What is essential hypertension
Essential hypertension was previously called hypertension, a new name was given with the transition to the International Classification of Diseases standard. A diagnosis of essential hypertension means that the patient suffers from chronic high blood pressure. The pathology today is diagnosed in 90% of the population and, if measures are not taken in a timely manner, can have serious consequences.
Measurement indicators are always recorded in the form of two numbers, the first of which is the upper pressure level, and the second is the lower pressure level. With essential hypertension, either an increase in only the first value or a simultaneous increase in both values can be observed. A deviation is considered to be an increase in points:
- for the top indicator above 140;
- for the lower value more than 90.
In the human body, even a deviation of pressure values by 10 points means the beginning of negative changes. If the indicators are significantly exceeded, there is a high risk of hypertensive crisis and stroke, which is an extremely dangerous development of events.
Stages of development
During essential hypertension, I distinguish the following stages:
- Stage I: blood pressure does not increase more than 140-160/90-99 mm. rt. Art., is asymptomatic, the risk of stroke or heart failure is about 5%, 15% of patients may develop cardiovascular pathologies;
- Stage III: blood pressure rises above 180/115-120 mm. rt. Art., the patient shows signs of atherosclerosis, hypertensive crises become more frequent, the risk of complications is 30%.
Causes of the disease
Essential hypertension is called primary, for the patient this means the absence of obvious pathologies of internal organs, a minor disturbance in the functioning of the cardiovascular system. Today, the disease is classified as a multifactorial pathology, that is, health problems can be caused by many circumstances.
Potential causes of blood pressure problems include:
- hypertension due to hereditary predisposition;
- excess body weight above normal;
- smoking, frequent drinking of alcohol;
- lack of physical activity;
- improper diet, excessive consumption of salt, coffee, strong tea;
- lack of water;
- deficiency of magnesium and vitamins;
- frequent stressful and emotional disturbances.
Previously, essential hypertension in the predominant number of cases was diagnosed in elderly people. In the last decade, arterial hypertension has been diagnosed in young patients. Doctors talk about the great influence of disrupted metabolic processes in the body due to the improper lifestyle and nutrition of modern people.
Disease prognosis
We already understand what essential hypertension is, but what is the prognosis for this disease? To predict the possible outcome of the disease, scientists have developed a special risk scale. It calculated the percentage of complications and mortality from the disease during the first ten years.
- Insignificant risk, which is less than five percent.
- Low risk, ranging from five to fifteen percent.
- Moderate risk, from fifteen to twenty percent.
- High risk, twenty to thirty percent.
- Very high risk, thirty percent or more.
When observing a patient, the doctor must determine which risk group he belongs to; this can be done using the following criteria:
- Risk factors, yes or no.
- High pressure level.
- Presence of affected organs.
For example, if the patient’s internal organs are not affected, the pressure readings are not too high and there are no complications, then the prognosis will be favorable. But if the patient has damaged internal organs, has had a stroke or heart attack, and has constant high blood pressure, then the risk of cardiac arrest is very high. In other words, this is a very poor prognosis.
How does essential hypertension manifest?
The first signs of pathological disorders are shown by the numbers on the tonometer, which at first may deviate slightly upward from the norm. Patients do not pay due attention to minor symptoms due to the fact that they do not cause discomfort in everyday life. Psychosomatics is expressed in the appearance of headaches, dizziness, and lack of strength. Periodically, tinnitus and a darkening effect in the eyes may appear.
Such symptoms are episodic in nature and appear as a result of increased physical activity, anxiety and stress, or non-compliance with nutritional rules.
Over time, such symptoms become more noticeable, and the frequency of their occurrence increases. Headaches become stronger as systolic pressure increases and can be prolonged. The use of analgesic drugs ceases to provide the proper therapeutic effect.
In the second stage, symptoms of blood pressure problems become obvious:
- feeling of anxiety;
- red complexion;
- increased degree of sweating;
- headache, sensation of pulsation in the temples;
- nausea, vomiting;
- feeling of pressure in the chest, shortness of breath;
- the effect of “flies”, darkening;
- swelling.
Long-term excess pressure is fraught with a decrease in visual acuity. The person becomes apathetic, and previously unusual irritability may appear.
