How menopause affects heart rate
A high level of estrogen in a young woman provides protection - prevents the development of ischemia, promotes the absorption of vitamins and microelements that affect the functioning of the heart and nervous system. Deficiency of sex hormones is manifested in the following:
- Low-density cholesterol increases, which can be deposited on blood vessels in the form of plaques. According to research, its increase ranges from 10 to 15%, the overall level of this substance increases by 5–10%, and triglycerides in the blood increase by 11%. The risk of developing atherosclerosis and coronary heart disease increases.
- Violation of fat metabolism leads to their deposition in the body. Often after menopause, a woman develops obesity and then type II diabetes. Elevated glucose levels also increase the risk of heart and vascular disease.
- Due to changes in the water-salt balance and insufficient absorption of microelements (potassium, magnesium, calcium), arrhythmia appears.
- The menstrual cycle stops, the blood thickens, and the likelihood of blood clots increases.
- Deviations in the nervous regulation system, for which estrogens were previously responsible, lead to autonomic crises and vascular spasms, and increased blood pressure. The attacks are accompanied by pain in the head and chest, palpitations often develop during menopause, and the risk of stroke and heart attack increases.
95% of women who come to see me are over 45 years old. Complaints of heart pain in younger people are usually caused by vegetative-vascular dystonia and neuroses. Approximately 1% have myocarditis.
For more information about what VSD is and how to deal with it, watch the video at the link below.
Bradycardia during menopause – All about hypertension
Sinus bradycardia is a slow heart rate of less than 60 beats per minute. The source of such slow impulses, as normal, is the sinus node, while all structures of the heart operate in a normal mode, the sequence of work of the ventricles and atria is observed.
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Sinus bradycardia can occur in healthy people, such as professional athletes. Their resting pulse, even during the daytime, can slow down to 40, and sometimes to 30-35 beats per minute.
In addition, there is a so-called constitutional-hereditary, or familial, form of bradycardia, and the Bonaparte family always comes to mind.
Sinus bradycardia also occurs in a number of pathological conditions, such as decreased thyroid function (hypothyroidism) with an overdose of drugs such as beta blockers, digoxin, cordarone, etc.
If the heart rate becomes very low, then symptoms of hemodynamic disturbances appear: dizziness, weakness, pre-syncope and fainting. However, this situation occurs with serious damage to the sinus node and is a complication of the underlying disease.
In most people, sinus bradycardia in the range of 60-50 beats per minute does not cause changes in hemodynamics and thus does not give any symptoms.
In such cases, there is no need to use drugs that accelerate sinus rhythm; you just need to identify the cause of the slow heart rate and exclude other pathologies of the cardiovascular system and, first of all, sick sinus syndrome (SSNS).
Arrhythmia in women during menopause
- 1 Etiology of the problem 1.1 Symptoms of arrhythmia
- 1.2 What could be the consequences?
- 2.1 Medicines for arrhythmia
Hormonal age-related changes can cause the development of arrhythmia in women during menopause. Extrasystology is a type of arrhythmia that most often affects women during menopause.
Such problems are not uncommon at this age, so you need to know what symptoms accompany this deviation and how to help yourself if attacks are too frequent.
Etiology of the problem
Signs of extrasystology are considered to be sharp contractions of the heart muscles. This can be a single spasm or a series of attacks. The ventricles of the heart contract. Against the background of menopause, this condition is complicated by hot flashes, anxiety, rapid heartbeat and pulse, and lack of oxygen. The woman suffers from mood swings and sweats profusely.
on
Such attacks reduce the productivity of the heart muscle by a quarter, negatively affecting the functioning of the brain, kidneys, and inhibits the saturation of nutrients in the coronary vessels.
In addition, women may suffer from attacks of atrial fibrillation. Women who abuse coffee, cigarettes and alcohol and are exposed to excessive stress, lack of sleep and overwork are at risk. The initial stages of the disease do not have pronounced symptoms, but if a woman has frequent heart pain and menopause has occurred, arrhythmia increases the risk of complications.
Symptoms of arrhythmia
Menopause is manifested by palpitations, mood swings, hot flashes and an unreasonable feeling of anxiety.
- the pulse accelerates, the woman feels a beating in her temples and veins;
- dizziness, panic fear of death, loss of consciousness develops;
- the heart flutters;
- a woman complains of a lack of air, it seems to her that her lungs do not open;
- Heat spreads throughout the body, arms and legs tremble.
What could be the consequences?
Arrhythmia leads to heart rhythm disturbances. As a rule, it is not treated in a mild form, but if attacks are repeated, in the absence of treatment, heart failure develops and irreversible changes occur in the myocardium. The combination of these pathologies can aggravate the course of attacks and can one day lead to death.
Treatment of arrhythmia during menopause
Before prescribing a course of treatment, the doctor will determine the form of the disease and its location. Single attacks are most often not treated. If there is dysfunction in the endocrine or digestive system, the treatment course is prescribed based on the underlying disease, since arrhythmia is often its consequence.
If the cause of the arrhythmia is neurogenic factors, the person should consult a specialist to receive a prescription for sedatives or sedatives. If while taking medications the patient feels a deterioration in her general condition, it is recommended to interrupt treatment and consult a neurologist to correct the course of treatment.
If the general course is ineffective, the doctor may prescribe radiofrequency ablation.
During menopause, arrhythmia can be prevented and sometimes cured if you follow simple rules:
- Adjust your work and rest schedule. The working day is no more than 8 hours, with a proper break, and rest thoroughly.
- Follow a diet or nutritional therapy, avoid fried foods and fatty foods. Cholesterol increases the risk factor.
- Exercise regularly, but do not overload your body.
- Take all necessary medications and, if necessary, visit a psychotherapist.
OUR READERS RECOMMEND!
