Causes
There are many causes of diseases accompanied by secondary arterial hypertension. The nature of the manifestation depends on the etiological factors. Renal pathology is characterized by increased diastolic pressure. Hemodynamic forms of diseases are manifested by high systolic pressure. The pathology of the endocrine system is characterized by a systole-diastolic increase in blood pressure.
The causes of symptomatic hypertension are grouped into groups that characterize the pathology. The following disorders are considered to be the causes that form hypertension syndrome:
- kidney damage of various origins;
- endocrine pathology with impaired hormone production;
- neurogenic factors associated with increased intracranial pressure;
- alcohol consumption;
- influence of toxic substances;
- presence of rare syndromes;
- cardiovascular pathology;
- use of medications;
- others.
The variety of causes makes it difficult to diagnose the secondary nature of hypertension and affects the timely identification and treatment of the causes of the pathology.
Preeclampsia due to hypertension
In patients with primary hypertension, gestosis in pregnant women, according to statistics, ranges from 36% to 86%. And this percentage difference is associated with the stage of hypertension.
Gestational hypertension occurs:
- Expressed in one-time increases in blood pressure, which are caused by fear or stress; the manifestation of “white coat syndrome”, when the patient is afraid of the doctor and the upcoming manipulations;
- Against the background of existing hypertension, the woman became pregnant with it (this is a separate risk group);
- Hypertension that first appeared during pregnancy, if it is caused by renal pathology or disturbances in the functioning of the cardiovascular system, then the name of the disease will be “pure gestosis.”
And if an increase in blood pressure (persistent) is noted after delivery, then this may be either a consequence of gestosis or an aggravated course of hypertension.
The risk group for pregnant women, which designates women with a high probability of gestosis, includes expectant mothers with extragenital pathology. These are dysfunctions of the central nervous system, these are renal pathologies, diabetes mellitus, obesity and, finally, already existing hypertension at the time of pregnancy. Women who have experienced it in a previous pregnancy are also susceptible to gestosis. Young expectant mothers (under 18 years old) and older ones (35+) are in the same risk zone. Like those mothers who gained more than 12 kg of excess weight during gestation.
Symptoms
Secondary hypertension is characterized by the presence of symptoms uncharacteristic of essential hypertension. The presence of the following signs helps to suspect such changes:
- development of hypertension at a young age;
- malignant course of the disease;
- sudden development of the disease;
- the occurrence of sympathoadrenal crises;
- refractory to drug therapy.
Symptomatic hypertension is accompanied by signs of the underlying disease. The purpose of the examination is to establish the secondary nature of hypertension.
How to treat symptomatic hypertension
The goal of therapy for such a pathology is to achieve a stable decrease in pressure. But this can only be done if the root cause of the disease can be established. Therapy can be medicinal (conservative) and surgical.
Surgical intervention:
- This is the main method for the treatment of tumors of the brain, as well as kidneys and endocrine organs;
- Surgery may be a way to treat hypertension if it is caused by heart defects.
Drug treatment is required if hormonal imbalances are not corrected surgically. Perhaps the appointments will be for life. The drugs that are used are considered to be antagonists of those hormones that are produced in excess. It turns out that these medications block the action of hormones and prevent the development of hypertension.
Classification
For symptomatic arterial hypertension, the classification was developed according to the primary etiological factor, which determines the following types of pathology:
- endocrine;
- renal;
- neurogenic;
- hemodynamic;
- medicinal;
- others.
Secondary hypertension is divided into the following types based on blood pressure levels, changes in the myocardium and fundus:
- transient;
- stable;
- labile;
- malignant.
Each form has characteristic features that form the basis for choosing the right treatment tactics.
Arterial hemodynamic
This form of secondary arterial hypertension occurs when the heart muscle and large vessels are damaged. According to the development mechanism, the following options are distinguished:
- stagnant;
- systolic;
- regional;
- rheological.
The clinical manifestations are based on disruption of normal blood flow through the main vessels. The causes of such disorders are atherosclerotic changes, developmental defects, and increased vascular tone.
Important information: What IVs are used for high blood pressure (hypertension) and their composition
Pulmonary hypertension
The development of pulmonary hypertension is a consequence of pathology of the bronchi and lungs, autoimmune diseases, vascular thrombosis, and heart defects. The initial manifestations of the disease are characterized by nonspecific symptoms:
- difficulty breathing;
- weakness, fatigue;
- tachycardia with minimal physical activity.
A high level of hypoxia determines the appearance of severe shortness of breath, cough, tachyarrhythmia, and hemoptysis. Timely diagnosis allows you to prevent the development of fatal complications.
Renal
Renal hypertension develops as a result of parenchymal, vascular, secondary lesions and is the most common. They have a progressive course and are characterized by the development of a malignant form.
The following signs help determine a diagnosis of renal pathology:
- young age;
- absence of cardiac and brain changes;
- fast development;
- malignant course;
- high diastolic pressure numbers.