Symptoms
Essential hypertension can occur for a long time without any obvious signs. Therefore, it is imperative to pay attention to how often the following symptoms bother you:
- weakness accompanied by nausea and chills;
- dizziness, headaches;
- “stars” and “spots” before the eyes;
- cardiopalmus.
If such symptoms bother you too often, and they are not associated with other diseases, then this is a reason to consult a doctor. If you measure your blood pressure when they appear and it turns out to be high, it is likely that hypertension is developing.
Stages and causes of hypertension development
The classification of the stages of development of essential hypertension is based on the criterion of the boundaries of pressure indicators. In total, it is customary to distinguish 3 types, each of which has its own symptoms and the nature of its effect on the human body.
The latter is characterized by very high blood pressure levels, which is accompanied by negative pathological disturbances in the functioning of vital systems and a decrease in the effect of medications.
The degree of violations that have occurred is determined by measuring indicators; the number of recorded cases is of great importance. What is important is not the one-time fact of recording a deviation from the norm, but the repetition of the event 3 or 4 times a month.
Primary
Primary essential hypertension occurs in 90% of people and is often detected during a medical examination. It is characterized by a slight excess of the following indicators:
- upper no more than 159;
- the bottom ranges from 90 to 99.
With a slight deviation from the norm, the patient does not feel much discomfort and for a long period may not be aware of the occurrence of a problem. The diagnosis is made based on the tonometer points. The first stage is associated with a high risk of various complications due to diabetes or problems with the functioning of internal organs. The high-risk group includes patients with a history of ischemic attacks or a stroke.
Second stage
The stage of progressive hypertension is characterized by a significant increase in blood pressure. Diagnosis criteria:
- upper 160-179;
- lower 100-109.
At stage 2, changes in the vascular walls are diagnosed and signs of hypertrophic changes in the myocardium appear. Such changes are not capable of significantly affecting the condition and functioning of internal organs. If self-treatment is attempted or there is no timely treatment, a person’s condition may worsen, and the disease may progress to the final stage, which is dangerous to health.
Third stage
The stage is considered the most severe, and the indicators are 180/110 or higher. Due to the risk of pathological changes, it is often called the “stage of organ change,” since with a high blood pressure value, pathological changes in the structure of blood vessels and organs are clearly visible. The totality of the nature of the lesion and existing risk factors determines the likelihood of complications.
Treatment of primary hypertension
Treatment of hypertension begins with lifestyle modification and non-drug therapy.
The lifestyle for a patient with essential hypertension consists of the following measures: – Quitting smoking and alcohol abuse. It has been proven that the poisons contained in cigarettes and alcohol, when entering the body, have a toxic effect on the inner wall of blood vessels and cause damage to it. – Limit the consumption of table salt in food to 5 – 6 g per day. Salt, namely the sodium it contains, promotes fluid retention in the body, increasing the volume of blood in the vessels. - Proper nutrition. You should exclude “harmful” foods from your diet - fast food, spicy, smoked, hot, salty, fatty and fried foods. It is recommended to increase the content of fresh vegetables and fruits, dairy products, cereals and cereal products in food. For proper functioning of the whole body, food must be taken at the same time, about 4 – 6 times a day. Choosing low-calorie foods without artificial additives, coupled with a diet, will also help normalize blood cholesterol levels and reduce excess weight in obesity. - Proper organization of physical activity. To maintain a good state of the cardiovascular system, it is not necessary to engage in weightlifting, extreme sports or spend every evening in the gym. Morning and evening exercises with a set of simple exercises will be quite sufficient if the patient currently has no contraindications to this, and the doctor does not recommend strict bed rest.
Systematic performance of the following gymnastics is an excellent remedy for high blood pressure:
Non-drug treatment methods include: - auto-training - psychotherapy - acupuncture - herbal medicine (valerian, St. John's wort, sage, motherwort, mint, lemon balm and other herbs) - electrosleep
These methods can help with the initial stage of hypertension, when there is no damage to target organs or complications. Otherwise, medications are prescribed, one or a combination of them:
– ACE inhibitors (angiotensin-converting enzyme) and ARA II (angiotensin II receptor antagonists) not only act on the main mechanism of sodium and fluid retention in the body, but also protect target organs from the further harmful effects of high blood pressure. Drugs – lysigamma, prestans, fosicard, zocardis, hartil; Lorista, valsartan, etc. - betta - adrenergic blockers and calcium antagonists reduce the tone of peripheral vessels, reducing vascular resistance. Drugs – betaloc, recardium, nebilet; amlodipine, felodipine, etc. - diuretics remove excess fluid from the body. Drugs - diuver, arifon, indapamide, veroshpiron, hydrochlorothiazide, etc. - other groups of drugs for angina pectoris, heart failure, heart attack and other complications - nitrates, antiplatelet agents, statins.
