Causes
Experts identify the main causes of vertebrobasilar syndrome:
- Cervical osteochondrosis (degenerative changes in the vertebrae), which negatively affects the patency of blood vessels in the brain and leads to spasms and impaired blood flow in the main arteries. According to statistics, every third patient with osteochondrosis is at risk of developing vertebrobasilar syndrome.
- The syndrome can be congenital - pathologies during pregnancy and childbirth (trauma, premature birth, any violation of the integrity of the blood vessels of the baby's brain), congenital anomalies (dysplasia, congenital circulatory disorder - hypoplasia, Kimmerly's disease - a congenital defect in the area of the connection of the vertebrae and the skull).
- Acquired injuries of the cervical vertebrae (accidents, road traffic and sports injuries).
- Vascular diseases, inflammatory processes of the walls of blood vessels (autoimmune inflammation of the branches of the aorta, arteritis).
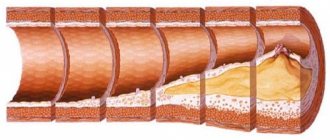
- Atherosclerosis (chronic blockage of blood vessels, deposition of cholesterol plaques), defects in the medial lining of blood vessels (aneurysms) and other vascular patency disorders (carotid artery stenosis, etc.).
- Diabetes mellitus type 2 (damage to small vessels of the brain).
- Hypertension, in which high blood pressure persists, resulting in disruption of the structure and basic functions of the arteries and heart.
- Phospholipid syndrome, which provokes the formation of blood clots in the veins and arteries, and other autoimmune pathologies (lupus erythematosus, Asherson syndrome, etc.).
- Damage (dissection) of arteries – dissection of the carotid and vertebral arteries.
- Thrombosis of blood vessels and veins (a pathology due to which a blood clot appears inside a vein or artery; the clot blocks and disrupts normal blood flow).
- Vertebral hernias, spondylosis and other pathological changes in the intervertebral discs compress the basilar or vertebral arteries, thereby impairing blood circulation.
Causes of cerebral aneurysms
The basis for the development of aneurysms is the congenital inferiority of the arterial walls. As age-related changes develop, degenerative processes occur in the walls of the aneurysm. It begins to gradually thin out, and the aneurysm increases in size. As a result of such changes, an aneurysm may rupture with the development of a life-threatening intracranial (intracranial) hemorrhage.
Arterial wall defects:
- muscle layer defects;
- damage to the internal elastic membrane of the wall;
- endothelial proliferation;
- damage to collagen fibers of the vessel;
- increasing rigidity of the artery wall and a decrease in its thickness.
Clinical picture and symptoms
“Brain” symptoms of vertebrobasilar insufficiency are associated with the blood supply to the brain, with dysfunction of the vertebral vertebral artery:
- the first and main symptom of vertebrobasilar syndrome is dizziness (sudden and short-term);
- possible fainting from frequent dizziness;
- instability when walking (the person suddenly swayed) is a symptom that specifies the disease; this is a state when a person has to concentrate, keep himself on his feet;
- nausea;
- frequent headaches (pressing, throbbing or dull);
- hearing impairment and the appearance of tinnitus, and the noise can be of different timbres; in advanced cases, tinnitus does not stop;
- there is some weakening of memory, attention becomes scattered and not concentrated;
- weakness, weakness, decreased performance, fatigue;
- irritability, causeless mood swings, crying and tantrums for no reason (more often in children);
- increased heartbeat (tachycardia), the patient feels feverish, and sweating increases;
- the appearance of unpleasant sensations in the throat (soreness, “lump in the throat”), the voice becomes hoarse;
- blurred vision is a fundamental symptom.
Important: it is not a decrease in visual acuity that occurs, but a difficulty in focusing vision, a feeling of blurriness of the surrounding world.
Epidemiology
According to Russian literature, the share of VBI among all cerebrovascular accidents is about 25-30% and about 70% of TIA. In 60-70% of cases, VBI is associated with damage to the extracranial parts of the VA. About 20-25% of all ischemic strokes develop in brain structures that receive blood supply from the arteries of the vertebrobasilar system. Atherosclerotic lesion (mainly of the extracranial part) of the VA is the cause of ischemic cerebrovascular accidents in the VBB in 20% of cases. The annual risk of stroke in patients with intracranial VA or OA lesions is 8 and 11%, respectively.
The prevalence of spondylogenic PA syndrome (spondylogenic VBN) among all neurological diseases is 3.8% and for osteochondrosis of the cervical spine - 30-42.5%. In case of injuries and damage to the cervical spine, according to foreign authors, structural and functional changes in the vertebral column occur in 19.7% - 33% of cases.