It is recommended to conduct a thorough examination to establish an accurate diagnosis and rational choice of therapy.
Pheochromocytoma
Chromaffin tumor, which produces catecholamines in large quantities. Clinical manifestations of symptomatic hypertension are associated with hormones entering the bloodstream. The peculiarity of the release of catecholamines determines the clinical variant of the disease.
The paroxysmal form is manifested by a crisis course, which is characterized by a triad of symptoms. The release of a large amount of adrenaline is accompanied by severe headache, hyperhidrosis, and severe tachycardia. Hypertensive attacks occur suddenly and resolve on their own. The persistent form can proceed without crises.
Patients have a characteristic appearance:
- underweight;
- pale skin;
- tremor and coldness of the extremities;
- increased excitability.
There are no specific complaints in the interictal period, which makes diagnosing the disease difficult. In most cases, the pressure normalizes after surgical treatment.
Primary aldosteronism
Adenomatous tumors of the adrenal cortex produce excessive amounts of aldosterone. This situation creates specific symptoms:
- persistent rise in blood pressure;
- hypokalemia;
- metabolic disorders.
The changes lead to severe muscle weakness, nocturia, and the appearance of seizures.
Diagnosis of Conn's disease consists of several stages:
- laboratory research;
- drug tests;
- instrumental examinations.
Women get sick more often. Characterized by a moderate increase in blood pressure, the development of alkalosis, and persistent hypokalemia. Severe complications are rare.
Itsenko-Cushing syndrome
The early development of arterial hypertension in Itsenko-Cushing syndrome is associated with hypersecretion of cortisol, a tumor of the adrenal cortex. Excess glucocorticoids changes the hormonal spectrum of the blood, which forms the clinical picture.
Important information: How often can Magnesia be injected intramuscularly for high blood pressure (hypertension) and what dosage is needed
External signs of the syndrome are as follows:
- excess body weight;
- moon-shaped face;
- hirsutism;
- hypertrichosis;
Weakness and muscle atrophy develop. It is characterized by moderate hypertension and is characterized by a benign course.
Special diagnostic algorithms allow you to make a timely and accurate diagnosis.
Medication
This form of hypertension is associated with taking certain groups of drugs that provoke a rise in pressure due to the vasoconstrictor effect, fluid retention, and changes in blood rheology.
Medicines that provoke the development of the disease are grouped as follows:
- hormonal contraceptives;
- catecholamines;
- sympathomimetics;
- tricyclic antidepressants;
- monoamine oxidase inhibitors;
- non-steroidal anti-inflammatory drugs.
The development of secondary hypertension is facilitated by uncontrolled and long-term use of drugs.
Neurogenic
The cause of the neurogenic form of the disease is closely related to the pathology of the nervous system. Brain tumors, injuries, and inflammatory processes are considered priority.
The formation of a neurogenic variant of the disease is provoked by:
- diencephalic syndrome;
- increased intracranial pressure;
- porphyria;
- lung pathology.
Neurogenic hypertension accompanies symptoms of damage to brain structures. Diagnostic methods are used to select the correct treatment tactics.
Description of the disease
Secondary, or symptomatic arterial hypertension is a pathology in which an increase in blood pressure (BP) is recorded, caused by another disease and of a secondary nature. For example, with damage to the kidneys, blood vessels, and endocrine system. It is registered in 5-10% of cases among people with high blood pressure. However, if we take into account the malignant course of hypertension, the incidence reaches 20%. It is often registered in young people - in 25% of cases under the age of 35 years.
It is important to identify and begin treatment for this condition as early as possible, since a constant increase in blood pressure leads to irreversible consequences for the heart and blood vessels.
The likelihood of developing severe complications, such as heart attack or stroke, even in young people, increases. Therapeutic effects involve treatment of the primary disease causing increased blood pressure. Correcting blood pressure levels with medications for an untreated primary disease most often does not have an effect.
Diagnostics
Difficulties in making a diagnosis are due to the variety of causes for the development of secondary arterial hypertension.
Diagnostic algorithms have been developed for each form of symptomatic hypertension. The use of a full range of measures increases the accuracy of diagnosis and provides the opportunity to decide on the choice of therapy.
Informative methods for diagnosing renal forms of the disease include:
- laboratory tests of blood and urine;
- angiography;
- ultrasonography;
- radioisotope renography;
- computed tomography;
- kidney biopsy examination.
Diagnostic studies for suspected endocrine nature of hypertension additionally include a biochemical blood test, hormonal spectrum, and indicators of carbohydrate metabolism. A computed tomography scan of the pituitary gland and adrenal glands is performed.
If tumor-like formations are detected, a radioisotope scan is prescribed.
Hemodynamic forms are subject to angiographic examination, including ultrasound and electrocardiography.
If the disease is neurogenic, a complete neurological examination is performed.
