. This condition is dangerous to human life and health.
So, the aggregation process can be triggered by diseases that are actively developing in the patient’s body. This condition is dangerous to health and requires immediate treatment, which will protect the person from serious consequences and death.
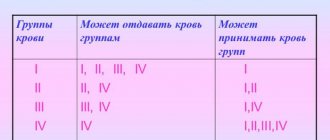
Cross reaction method results
After five minutes, the samples are ready for examination. The options are:
- gluing occurred in both drops – group 1;
- flakes are not observed in any of the samples – group 4;
- the process is visible in one sample - group 2 or 3 (depending on where exactly the blood clotted).
How does red blood cell aggregation occur?
The simplest aggregation of red blood cells can be seen under a conventional microscope, when there is a small drop of blood on a glass slide.
It gradually forms glued columns, “packs” of red blood cells, which are called coin columns. The density of these columns gradually increases, and then it is no longer visible that they are glued together from individual red blood cells.
They represent a solid conglomerate. This phenomenon is called homogenization in the laboratory.
Fortunately, this process is completely reversible, and in the body, erythrocyte sludge (this is the name given to similar structures) can disintegrate into individual cells.
The important clinical significance of red blood cell aggregation is that these clots of individual cells disrupt capillary blood flow because they impair the fluidity of the blood, or its rheological properties.
In large vessels, such as the aorta, subclavian artery, and large vessels of the liver, erythrocyte aggregation is invisible. But in small capillaries it can no longer be ignored.
This phenomenon can develop quickly and strongly throughout the entire body, which is observed in some diseases.
In the event that aggregation of red blood cells occurs due to some toxin, acute infection, for example, malaria, lobar pneumonia, or various shocks, then a serious obstacle to microcirculation occurs throughout the body. Blood flows very poorly from small arteries into the capillary system.
In addition, aggregation, if it occurs inside small capillaries, has a very bad effect on gas exchange in tissues. There is the science of pathophysiology, which studies typical pathophysiological processes that damage various structures of the body. From the point of view of this science, the limit of harm is the complete stop of capillary blood flow, or stasis.
As a result, severe metabolic and tissue acidosis occurs, or an increase in blood acidity occurs.
This condition requires treatment, but in this case it is not cardiac aspirin that is used, but specific therapy aimed at removing toxins from the human body, intensive therapy aimed at restoring capillary blood flow and microcirculatory function. The most common causes of red blood cell aggregation are:
- a hemodynamic factor that determines the behavior of red blood cells in the blood flow.
This factor is significantly influenced by the concentration of red blood cells. It is clear that if the patient is dehydrated, then the red blood cells are close to each other, and their aggregation will certainly occur;
- the second factor is plasma.
This factor determines the state of the blood plasma and the presence of various substances in it that help red blood cells approach or repel. Taking aspirin will be the plasma disaggregation factor. Its molecules, being in the blood plasma, prevent red blood cells from coming together and sticking together.
Finally, the third factor is electrostatic. This is nothing more than the ordinary forces of Coulomb attraction of unlike charges. This factor also helps the red blood cells clump together and become sticky.
What are the risks of cold agglutinin testing?
Possible risks of a blood test for cold antibodies can only be associated with the blood collection itself. In particular, the appearance of bruises at the puncture site and inflammation of the vein (phlebitis). Warm compresses several times a day will relieve phlebitis. If you are taking blood thinning medications, you may bleed at the puncture site.
What can interfere with cold agglutinin testing?
The cold agglutinin test result will be inaccurate if you are taking antibiotics, especially penicillin and cephalosporin.
Interpretation of test results
The test results are given in the form of a titer. Titer is the extent to which a blood sample can be diluted until cold agglutinins are detected. A titer of 1:80 means that cold agglutinins can be detected when one part of the sample is diluted with eight parts of saline.
Higher numbers indicate that there are more cold agglutinins in the blood. This means there may be infections such as mycoplasma pneumonia, malaria, infectious mononucleosis, or other viral conditions.
Liver cirrhosis, hepatitis C and autoimmune disease can also cause increased levels of cold agglutinins.
Cold agglutinin syndrome is a condition in which the body's red blood cells are prematurely destroyed and the production of new cells is unable to replace the losses.