The main syndromes of acute VBD (corresponds to TIA in VBD according to domestic classifications):
- 1) the duration of characteristic subjective complaints and objectively detected neurological disorders does not exceed 24 hours, more often 5-30 minutes;
- 2) vestibular syndrome: dizziness of a predominantly systemic nature, nausea, vomiting, imbalance, spontaneous small-scale (horizontal, horizontal-rotatory, vertical) nystagmus;
- 3) cerebellar syndrome (homolateral to the side of the affected VA or bilateral): unsteadiness when standing and walking, impaired coordination in the limbs, intention tremor when performing coordination tests, handwriting impairment, muscle hypotonia in the limbs, large-scale horizontal nystagmus, muscle asynergies, adiadochokinesis;
- 4) visual disorders (symptoms depend on the location of ischemic damage to certain brain structures): decreased visual acuity and blurred vision, photopsia, loss of individual areas (quadrant hemianopsia) or halves (homonymous hemianopsia) of opposite visual fields, visual agnosia;
- 5) damage to the cranial nerves (symptoms depend on the location and volume of the ischemic focus in the brain stem, alternating syndromes are rare): diplopia, facial numbness, weakness of the facial muscles, hearing loss or tinnitus, dysarthria, dysphagia, dysphonia;
- 6) movement disorders (on the side opposite to vertebrobasilar ischemia): transient weakness in the arm and leg or in all extremities, revival of deep reflexes with the appearance of pathological flexion reflexes in the arms (Rossolimo et al.) and extensor reflexes in the legs (Babinsky et al. .), weakness and numbness in the arms due to ischemia of the superior medullary basin;
- 7) sensory disorders: numbness of the face (half or in the Zelder zones) on the side affected by VA, numbness in the limbs on the side opposite to vertebrobasilar ischemia;
 attacks of falling: dyscirculatory syncope, Unterharnscheidt syncope, drop attacks;
attacks of falling: dyscirculatory syncope, Unterharnscheidt syncope, drop attacks;- 9) paroxysmal short-term memory impairment;
- 10) psycho-emotional disorders: fear, anxiety, emotional lability, increased fatigue, sleep disturbances;
- 11) headache in the occipital or cervico-occipital region.
Clinical manifestations are “danger signs” indicating a high probability of stroke in the VSB:
- depression of consciousness;
- the duration of focal vertebrobasilar neurological symptoms is more than 6 hours;
- the presence of severe paresis/paralysis in the limbs;
- the presence of a distinct alternating brainstem syndrome (Weber, Millard-Gubler, Jackson, Wallenberg-Zakharchenko, etc.);
- severe systemic dizziness lasting more than 1 hour, aggravated by head and eye movements, with repeated vomiting;
- intense headache of cervical-occipital localization;
- horizontal paresis of gaze towards the focus of brainstem ischemia;
- acute Horner's syndrome (ptosis, miosis, enophthalmos) on the side of the focus of brainstem ischemia;
- stem hiccups;
- bulbar syndrome;
- disturbances of vital functions (cardiovascular and respiratory systems).
The main syndromes of chronic VBD (corresponds to dyscirculatory encephalopathy in VBD according to domestic classifications):
- 1) permanent manifestations of VBI - symptoms and syndromes that are observed for a long time, do not always depend on provoking factors and can be detected in a patient outside of an ischemic attack in the VBP;
- 2) dizziness of a non-systemic nature with imbalance and the absence of vestibulo-vegetative disorders (nausea, vomiting, etc.);
- 3) cerebellar syndrome: moderate static-locomotor ataxia with impaired standing and walking;
- 4) periodic moderate headache of occipital or cervico-occipital localization, often depending on the position of the head;
- 5) tinnitus with gradual hearing loss;
- 6) progressive decline in memory, often short-term;
- 7) frequent attacks of falling and fainting;
 pyramidal insufficiency in the limbs in the form of asymmetry and revitalization of deep reflexes;
pyramidal insufficiency in the limbs in the form of asymmetry and revitalization of deep reflexes;- 9) elements of pseudobulbar syndrome;
- 10) psycho-emotional and vegetative disorders.
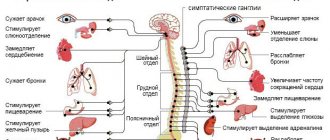
The main syndromes of spondylogenic VBN (corresponds to vertebral artery syndrome or posterior cervical sympathetic Barré-Lieu syndrome according to domestic classifications):
- 1) symptoms occur paroxysmally (less often permanently) after a sudden movement of the head (more often symptoms of VBI occur when hyperextension in the cervical spine, turning the head to the opposite side or homolateral lateral tilt of the head);
- 2) the appearance and reduction of all manifestations of VBI are clearly dependent on the position of the head and cervical spine;
- 3) positive De Klein's sign: the appearance or intensification of VBI symptoms after rotation and extension in the cervical spine;
- 4) sympathalgic headache of cervico-occipital localization with a characteristic hemicranic spread from the suboccipital zone to the frontotemporo-orbital region;
- 5) dizziness of various types, often combining systemic and non-systemic nature;
- 6) noise or hearing loss in one ear (on the side of compression or irritation of the PA);
- 7) transient visual disturbances: a feeling of sand in the eyes and fog in front of the eyes, photopsia, a transient decrease in visual acuity;
 cerebellar syndrome in the form of static-locomotor ataxia, depending on movements in the cervical spine;
cerebellar syndrome in the form of static-locomotor ataxia, depending on movements in the cervical spine;- 9) attacks of falling and fainting, occurring immediately after a sudden movement of the head;
- 10) suprasegmental and peripheral autonomic disorders in the cervical-collar region;
- 11) spondylogenic (cervicogenic) pain syndromes in the neck, shoulder and arm, caused by degenerative-dystrophic lesions of the cervical spine.