Differences between secondary (symptomatic) and primary hypertension
Symptomatic hypertension - what is it? This is a disease provoked by pathologies of those organs or systems that are involved in pressure mechanisms. It occurs much less frequently than the primary one. Primary hypertension is also called essential hypertension. Why such hypertension develops has not been precisely clarified to this day.
And if it is not clear what exactly causes it, then it is established by excluding problems with those organs that theoretically could trigger the disease. For example, the patient has healthy kidneys, no endocrine or nervous problems, and no disorders of the heart or vascular network. Today it is customary to call primary arterial hypertension a multifactorial disease, and a combination of causes leads to the disease.
Treatment
The goal of therapy is to eliminate the causative factor causing the rise in blood pressure. The treatment provided must be comprehensive, aimed at the underlying disease.
The complex of treatment measures includes:
- drug therapy;
- surgery;
- preventive actions.
Symptomatic hypertension requires a precise choice of treatment method, which depends on the nature of the primary pathology, examination results, and the body’s reaction.
Medication
Drug therapy is carried out for all variants of the disease. They use drugs from different groups. It is advisable to carry out early correction of blood pressure in case of secondary hypertension. The goal is to prevent the formation of persistent disorders in target organs.
Important information: How to take hydrogen peroxide to treat hypertension (high blood pressure)
Drug therapy is aimed at:
- suppression of hormone synthesis;
- achieving the target level of hemodynamics;
- relief of crisis situations;
- symptomatic treatment.
When using medications, it is important to monitor basic hemodynamic parameters to prevent a critical decrease in glomerular filtration.
To normalize the situation, prescribe:
- adrenergic blockers;
- aldosterone antagonists;
- potassium-sparing diuretics;
- sartans;
- calcium antagonists;
- ACE inhibitors.
Phentolamine and sodium nitroprusside are used to relieve crises. Taking medications does not bring the desired result without radical treatment of the primary pathological process.
Surgical
Surgery is the most effective treatment for most diseases accompanied by secondary hypertension. Examination data and drug tests will make it possible to predict the results of the operation. A successful outcome depends on the ability to preserve the organ that has been subjected to ischemia.
The operation is indicated for:
- malformations of the heart and blood vessels;
- tumor formations that secrete large amounts of hormones;
- malignant neoplasms;
- kidney pathologies;
- inability to perform angioplasty.
The extent of surgical intervention in the presence of a tumor depends on its morphology and size. The malignant nature of the tumor is an absolute indication for surgical treatment.
If surgical treatment is not possible, radiation and chemotherapy are resorted to.
Preventive
A set of measures has been developed to avoid the development of complications and prevent the progression of the disease. These priority measures include:
- maintaining a healthy lifestyle;
- limiting physical activity;
- prevention of stressful situations;
- balanced diet.
Preventive measures to prevent the development of secondary hypertension have not been developed for most of the underlying factors.
Patients must be under constant medical supervision, give up bad habits, and strictly follow all prescriptions.
Resistant arterial hypertension
Arterial hypertension (AH) is defined as resistant (refractory) if, while taking three or more antihypertensive drugs of different classes (one of which is a diuretic) in doses close to the maximum, it is not possible to achieve a target blood pressure (BP) < 140/90 mm rt. Art. in most patients with hypertension (or < 130/80 mmHg in patients with diabetes mellitus and renal failure).
The ALLHAT study found that approximately 47% of patients remained resistant to antihypertensive therapy one year after randomization, despite the rigorous titration and drug combination regimens used in the study. Similar results (43% resistant patients) were obtained in the Syst-Eur Study. According to Yakovlevitch and Black, suboptimal drug regimen is the most common cause of resistance (43%), the next most common cause is drug tolerance (22%), followed by secondary hypertension (11%), low compliance (10%).
Refractory hypertension (RAH) can be divided into two broad categories: true RAH and pseudo-resistant hypertension.
PSEUDO-RESISTANT AG
Problems associated with blood pressure measurement
A large number of publications in the medical press and guidelines are devoted to the basic rules for measuring blood pressure, as well as technical factors influencing blood pressure levels. However, general practitioners often neglect the existing rules for measuring blood pressure, which entails a number of errors:
- using a small cuff;
- measuring blood pressure without prior rest;
- rapid release of air from the cuff:
- measuring blood pressure on one arm;
- auscultation before palpation blood pressure measurement.
Pseudohypertension is diagnosed quite rarely: in the case when blood pressure measured using the Korotkoff method does not correspond to the true (intra-arterial) blood pressure level. This phenomenon, associated with severe atherosclerosis and calcification of the brachial and radial arteries, is observed in elderly patients. Thickening and compaction of the arterial wall with age leads to the fact that in order to achieve compression of a stiff artery, a higher pressure (above the true one) is required in the cuff, which leads to an overestimation of blood pressure figures. The presence of pseudohypertension in a patient can be suspected if the following signs are present:
- absence of target organ damage;
- calcification of the brachial and other arteries according to research data (X-ray, ultrasound);
- Blood pressure in the brachial artery is higher than in the legs (which once again illustrates the need for a complete propaedeutic examination of the patient);
- symptoms of hypotension during antihypertensive therapy in the absence of a pronounced decrease in hypertension (usually interpreted in elderly patients as a worsening of the neurological symptoms of dyscirculatory encephalopathy in the vertebrobasilar region);
- severe systolic hypertension.