Our readers successfully use ReCardio to treat hypertension. Seeing how popular this product is, we decided to bring it to your attention. Read more here...
Medicines for arrhythmia
To normalize heart rate during menopause, it is important to begin treatment after consulting a doctor.
The treatment course is prescribed by the doctor after the patient has completed all the necessary examinations and tests. The specialist must understand the true cause of the development of the disease and only then make a decision on the need for therapy.
You cannot decide on your own which medications will be effective. At best, this will lead to a return of unwanted symptoms after stopping the medication.
In the worst case, uncontrolled medication use can cause complications of concomitant diseases and cause the woman’s premature death.
Classic prescription for arrhythmia:
- beta blockers to reduce the effects of stress hormones;
- antioxidants to improve the supply of nutrients to the coronary vessels;
- sedatives;
- sodium channel blockers.
Healer's Recipes
Before starting to use a traditional first aid kit, you should consult a doctor, since herbal mixtures can aggravate the course of concomitant diseases. Most often, herbs are prescribed as mild sedatives.
Infusions of mint, valerian, lemon balm, motherwort, and mixtures thereof are widely used. The dosage forms are very diverse - infusions, teas, decoctions. We must be aware that arrhythmia cannot be cured with herbs alone.
However, taking them regularly helps normalize sleep, improve the functioning of the gastrointestinal tract, relieve nervous tension, and help cope with stress.
Preventive recommendations
To avoid the development or occurrence of atherosclerotic changes, hormonal replacement therapy with estrogen-based drugs is sometimes prescribed.
If this therapy is contraindicated for any reason, it is possible to use herbal preparations containing phytoestrogens.
This treatment is considered an excellent prevention of stroke and myocardial infarction.
Measures to prevent arrhythmia during menopause differ little from recommendations for patients of other ages or men. Don't overeat or lead a sedentary lifestyle. It is recommended to add physical activity, give up bad habits, control blood pressure levels, and normalize weight. These simple methods will help you avoid most age-related changes.
on
Source: https://1gipertoniya.ru/lechenie/bradikardiya-pri-klimakse/
Symptoms of menopause
Intense hormonal changes and a decrease in the influence of estrogen are often accompanied by so-called hot flashes, irritability, depression, pressure fluctuations, arrhythmia and tachycardia.
The symptom complex in which women experience a feeling of heat, or a hot wave, is called a hot flash. This phenomenon is observed in the first months, and sometimes years after the cessation of regular menstruation. Signs appear with varying intensity, but usually boil down to the following sensations:
- a hot wave or heat suddenly appears in the upper part of the body (chest, head, neck), and can spread throughout the body;
- there is profuse sweating, increased heart rate, increased blood pressure;
- there is shortness of breath, a feeling of fear or severe weakness;
- at night this phenomenon is accompanied by insomnia;
- The frequency of attacks varies - from several times a day to 10-20 times a month.
As observations by scientists in many countries show, hot flashes after the cessation of menstruation are observed everywhere. But if in Europe 70% of women suffer from them, then in Asia - only 5-15%.
The causes of hot flashes are still not reliably known. There are theories that thermoregulation is disrupted due to constant fluctuations in the level of estrogens, which act as stimulants in a certain area of the hypothalamus. A disorder of the autonomic nervous system and a decrease in the activity of the adrenal cortex are also important. Factors that provoke hot flashes and palpitations during menopause:
- the predominance of fatty foods in the diet;
- alcohol, drug use and smoking;
- neurosis, stress;
- mental characteristics (tendency to mood swings).
Tachycardia
Irregular pulse and increased heart rate occur due to fluctuations in hormones. Estrogens cease to perform a protective function, so menopause and tachycardia are often associated. According to my observations, more often this occurs in the form of paroxysms, when after overexertion or even for no apparent reason, the pressure rises and the pulse reaches 100–130 beats. Less common are persistent increases in blood pressure and hypertension, as well as orthostatic manifestations - when changes occur during a sharp transition from a horizontal to a vertical position or vice versa. The entire set of changes that occur in the heart during hormonal changes is often called dishormonal cardiomyopathy by cardiologists.
If, against the background of the onset of menopause, you have pain and discomfort in the chest, we recommend reading the article “Pain in the heart during menopause.”
Rapid heartbeat during menopause: symptoms and treatment of tachycardia
You should not tolerate and ignore rapid heartbeat during menopause. Tachycardia is both a typical sign of menopause and a symptom of the development of a number of diseases.
Therefore, a woman must be examined by a cardiologist, gynecologist and the doctors recommended by them.
From this article you will learn: what are the causes of this phenomenon, what other accompanying symptoms may exist, how and when to treat such tachycardia or extrasystole, and how to behave during a sudden attack.
Causes of heart palpitations during menopause
In women after 40 years of age, reproductive function gradually fades away. The amount of estrogen in the body decreases. Its deficiency indirectly affects the increase in adrenaline synthesis, and this hormone directly affects the strength and speed of heart contractions.
An increase in its level can cause rapid heartbeat and other myocardial rhythm disturbances. Menopausal changes also affect metabolic processes, the functioning of the nervous and other systems of the body.
A decrease in the concentration of sex hormones in women over 40 years of age entails:
- changes in the biochemical composition of blood;
- deterioration of the rheological properties of blood;
- loss of elasticity of vascular walls;
- emotional instability;
- increase in body weight;
- deterioration in sleep quality.
Due to insufficiency of estrogen, a woman is more susceptible to stress, her heart beats, problems with cholesterol begin, the condition of arteries and veins worsens, the lumen of blood vessels narrows due to the accumulation of fatty plaques, and weight often increases. Increased blood viscosity, instability of mood and sleep, and other changes during menopause put strain on the heart muscle and arteries.
On a note! After 45 years, the risk of hypertension, progressive tachycardia, and other cardiovascular diseases increases. Their development may be hidden by the symptoms of menopause. Therefore, you need to be regularly examined by a cardiologist and other doctors.