Diagnostics
It is difficult to make an accurate diagnosis of vertebrobasilar syndrome as a result of one examination, since the manifestations (symptoms) of each patient manifest themselves individually, and the diagnosed signs are often the causes of other diseases.
To differentiate symptoms, exclude other pathologies and make an accurate diagnosis, additional studies are prescribed to the patient:
- Doppler studies (vascular ultrasound), which studies the speed of blood flow through the arteries and checks for the presence of occlusions;
- Angiography of blood vessels is carried out in order to assess their condition (pathological narrowing or dilatation of blood vessels), for this purpose a special substance is injected into the vascular bed and at this moment pictures are taken, which makes it possible to study the diameter of the walls in the arteries; an x-ray of the spine is also prescribed (study of the general condition, clinical changes in the building);
- CT and MRI are prescribed to detect intervertebral hernia; MRI of the brain studies the condition of blood vessels, structure, sections of problem areas are taken, and the specifics of blood movement are examined; hyperventilation tests study disorders of the entire cardiovascular system;
- infrared thermography studies the condition of the necessary part of the body, assesses the general condition of the spine (based on thermal fields); REG of cerebral vessels studies the blood path (blood supply to the brain), the presence of blockage and damage to blood vessels;
- blood chemistry.
Next, we will consider in more detail vertebrobasilar insufficiency against the background of cervical osteochondrosis.
Symptoms of transient ischemic attack
The symptoms of this attack have vivid manifestations, but these manifestations have a short time period and by the time the ambulance team arrives, their severity is very often erased, so doctors make a preliminary diagnosis of a transient ischemic attack based on residual signs.
Symptoms of a transient attack with vertebrobasilar insufficiency:
- Problems with the speech apparatus due to numbness of the mouth, lips and tongue;
- Difficulty swallowing;
- Difficulty breathing (lack of air in the lungs) - shortness of breath;
- Attack on the lower extremities - sudden immobility, numbness of the extremities, inability to stand (fall), fainting;
- Loss of vision for a certain period of time;
- Loss of orientation on the ground;
- Inability to perceive human speech;
- Disorientation;
- Hand tremors;
- Convulsive contractions of the body and trembling;
- Trembling in the lower extremities;
- Limited movement of the limbs of the body;
- Numbness of a body part.
A transient attack with vertebrobasilar insufficiency provokes an ischemic stroke. What pills to take and what course of therapy after an attack?
Mexidol tablets give a good effect in treating a transient attack.
The course of drug therapy with this drug is up to 6 calendar weeks.
If vertebrobasilar insufficiency is treated incorrectly, or this pathology syndrome is not treated at all, after the first transient attack, even in a mild form, an ischemic stroke occurs within 5 calendar years and in most cases, the result of its development is death.
Classification according to ICD-10
According to the international classification of diseases, the disease is called vertebrobasilar arterial system syndrome.
ICD-10 code - G45.0
Vertebrobasilar syndrome is a deficiency in the supply of blood to the brain (trunk, cerebellum, occipital lobes), when blood flow in the vertebral and basilar arteries is disrupted and brain cells do not receive nutrition.
Reference. Anatomically, the vertebral arteries are located in the transverse processes of the cervical vertebrae, that is, in the bone canal. In the place where the vessel is thrown over the first vertebra (when the arteries are bent), it lies closely on it and can be pressed down.
Any abnormal position of the vertebrae, any bone growth in the joints of the spine, including deformation of the vertebral discs (cervical osteochondrosis) can irritate the vertebral artery, to which the artery reacts with spasm.
As a result, there is a disruption of blood flow in the vertebrobasilar region, where the cerebellum, medulla oblongata and certain structures of the occipital lobes of the brain (vision areas) are located.
Giant aneurysms of the cerebral arteries
Types of cerebral artery aneurysms:
- saccular aneurysm (can be giant)
- fusiform aneurysm (can be giant)
- dissecting aneurysm
- mycotic aneurysm
Classification of cerebral artery aneurysms by size:
- ≤6 mm – small aneurysm
- 7 to 12 mm - medium aneurysm
- 13 to 24 mm – large aneurysm
- ≥25 mm—giant aneurysm
Giant aneurysms of cerebral arteries with a diameter of more than 2.5 cm in patients have the same location as small aneurysms. Most often, giant aneurysms of the cerebral arteries are localized in the intracerebral part of the internal carotid artery, the bifurcation of the middle cerebral artery and at the apex of the basilar artery. Although it is possible for them to rupture, such aneurysms usually cause neurological symptoms as a result of compression of the brain as they increase in size.
The development of edema of brain tissue in the case of compression by a giant aneurysm can become irreversible and lead to severe compression of the brain and death of the patient. This outcome is especially likely if the giant aneurysm is located in the bifurcation of the middle cerebral artery. In this case, a neurosurgical operation aimed at decompressing the brain remains the only adequate treatment method. Such an operation for a giant aneurysm of the cerebral artery is technically difficult to perform and often leads to complications due to cerebral edema in the patient.