The existence of pseudohypertension can be verified by the presence of Osler's sign - palpation of the brachial artery even when the intracuff pressure exceeds systolic blood pressure. Final confirmation of the diagnosis is possible only with intra-arterial blood pressure measurement.
Low compliance
Compliance (patient adherence to therapy) is defined as the patient's ability to accurately follow clinical instructions for taking medications and lifestyle modifications. Taking medications in accordance with medical prescriptions in at least 80% is the most common characteristic of medication compliance. Low compliance occurs in more than 50% of patients, including those included in clinical trials. It is noteworthy that the number of patients with low adherence to therapy decreased to 10% among patients observed by specialists in the treatment of hypertension (USA), which demonstrates the importance of specialist qualifications and the lack of time factor in communication with the patient, which is present with general practitioners.
Numerous factors, such as the cost of medications, the low intellectual level of the patient, the complexity of the administration and dosage regimen, etc., should be analyzed by the doctor when diagnosing RAG and suspecting low adherence to therapy. Careful questioning remains one of the best methods for determining whether a patient is adherent to treatment. The clinician should set realistic short-term goals for all specific components of treatment (weight control, salt reduction, physical activity, alcohol reduction, and, if possible, a single or double dosage regimen) and individualize their recommendations as much as possible based on the specific clinical situation, social and family characteristics of the patient.
Errors in prescribing medications
Such errors are a common cause of the development of pseudo-resistant hypertension. Despite the huge number of clinical studies, the constant publication of research and methodological materials in the medical press, widespread discussion of the rules of prescription and combination of drugs among general practitioners and cardiologists, errors in the dosing and combination of antihypertensive drugs are quite common.
Modern tactics of drug antihypertensive therapy provide the possibility of choosing between monotherapy and combination therapy. To achieve target blood pressure levels in most patients, especially with grades I–III increases in blood pressure, combination therapy is required.
Among the advantages of combination antihypertensive therapy are the following:
- the use of drugs with different mechanisms of action makes it possible to control several pathogenetic links of hypertension;
- the drugs included in the combination are used in lower doses, which reduces the likelihood of side effects;
- when prescribing fixed combinations (two drugs in one tablet), adherence to therapy improves.
The following drug combinations are considered effective and well tolerated:
- diuretics and β-blockers (atenolol, bisoprolol);
- diuretics and ACE inhibitors (captopril, lisinopril, enalapril) or angiotensin II receptor antagonists (valsartan, losartan);
- calcium antagonists (dihydropyridines: amlodipine, nifedipine) and β-blockers;
- calcium antagonists and ACE inhibitors or angiotensin II receptor antagonists;
- calcium antagonists and diuretics;
- α-blockers (doxazosin, terazosin) and β-blockers.
Other combinations with centrally acting drugs (α2-agonists, imidazoline I2 receptor agonists), as well as a three- or more-component regimen can be used.
It is recommended to use long-acting drugs that provide an effect within 24 hours and require a single dose per day, which significantly improves adherence to therapy.
An inadequate regimen of drug use means the prescription of antihypertensive drugs in low doses, the use of pathogenetically illiterate combinations (drugs of the same class, for example verapamil and dihydropyridine, or drugs with a similar mechanism of action - an ACE inhibitor and an angiotensin II receptor antagonist - or similar side effects).
The algorithm for optimizing antihypertensive therapy is shown in Figure 1.
| Figure 1. Algorithm for optimizing drug therapy |
Thus, in the case of resistant hypertension, the clinician must carefully analyze the prescribed antihypertensive therapy regimen: make sure that the prescribed doses are adequate and the pathogenetic justification of the combinations used, as well as the correctness of the prescribed therapy regimen (correlation between the duration of action and the frequency of drug administration). If necessary, another drug should be added to the regimen used, taking into account the individual characteristics of the patient (target organ damage, associated and concomitant pathology).
TRUE RESISTANT AG
Increased variability and reactivity of blood pressure
“White coat hypertension” (“office hypertension”, “office hypertension”) is defined as a state of stable increase in blood pressure during measurement at a doctor’s appointment with normal values outside the hospital. Considered as a manifestation of stress-induced hypertension. According to Brown et al., 2-3 out of every 10 patients with resistant hypertension have good blood pressure control (mean value less than 135/85 mm Hg) with 24-hour blood pressure monitoring. Patients with this phenomenon often demonstrate increased sensitivity to antihypertensive drugs, which significantly reduce “non-stress” blood pressure and can cause symptoms of hypotension. In this case, patients independently discontinue antihypertensive drugs or begin to take them chaotically, which significantly complicates the management of these patients and reduces compliance.