It is preferable to start treatment with non-drug methods (at stage I); if there is no effect, prescribe one drug at a low dose. At the stage of target organ damage, with the development of complications, with a persistent increase in pressure to significant levels, it is recommended to take a combination of drugs. Combined drugs – Exforge (valsartan + amlodipine), Lozap plus (hydrochlorothiazide + losartan), Aritel plus (hydrochlorothiazide + bisoprolol) and many others.
Consequences of all stages of essential hypertension
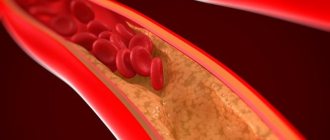
Constant excess pressure forces the vessels to take the blow, which leads to deformation of the walls due to a constant attempt to increase the lumen for better blood passage. The load leads to irreversible consequences, the walls of blood vessels lose their elasticity and become dense, and lose the ability to quickly respond to changes in blood pressure. The heart, in an attempt to adapt to the need to work more, begins to change, the walls of the myocardium thicken. The pathology carries a very high risk of heart attack.
Over time, the patient develops angina, heart rhythm disturbances, gastric insufficiency and pulmonary edema. Changes are expressed in a person’s image and behavior, he becomes apathetic, is often depressed, and problems with memory and vision appear.
Etiology
Genetic predisposition
Twin studies suggest that heredity plays a major role in the etiology of hypertension.
Approximately 50% of patients have a hereditary predisposition to EG, caused by mutations in the genes of angiotensinogen, angiotensin II receptors, angiotensin-converting enzyme, renin, aldosterone synthetase, β-subunit of amiloride-sensitive sodium channels of the renal epithelium, etc.
Other factors
- Obesity increases the risk of hypertension fivefold. More than 85% of cases of hypertension occur in patients with a body mass index of more than 25.
- Smoking: reduces endothelium-dependent vasodilation, increases the activity of the sympathetic nervous system, and is a risk factor for the development of coronary heart disease.
- Excessive consumption of table salt: excess sodium increases the volume of circulating blood, causes swelling of the walls of arterioles, and increases the sensitivity of the vascular wall to vasoconstrictor factors.
- Insufficient intake of calcium and magnesium, trace elements and vitamins from water and food.
- Alcohol abuse.
- Low physical activity, physical inactivity.
- Psycho-emotional stressful situations.
- Replication of pathogenic microorganisms, especially increasing under various stress conditions, associated with isolated systolic hypertension and systolic-diastolic hypertension, replication of cytomegalovirus. This was observed in Russia, then in the mid-Atlantic states of the United States, Kazakh, and Chinese populations, although in US populations as a whole the data have not yet been sufficiently studied. This is due to the fact that increased expression of angiotensin II and renin in the blood and tissues, certainly observed as a result of exposure to cytomegalovirus, does not always lead to the development of arterial hypertension, since, for example, people of the African race on average have very high levels of angiotensin II and renin, their hypertension is indeed more severe, but in Cuba, Puerto Rico and especially in Africa, the prevalence of hypertension is usually much lower than among US whites.
- The occurrence of arterial hypertension depends on the person’s age. At a young age, mainly secondary hypertension - due to smoking, alcoholism, drugs, vertebrobasilar insufficiency, congenital anomalies of blood vessels, kidneys, adrenal glands, pituitary gland. In middle age - due to excess body weight, neuropsychic stress or past diseases with damage to the heart, blood vessels, and kidneys. And after the age of 40, this is almost always the result of sclerotic vascular lesions;
- Gestational hypertension is hypertension that some women develop during pregnancy. It usually goes away after childbirth, but sometimes the disease can be prolonged, and women who have had hypertension in pregnancy, as well as preeclampsia and eclampsia, which are also accompanied by hypertension, are more likely to develop hypertension in subsequent years.
- Among Africans living in industrial societies, essential hypertension is four times more common than among whites, develops more quickly and leads to greater mortality, and the prevalence, but not the severity, of essential hypertension among them decreases with a decrease in overt or covert racism.