Thrombosis of the basilar artery/syndrome of the apex of the basilar artery.
Forms of the disease (acute and chronic)
As you know, all symptoms of the disease can be permanent or temporary.
In the acute form of vertebrobasilar insufficiency, temporary symptoms occur during transient ischemic attacks (acute cerebral circulatory disorders).
The duration of ischemic attacks is from 2 - 3 hours to 2 -3 days. The patient experiences pressing pain in the back of the head, dizziness, and discomfort in the cervical vertebrae.
Important: prolonged attacks cause a stroke.
In more favorable cases, an ischemic attack does not last long and is accompanied by microdamage to the nervous tissue.
Reference! The cause of transient ischemia can just be cervical osteochondrosis with compression (spasm and constriction), and as a consequence, developing vertebrobasilar syndrome.
In the chronic form of the disease, in addition to the presence of constant symptoms, there is an increase in exacerbations (frequent and prolonged ischemic attacks).
Important: lack of medical care and self-medication leads to the development of chronic vertebrobasilar insufficiency.
Forecast
With timely treatment, the disease recedes, and the symptoms of VBI no longer bother the patient. Sometimes, in the first stages, therapeutic exercises and a course of massages are enough. But cervical osteochondrosis, which is often the cause of VBI, cannot be treated completely. The disease accompanies a person throughout his life. But with the right lifestyle and regular exercise, the period of remission will last a very long time. If the disease is diagnosed in a timely manner in a child, the course of treatment may not even include medication, but be based only on physical therapy. If you ignore the signs of the disease, VBI will progress and eventually manifest itself in the form of ischemic attacks. The worst option is a stroke.
Consequences
At the initial stages, the disease does not manifest itself acutely; if symptoms are present, treatment is carried out on an outpatient basis, under regular medical supervision.
Attention! The presence of acute symptoms requires immediate hospitalization in the neurological department for diagnosis and treatment.
The consequences may be irreversible:
- drop attacks;
- speech and swallowing disorders;
- microstroke;
- stroke;
- encephalopathy;
- neurological deficit.
Find out what the dangers of CHS threaten our body here.
Basic principles of vascular health
The vertebrobasilar basin is not the only vascular conglomerate in which certain disorders can be observed that can lead to serious consequences. Any blood vessel plays its role in the body, and its blockage and narrowing of the lumen can cause pathology. That is why the prevention of vascular disorders should become one of the principles of maintaining one’s own health for every person. Unfortunately, many pathologies develop in the womb, and it is often very difficult to compensate for them with the real efforts of doctors, the patient and his relatives. But acquired vascular problems are the fault of the person himself, who neglects his health and does not listen to his body. A correct daily routine, a change in activities, a rational, nutritious diet, regular medical examinations, and careful attention to your health will help maintain the functionality of the cardiovascular system.
The vertebrobasilar basin is a vascular structure that supplies blood to the brain. It carries a huge load, providing oxygen and nutrients to many parts of the main organ. Disturbances in the blood flow of this system can cause pathological processes in many systems of the human body, deterioration of its vital functions and even death. To prevent this from happening, you need to listen to the signals that your body gives about impending problems.
Features in children and adolescents
Vertebrobasilar syndrome has recently become significantly younger due to congenital anomalies, trauma during childbirth (occurs in children 3–5 years old), a sedentary lifestyle, injuries, etc. (in children 7–14 years old).
Reference. The disease in childhood is easily treatable. Only in severe clinical cases is drug treatment and surgery performed. How to recognize signs of vertebrobasilar insufficiency in children?
- posture is disturbed;
- the child gets tired quickly, drowsiness, and performance decreases sharply;
- irritability appears, crying for no reason;
- dizziness, nausea, and frequent fainting are possible;
- reacts sharply to stuffiness and stale air;
- the child chooses the wrong position when sitting (sitting askew).
Important! If symptoms occur or after a recent injury to the spine or neck, you should immediately contact a neurologist for an initial evaluation. The sooner the cause is identified and a diagnosis is made, the more effective the treatment will be.
Is it possible to cure vertebrobasilar arterial system syndrome?
Vertebral pathology, how to treat? By identifying the symptoms, treatment is prescribed that is appropriate to the established diagnosis.
In case of a crisis of the acute stage of vertebrobasilar insufficiency, the patient is assigned a bed in a hospital, so that during the period of drug treatment the patient is constantly under the supervision of medical personnel. Monitoring the patient's condition will help prevent the consequences of this crisis - stroke.
Chronic circulatory disease, which occurs in a mild stage, should be treated on an outpatient basis.
For the treatment of vertebrobasilar insufficiency, drug treatment is used with physiotherapeutic treatment to strengthen the therapeutic effect.
The drug course of therapy is prescribed individually by the treating doctor, because there is no standard treatment in medicine for vertebral disorders.
Vertebral insufficiency cannot be treated with medications alone, so the complex treatment of this therapy includes physiotherapeutic techniques, treatment with traditional medicine, as well as therapeutic exercises (physical therapy).
In severe cases of pathology, surgical intervention is resorted to.