Other conditions that may cause high cold agglutinins include scleroderma, hemolytic anemia, rheumatoid arthritis, or multiple myeloma. High titers greater than 1:1000 may indicate the presence of lymphoma.
Very high titre levels can cause an individual's body to develop a tendency to form blood clots when the body is exposed to cold temperatures.
Reasons for thick blood leading to increased blood viscosity:
- Human blood is more than 90% water. All fluids in the body have special properties, such as structure, weak alkalinity of 7.43 on the Ph scale, ORP (oxidation-reduction potential) within - 50 mV, low surface tension of 43 dynes/cm2 and sufficient mineralization in homeopathic doses. When we use: dirty;
- chlorinated;
- destructured;
- carbonated water with a high surface tension (for example, tap water has a surface tension coefficient of up to 73 dynes/cm2), the body is forced to spend a lot of cellular energy transforming the water just so that it can penetrate into the cell. Poor quality of water entering the body is the main cause of thick blood .
Why does red blood cell agglutination occur?
Agglutination of the erythrocyte mass becomes a consequence of the biochemical interaction of antigen molecules localized in the structure of the blood cell membrane with antibodies found in the plasma. This reduces the natural negative charge of red blood cells and brings them closer together. Agglutinin molecules that do not correspond to the blood type can form “bridges” between red blood cells. As a result, a blood clot forms, hemolytic disease develops, and even death.
The adhesion of red blood cells (hemagglutination reaction - HRA) is caused by various factors, which depend on the nature of the agglutinating agent on the surface of the formed element or in the plasma:
- Cold agglutinins. They can be detected in the blood during diseases caused by viruses and bacteria, some neoplasms and hypothermia, causing symptoms of intravascular hemolysis. Cold agglutinins can be found in low titers in healthy people without causing noticeable hemolytic manifestations. By chemical nature, these are usually immunoglobulin proteins (most often IgM). They are activated when the temperature drops below 37°C, for example, when blood enters the upper or lower extremities or other parts of the body prone to hypothermia. Cold agglutinins, depending on the type, can exhibit activity and be localized differently: act in a wide or narrow temperature range, when the temperature is restored, remain fixed on the surface of the erythrocyte or be in the plasma.
- Erythrocyte antigens. Today, more than 400 antigen systems have been identified, the combination of which is individual for a person. Most of them have weak antigenic properties and do not cause noticeable agglutination of red blood cells. The most critical systems for blood transfusion are the ABO and Rhesus systems, incompatibility of which can cause clumping of blood cells followed by transfusion shock.
- Hemagglutinogens that determine blood group. In the structure of erythrocyte membranes there are specific markers-antigens of a glycoprotein nature (agglutinogens A and B), and in the plasma there are specific immunoglobulin substances-antibodies (agglutinins alpha and beta). One of four possible combinations of these antigens and antibodies determines the blood type, which is genetically determined and cannot change throughout life. Agglutinogens and agglutinins of the same name cannot be present in the human body at the same time, otherwise red blood cells will stick together, followed by hemolysis. This is one of the genetically developed reactions of the body, aimed at preserving antigenic individuality and the basic principle of blood transfusion.
| Blood type | Agglutinogen | Agglutinin |
| 0 (I) | Absent | αβ |
| A (II) | A | α |
| B (III) | IN | β |
| AB (IV) | AB | absent |
- Antigens of the Rh system. Rh antigens (Rh) are lipoproteins by chemical nature. Antigens of the Rh system are represented by several types (C, E, D), the strongest of them is the D type. People who have such an antigen are called Rh-positive, the rest are called Rh-negative. Normal plasma does not contain antibodies to Rh antigens. They appear due to violation of the rules of blood transfusion and in case of Rh conflict during pregnancy.
- Viral and bacterial agglutination of erythrocytes. Aggregation of red blood cells in certain viral or bacterial diseases may occur due to direct interaction of the virus or bacteria with the surface structural molecules of red blood cells or due to a reaction with the titer of immunized serum of red blood cells specifically sensitized with the desired antigen (in vitro). Agglutination of blood cells occurs after the adsorption of the virus on the surface of the red blood cell. In most viruses, hemagglutinin is a structural component of the virion.
Specific markers - antigens of glycoprotein nature (agglutinogens A and B)
All the details about the process of red blood cell aggregation
Everyone knows that the human body consists entirely of cells and approximately a quarter of them are occupied by red blood cells. These cells are microscopic elastic particles, biconvex in shape . Their size does not exceed only 8-10 microns, which allows them to move freely through blood vessels. Below we will look at the process of red blood cell aggregation.