Diagnostics
Timely identification of problems with blood pressure largely determines the success of treatment and prevents the disease from developing into more complex forms. The patient can independently record pressure readings measured using a conventional tonometer over a certain period. To identify the frequency of pressure surges and the reasons for their occurrence, the doctor prescribes daily blood pressure monitoring - the ABPM method. A special device is installed on the patient’s body, which will automatically measure and record blood pressure when the time for readings is taken.
To make a diagnosis, the following types of studies are prescribed:
- urine and blood analysis;
- physical diagnosis, that is, listening to the heart rhythm, identifying murmurs;
- ECG;
- fundus examination;
- Ultrasound of internal organs.
Based on the examinations performed, the doctor makes a diagnosis and determines the course of therapy.
renovascular hypertension
See also in other dictionaries:
ARTERIAL VASORENAL HYPERTENSION - honey. Vasorenal arterial hypertension (AH) is symptomatic (secondary) hypertension caused by ischemia of the kidney(s) due to occlusion of the renal arteries. Frequency. 0.5% of all hypertension. Etiology • Atherosclerosis of the renal arteries (accounts for 60 70% ... ... Directory of diseases
vasorenal hypertension - (h. vasorenalis; lat. vas vessel + ren kidney; syn. G. renovascular) arterial G. caused by impaired blood supply to the kidneys, usually due to narrowing of one or both renal arteries ... Big medical dictionary
ARTERIAL RENOPARENCYMATOUS HYPERTENSION - med. Renoparenchymal arterial hypertension (AH) is symptomatic (secondary) hypertension caused by congenital or acquired kidney disease. Etiology • Bilateral kidney damage (glomerulonephritis, diabetic nephropathy, ... ... Disease reference
Pulmonary hypertension - Pulmonary circulation ... Wikipedia
Arterial hypertension - This article should be Wikified. Please format it according to the rules for formatting articles... Wikipedia
Essential hypertension - (hypertension, EG, hypertension, primary hypertension) a form of arterial hypertension, a chronic disease, the main clinical sign of which is a prolonged and persistent increase in blood pressure (hypertension), diagnosis ... ... Wikipedia
Essential arterial hypertension - Essential hypertension (hypertension) is a disease caused by many different factors; it is based on a genetic polygenic structural defect that causes high activity of pressor mechanisms... ... Wikipedia
ARTERIAL HYPERTENSION - characterized by a persistent increase in blood pressure above the physiological norm (140/90 mm Hg). In the vast majority of cases, the cause of the increase in blood pressure cannot be established, and they talk about essential hypertension, or essential hypertension... ... Encyclopedic Dictionary of Psychology and Pedagogy
High blood pressure - Arterial hypertension Thickening of the arterial wall due to hypertension. Microphotograph of ICD 10 I10. I...Wikipedia
Treatment of essential hypertension
To treat problems with blood pressure, complex therapy is prescribed, the content of which is determined only by a doctor. Drug treatment in the form of prescribing medications with a blood pressure lowering effect is of primary importance. In some cases, it is enough to eliminate the root cause to normalize the indicators. Often this situation is associated with stressful circumstances, and after the nervous system is brought back to normal, blood pressure stabilizes.
Non-drug
Non-drug methods of influencing blood pressure involve using the capabilities of several tools at once. This therapy involves changes in the following areas of the patient's life:
- adjusting the diet, constant adherence to the diet;
- limiting physical activity, reducing psycho-emotional overload;
- conducting psychotherapy courses;
- completing a course of physiotherapy;
- herbal medicine.
The diet for essential hypertension prohibits the abuse of salt, the amount of which should not exceed 6 g. Smoking, alcohol, fatty foods, tea and coffee are excluded from the patient’s life. If there is excessive body weight, forces are directed towards weight loss, as a result of which pressure stabilization will be observed at the same time.
Recommended exercises include walking and swimming.
Heavy sports and heavy lifting are prohibited for patients with essential hypertension.
Medication
To make a correct diagnosis and the extent of damage to internal organs, it is important to seek medical help in a timely manner. Even if you have elevated blood pressure, you cannot carry out a course of self-treatment using the analogy method, and start using medications prescribed to a relative or friend.
Therapy of essential hypertension involves a course of taking the following types of prescriptions:
- diuretics;
- drugs of the ACE inhibitor group;
- potassium and angiotensin antagonists.