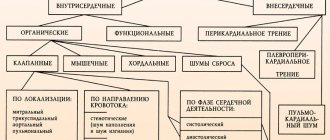
Possible types of heart rhythm disturbances
In women aged 40–65 years, the normal heart rate is considered to be 70–85 per minute. In a calm state, the heart beats smoothly, without shocks, interruptions or other disturbances. Before measuring your pulse, you need to sit for ten minutes, regain your breathing, and calm down.
Deviation of heart rate from the norm is a symptom of the development of one of the diseases:
| Type of heart rhythm disorder | Possible pathology | Brief description of the violation | Main symptoms |
| Hormonal tachycardia | Hyperfunction of the adrenal glands, thyroid and/or pancreas. | An increase in heart rate is caused by an excess of hormones (thyroid, glucagon, catecholamines). There are no organic myocardial lesions. | Chest pain, suffocation, dizziness, rapid heartbeat. |
| Sinus (nodal) tachycardia | Cardiac or respiratory failure, inflammation of myocardial tissue, hypoxia. | The rhythm of the sinus region remains unchanged, but the heart contracts more often. | Heart rate more than 90 beats/min, panic attack, fear of death, oxygen starvation, weakness. |
| Ischemic tachycardia | Myocardial ischemia (CHD). | An increase in heart rate is caused by the need to deliver oxygen to the tissues of the brain and internal organs. Complications include ventricular fibrillation. | Constant feeling of discomfort in the chest, headache, shortness of breath, rapid pulse. |
| Extrasystole | Heart attack, cardiosclerosis. | A rhythm disturbance of all myocardial structures or extrasystoles is characteristic. | “Frozen” heart, uneven beats, lack of air. Sweating and hot flashes often occur. |
| Paroxysmal tachycardia | Hypertensive crisis, cardiomyopathy, congenital myocardial defect. | At rest, the disorder is not diagnosed by ECG. During exercise, the heartbeat accelerates and the rhythm of contractions is maintained. | Sweating, weakness, chest discomfort, hot flashes, heart rate over 150 beats/min. |
| Bradycardia | Impaired transmission of impulses from the sinus node, poisoning, cardiomyopathy. | Heart rate below 60 beats/minute is typical. | Semi-fainting, difficulty breathing, drop in blood pressure, weakness, and sometimes aching pain in the heart area. |
| Atrial fibrillation | Complications of rheumatism, heart disease, hypertension. | Uneven atrial excitation/contraction. | Heart rate over 300 beats/min, interruptions in myocardial function, pain behind the sternum, pulse jumps chaotically. |
At night, a woman can experience up to 20 attacks of tachycardia and hot flashes. Doctors believe that the cause of their appearance is a hormonal imbalance combined with inadequate surges of adrenaline caused by malfunctions of the aging pituitary gland. For nighttime episodes of palpitations, you need to wipe your face and neck with a wet towel, drink water, take a reclining position and/or do breathing exercises.
Attention! If your heart is stabbing, you feel compression, pain in its area, or there is other discomfort behind the sternum, you should urgently be examined by a cardiologist. Against the background of chronically elevated heart rate, arrhythmia or bradycardia, myocardial diseases often develop.
Additional symptoms
Age-related changes in the sexual sphere last a long time - from 2 to 10 years. During this period, tachycardia can be supplemented by pressure surges, attacks of dizziness, shortness of breath, irritability, angina pain, arrhythmia, panic attacks, and malaise.
Hot flashes are considered the most common symptom of menopause. They occur during the premenopausal period and are caused by hormonal imbalance.
Signs of the tide:
- tachycardia (the heart “jumps out” of the chest);
- noise in ears;
- anxiety;
- feeling of heat in the heart, face, neck;
- intense sweating;
- redness of the skin in the upper torso, neck, head;
- pressure surge.
At high tide there is not enough air. When choking, a woman tries to unbutton her collar and take a deep breath. If, in addition to the listed signs, the face turns pale or the skin of the nasolabial triangle appears bluish, then these are symptoms of a heart attack. Immediate medical attention is needed here.
In what cases should you consult a doctor?
Irregular or stable heart rhythm disturbances indicate the development of diseases, so it is advisable for a woman to have an unscheduled examination by a cardiologist. Severe menopausal syndrome is also not normal and must be treated with the help of doctors.
Attention! An ambulance is urgently called in case of pain in the heart area, persistent attack of tachycardia or suffocation, sudden decrease/increase in blood pressure, lightheadedness, severe dizziness.
How can you get rid of tachycardia during menopause?
To normalize the rhythm of heart contractions, you need to provide your body with the most favorable conditions for functioning. First of all, you need to get rid of bad habits and control your emotions. These measures can reduce the severity of menopausal syndrome.
Here's what you need to do during an attack of tachycardia during menopause:
- Open the window.
- Unfasten the buttons at the collar and remove the bra.
- Sit in a comfortable position and relax.
- Breathe evenly and deeply.
- Calm down, drink some water.
If tachycardia does not go away on its own, the doctor prescribes medications. In case of a sharp deterioration in health against the background of an increased heart rate, call an ambulance.
Let's take a closer look at the treatment methods.
General recommendations
It is advisable to ventilate the room 2-3 times a day, walk in the fresh air more often, take a contrast shower, and perform breathing exercises. These measures increase the tone of the body, normalize the functioning of all systems and internal organs, strengthen the immune system, and saturate the cells with oxygen. They are able to support the heart during illness, age-related changes, stress, and prevent tachycardia.
Women during premenopause and menopause need to do gymnastics, yoga, swimming or other types of physical activity every day.
Regular exercise strengthens the heart, relieves psycho-emotional stress, and prevents weight gain.