Drug treatment
Drugs prescribed for the treatment of vertebrobasilar insufficiency:
- A group of vasodilating medications (vasodilators). These medical products prevent occlusion. With these drugs, chronic vertebrobasilar insufficiency syndrome is treated in the spring or early autumn. The dosage is prescribed to a minimum, and according to the prescribed medication course regimen it is increased. If during therapy there is no positive effect on the body, the drug is replaced with another medication;
- A group of antiplatelet agents - reduce the coagulation ability of blood plasma. This group of drugs is used to reduce the risk of blood clots in the basilar vessel. A drug from the antiplatelet group is Aspirin, which for vertebrobasilar syndrome must be taken daily. For pathologies of the digestive tract, Aspirin is taken after eating, and it is forbidden to take it on an empty stomach. If Aspirin does not have a positive effect on the coagulation process in the body, then replace it with antiplatelet agents - Dipyridamole, or the drug Ticlopidine;
- A group of metabolic and neotropic drugs. These medications are intended to improve the functional abilities of all parts of the brain in cases of vertebrobasilar insufficiency. These drugs include: Piracetam, the drug Actovegin, the nootropic drug Cerebrolysin, the drug Semax;
- Group of antihypertensive drugs. This group of drugs is intended to control blood pressure index. In case of vertebrobasilar insufficiency, the blood pressure index is high, therefore, during drug therapy, this group of drugs is included in the list of mandatory ones;
- Drugs that relieve the main symptoms of this syndrome - painkillers, hypnotics;
- To relieve symptoms of severe dizziness, antidepressants are prescribed, as well as antiemetics if nausea caused by dizziness causes a vomiting reaction.
Symptoms of vertebrobasilar insufficiency
Surgical methods
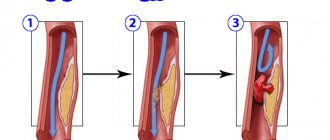
In severe stages of vertebrobasilar insufficiency, when drug therapy does not show any effect in treatment, a surgical treatment technique for the vertebrobasilar vascular system is used.
Methods of surgical correction of the vascular basilar system of the brain:
- The method of surgical correction is microdiscectomy of the spine. It means removing the hernia between the vertebrae and stabilizing the function of the spine. This operation falls into the category of neurosurgical intervention, and is performed by a doctor - a neurosurgeon;
- Laser correction technique for discs between vertebrae;
- The endarterectomy technique is a method of removing cholesterol atherosclerotic plaque inside an artery. This technique allows you to improve blood flow by removing plaque and increasing the lumen inside the artery;
- Angioplasty of the basilar artery. This technique allows you to insert a stand into the vertebral vessel, which prevents narrowing of this part of the artery. The dilation of the vessel ensures normal blood flow in the cerebral circulatory system;
- For arterial stenosis, the stenting technique is used - this is a method through puncture of the artery (aneurysmectomy) of the femur and a stand is inserted through the femoral vessel to the site of destruction of the aorta. When the stand arrives at the site of the defect, opening, it strengthens the wall of the affected part of the artery from the inside, and thereby prevents its rupture.
Stenting technique
Physiotherapy
For the treatment of vertebrobasilar insufficiency, there are several physical therapy techniques:
- Therapeutic restorative massage - improves blood flow to the brain. Massage is used on the entire spine, and is also used on certain areas of the body: thoracic massage on the spine, cervical massage, head massage to increase blood circulation in it;
- Exercise therapy is a physical therapy complex. With the systematic use of exercise therapy, you can improve your back posture. Also, exercises strengthen all parts of the spine and also relieve muscle spasms;
- Manual rehabilitation therapy for vertebrobasilar insufficiency - helps restore all functions of the spine, as well as the blood flow system;
- The hirudotherapy technique is a therapeutic process for vertebrobasilar insufficiency using leeches, helping to restore vascular disorders and pathologies. Hirudotherapy reduces blood pressure index;
- Treatment method: reflexology. This method involves the use of acupuncture in therapy. This method relieves muscle spasms, which improves blood supply to the brain. The use of this method is especially effective for osteochondrosis of the cervical spine;
- The method of physiotherapy for vertebrobasilar insufficiency is magnetic therapy;
- Wearing a corset around the neck during therapeutic courses. For injuries to the cervical vertebrae, this method is simply necessary for effective rehabilitation.
Treatment with folk remedies
Recipes from traditional healers help as an adjuvant in drug therapy for vertebrobasilar insufficiency. This traditional medicine technique can only enhance the therapeutic effect of treatment, but cannot replace drug therapy.
Folk remedies alone cannot cure the syndrome of the vertebrobasilar arterial system, and time lost in treatment will only aggravate the syndrome of vertebrobasilar insufficiency, which will lead to irreversible processes in the bloodstream system, as well as in parts of the brain.
This threatens an attack of ischemic stroke, which quite often ends in death.