Each group of drugs has a number of contraindications, so prescriptions should be made by a doctor in accordance with the examination results and the presence of concomitant diseases. In most cases, monotherapy with an ACE inhibitor is prescribed at the first stage, and other medications are gradually introduced to enhance effectiveness.
Treatment of primary hypertension
If the symptoms of essential or renovascular hypertension are confirmed by laboratory and instrumental studies, then treatment is required. The following drugs are used to lower blood pressure:
- beta-blockers (Concor, Niperten, Coronal, Metocard, Egilok, Metoprolol Organica, Betalok);
- ACE inhibitors (Prestarium, Perineva, Captopril-STI, Captopril Sandoz, Capoten, Perindopril-SZ);
- angioplatelet agents (Thrombo ACC, Aspirin Cardio, Cardiomagnyl);
- statins (in the presence of atherosclerosis or dyslipidemia);
- sedatives.
If diabetes is detected, medications are prescribed to lower blood glucose levels. Diuretics are often included in the treatment regimen. When selecting medications, the following are taken into account:
- their tolerability by humans;
- duration of therapeutic effect;
- degree of blood pressure reduction;
- person's age;
- indications and contraindications.
It is necessary to begin treatment with small doses of medication. If the drug is ineffective, it is replaced. ACE inhibitors are most in demand for arterial hypertension. They disrupt the formation of an enzyme that promotes the synthesis of angiotensin. The latter narrows the blood vessels. These drugs act on the renin-angiotensin and kallikrein-kinin systems.
Kapoten has a powerful effect. It is often used to lower blood pressure during a hypertensive crisis. Often, for high blood pressure, several medications are prescribed at once. Calcium channel blockers are often used. These include Verapamil, Amlotop and Nefidipine. They have the following effect:
- dilate blood vessels;
- reduce blood pressure;
- change heart rate.
In advanced cases, it may be necessary to prescribe cardiac glycosides. They are indicated for developed vascular insufficiency. Antiplatelet agents are used to prevent thrombosis, heart attack and stroke.
Other treatments
It is necessary to know not only the causes of the development of essential arterial hypertension, what it is, but also non-drug methods of therapy. These include:
- therapeutic nutrition;
- lifestyle changes;
- smoking cessation;
- refusal of alcoholic products;
- stress relief (relaxation);
- head massage;
- increased physical activity;
- dosing of physical activity.
It is important to eliminate negative environmental factors (noise, vibration). To reduce the frequency of attacks, you need to eliminate stress. To do this, it is necessary to avoid emotional experiences. Psychotherapy is provided if necessary. Proper organization of the work regime is of great importance. During tiring work, it is necessary to take breaks.
If possible, it is better to go to bed before 11 pm. It is recommended to walk for half an hour every day. If there is a lipid metabolism disorder, all patients should adhere to proper nutrition. The diet involves limiting salt intake to 4-5 g per day, avoiding alcohol and fatty foods, and enriching the diet with sources of vitamins and minerals (sea fish, walnuts, fruits, vegetables, berries, herbs).
Sometimes refractory hypertension develops. Its peculiarity is resistance to therapy. Essential hypertension may require hospitalization. It is indicated for a developed crisis that cannot be eliminated by medications. Patients are hospitalized in case of heart attack, pulmonary edema and stroke. If secondary hypertension is detected, then the underlying disease (glomerulonephritis) must be treated.
Possible complications
Serious health problems in patients can be observed already at the second stage of the disease, up to a hypertensive crisis. With the development of pathology, damage occurs to internal organs, which in medicine are usually called targets. Possible complications of the following organs:
- brain;
- eyes;
- heart muscle;
- kidneys;
- blood vessels.
As a result of poor blood supply, brain nutrition processes are disrupted. The result is headaches and tinnitus. Over time, the processes of memory and mental activity are disrupted. With increased pressure, the risk of microinfarctions, strokes, and degeneration of brain tissue increases significantly.
An increase in pressure levels directly affects the retina and its tissues. As a result of its detachment, vision is impaired. Increased stress on the heart leads to a hypertrophied state of the myocardium, the muscle is depleted as a result of malnutrition. As a result, the risk of heart attack and coronary death increases significantly. Against the background of high blood pressure, renal failure often occurs, which aggravates the patient's condition. The danger to the circulatory system is associated with atherosclerosis.