In order not to provoke tachycardia, it is important to correctly select the degree of stress on the cardiovascular and musculoskeletal system. Instructors or physical therapy specialists will help you create a set of exercises.
To prevent tachycardia and menopausal syndrome, it is advisable for women to eat:
- nuts;
- pomegranate;
- seafood;
- legumes;
- bananas;
- fresh vegetables;
- other foods high in phytoestrogens, magnesium, and B vitamins.
It is recommended to eat small meals, drink at least 1 liter of water per day, and give up alcohol, strong tea and coffee.
To normalize sleep, prevent stress, and restore emotional stability, it is better to take relaxing baths in the evening. You can add herbal decoctions with valerian and pine needles to the water. You need to sleep at least 7 hours. You should not be physically overtired during the day, so you need to control the degree and duration of stress. In stressful situations, it is recommended to use stress balls.
It is important for women of menopausal age to carry out psychoprophylaxis. If your health worsens and tachycardia develops, you need to calm yourself down and voice what you will do now to relieve the attack. This method helps control emotions, prevents a panic attack, and has an indirect effect on stabilizing heart rate and blood pressure.
Hormone replacement therapy
Replacement therapy is used to eliminate severe menopausal syndrome due to estrogen deficiency. For women of menopausal age, it is advisable to regularly monitor hormonal status and heart function. Based on the test results, it is easier for the gynecologist to choose a medicine for tachycardia.
Here are the drugs most often prescribed for menopause:
- Remens.
- Cyclo Proginova.
- Climaxan.
- Trisequence.
- Angelique.
Hormone-containing drugs do not suppress the functions of the thyroid gland and genital organs. A moderate increase in low estrogen levels prevents attacks of tachycardia and reduces the severity of other manifestations of menopause.
Heart medications
With the onset of decline in reproductive function and postmenopause, doctors prescribe antiarrhythmic drugs to maintain a normal heartbeat.
Arrhythmia can be removed with drugs containing the following active ingredients:
- sotalol;
- amiodarone;
- magnesium orotate;
- esmolol;
- verapamil.
Antiarrhythmitics are used to relieve symptoms of tachycardia and other types of arrhythmias. Such medications do not treat cardiovascular disease or menopausal syndrome.
Tachycardia during menopause is also eliminated using drugs with an antiarrhythmic effect:
| Group of drugs | Direction of action | Name of drugs |
| Cardiselective β-blockers | Reduce heart rate in stressful situations | Concor, Bisoprolol |
| β-blockers | Reduces the frequency and force of heart contraction | Trazicore |
| Sodium channel antagonists | Slow down conduction in the atrium, lengthen the time of heartbeat | Quinidine, Aymalin |
| Calcium antagonists | Reduces the force of myocardial contractions, relieves spasms, slows the heartbeat | Amiodarone, Diltiazem |
| Metabolic means | Improves cellular metabolism and tissue respiration in the myocardium | Riboxin |
Attention! To normalize increased heart rate in women over 40 years of age, antiarrhythmic drugs are prescribed in long courses. During the period of their use, you need to consult a cardiologist once every 3 weeks and have an electrocardiogram done.
How and with what to treat
Depending on the causes and characteristics of the symptoms, I recommend a specific treatment regimen for arrhythmia and tachycardia during menopause in women. The important thing is that paroxysms can often be eliminated on your own, but this should be done correctly.
At home
You can try to cope with the attack yourself:
- calm down, sit down or lie down, take sedatives;
- provide access to air, ventilate the room, unbutton tight clothing;
- take a deep breath, hold your breath and then exhale slowly;
- press on the eyeballs and release, repeat 3-5 times;
- Place your face in cold water for a few seconds.
A doctor is called in the following cases:
- during an attack, pain occurs in the chest;
- dizziness, weakness, dark vision appears;
- pressure drops or rises sharply.
Arrhythmias during menopause can occur as a result of acute myocardial ischemia or cerebrovascular accident. Therefore, they should not be taken lightly.
The appearance of a strong heartbeat during menopause
Palpitations are another common complaint among patients over 40 years of age. This deviation can occur without pain, but it also instills fear for health. Tachycardia during menopause is not uncommon, and its causes also lie in changes in hormonal levels. Symptoms of tachycardia during menopause are:
- A sharp increase in the number of heart beats;
- Sudden dizziness;
- Feelings of anxiety, panic attacks;
- Shortness of breath, lack of air.
Read
Uterine bleeding during menopause
Most often, this symptomatology occurs against the background of hot flashes, increased physical activity or emotional arousal. If after a short rest the symptoms weaken, we can say that the disorder is caused by menopausal changes, but if the symptoms persist and blood pressure creeps up, you should definitely call the emergency room.
Important! Strong heartbeat during menopause can develop not only due to hormonal imbalance, but also as a result of vascular diseases, which necessarily require qualified treatment.
Case from practice
A 56-year-old woman came to the clinic with complaints of rapid heartbeat, arrhythmia, a feeling of lack of air and increased blood pressure during an attack. The ECG showed no signs of ischemia; some flattening of the T wave was observed on the posterior wall of the left ventricle, which can be considered as an indirect sign of hormonal imbalance or myocardial dystrophy.
I recommended: sedatives, Remens, Bisoprolal. To prevent attacks - a diet low in animal fats, consumption of predominantly protein and plant foods, consultation with a gynecologist-endocrinologist. After two weeks of treatment, the condition returned to normal, and attacks began to occur less frequently. Currently taking hormone replacement therapy.
Qualified help
To stop an attack, my colleagues and I usually recommend the following drugs:
- "Lidocaine."
- Antihypertensive drugs (beta blockers Atenolol and Carvedilol work best).
- Sedatives, and in case of severe anxiety - tranquilizers or antidepressants with serotonin reuptake.