The main function of these cells is to transport oxygen to tissues from the lungs and transport carbon dioxide in the opposite direction . In clinical practice, this process is also called blood transport function. It is carried out thanks to hemoglobin, which accounts for about 95-97% of the mass of proteins in the cytoplasm of red blood cells.
Red blood cells have six main properties:
- Plasticity or ability to undergo reversible deformation.
- Providing creative connections, thanks to which intercellular interaction is carried out.
- Osmotic stability.
- Sedimentability (SOE).
- Destruction. The destruction of red blood cells occurs in approximately 120 days.
- Aggregation.
It is noteworthy that the ability to aggregate is the most important property of these cells.
As a result of this process, rheological disorders occur in the body.
What is red blood cell aggregation
The term aggregation from Latin literally means “joining”. The process of aggregation consists in combining or combining cellular elements into one system . This is the ability of red blood cells to form “coin columns” and their conglomerates of different sizes and densities in the circulatory system.
This process is clearly visible under a microscope in a fresh blood drop, as well as during biomicroscopic examination of small vessels. The density of the aggregates increases over time, and the boundaries of individual blood cells begin to decrease.
Red blood cells, blood transfusion
Previous66Next
| Rice. 194. Erythrocytes: 1 - erythrocyte membrane; 2 - cytoplasm. |
They are formed in the red bone marrow (5-10 million/sec), life expectancy is 3-4 months, destruction (hemolysis)
occurs in the liver and spleen.
Structure.
Mature red blood cells are biconcave, anucleate cells.
The cell membrane may contain agglutinogens A
, or
B
,
Rh+
- protein, and other proteins. Under the shell there is cytoplasm with a large amount of hemoglobin (the nucleus and other cell organelles are completely absent in mature human erythrocytes). The diameter of erythrocytes is about 7-8 microns, thickness - 2-2.5 microns (Fig. 194).
Functions.
The main functions of red blood cells are related to the transport of oxygen to the tissues and carbon dioxide to the lungs.
Hemoglobin
is a protein
having a quaternary structure and consisting of 4 hemes
, containing Fe2+ and
globin
from four polypeptide chains (2 α-chains and 2 β-chains).
Hemoglobin easily combines with oxygen: Hb + 4O2 = Hb(O2)4, this compound is called oxyhemoglobin
, the connection of Hb with carbon dioxide is
carboxyhemoglobin,
with carbon monoxide is
carboxyhemoglobin
, and the affinity for carbon monoxide in hemoglobin is 300 times higher than for O2 .
The transport of gases is facilitated by the small size of erythrocytes (the more oxygen a given type of mammal requires for life, the smaller the size of erythrocytes); The biconcave shape facilitates the diffusion of gases into the cell and makes it possible for the cell to deform when passing through the capillaries. The number of red blood cells increases if a person lives high in the mountains. For the formation of red blood cells (erythropoiesis)
Vitamin B12 is required;
When there is a lack of oxygen in the blood, the kidneys produce erythropoietin
, which accelerates erythropoiesis.
A decrease in the blood's ability to carry oxygen is called anemia
. The causes of anemia may be a decrease in the number of red blood cells, the amount of hemoglobin, a lack of vitamin B12 and iron in foods, and blood loss.
Blood transfusion, Rh factor.
When blood is transfused from a donor to a recipient,
agglutination
(sticking) and
hemolysis
(destruction) of red blood cells are possible.
To prevent this from happening, it is necessary to take into account the blood groups discovered by K. Landsteiner and J. Jansky in 1900. Human blood plasma may contain special proteins called agglutinins
, which interact with
agglutinogens
in the membrane of red blood cells, causing their agglutination.
It is known that agglutinin α
, contained in plasma, glues red blood cells containing
agglutinogen A
;
agglutinin β
- glues together red blood cells containing
agglutinogen B
.
The first blood group does not contain agglutinogens in erythrocytes and is called group zero (0), the blood plasma of this group contains αβ
;
in people with the second group, agglutinogen A
, and agglutinin
β
;
in people with the third group, agglutinogen B is in the erythrocytes, and agglutinin α is in the plasma; the fourth group has agglutinogens AB
, there are no agglutinins in the blood plasma.