In this case, it is recommended to carry out out-of-office blood pressure measurements (24-hour monitoring and blood pressure self-monitoring diaries) before adjusting the antihypertensive therapy regimen. Despite the relative simplicity of diagnosing this phenomenon, clinicians often underestimate its prevalence and significance, which leads to errors in the selection of drug therapy regimens and decreased compliance.
Baroreflex failure
Blood pressure instability with periods of significant increases and decreases occurs in patients with damage to baroreflex function. This condition is quite rare and very difficult to diagnose.
Physiological resistance (volume overload)
The most common cause of physiological resistance to hypertension is volume overload. Excessive salt intake may cause the development of RAH in treated patients. The use of direct vasodilators (minoxidil, hydralazine), adrenergic blocking drugs (α-blockers and β-blockers) and large doses of potent diuretics can lead to increased fluid retention and the formation of RAG. The most common cause of persistent hypervolemia is the administration of a single daily dose of furosemide. The decrease in intravascular volume within a few hours of furosemide is followed by activation of the renin-angiotensin-aldosterone system (RAAS) with sodium retention mechanisms that restore all lost sodium during the brief interval of natriuresis. If renal function is preserved, a morning dose of long-acting hydrochlorothiazide (12.5–25 mg) can break this vicious cycle. All drugs that lower blood pressure also reduce renal perfusion pressure and glomerular filtration, which leads to sodium and fluid retention.
Unfortunately, many patients with RAH who are receiving multiple antihypertensive medications are not prescribed diuretics in adequate doses. Limiting salt intake in itself leads to adequate control of circulating plasma volume, lowering blood pressure, improving treatment tolerability, and reducing the number of antihypertensive drugs used. With a decrease in salt intake, the effectiveness of all antihypertensive drugs increases, with the exception of calcium antagonists.
If volume overload is suspected, the amount of sodium in 24-hour urine should be determined. At the same time, inadequacy in the implementation of dietary recommendations is often found in patients who claim to follow a low-salt diet. In patients who do not follow a low-salt diet, sodium excretion increases.
Drug interactions
Identification of drugs that reduce the effectiveness of antihypertensive therapy is extremely important, as it helps to individually optimize therapy in patients, taking into account the mechanism of action of the drugs used. Let's focus only on the most frequently used ones.
Steroids. Hypertension is reported in more than 20% of patients taking synthetic corticosteroids. Taking these drugs can also cause hypertension resistance. A risk factor for the development of RAH is old age. Medicinal substances such as natural licorice, phenylbutazone, carbenoxolone, prednisolone, and cortisol preparations have mineralocorticoid activity. Taking these drugs in moderate doses can lead to pseudohyperaldosteronism (sodium retention, hypervolemia, hypokalemia with metabolic alkalosis and suppression of plasma renin and aldosterone). Ointments, antihemorrhoidal drugs, eye drops, inhaled bronchodilators, nasal antiallergic sprays may contain substances with significant mineralocorticoid activity. Some of these drugs may contain sympathetic amines. To reduce blood pressure and overcome refractoriness, it is necessary to stop using these drugs. In cases where steroid therapy is mandatory, diuretics are effective drugs. Potassium monitoring is necessary during diuretic therapy, since these drugs can increase hypokalemia in steroid-dependent hypertension.
Sex hormones. Oral contraceptives are capable of inducing hypertension in approximately 5% of cases when using high-dose combinations of estrogens and progestins. Risk factors for the occurrence and worsening of hypertension are smoking, obesity, race (African Americans), diabetes, and renal pathology. Cases of the development of malignant hypertension while taking oral contraceptives have been described. The next risk group for developing RAG is men taking estrogens for the treatment of prostate cancer. Danazol, a semisynthetic androgen used to treat endometriosis and hereditary angioedema, can lead to hypervolemia and worsening hypertension.
Drugs affecting the sympathetic nervous system . Phenylephrine, prescribed in the form of eye drops, and adrenaline-like substances used topically for glaucoma, can lead to an increase in blood pressure in normotensive patients and patients with hypertension. Adding α-blockers, α- and β-blockers to the antihypertensive regimen neutralizes these effects.
Most undesirable anorectics consist of a combination of antihistamine-like substances and adrenergic agonists (usually phenylpropanolamine, ephedrine, pseudoephedrine, or caffeine). α-adrenergic intoxication induced by nasal and oral decongestants and antitussives containing large doses of oxymetazoline, phenylephrine, and ephedrine can induce hypertension or aggravate existing pathology. The drugs of choice are α-blockers, α- and β-blockers.