Hormone replacement therapy provides good results in the treatment of tachycardia during menopause; many women around the world resort to it. It eliminates hot flashes, rhythm disturbances, protects against the risk of developing osteoporosis, and prevents cardiovascular diseases.
If you want to know everything about tachycardia, we recommend watching the video below at the link. Causes, symptoms, diagnosis and signs that it’s time to see a doctor - talk about all this in 7 minutes. Enjoy watching!
Expert advice
To prevent the development of tachycardia during menopause, I recommend doing the following:
- follow a diet that includes dairy and plant foods, seafood (Fig. 1);
- combine physical activity and rest;
- to walk outside;
- do yoga, meditation, relaxation practices;
- if necessary, take hormonal medications (only under the supervision of a specialist);
- From time to time take a course of vitamins and minerals.
During menopause, the risk of developing cardiovascular diseases is high. Get tested regularly (ECG, biochemical blood test to determine cholesterol, tonometry). Get rid of bad habits - smoking and drinking alcohol significantly aggravate the condition during hot flashes and lead to the development of heart attacks and strokes.
The following sources of information were used to prepare the material.
Menopause is often accompanied by arrhythmia - a violation of the uniform contraction of the heart. In most cases, the beats per minute increase, exceeding 90 times. Tachycardia during menopause, treatment with drugs that support the heart is required, although it appeared for a physiological reason. Therefore, supervision by a cardiologist is necessary to prevent cardiovascular diseases.
Increased heart rate during pregnancy
Tachycardia is also a common occurrence in women during pregnancy. The reasons for it are also primarily related to hormonal changes - during pregnancy, the level of progesterone increases, causing the heart to work at an accelerated pace. The clinical picture is aggravated by pathological conditions:
- anemia, hypovitaminosis;
- dehydration caused by manifestations of toxicosis;
- overweight;
- bad habits (smoking, alcohol);
- as well as the use of vasoconstrictor drugs (for example, nasal drops) and other reasons.
Leaving tachycardia unattended in women is dangerous, especially for the health of the unborn baby. Therefore, it is necessary to tell your doctor about the condition and undergo an examination.
Causes of tachycardia
The decline of reproductive function entails vegetative, hormonal, and metabolic changes in the body. This negatively affects your overall health. There is less estrogens in the blood, which contribute to the elasticity of blood vessels, the regulation of lipid metabolism, and the maintenance of normal cholesterol levels. Therefore, atherosclerotic plaques grow more intensively.
Reduced estrogen production impairs blood flow through the vessels, causing tachycardia.
Due to a lack of sex hormones, the amount of sodium ions in the lymph increases. An excess of a microelement retains fluid in the tissues, causing a deficiency of magnesium, calcium, potassium, which affects myocardial contraction. Due to the thickness and viscosity of the blood, tachycardia and tremor appear, blood pressure increases, and heart failure may develop.
Hormonal fluctuations also negatively affect a woman’s psycho-emotional state. She can experience attacks of fear for no reason, is often irritated, melancholy, and suffers from insomnia. Emotional instability is one of the physiological causes of tachycardia and heart pain during menopause.
During reproductive age, estrogens are produced in the ovaries. With the fading of their functioning, the production of sex hormones is done at the expense of adipose tissue, so in women after 40 years of age, body weight begins to increase. This process is necessary to quickly compensate for the lack of estrogen. But excess weight additionally puts stress on the heart and circulatory system, causing tachycardia.
Causes
Provoking factors for the development of tachycardia in women vary in different groups of patients, correlating with age and other characteristics. Often the only way to cure this pathology is to eliminate the cause of tachycardia.
In young women
What could be the causes of tachycardia in women under 40 years of age, when the level of estrogen in the hormonal background of the female body protects blood vessels from lipoproteins? It would seem that nature itself has taken care of women’s health, but complaints from young women about tachycardia are not uncommon. Cardiologists explain the situation by neurogenic causes, stress caused by:
- the workload of young specialists with responsible tasks in the workplace;
- abuse of coffee or tonic drinks;
- household chores (as a rule, women of this age have children who go to school and require special attention, time and effort from the mother);
- congenital lability of the nervous system, NCD, patients often describe situations where the trigger for an attack is the usual sound of an alarm clock in the morning.
There are frequent cases of the development of tachyarrhythmia due to the use of certain medications (drug or toxic tachycardia), infectious diseases and increased body temperature, hypovitaminosis and anemia, severe blood loss during heavy periods, and also reflexively - as a reaction to severe pain.
In patients over 45 years of age
The causes of tachycardia in women over 45 years of age are associated with the decline of reproductive function and hormonal changes. A gradual decrease in estrogen levels leads to symptoms of tachycardia in women during menopause:
- strong throbbing in the throat or chest;
- fatigue, weakness;
- shortness of breath;
- anxiety and panic attacks;
- feeling of additional heartbeats;
- dizziness;
- hot flashes.
Doctors call all these symptoms normal for women before menopause and suggest not to worry too much, saying that tachycardia and menopause are compatible conditions. At the same time, a decrease in estrogen levels in the blood leads to vasoconstriction and, as a result, an increase in blood pressure. Therefore, the causes of tachycardia in women after 50 years of age, as a rule, lie in existing cardiovascular diseases or endocrinological disorders.
At normal pressure
If tachycardia during menopause is explained by hormonal changes and a gradual decrease in blood pressure, then what makes the heart beat quickly at normal pressure? The causes of tachycardia in women with normal blood pressure can be any provoking factors of tachyarrhythmia, including neurogenic ones. A woman’s lifestyle and physical activity are also of considerable importance. For a normal heartbeat, these parameters must be normal:
- healthy, full sleep;
- sufficient but moderate physical activity;
- a balanced diet (to avoid anemia and hypovitaminosis).
If, against the background of normal blood pressure, tachycardia often makes itself felt, the most correct decision is to see a doctor and get examined.