Primary arterial hypertension
Essential arterial hypertension is a chronic non-infectious disease characterized by a persistent increase in systolic and diastolic blood pressure with repeated measurements. The optimal pressure is 120/80 mmHg. This pathology manifests itself mainly at the age of 30-45 years. Recently, cases of hypertension in young people have become more frequent.
This disease is directly related to a person’s lifestyle. Very often, essential arterial hypertension is combined with atherosclerosis. This disease should not be confused with secondary arterial hypertension. The latter is caused by somatic pathology (kidney diseases, pheochromocytoma). An example is renovascular hypertension.
Degrees and stages of hypertension
Hypertension has a benign or malignant course. In the latter case, this pathology progresses rapidly and is accompanied by frequent crises. There are 3 degrees of this disease. Primary arterial hypertension of the 1st degree is not always clearly manifested. Blood pressure ranges from 140/90 to 159/99 mm Hg. Art.
With primary hypertension of the 2nd degree, the pressure ranges from 160/100 to 179/109 mm Hg. Art. The most dangerous is grade 3. With it, blood pressure reaches enormous values (up to 180/110 mm Hg or more). The classification takes into account both systolic and diastolic pressure. The first occurs at the moment of contraction of the heart, and the second - in diastole.
Depending on the degree of dysfunction of target organs, 3 stages of hypertension are distinguished. In the early stages of hypertension, there are no symptoms. Stage 2 is different in that changes in organs are detected. This may include thickening of the heart chambers and damage to the retina. With grade 3 hypertension, both objective and subjective signs of pathology are revealed. There is a high risk of stroke and heart attack.
Why does blood pressure rise
The reasons for the development of essential (primary) hypertension are varied. The following etiological factors are of greatest importance:
- bad heredity;
- unbalanced diet;
- smoking;
- alcohol addiction;
- drug use;
- atherosclerosis;
- overweight;
- diabetes;
- physical inactivity;
- lipid metabolism disorder.
Attacks of increased blood pressure are provoked by stress, drinking alcohol, dietary errors, and a decrease in atmospheric pressure. Essential and renovascular arterial hypertension are caused by the following disorders:
- water and sodium retention;
- activation of the sympathetic-adrenal system;
- increased release of neurohormones;
- increased vascular tone.
Irreversible changes occur when arterial walls thicken and peripheral resistance is high. Over time, sclerosis develops. This leads to disruption of the blood supply to organs (heart, brain, kidneys, eyes). Conditions such as encephalopathy, nephrosclerosis and heart damage develop.
The primary risk factor for the development of hypertension is poor nutrition.
It has been established that daily consumption of table salt in amounts of more than 5 g increases the risk of developing the disease.
A dangerous condition is dyslipidemia. Increased levels of total cholesterol and LDL often lead to atherosclerosis. With it, the lumen of blood vessels narrows. The smaller it is, the higher the blood pressure.
Dyslipidemia is more often detected in people whose diet regularly contains foods rich in animal fats and simple carbohydrates. You cannot eat fatty meat, fish, mayonnaise, eggs, lard, sour cream, cream, fatty cottage cheese, sausages and butter every day. An artery can become clogged with plaque if the diet lacks vitamins and polyunsaturated acids.
Essential hypertension is more often detected in people with increased mental stress. The risk group includes programmers, chess players, and accountants. Working at night has a bad effect on blood vessels. There is a high probability of developing hypertension during prolonged work in conditions of noise and exposure to vibration.
How does high blood pressure manifest?
Symptoms of essential hypertension depend on the level of blood pressure, stage and condition of vital organs. In the early stages of the disease, the following signs are observed:
- transient headache;
- dizziness;
- noise in ears;
- sensation of pulsation;
- sleep disorder;
- fast fatiguability;
- decreased performance;
- feeling of heartbeat;
- nausea.
Neurological disorders come to the fore, since the brain most strongly feels the lack of oxygen. The most common complaint is headache. It is localized in the occipital or frontal lobe. Floaters often appear before the eyes. In the later stages, when the heart function is disrupted, shortness of breath appears.
Initially, it occurs only during physical activity. Then shortness of breath bothers me constantly. She appears alone. The main manifestation of hypertension is a persistent increase in blood pressure. During an attack, the following symptoms are observed:
- dyspnea;
- facial redness;
- sweating;
- feeling of numbness in the limbs;
- dull pain in the chest.