Non-steroidal anti-inflammatory drugs. NSAIDs may potentiate the increase in blood pressure and compete with antihypertensive drugs. NSAIDs increase the risk of developing hypertension by 40%. NSAIDs interact with some antihypertensive drugs, such as diuretics, beta-blockers, ACE inhibitors, but not with calcium channel blockers - centrally acting drugs whose antihypertensive effectiveness is not related to the production of prostaglandins. Indomethacin, piroxicam, and naproxen cause significant increases in blood pressure, while sulindac and full-dose aspirin have the least effect on blood pressure. Minimum doses of aspirin do not affect blood pressure in patients with hypertension. Selective cyclooxygenase-2 inhibitor drugs (celecoxib, rofecoxib) do not increase blood pressure and do not have dose-dependent effects on blood pressure. Meta-analyses have shown that NSAIDs lead to an increase in mean blood pressure of 4–5 mmHg. Art. They cause sodium retention and increased sensitivity to pressor hormones. Given the high prevalence of joint and spine diseases among elderly patients, clinicians should be keenly aware of the possible interactions of NSAIDs with antihypertensive drugs.
Tricyclic antidepressants. Tricyclic antidepressants antagonize the hypotensive effects of adrenergic blockers such as guanethidine, which can lead to a significant increase in blood pressure. These drugs prevent the accumulation of antihypertensive drugs in adrenergic nerve endings, where they block the transmission of nerve excitation. Similar interactions have been described for other antihypertensive drugs (methyldopa, clonidine).
Associated states
Metabolic syndrome and obesity. The prevalence of metabolic syndrome is currently becoming epidemic and in some countries, including Russia, reaches 25–35% among the adult population.
In patients with metabolic syndrome, the effectiveness of antihypertensive drugs is reduced, and a two-component regimen, as a rule, does not allow achieving target blood pressure. This is due to the pathogenetic features of hypertension in metabolic syndrome.
Normally, insulin has vascular protective effects and causes insulin-mediated vasodilation. But with chronic hyperinsulinemia and insulin resistance, other pathophysiological mechanisms leading to hypertension are triggered: stimulation of the sympathetic-adrenal system (SAS), RAAS; an increase in the content of intracellular Na+ and Ca2+, a decrease in K+ with an increase in the sensitivity of the vascular wall to pressor influences; increased reabsorption of Na+ in the proximal and distal tubules of the nephron (fluid retention with the development of hypervolemia). Of particular importance is the stimulation of proliferation of smooth muscle cells of the vascular wall under the influence of hyperinsulinemia (narrowing of arterioles and increased vascular resistance).
Failures in the treatment of hypertension in metabolic syndrome are usually due to the focus of therapeutic tactics only on hypertension. Successful therapy is based on the principle of simultaneous correction of all links in the pathogenesis of metabolic syndrome, a comprehensive impact on the causes and consequences of insulin resistance: lifestyle changes, treatment of obesity, treatment of carbohydrate metabolism disorders, treatment of dyslipidemia. When selecting antihypertensive therapy, the following features should be taken into account: metabolic effects of antihypertensive drugs (effect on lipid spectrum, insulin resistance, glucose and uric acid levels); the need for more frequent use of a 3- and 4-component therapy regimen with an impact on various parts of the pathogenesis of hypertension characteristic of metabolic syndrome.
Smoking leads to a transient increase in blood pressure and increased blood pressure variability. With a large number of cigarettes smoked, the duration of episodes of hypertension increases. The antihypertensive effectiveness of β-blockers in smoking patients with hypertension is reduced.
Alcohol. Alcohol abuse (chronic alcohol intoxication) leads to increased blood pressure in normotensive patients and induction of resistance to antihypertensive drugs. There are dose-dependent hypertensive effects of alcohol. The main type of treatment is to stop or reduce drinking. In some cases, stopping alcohol intake does not improve blood pressure control.
Genetic features
The polygenic syndrome of essential hypertension includes a wide range of hemodynamic and neuroendocrine features. Thus, plasma renin activity partially determines individual sensitivity to β-blockers, ACE inhibitors, and angiotensin II receptor antagonists. The connection between changes in the angiotensinogen gene and salt sensitivity is widely known. Genetically determined changes in drug metabolism, such as accelerated metabolism (hydralazine), have been described, but significant genetic features of metabolism have not been confirmed for the main classes of antihypertensive drugs. It is generally accepted that sensitivity to diuretics is high and relatively low to ACE inhibitors, β-blockers, and angiotensin II receptor antagonists in black patients.
Secondary forms of hypertension
Progression of renal failure is the most common and easily diagnosed cause of hypertension resistance. Renovascular disease is common among patients with previously controlled hypertension, especially if atherosclerotic lesions were present in other vascular territories. Over the past few years, the understanding of the impact of primary hyperaldosteronism (PHA) on the prevalence of RAH has changed significantly. Researchers have noted a high incidence of PHA. Many of these patients have normal plasma potassium levels but elevated plasma aldosterone relative to renin. Most of them are diagnosed with bilateral adrenal hyperplasia, for which surgical treatment is not indicated. The drug of choice in this case is spironolactone.