For hypotension
Low blood pressure (hypotension) is usually perceived as a sluggish condition that does not cause any special problems to a person.
Women who are hypotensive, as a rule, adapt to this feature of their body and know how to quickly bring themselves to their senses. But sometimes a sharp drop in blood pressure suddenly begins to be accompanied by an accelerated heartbeat, which causes anxiety and even panic in a woman. The reasons for this behavior of the heart are understandable - due to sluggish blood circulation, it senses a lack of oxygen and tries to replenish it with an accelerated frequency of contractions.
For hypertension
The reasons for an accelerated heart rate with hypertension may be different in each specific case. Arterial hypertension itself in women develops mainly due to impaired metabolism (bad diet, excess fat and salt in food), a sedentary lifestyle, and hereditary diseases.
The causes of tachycardia in women against the background of hypertension are inextricably linked with the causes of this very underlying disease, as well as with other pathologies that can manifest themselves in a similar way.
Symptoms of tachycardia during menopause
At rest, in people aged 40-60 years, the norm is a pulse of 60-85 times per minute with an average blood pressure of 140/80. With tachycardia, these indicators increase significantly. When the heart is tense, a sufficient amount of oxygen and nutrients must be supplied to the tissues with the blood. This does not happen with a rapid heartbeat
With tachycardia there is no time for complete contraction, but with relaxation there is quality rest for the muscles. Therefore, palpitations may be accompanied by chest pain.
Symptoms of physiological tachycardia:
- pulsation in the veins of the neck, temples;
- dizziness;
- panic attack;
- loss of balance;
- lack of air (shortness of breath);
- noisy inhalations and exhalations;
- hot flashes in the head, neck, chest;
- feeling of stuffiness;
- increased sweating;
- trembling of fingers;
- skin redness;
- frequent heartbeat.
Tachycardia may be accompanied by attacks of extrasystole. It feels as if the heart was suddenly pushed several times, followed by extraordinary contractions, and then it seems to freeze. The attack suddenly begins and ends, but the heartbeat remains rapid for a long time, and weakness appears throughout the body. Extrasystoles can disrupt blood circulation in the brain, causing a stroke, so such arrhythmia must be treated.
First aid for tachycardia
At the initial signs, the woman is recommended to take medicine (Valocordin, Valerian, etc.). Then you need to open a window or window - with tachycardia you need more fresh air to increase the oxygen level in the room. A panic attack can be eliminated with breathing exercises.
You need to breathe deeply and simulate a strong cough. This will simultaneously fill the lungs with air and calm the tachycardia faster. You can also wash or lie down and place a cold compress on your forehead.
Treatment of tachycardia during menopause
If a violation of the rhythm of contractions is associated with menopause, the doctor prescribes cardiac medications, hormonal, sedatives, multivitamin and mineral complexes. With their help, the work of the heart is corrected, provoking factors are eliminated - lack of estrogen, nervous excitability, vascular inconductivity, etc.
Tachycardia is classified into sinus, ventricular and atrial. Only a doctor can determine the type, so all medications, including those that eliminate arrhythmic contractions, are taken as prescribed by a cardiologist. Correctly selected medicine corresponding to the type of arrhythmia increases its effectiveness, accelerates the effect of substances, and reduces heartbeat. During menopause, treatment with other medications is prescribed when pathology is identified.
Sedatives prevent the acute manifestation of menopausal symptoms, against which tachycardia occurs - nervousness, attacks of fear, hot flashes, and so on:
The following herbal preparations are used for this purpose:
- Inoclim;
- Persen;
- Remens;
- motherwort, mint, hawthorn, valerian.
To regulate blood pressure and heart rate and restore its contractile function, doctors prescribe beta blockers:
- Atenolol;
- Propranolol;
- Concor (Bisoprolol);
- Metoprolol;
- Esmolol;
- Egilok.
The third generation of selective beta1 blockers includes Nebivolol and Carvedilol. The drugs eliminate tachycardia.
At the same time, agents with antioxidants are attributed to improve myocardial function and coronary circulation:
- Vitrum-forte Q10;
- Omacor;
- Essentiale;
- Vitrum cardio;
- Asparkam and other drugs.
Restores the rhythm of heart contractions, blood flow, blood pressure and Na-channel blocker - Flecainide, Allapinin, Quinidine, Ritmodan, Ritmonorm, Mexarithm, Novocainomide and other means.
Complex therapy for tachycardia
It is recommended to donate blood more often to monitor hormone levels. The analysis is useful when a doctor selects estrogen-containing herbal products. If tachycardia during menopause occurs due to a lack of this substance in the body, sage, boron uterus, shepherd's purse, lemon balm, rosemary and other herbal remedies are prescribed.
For tachycardia, daily walks in the fresh air and exercise therapy are recommended. Physical activity has a beneficial effect on the nervous system, and light exercise strengthens the heart and blood vessels.
To reduce cholesterol levels and normalize blood pressure, you must adhere to the Pevzner diet (table No. 10). Consumption of vegetable and berry juices, rosehip and hawthorn decoction accelerates the treatment of tachycardia. Excluded from the diet:
- yeast dough products;
- fat meat;
- salo;
- mayonnaise;
- coffee.
It is recommended to replace sugar with honey and reduce the consumption of sweets. They eat more fresh fruits, raw vegetables, and cereals. Products should contain many B vitamins, folic and ascorbic acid, potassium, magnesium, zinc, calcium and other beneficial substances.
What happens in the body during menopause?
Without exaggeration, we can say that a woman’s entire life from birth to old age is under the influence of the hormone estrogen. He is responsible for ensuring that the woman fulfills her main purpose - to give birth to children. It makes the figure feminine, the skin beautiful and elastic, the nerves strong, and the heart resilient. Statistics show that in active working age, it is mainly men who suffer from heart problems. And all because the female body has a powerful protector - estrogen. It regulates fat metabolism, water-salt balance and most other important processes.