If the donor's blood contains agglutinogens that are glued together by the recipient's plasma, complete agglutination of the donor's red blood cells occurs (+). Partial agglutination (- +) is possible if some of the recipient's red blood cells stick together with donor blood agglutinins.
Red blood cells of group 1 are not glued together by the recipient's plasma, therefore the first group is called a universal donor
, but when the first group is transfused to the second, third and fourth, partial agglutination of the recipient’s red blood cells occurs, so only blood of the same group is transfused.
The fourth blood group does not contain agglutinins in the plasma and does not glue the red blood cells of a donor of any group; it is called a universal recipient
, but partial agglutination of one’s own red blood cells with donor plasma agglutinins is possible. In addition to the ABO system, there are other antigen systems, so it is best to infuse your own blood, prepared in advance.
Table 3.
Blood transfusion using the ABO system
| D R | 1 — 0 αβ | 2 - A β | 3 - V α | 4 — AB — — |
| 1 — 0 αβ | — | + | + | + |
| 2 - A β | — + | — | + | + |
| 3 - V α | — + | + | — | + |
| 4 — AB — — | — + | — + | — + | — |
In 1940, K. Landsteiner discovered that 85% of people in the membranes of their red blood cells contain the protein Rh factor (Rh+).
When repeated transfusion of Rh-positive
(Rh+)
blood, compatible according to the
AB0
, to a Rh-negative
(Rh-)
transfusion shock
is observed associated with agglutination of the donor's red blood cells by the recipient's Rh antibodies.
If a woman is Rh-
, and the fetus is
Rh+
a Rh conflict
arises associated with the destruction of the red blood cells of the fetus, which is especially dangerous during the second pregnancy. Blood groups and the Rh factor are inherited and remain in a person throughout his life.
Blood clotting
The most important protective function of blood. This process is influenced by 13 factors present in the blood plasma, as well as 12 factors secreted by platelets. Most Important 5: Fibrinogen
,
prothrombin
, tissue and blood
thromboplastin
,
Ca2+ ions.
Platelets, flat, anucleate cells, are formed in the red bone marrow and live 5-11 days.
They are destroyed in the liver and spleen. Like leukocytes, they are capable of movement and the formation of pseudopodia. The most important function is participation in hemostasis
(blood clotting).
© At the first stage
hemostasis, when vascular damage occurs, tissue thromboplastin is released, platelets adhere to the damaged cells and are destroyed, and platelet thromboplastin is released
.
© At the second stage
hemostasis under their influence, with the participation of Ca2+ and other coagulation factors, prothrombin in the blood plasma is converted into thrombin.
© At the third stage
thrombin causes the polymerization of fibrinogen dissolved in plasma into insoluble fibrin fibers, in which blood cells are retained, a clot is formed, and bleeding stops.
Blood plasma without fibrin is called serum
.
Hemophilia
- blood incoagulability, a disease associated with a recessive mutation in the sex X chromosome. Since men have only one X chromosome in their cells, hemophilia most often affects men.
There is also an anticoagulant system
, thanks to which blood clots dissolve, the blood in the vessels does not clot.
In the cells of the liver, lungs and some leukocytes (basophils), heparin
, which prevents blood clotting.
Previous66Next
Date added: 2016-05-30; views: 2916; ORDER A WORK WRITING
Similar articles:
Blood scan, thick blood and causes of increased blood viscosity
Our center performs blood scanning , which allows us to visually determine the causes of thick blood during hemoscanning diagnostics. Let's take a closer look at what human blood is and its functions, what thick blood is and the reasons that contribute to increased blood viscosity.
Normal human blood viscosity * Normal human blood viscosity *
Human blood is an opaque, red liquid consisting of:
- pale yellow blood plasma;
- formed elements suspended in it:
- erythrocytes (red blood cells);
- leukocytes (white blood cells);
- platelets (blood platelets).
Human blood performs very important functions in the body:
- Human blood serves as transport for various substances, hormones and heat within the body (cardiovascular system). The blood carries respiratory gases - oxygen O2 and carbon dioxide CO2.
- Blood participates in water-salt metabolism in the body and ensures the maintenance of the constancy of its internal environment (homeostasis).