Obstructive sleep apnea syndrome (OSAS) . According to H. Issakson et al., among patients with refractory OSA is detected in 56% of cases.
Typical “morning” hypertension caused by OSA, predominantly diastolic, is difficult to correct with conventional antihypertensive drugs. Clinicians often underestimate the significance of this condition and do not include questions regarding the patient’s snoring and the presence of sleep apnea in the traditional history-gathering scheme. And this is necessary especially in obese patients.
There are quite contradictory data regarding the effectiveness and safety of antihypertensive drugs of various groups in patients with OSA. Thus, a number of side effects have been identified during treatment with certain antihypertensive drugs, in particular, inhibition of muscle tone in the upper respiratory tract during treatment with β-blockers, α-methyldopa, as well as as a result of metabolic alkalosis caused by diuretics. Other studies confirm the positive effects of diuretics in the form of a reduction in the number of episodes of breathing disorders during sleep. Clearly positive data have been obtained with the use of calcium antagonists and ACE inhibitors.
However, for successful treatment of hypertension in OSA, it is necessary to carry out a set of therapeutic measures aimed at eliminating OSA. The most effective treatments currently are uvulopalatopharyngoplasty and CPAP therapy (continuous positive airway pressure).
The diagnostic algorithm for RAG is presented in Figure 2.
It must be remembered that the cause of hypertension resistance can be a combination of several exogenous factors and also secondary forms of hypertension. Treatment of RAG involves the elimination of exogenous factors and the use of maximum tolerated doses of drugs in a multicomponent treatment regimen, including long-acting diuretics. Many studies prove the necessity and advisability of adding spironolactone to a 3- or 4-component therapy regimen in patients with RAG.
Literature
- Oparil S., Michael A. Weber. Hypertension: A Companion to Brenner and Rector's The Kidney, 2000.
- Erdine S. Resistant hypertension. ESH. Scientific Newsletter, 2003; 4: N15.
- Hypertension Primer, Third Edition, 2003 American Heart Association.
- European guidelines for the diagnosis and treatment of arterial hypertension, 2003.
T. V. Adasheva, Candidate of Medical Sciences, Associate Professor MGMSU, Moscow
Prevention of SAH
Secondary hypertension can also be prevented, and there is nothing difficult or impossible in preventing the disease.
7 points for the prevention of secondary arterial hypertension:
- Rules for healthy eating instead of diets. First, it is recommended to take a test for overeating: perhaps the fact is that you do not have the principle of moderation in eating. Then you have to determine how many meals a day you should have: some people eat strictly three times a day, no snacking, and that's fine. There should always be breakfast - don't replace it with a cup of coffee. Breakfast is always hearty and nutritious, but it is not the same as fatty and heavy. A complete lunch: protein and vegetables. Dinner is the same: raw vegetables, grilled, or in a salad, plus lean protein (chicken, turkey, beef, rabbit) or any fish or seafood.
- Must-haves to fuel the body. This can include various bioactive complexes and biological food additives. Today, it's easy to find lists specifically for women that include curcumin, fish oil, raw probiotics, collagen, etc. There are lists for maintaining men's health - these are sunflower lecithin, Omega-3, vitamin D, etc. Vitamin-mineral complexes and dietary supplements, when chosen wisely, help to avoid age-related diseases, deterioration of the condition of tissues and organs, and immune failures.
- Sports and physical education are our everything. For many, the topic of healthy lifestyle is unpleasant to the point of grinding teeth, but there is no need to treat it as something intrusive and complicated. 7000-8000 steps a day, which you record with a pedometer - and you are already on the move, already “running away” from hypertension. Find your version of physical activity.
- To give up smoking. No matter how much we talk about it, in the minds of many people this question is impenetrable. Today, people in their early thirties are forced to take blood thinners because their body has wasted its resources prematurely due to smoking.
- Ability to withstand stress. This was mentioned above, but it can be repeated - stress is not just a bad mood, apathy, or a pessimistic scenario. These are special reactions in brain structures that lead to disruptions in the regulation of important processes in your body.
- Timely diagnosis. This point has nothing to do with well-being. Both people of modest means and wealthy patients often equally dislike visiting doctors. Even when nothing worries you - just getting tested, appearing to specialists is something extremely complicated for them. But this is an indicator of immaturity and irresponsibility. And your state of health will definitely remind you of this.
- Life is like joy. Not a single physician would argue with the fact that recovery and the ability to maintain one’s health capital also depend on the patient’s worldview, sense of humor, and ability to correctly live through various situations. Some give up even before they start treatment - they become depressed from completely treatable diagnoses, feel sorry for themselves and do not take constructive steps. And doctors will also note that cheerful people who know how to treat themselves and the world around them with irony endure even complex treatment more easily, they are more active and less fixated on living through their suffering.
Probably, you can add a few more points to this list, but even if you think carefully about each of them, you will push the danger of developing hypertension a little away from yourself.