And then there comes a time when its production begins to decline. This entails many negative consequences, for which a woman needs to be prepared. One of them is tachycardia during menopause. The entire menopausal period is divided into three stages:
- Premenopause, when disruptions occur in the menstrual cycle. This is a difficult period for a woman; she begins to feel ailments associated with disruption of many organs and systems, whose work depends on estrogen and its components.
- Menopause. At this time, menstruation has already stopped, but the restructuring of the body continues.
- Postmenopause is a state in which a woman will remain for the rest of her life. If she goes through the previous two correctly (following the doctor’s advice), then with the end of menopause the painful syndromes will also end.
The quality of life during the first two stages largely depends on the individual characteristics of the body, the strength and duration of various syndromes, and on how attentive the woman is to herself.
Causes of tachycardia during menopause
Estrogens affect the functioning of almost all organs and systems of the female body - nervous, digestive, endocrine and cardiovascular. They regulate blood pressure, prevent cholesterol levels from rising, and maintain the elasticity and firmness of the vascular wall. Estrogen affects calcium metabolism and maintains water-salt balance. Under the influence of this hormone, the blood retains its fluid properties. One of the first signs of the onset of premenopause is often tachycardia - rapid heartbeat. This heart begins to respond to changes in hormonal levels.
| Changes | What's happening | Consequences |
| Violation of water-salt balance | The entry of sodium ions into the lymph, an increase in blood volume and viscosity, a decrease in magnesium and potassium content | Fluid retention in the body leading to edema, increased risk of blood clots, increased stress on the heart |
| Lipid metabolism disorder | Weight gain, fat deposits in the abdomen and shoulder girdle, increased cholesterol levels | Increased load on the heart, deterioration of the conductivity of the arteries due to the formation of plaques in them. |
| Increased production of catecholamines - adrenaline, norepinephrine and dopamine. | Depression, frequent mood swings, increased irritability | Increased blood pressure, increased heart rate, arrhythmia |
| Increased thyroid function – hyperthyroidism | Increased release of thyroid hormones into the blood | Changes in psycho-emotional state, heart rhythm disturbances |
These are not all the reasons why tachycardia may appear during menopause. It can be provoked by existing diseases that are aggravated by menopause - diabetes, hypertension, heart pathologies and others. Increasing the load on the heart forces it to work with greater intensity, which leads to accelerated wear and tear of the heart muscle.
Prevention
There is a set of measures aimed at reducing the symptoms of the pathology. Normalization of heart rate during menopause is facilitated by proper nutrition and an active lifestyle.
A woman is advised:
- Actively engage in physical exercise, but do not overload the body. Jogging in the mornings and evenings is suitable.
- Avoid being in stuffy rooms. It is especially important to ventilate the room before going to bed. Drafts should be avoided, as a weakened body is more susceptible to colds.
- Do not participate in quarrels and conflicts. Stressful situations have a negative impact on the heart muscle and can trigger a heart attack. For depression, it is recommended to visit a psychologist's office.
- Regularly conduct examinations and take tests. This will prevent unexpected attacks of arrhythmia.
- Maintain a work-rest schedule
- Pay attention to proper sleep.
Bad habits such as drinking alcohol and smoking are excluded. It is useful to take baths with a calming effect. They add oils or extracts of valerian, sage and pine needles.
Symptoms of tachycardia
Tachycardia, which is often accompanied by arrhythmia, is manifested by the following symptoms:
- noticeable increase in heart rate;
- panic attack - a growing feeling of fear of loss of consciousness and even death;
- dizziness;
- feeling of chest compression;
- dyspnea.
Heart contractions alternate with periods of rest of the heart muscle. During tachycardia, these periods of relaxation are sharply reduced due to the need to pump the required amount of blood to continuously supply tissues and organs with nutrition. This increased load on the heart additionally gives the following symptoms:
- chest pain;
- pulsation in temples;
- hot flashes - a feeling of heat that covers the head, neck and chest;
- trembling in hands;
- loss of balance;
- feeling of stuffiness;
- sweating;
- redness of the skin.
Symptoms occur during moments of emotional outbursts and physical stress. They do not pose a serious health risk and usually go away after a short rest. However, prolonged tachycardia, which is also accompanied by an increase in blood pressure, requires emergency care.
Tachycardia is often accompanied by arrhythmia. Its symptoms are interruptions in the work of the heart of the extrasystolic type. They are felt like a jolt of the heart, followed by its fading, and then with an uneven beating. Sometimes women describe this condition as follows: “the heart is tumbling.” After the rhythm is restored (this usually happens within a few minutes), the heart continues to beat faster for some time.
What is cardiac tachycardia and why is it dangerous?
Tachycardia, or tachyarrhythmia, is a violation of the heartbeat rhythm in which the heart rate (HR) is accelerated, but their rhythm is not disturbed, that is, the intervals between heartbeats are reduced, but they are equal to each other. The most typical and safe acceleration of heart rate occurs in any healthy organism under physical or emotional stress or the influence of other external factors - coffee, alcoholic drinks, etc. This tachyarrhythmia is called physiological or functional, it is transient in nature (the normal heart rate is restored within 10 –15 minutes) and is not dangerous.
If signs of cardiac tachycardia in women appear in a calm state or normal heartbeat is not restored for a long time, there is reason to think. The dangers of cardiac tachycardia in women can be judged from the list of consequences of this condition:
- prolonged oxygen starvation of the most important organs;
- ischemia of the heart and brain;
- ventricular fibrillation.
Complications of pathological tachyarrhythmia can cause heart failure, heart attack, severe forms of coronary artery disease, and even cardiac arrest in women.