- The protective function of human blood is to provide immune reactions and create blood and tissue barriers against foreign substances, microorganisms, and defective cells of one’s own body.
Blood is the main living medium, on the quality of which all processes occurring in organs and cells depend.
In case of disturbances in the quality of human blood:
- blood viscosity ( thick blood );
- acidification;
- increased blood cholesterol levels;
- presence of hostile bacterial flora (fungi, parasites)
the main transport function of the blood becomes difficult, which leads to disruption of redox processes in all organs and tissues, including the brain, lungs, heart, liver, and kidneys. The quality of human blood composition must be maintained within the limits of optimal homeostasis, eliminating causes leading to impaired blood viscosity.
Fatigue, drowsiness during the day, memory impairment are the most common and obvious signs of a violation of the composition of human blood (thick blood).
Thick blood - sticking of red blood cells (sludge) * Thick blood - sticking of red blood cells (sludge) *
Causes of high acidity
Everyone knows that the normal blood pH is 7.43 units. This blood constant is practically unchanged and ranges from 7.45 to 7.33 units .
When the plasma pH shifts to the acidic side, the erythrocyte membranes change their charge from negative to positive.
The higher the level of such “acidification,” the more positively charged the membranes of red blood cells become in the blood and the more strongly they stick together. The longer and more closely the red blood cells stick together, the higher the degree of “acidification” of the plasma.
In an insufficiently alkaline environment, blood cells lose their mobility, which leads to a decrease in the ability of blood cells to perform a transport function and the development of oxygen starvation.
An important role in assessing the condition of the blood is played by the size, shape, and degree of coloring of red blood cells in the blood.
Normally, red blood cells in human blood should be the same size, large, round in shape, with clearly defined edges, intensely colored, not glued together, and mobile (mobility is due to the mutual repulsion of similarly charged red blood cell membranes). These indicators indicate the health of red blood cells and the normal acid-base balance of the blood. Separately located round red blood cells in human blood, having different sizes, indicate a lack of B vitamins, folic acid and iron in the human body.
The presence of red blood cells in the blood with “bitten”, “jagged” edges indicates a large number of free radicals , which is often a consequence of the activation of peroxide oxidation in the body, as well as prolonged work at the computer and exposure to high doses of radiation (office workers, accountants, bank employees) , insufficient presence of antioxidants in food.
A large number of free radicals leads to the development of more than 80 chronic diseases and oncology.
Assessing the state of platelets in the blood provides additional information about the patient's health status. The accumulation of large groups of platelets in the blood indicates a predisposition to thrombosis.
This picture is often observed when the body is allergic, the presence of a large number of antibodies in the blood plasma (infectious, autoimmune processes).
The purity of human blood plasma is of particular importance .
Presence of inclusions in blood plasma:
- cholesterol crystals;
- uric acid salts;
- orthomonophosphoric acid salts;
- bacteria, larvae, fungi and their spores;
- rapidly falling fibrinogen spicules,
is an indication of predisposition to the development of the disease. Early loss of fibrinogen spicules indicates signs of liver stress or overwork. The presence of a large number of fungi, pathogenic bacteria, helminth larvae, and protozoa indicates the presence of dysbacteriosis .
Cholesterol crystals in human blood form when the amount of cholesterol in the blood is increased and the body is not able to completely utilize it on its own. Increased blood cholesterol levels can cause the development of cardiovascular diseases.
Uric acid salts indicate a violation of the filtration ability of the kidneys, a predisposition to the formation of sand, urolithiasis, and gout.
Salts of orthophosphoric acid indicate a pronounced disturbance of phosphorus-calcium metabolism, calcium deficiency in the body, which again is a prerequisite for the development of various pathologies.
Hemoscanning as a diagnosis using a drop of live blood helps to select an individual comprehensive health program for the patient and can be used to evaluate the results of treatment based on blood composition and the necessary correction of treatment course procedures.