How does SAG manifest?
The most indicative symptom of hypertension is persistently high blood pressure or frequent pressure surges. All other symptoms are secondary, and different patients exhibit their own set of symptoms. For example, one person simply experiences increased pressure, a headache, and an inexplicable feeling of anxiety. Another person, in addition to increasing values on the tonometer, experiences nausea and even vomiting, his face turns red, and his fingers tremble.
Common symptoms of SAH include:
- Dizziness that occurs suddenly;
- Constant feeling of fatigue, weakness, powerlessness;
- The appearance of attacks of obsessive nausea and, in some cases, vomiting;
- Development of pain in different parts of the head;
- Psycho-emotional status disorders;
- An increase or, conversely, a decrease in body temperature;
- Pain behind the sternum;
- Tinnitus (in one ear);
- Swelling of the face;
- Rapid pulse.
Surveys of patients show that they sometimes suffer from panic attacks - they are overcome by the fear of death, they sweat intensely, and their heartbeat increases. Panic attacks are not unique to hypertension, but, of course, this symptom cannot be ignored.
Like a rapid pulse, it is too common a symptom to make any diagnoses based on it alone. Sometimes it's just excitement, and sometimes it's a really worrying sign. But it shouldn’t scare you: fear doesn’t solve anything, but a timely trip to the doctor can save you from serious problems.
Renal hypertension
Renal symptomatic hypertension develops against the background of diseases of the urinary system. Renal symptomatic hypertension includes renovascular and renoparenchymal forms.
Renal hypertension develops against the background of diseases of the urinary system
Renovascular form
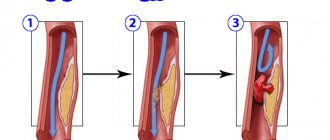
The most common type of symptomatic renal hypertension. Blood pressure increases due to decreased circulating blood volume. Little fluid reaches the kidneys, which leads to insufficient filtration.
To eliminate the disorder, the body begins to produce more renin, which is responsible for regulating blood pressure. Excess renin leads to vascular spasm, the lumen of blood vessels narrows, blood moves more slowly through the arteries, and pressure increases.
Causes of renovascular symptomatic hypertension
The main causes of symptomatic hypertension of the renovascular type:
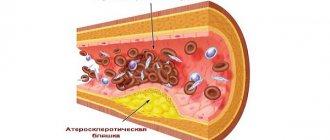
- atherosclerotic disorders: the most common cause of high blood pressure, in which the vessels allow less blood to pass through due to cholesterol plaques;
- blockage of blood vessels by blood clots: blood flow slows down due to blood clots that accumulate in the vessels;
- inflammatory processes in the kidneys: pyelonephritis, autoimmune diseases, other kidney dysfunctions.
Less commonly, blood pressure increases due to compression of the kidney arteries by neoplasms, inflammation of the vascular walls, or vascular overgrowth.
Symptoms
Clinical signs of renovascular symptomatic hypertension are easy to recognize:
- severe pain in the head, especially in the occipital region;
- vomiting: attacks of vomiting may signal the development of ischemia;
- loss of strength, sleepy state: complete loss of interest in the environment, such deviations can signal serious disturbances in the structure of the brain;
- low pulse pressure: the difference between systolic and diastolic indicators does not exceed 20 points.
Renovascular hypertension is accompanied by pain during urination, decreased daily diuresis, and polyuria.
Renovascular symptomatic hypertension is more common in women under 30 years of age and in men after 50 years of age. The patient feels satisfactorily; there are no sudden increases in pressure. With renovascular hypertension, the likelihood of developing a hypertensive crisis remains low.
A sign of renovascular hypertension may be pain in the back of the head
Diagnosis and treatment
Before drawing up a treatment regimen, the doctor conducts a full examination. To cure renovascular hypertension, it is necessary to determine the root cause of the pathology. To normalize blood pressure, complex treatment will be required. Antihypertensive drugs will not lead to improvement.
Renoparenchymatous
This type of symptomatic renal hypertension is less common.
Causes of pathology
Renoparenchymal symptomatic hypertension develops against the background of inflammation, which provokes excessive production of renin.
Symptoms
Renoparenchymal symptomatic hypertension has similar symptoms. High blood pressure is accompanied by swelling, pain in the lumbar region, and impaired urination.
Diagnosis and treatment
To diagnose symptomatic hypertension of the renoparenchymal type, it is necessary to conduct a comprehensive examination, including a general urinalysis, ultrasound, scintigraphy, and magnetic resonance imaging.
Renoparenchymal renal hypertension cannot be triggered. At the first signs of illness, you should immediately consult a doctor, who will draw up a treatment regimen according to your indications. Left untreated can lead to heart attack and other complications.
Treatment is carried out in a hospital. The doctor prescribes a complex of antihypertensive drugs, sometimes surgical intervention may be required. The patient is in a hospital until his condition is completely stabilized.