First aid
Symptoms of tachycardia during menopause are quite painful. To alleviate the condition, you need to provide yourself with first aid. To do this, you should always have sedatives on hand - Valocardin, Corvalol or regular valerian. They will quickly relieve a panic attack and normalize your heart rate. An influx of fresh air and a cold compress on the forehead will help. Another way to restore breathing is to imitate a strong cough. It will help your lungs fill with air and calm your heartbeat.
Treatment of tachycardia during menopause
Her future health depends on how carefully and attentively a woman treats her condition during menopause. To ensure that tachycardia does not leave consequences in the form of coronary heart disease, hypertension and other cardiac disorders, it must be treated. Only a doctor can prescribe therapy after determining the type of tachycardia. If frequent attacks of extrasystole (arrhythmia) are observed, they can lead to the development of paroxysmal tachycardia, and this is a very dangerous syndrome. The best results come from comprehensive treatment.
Any foods that irritate the body - spicy foods, caffeine, alcohol - should be excluded from the diet. Nutritionists talk about seven “magic” foods that “save” women during menopause:
- Whole grain breads. Cereals contain large quantities of phytoestrogens, which will help maintain hormonal levels, which will have a positive effect on heart function.
- Soy is an indispensable component of the diet for a woman over 40 years of age. In addition to phytoestrogens, it is rich in minerals and vitamins.
- Dairy products that contain calcium. During menopause, the female body suffers huge losses of this mineral.
- Fish is a source of polyunsaturated fatty acids, vitamin D, microelements and protein.
- Vegetables as a source of vitamins. Particularly useful are tomatoes (cherry), zucchini, cabbage, pumpkin, green (green) beans, broccoli, beets and herbs.
- Fruits, like vegetables, will replenish your reserves of vitamins and minerals. Apples strengthen the heart muscle and lower cholesterol levels. Pears are a source of antioxidants, strawberries prevent heart and vascular diseases. The same applies equally to cherries, raspberries and black currants.
- And finally, the universal medicine is honey.
Of course, in addition to these seven types of products, the diet should include meat and cereals.
Medicines and physical activity
To eliminate nervousness and panic attacks, sedatives are prescribed. They help reduce hot flashes, the most unpleasant symptom of menopause. Such drugs include Klimara, Divina, Proginova, Corvalol and others.
To normalize blood pressure and heart rate, beta blockers are used: Atenolol, Propranolol, Egilok, Concor. It is impossible to manage treatment without vitamin complexes. Vitrum Cardio, Essentiale, Asparkam, Omakor and others are designed especially for women during menopause. Among antiarrhythmic drugs, Novocainamide, Ritmonorm, Allapinin and some other drugs that block sodium channels are in demand.
Among traditional medicine, the most effective are infusions and decoctions of sage, boron uterus, lemon balm, rosemary, and shepherd's purse.
Moderate physical activity and physical therapy are absolutely indispensable for maintaining heart health. They strengthen the heart muscle, improve blood circulation and, of course, lift your mood.
If you are constantly bothered by the symptoms of tachycardia, be sure to get it treated. After all, menopause is not a reason to put an end to a woman’s life. Fortunately, perestroika syndromes end sooner or later, new meanings appear in life, and it again becomes beautiful and amazing.
Treatment
If rapid heartbeat during menopause bothers you for a long time, then you need to treat this phenomenon. It is worth contacting a therapist, who will then send you to a highly specialized doctor.
Treatment in the future will depend entirely on the diagnosis made by the doctor. If tachycardia as a separate disease is confirmed, then you will be prescribed calcium antagonists, cardiac glycosides and other serious drugs. If left untreated, tachycardia will lead to heart failure.
However, such a diagnosis is rarely made, because palpitations are a symptom of menopause. It is treated, like all other manifestations of menopausal syndrome, with hormonal therapy. You can also take phytoestrogens, but this should only be done for mild symptoms. Treatment of palpitations during menopause should be comprehensive.
Medicines
Table of blood pressure categories.
Symptoms that occur during menopause require attention and prompt treatment. To prevent any of the manifestations from becoming a complication or becoming chronic, you need to seek medical help in a timely manner. What to do with tachycardia during menopause?
Medicines such as sedatives, beta blockers, antioxidants, and sodium channel blockers will help.
Doctors usually prescribe the following drugs: Concor, Remens, Mexicor, Allapinin, Preductal. You can supplement the treatment with vitamins A, B, C, E.
Indications for such drugs usually include arterial hypertension, coronary heart disease, angina pectoris and chronic heart failure.
The drugs have many contraindications, so it is very important to follow your doctor’s recommendations.
Traditional methods
If the symptoms do not bother you too much, and you do not want to see a doctor yet, you can try treatment with traditional methods. This will also be a good help in standard treatment.
Mainly used for this purpose are herbs such as sage, hawthorn, rosemary, blackberry, St. John's wort, motherwort, and wormwood.
They are used both internally and as bath preparations. However, there is no need to take hot baths; limit them to warm water. Deep baths are also not recommended.
Let's give some examples of recipes.
The first one looks like this. Brew cucumber seeds, valerian roots, hawthorn, mint herb, rowan fruits and raspberries in 500 ml of water. You need to insist in a thermos for two hours. Then drink half a glass 3 or 4 times a day.
Let's move on to the second method. In 500 ml of alcohol you need to infuse 50 g of knotweed, yarrow, lemon balm and shepherd's purse. Leave for a week in a dark room. Take 10-15 drops three times a day.
There is another way. You need to infuse a glass of boiling water and a tablespoon of crushed cyanosis root. Next you need to drink a third of a glass 3 times a day.
You can also prepare a decoction with sage and flax seeds. Add a spoonful of the mixture to a glass of water and leave for 15 or 20 minutes. Next you need to strain and drink.
Melissa and mint teas will also help.
If you have intolerance to certain components, consult your doctor. This is what the treatment of tachycardia during menopause looks like.