To thin the blood and prevent blood clotting, the following medicinal plants are used that contain a high content of vitamin C:
- Lemon and lemon juice. Add 0.5 lemon juice to 2000 milliliters of water and drink this water. Drink in one day. The next day make a new drink;
- Orange and fresh orange. 200 milliliters per day will help prevent thrombosis;
- Currant berries. There are berries in any form - fresh, frozen, currant compote;
- Raspberries are not only an anticoagulant, but also an excellent plant for strengthening the immune system;
- Rose hip. Rose hips are the leader in the amount of vitamin C in them. A good anticoagulant, but it should not be taken in large quantities, because it has diuretic effects;
- Also, a good anticoagulant is kiwi, berries, grapes, fruits, and tomatoes;
- Garlic is a herb that will help thin the blood. Recipe: Grind 3 large heads of garlic in a blender (or using a meat grinder). Place in a glass jar and hide in a dark place for 3 calendar days. After this time, you need to strain this mixture and add lemon juice and natural honey to it. Everything is in equal proportions. Take 1 spoon before bedtime. A course of medication with this drug is 30 calendar days;
- Vasodilator recipe for medicinal herbs for vertebrobasilar insufficiency: fruits of the hawthorn plant (20.0 grams), pour 200.0 milliliters of boiling water and boil in a steam bath for 5 minutes. Leave covered for 30 minutes and, after filtering, take one spoon 20-30 minutes before meals. The course of therapy is at least 30 calendar days.
Gymnastics
Therapeutic gymnastics for vertebrobasilar insufficiency is done constantly, without multi-day courses. It can also be used as disease prevention. All movements are made smoothly and not through force. At a slow pace, even breathing.
Gymnastics exercises for basilar syndrome:
- Stand up straight, bring your toes together, work with your head - bend your head forward and you need to touch your chin to your chest. Stand in this position for 5-7 seconds and take the starting position. Repetition frequency - 10 times. Also perform head exercises on one side 10 times and on the other side 10 times;
- Head rotations can be done only after completing the first exercise. Slow rotations of the head are made in the direction of the clock hands, and then counterclockwise. This exercise is also done 10 times;
- Neck exercise: Pull your head forward. Stand in this position for no more than 5 seconds and return to the starting position. And so 10 times;
- Next is a set of exercises for the torso. Turn the body to the right side, then to the left. Each turn is practiced 10 times;
- At the end of the gymnastics complex, work with the legs. Raise your leg and stand on one leg for at least 5 seconds. The right and left legs are worked out alternately 10 times each.
Head rotation
Treatment
Attention! Only a doctor, after establishing a diagnosis, prescribes comprehensive treatment depending on the severity and course of the disease.
To treat vertebrobasilar syndrome against the background of cervical osteochondrosis, the specialist prescribes combination therapy (medicines and special procedures) strictly individually .
Medication
The disease involves problematic blood vessels; to prevent complications (strokes), antiplatelet agents are prescribed - substances that prevent the formation of microthrombi at the circular level. This is mainly low-dose aspirin.
Vasoactive agents with vasodilating properties. These drugs act on blood microcirculation, on the final part of the vascular bed. Drugs that stimulate metabolic processes in brain tissue, especially for older people, are metabolites and nootropics (glycine, piracetam, cerebrolysin, etc.).
For high blood pressure, special medications are prescribed - pressure regulators. Various antispasmodics (tantalum, ketorol, etc.) are used to relieve pain and spasms.
Antiemetics, sleeping pills or antidepressants are mandatory to relieve persistent symptoms.
Surgical methods
Modern medicine has interactive technologies in performing surgical operations:
Angioplasty – restoration of vascular plasticity. A special catheter is inserted into the narrowed vessel and a spacer is installed - a stent, which opens the vessel.
For atherosclerosis, endarterectomy is used (removal of cholesterol plaque from the artery itself), due to which blood flow in the vessels is restored. In some cases, the patient is prescribed microdiscectomy (correction of spinal discs by a neurosurgeon).
Folk remedies
Attention! All folk remedies are an addition to general treatment, and not a panacea for the disease!
- lemons, kiwi, currants and other fruits contain vitamin C, which thins the blood and improves blood circulation;
- extracting garlic with lemon and honey (in equal proportions) improves blood flow;
- horse chestnut reduces blood clotting;
- to reduce blood pressure, herbal decoctions are recommended: corn silk, rue, mint and valerian (in equal proportions); take 100 g before meals for a month;
- to dilate blood vessels, drink hawthorn tincture or a decoction of chamomile, St. John's wort, immortelle and birch buds (herbs in equal proportions).
Additional Methods
Important: before manual therapy, massage and other additional methods are prescribed, the patient must undergo an examination that excludes all contraindications to such procedures.
- acupressure of the muscles of the neck, spine, base of the skull improves blood flow, especially helps in the early development of the disease;
- therapeutic exercises relieve muscle spasms and strengthen the spine;
- manual therapy copes well with VBI against the background of cervical osteochondrosis, stabilizes the functioning of joints, tissues and vertebrae;
- hirudotherapy (leeches) helps in the treatment of blood vessels;
- reflexology (acupuncture, acupuncture) will effectively relieve spasms in the neck muscles;
- Using cervical collars to support the head makes it possible to “unload” the neck.
Treatment of cerebral aneurysm in Israel
- Bed rest is indicated.
- Monitoring blood pressure levels (optimal level 120–140 mmHg.
- Sedative and analgesic drugs are indicated: calcium antagonists (nimodipine), beta-blockers.