Possible tremor. Late manifestations of essential hypertension include edema. Most often they are localized on the arms. Possible puffiness of the face and swelling of the eyelids. This symptom may indicate kidney involvement. Cardiac edema is symmetrical, worse in the evening, cold, more persistent. With kidney pathology, they are warm, disappear quickly and are most often localized on the face. When the retinal arteries narrow, visual acuity decreases.
What does arterial hypertension lead to?
Vasorenal and essential hypertension are dangerous due to their complications. The disease is characterized by a long course. Complications develop over several years. The most common consequences of hypertension are:
- crises;
- acute cerebrovascular accident (ACVA);
- myocardial infarction;
- acute and chronic heart failure;
- nephrosclerosis (wrinkling of the kidneys);
- aortic aneurysm;
- cardiac asthma;
- pulmonary edema;
- retinal detachment;
- blindness;
- uremia (severe renal failure);
- angina pectoris.
Primary arterial hypertension progresses. If drug treatment is not carried out, the risk of complications increases. Most often, this pathology is accompanied by crises. This is a condition in which blood pressure rises briefly and sharply. Triggering factors include stress, climate change, and alcohol intake.
The attack lasts from several hours to a day or more. During a crisis, the blood supply to the brain deteriorates significantly. This is fraught with a stroke. A hypertensive crisis is manifested by fear, tachycardia, a feeling of lack of oxygen, weakness, and sweating. The patient's face turns red. Nausea, vomiting and dizziness are common.
Speech difficulties and sensory disturbances may occur. In severe cases, chest pain appears similar to angina pectoris. This condition requires emergency assistance. Crises occur at any stage of the disease. Without help, a heart attack or stroke is possible. The latter is associated with acute ischemia. The most unfavorable prognosis is observed with malignant hypertension.
Prevention
In the absence of a genetic predisposition, the occurrence of essential hypertension can be prevented. To reduce the risk of developing hypertension, doctors recommend adhering to the following rules:
- dose physical activity;
- avoid stressful situations and respond adequately to what is happening;
- lifestyle changes;
- normalize your diet;
- Use medications only as prescribed by a doctor.
Doctors recommend periodically measuring blood pressure, which will allow timely detection of the problem. Walking in the fresh air, the daily duration of which should be at least 1.5 hours, is considered a good prevention of the disease. If there is a slight deviation of pressure readings from the norm, jogging at a slow pace is acceptable; gymnastics and yoga have a good effect of improving well-being.
Treatment of primary hypertension
An important point in treatment is reducing the risk of cardiovascular complications. This requires not only drug therapy, but also lifestyle changes.
Drug treatment
Conservative therapy can only be prescribed by a specialist. He will take into account all the important features of the pathology, which will allow him to select the optimal drugs for a particular case from a huge selection of medications.
Drug treatment can be performed in different ways. Monotherapy involves the use of one drug. Combination treatment means the simultaneous use of several medications.
For essential hypertension, the following groups of drugs can be used:
- Angiotensin-converting enzyme inhibitors. A decrease in blood pressure is ensured by exposure in several directions at once.
- Angiotensin receptor blockers. The action of such drugs involves vasodilation.
- β-blockers. These medications work in several ways, dilating blood vessels, slowing the heartbeat and normalizing the heart rate.
- Calcium antagonists.
- Diuretics. There are several groups of such drugs. Thiazide agents promote the excretion of sodium with water. Potassium-sparing medications have a weak diuretic effect, but they retain potassium in the body. The most powerful action is found in loop drugs.
- According to indications, they resort to an α-blocker. They belong to centrally acting medications. This therapy reduces the activity of the nervous system, causing blood pressure levels to decrease. The action of the drugs is based on vasodilation and a decrease in total cholesterol in the blood.
During a hypertensive crisis, the patient needs rest and bed rest. In a medical facility, they usually resort to Enalaprilat, Nitroglycerin, β-blockers, diuretics, and antipsychotics.
ethnoscience
Alternative medicine is also appropriate in the treatment of essential hypertension. You can use the following folk recipes:
- Red pine cones. An infusion is prepared from them. The raw materials must be washed and dried, then filled into a glass container. It must be filled to the top with alcohol or vodka. Leave in the dark for 15-20 days. The finished product should have a dark red color. It is necessary to take a teaspoon half an hour before meals three times a day.