Material Blood scan, thick blood and causes of increased blood viscosity viewed 107519 times
Red blood cells
Red blood cells, or, scientifically, erythrocytes , deliver the oxygen we inhale from the lungs to the cells of the body. Hemoglobin, a bluish-red pigment containing iron, helps them in this. Here's how it happens. In the lungs, where the capillary vessels are especially narrow and long, red blood cells literally have to squeeze through them. They are pressed against the walls of the capillaries, and only the thinnest layer of epithelium separates them from the alveoli - the pulmonary vesicles that contain oxygen. This layer does not prevent the hemoglobin iron from capturing oxygen and, forming an unstable compound oxyhemoglobin with it, supplying red blood cells with oxygen. At the same time, hemoglobin changes its color. The same thing happens with blood: from dark red, when saturated with oxygen, it becomes bright scarlet. Now red blood cells carry oxygen throughout the body. With the help of oxygen, body cells burn (oxidize) the hydrogen they extract from food, turning it into water and producing ATP. At the same time, carbon dioxide is formed. Some of it enters the red blood cells. Most of the blood plasma is delivered to the lungs, and from there carbon dioxide is expelled when exhaled.
It is not easy to provide oxygen to 100 trillion. cells. Therefore, the number of red blood cells in human blood is very large: about 25 trillion. If you stretch them into a chain, its length will be 200,000 km - you can encircle the globe five times. The total surface area of red blood cells involved in gas exchange is also large - 3200 square meters. m. This is the area of a square with a side of about 57 m.
Red blood cells live very short. After just four months they are destroyed (this happens mainly in the spleen). Therefore, every day more than 200 billion new red blood cells are formed in the bone marrow.
Red blood cell aggregation: what is it? how is it happening?
Many people who do not have a medical background may think that red blood cell aggregation is the name of some laboratory test.
In fact, this is a condition that medicine has been fighting for many years. Let's remember the well-known aspirin. It is taken not only as an antipyretic.
Aspirin is a disaggregant, that is, it prevents the aggregation of platelets, but blood is a single system.
There is a whole group of drugs called disaggregants (antiplatelet agents). And they all serve to prevent this phenomenon of aggregation of different blood cells from occurring.
Everyone knows the so-called special, “heart” aspirin. Its task, in simple words, is to “thin” the blood. Of course, it does not discharge the blood at all, but rather prevents aggregation.
Aggregation is the gluing of red blood cells, platelets and any formed elements.
Aggregation and agglutination, what is the difference?
From a physics point of view, aggregation is the combination of various particles that are influenced by attractive forces and various intermolecular forces. The result of aggregation is the gradual enlargement of particles.
If we are talking about the splitting of a large particle into separate small fragments, then we are talking about disaggregation. In simple terms, aggregation is sticking together.
As a result of the aggregation of particles, they gradually become so heavy that they simply cannot be suspended and begin to gradually settle. This process is called sedimentation.
As for agglutination, there is a difference between it and aggregation. During agglutination, a variety of formations stick together and also precipitate, for example, blood cells, tissue cells, bacteria, various non-living chemical particles on which various active molecules are located.
The difference is that the resulting agglutination reaction is caused by antibodies, and these antibodies are called agglutinins. The agglutination reaction is precisely an important laboratory test that allows you to identify various antibodies.
They can be found in the blood, in various tissues, in body fluids, and the agglutination reaction is often used in the diagnosis of infectious diseases and immune disorders.
A classic example of an agglutination reaction is the Widal reaction, which is used to diagnose typhoid fever.
As you can see, both reactions occur in the human body, but erythrocyte aggregation is a universal process, which sooner or later leads to thrombosis, heart attacks, strokes, and causes vascular disasters.
Therefore, it is the aggregation of erythrocytes that is the condition that needs to be combated, since ultimately it is this process that triggers a long-term mechanism leading to early death and disability.
Let us take a closer look at the phenomenon of erythrocyte aggregation and the factors contributing to erythrocyte aggregation.
About aspirin
We must reveal the secret. The use of aspirin and other drugs that are classified as antiplatelet agents, such as clopidogrel, ticlopidine, dipyridamole, begin to affect not red blood cells at all, but platelets. Aspirin has a classic mechanism: it first slows down the action and then destroys the enzyme cyclooxygenase, which is an inflammatory enzyme.
As a result, platelets stop producing a compound called thromboxane. And this thromboxane promotes platelet aggregation and constricts blood vessels.
The use of aspirin prevents the formation of platelet lumps, but it must be remembered that any interference with the normal fluidity of the blood immediately affects the most common cells - red blood cells. This is the therapeutic effect of disaggregants. As for the treatment of erythrocyte aggregation itself, these are infusions of various crystalloid and colloid solutions, and drugs that enhance microcirculation.