- Drugs that dilate blood vessels are used, which improve the rheological properties of blood, improving cerebral circulation.
The only radical treatment method is surgery, the purpose of which is to “switch off” the aneurysm from the blood circulation.
Surgery. The main method of treating arterial aneurysms is direct intracranial intervention with exposure of the damaged vessel and “switching off” the aneurysm from the circulation. Currently, the endovasal (intravascular) method is successfully used.
- One of the indispensable conditions for the least traumatic “switching off” is the use of microsurgical techniques, frontotemporal (pterional) access with resection (removal) of elements of the sphenoid bone.
- Endovascular “switching off” of aneurysms: special catheters are used with balloons filled with polymer material, which automatically separates from the catheter when a certain value is reached. Such operations are performed under fluoroscopy in real time. The balloon is inserted into the cavity of the aneurysm, clogs only its neck, and the aneurysm is “switched off” with the artery. You can thrombose the aneurysm cavity using a thin platinum wire, which is inserted through a catheter into its cavity, plugging the aneurysm cavity.
- Removal of hematomas. Intracranial hematomas resulting from aneurysm rupture are removed during aneurysm clipping, i.e. main operation.
Treatment at ASSUTA and HADASSA clinics
Are you interested in treatment in Israel?
The largest professional hospitals in Israel - Assuta in Tel Aviv and Hadassah in Jerusalem - offer a real opportunity to receive high-quality and specially selected treatment from excellent specialists at reasonable prices.
We help you find a solution to your health problems, and also provide complete information about the best Israeli doctors.
How much does treatment cost in Israel?
The price of treatment plays a decisive role in deciding whether to travel to Israel.
Each medical case is unique, so we provide our patients with estimated prices for diagnosis, rehabilitation and treatment in hospitals, and also talk about how to plan a trip and save money during treatment in Israel.
Our main goal is a high-quality medical program at an affordable price.
Content
Prevention
Gymnastics
Light exercises are recommended; even non-athletic and obese patients can do exercises without sudden movements.
Important: the effectiveness of gymnastics lies in its regularity.
It's better to practice in the morning. Then a contrast shower and a light massage are required. When performing exercises, you must breathe correctly - through your nose, breathing evenly.
Exercises are performed slowly and smoothly, these can be tilting the head to the right and left, rotating the head, stretching, raising arms and legs, turning the body, jumping. The ability to stand alternately on one leg with your eyes closed is considered effective.
For prevention , it is good to visit the pool and go swimming in the sea in the summer - this perfectly strengthens the spine and improves blood flow.
Right way of life
To reduce the risk of vertebrobasilar syndrome and osteochondrosis, you must, first of all, think about your health and give up (or at least minimize) everything harmful:
- fatty foods;
- alcohol;
- smoking;
- pickles and smoked meats;
- “junk” food - chips, crackers, fast food, etc.
You can get more complete information on proper nutrition here.
The following are considered mandatory actions:
- any movements - walking, fitness, exercises, etc.;
- walks in the open air;
- blood pressure control (especially after 40 years);
- weight stabilization (obesity is a huge risk factor);
- annual general examination (physical examination), observation by a doctor (for even minor symptoms).
Which doctor treats vertebrobasilar syndrome?
Therapy for vertebrobasilar syndrome and its insufficiency is considered by neurologists. If the syndrome has taken a complicated form of stroke, then treatment is developed by vascular surgeons.
Also, with the development of pathology, concomitant diseases arise, then specialized doctors are involved in therapy:
- Doctor otoneurologist;
- Cardiologist;
- Manual therapy specialist;
- Ophthalmologist;
- Physiotherapist.
1.2. Change in the number of vessels
1.2.1. Reducing the number of vessels
ICA agenesis: 0.01% Fig.11 , Fig.47 :
Around day 24 of embryogenesis, the ICA develops from the dorsal aorta and third arch. Subsequently, at approximately the 5th - 6th week, the base of the skull begins to take its shape. Thus, absence of ICA will result in absence of the carotid canal, identification of which is the most practical method in identifying this anomaly in a clinical setting. Typically, patients with ICA agenesis are asymptomatic due to well-developed collateral circulation through the ECA and vertebrobasilar system [2].
Aplasia of the A1 segment: 1-2%. Fig.12 and Fig.15 :
In this situation, both A2 segments are supplied by the existing A1 segment [2].
Azygos ACA: less than 1% Fig. 13 :
Both A1 segments form a common A2 segment, which supplies blood to both hemispheres[2].
Lack of Acom: 5% Fig.14 [2]:
Typically, the absence of the anterior communicating artery (Acom) is not easy to detect on time-of-flight MR angiography because the artery may be present but the flow signal is too weak to be visualized.
Lack of Pcom: 0.6% Fig.15 :
The posterior communicating artery (Pcom) is usually smaller than the P1 segment. Complete absence is rare [2].
Artery of Percheron: 4-11.5% Fig. 16 :
The thalamo-mesencephalic arterial supply can be divided into 3 types: type 1 is the most common, with perforating arteries on both sides arising from the P1 segments; type 2 , known as the artery of Percheron, arising from one of the P1 segments, supplying both sides; type 3 is an arch that connects both P1 segments and from which the perforating arteries arise [5].
1.2.2. Increase in the number of vessels
Incremental MCA: 2.7% Fig. 17 :
Literary definitions of accessory middle cerebral artery (MCA) and MCA duplication are quite dichotomous. In this paper, we use the definition of Teal et al., who limited the term “accessory MCA” to the branch arising from the anterior cerebral artery (ACA) and the term “duplicate MCA” to the artery arising from the distal segment of the ICA [6]. To distinguish an accessory MCA from a duplex one, the dominant vessel must be identified by carefully searching for the MCA bifurcation. Comparison with the contralateral side is also useful to find the level of ICA bifurcation [1].
Duplication: refers to two separate arteries that do not exhibit distal fusion. For example:
- MCA duplication: 0.2-2.9% Fig. 18 : MCA duplication is an artery that arises from the ICA and runs parallel to the main trunk of the MCA. This variant should not be confused with early branching of the MCA, in which a short single M1 segment is present. It should also not be confused with the anterior temporal branch, which often arises from the M1 segment.
- Acom doubling: 18% Fig. 19 [1].
- SCA doubling: 14% Fig. 12 [2].
Trifurcation:
- ACA trifurcation: 2-13% Fig. 20 : trifurcation refers to the presence of three A2 segments and is described by various names such as pericallosal triplex, arteria mediana corporis callosi and persistent primitive median artery of the corpus callosum [2]. Early origin of a frontopolar branch, for example from Acom, may appear as a third A2 segment.
MCA trifurcation: 12% Fig. 21 : The horizontal segment of the MCA is divided into superior and inferior trunks in approximately 78%. In 12% there is an additional (middle) trunk, this situation is called trifurcation, and the presence of more than 3 trunks, for example, quadrifurcation, is observed in approximately 10% Fig. 22 [2].
Fig. 11 Agenesis of the left ICA. TOF MRA (a), no signal from the flow in the left ICA. MIP CTA (c), CCA continues as ECA with no ICA. Bone window CT (b), absence of bony carotid canal on the left side. The normal carotid duct on the right side is marked with a red arrow for comparison.
Fig. 12 3D MRA, absence of A1 segment of ACA, both A2 segments extend from the contralateral side. Note the partial fetal PCA (white arrow), duplication of the superior cerebellar artery (blue arrow), and hypoplastic vertebral artery (red arrow) that terminates as the PICA.
Fig. 13 3D MRA, fusion of both A1 segments to form a single A2 segment (azygos ACA) (arrow).
Fig.14 3D TOF MRA, no Acom.
Fig. 15 3D TOF, absence of Pcom and A1 segment on one side. The significance of this option is that if the ICA is occluded on that side, there will be no possibility of collateralization through the circle of Willis. Incidental finding: aneurysm of the terminal portion of the contralateral ICA (arrow).
Fig. 16 MIP (a) and 3D TOF (b), type 2 thalamo-mesencephalic arterial supply (artery of Percheron) with a single arterial trunk (arrow) arising from the P1 segment, the branches of which supply blood to both sides.
Fig. 17 3D TOF, additional MCA (arrow) extending from the A1 segment.
Fig. 18 3D TOF of a duplicated MCA (red arrow) extending from the distal ICA. This artery should not be confused with the anterior temporal branch (white arrow), which is a common finding.
Fig. 19 3D TOF, Acom duplication (white arrows), proximal A2 segment fenestration (red arrow), A1 segment aplasia and complete fetal PCA (blue arrow).
Fig. 20 3D TOF, ACA trifurcation with three A2 segments (arrows), the third branch arises from Acom
Fig.21 3D TOF, MCA trifurcation with additional middle trunk.
Fig.22 3D TOF, MCA quadrifurcation.
Physiotherapy
With vertebrobasilar insufficiency, physical activity should not be high. It is advisable to study systematically according to a strict schedule, distributing the main loads in the morning hours. Physical exercise should be completed with water procedures to relax. You should not make sudden movements and become overtired. Proper nasal breathing is very important.
Examples of therapeutic exercises for VBI:
- The patient stands straight, legs together, feet do not turn out. The chin tries to reach the sternum. Freezes for a short time in this position. Brings his head back. 10 reps;
- From the same position, the head tilts in turn towards the shoulders, the shoulders remain in the same place. In each position there is freezing for a short time. 10 repetitions in each direction;
- Smooth head rotations, 10 repetitions in each direction;
- The patient reaches his crown towards the ceiling and freezes for 4-5 seconds. Relieves tension. 10 repetitions;
- Gradual movements of the head forward and back. 10 repetitions;
- The patient stands straight, raises his arms and joins them above his head, freezes for a short time and returns to the starting position. 10 repetitions;
- Turns the body in different directions with freezing for a short time. 10 repetitions;
- Raise the straight leg forward with freezing for 4-5 seconds. 10 repetitions on each side;
- Prolonged standing on 1st leg;
- Jumps with 180 degree turns (with sufficient preparation).
 attacks of falling: dyscirculatory syncope, Unterharnscheidt syncope, drop attacks;
attacks of falling: dyscirculatory syncope, Unterharnscheidt syncope, drop attacks;