- Rosehip infusion. 100 grams of dried berries need to be brewed with a liter of boiling water and infused in a thermos. The finished product can be drunk instead of tea, but in moderation, as it has a fixing effect.
- Viburnum infusion. You need to pour 1.5 cups of berries with a liter of boiling water and leave in a glass container for 5 hours. Then strain the mixture by rubbing the berries through a sieve. Add a glass of honey. Take a third of a glass three times a day for 2 weeks before or after meals.
You should consult your doctor about the possibility of using traditional medicine. Some ingredients may be contraindicated in a particular case. Plant materials may cause individual intolerance.
Lifestyle
A person diagnosed with essential hypertension needs to change his lifestyle. A prerequisite is giving up bad habits. Smoking and alcohol should be avoided completely.
You need to include more plant foods in your diet. The amount of animal fats should be reduced. The diet should contain sufficient amounts of calcium and potassium. These microelements are contained in dairy products, grains, vegetables and fruits. The use of table salt should be limited - no more than 5 grams per day.
If you are overweight, it is necessary to normalize it. Moderate physical activity is required. If it is not possible to play sports, then you need to walk more. You should walk 10 thousand steps a day.
It is important to normalize your daily routine. An optimal combination and sequence of sleep, work and intermediate rest is necessary.
Diagnosis of hypertension
The diagnosis of essential hypertension is closely related to repeated blood pressure measurements. It is advisable to carry out 24-hour monitoring. However, due to the large number of hypertensive patients, it is not possible to provide an extensive specialized examination to each patient. The main diagnostic methods for high blood pressure are:
- anamnesis (family),
- gynecological examination,
- study of pulse in large vessels,
- measuring blood pressure in different positions (sitting, standing, lying down),
- measuring pressure in the lower extremities,
- Analysis of urine,
- blood biochemistry (study of potassium, glucose, cholesterol levels),
- ECG,
- fundus examination.
Important! In diagnosing high blood pressure, it is advisable to perform a chest x-ray, study the level of uric acid in the serum and protein in the urine.
Classification
There are three classifications of essential hypertension.
It is divided into forms:
- benign - the pathology manifests itself rarely and easily recedes under the influence of medications, most of the time the patient feels normal;
- malignant - the pathology manifests itself sharply and suddenly, the pressure rises to very high levels and is not reduced by medications, there are suspicions of damage to internal organs.
According to the difference in the level of measured pressure, namely systolic (“upper”) and diastolic (“lower”):
| Degree | Systolic pressure | Diastolic pressure |
| 1st degree | from 140 to 159 | from 90 to 99 |
| 2nd degree | from 160 to 179 | from 100 to 109 |
| 3rd degree | from 180 and more | from 110 and more |
There is also a classification that distinguishes the stages of the disease according to the effect of increased pressure on internal organs (the so-called target organs: brain, heart, kidneys, blood vessels):
- Stage 1 - there are no changes in target organs;
- Stage 2 - changes appear without affecting functionality. At this stage, left ventricular hypertrophy, atherosclerotic plaques, and narrowing of the retinal arteries may appear.
- Stage 3 - functionality is impaired. Cardiac circulatory disorders, kidney disease, aneurysms, strokes, heart attacks, etc. may occur.
Risk factors for target organ damage in the first and second stages may include:
- age, gender and hereditary predisposition;
- wrong lifestyle;
- diabetes mellitus and high cholesterol;
- impaired glucose tolerance;
- obesity and physical inactivity;
- increase in fibrinogen.
Possible treatment options
Treatment of EG should be aimed at reducing the likelihood of vascular and cardiac pathologies, the development of complications, and reducing mortality.
With primary EG, drug treatment is not required; it is enough to adjust your lifestyle.
Therapy without drugs
Therapy without medications includes preventive measures aimed at following the rules (you can read more about options for treating hypertension without pills here):
- exclusion from the diet of polyunsaturated fats, which lead to the creation of plaques in blood vessels;
- limiting salt in the diet to 5 grams per day;
- meals up to 6 times a day, in small portions, to prevent overeating;
- drinking at least 2 liters of water per day;
- a balanced diet, with the addition of vegetables, fruits, lean meat;
- eliminating bad habits;
- increasing night sleep to 8 hours;
- ensuring emotional calm, without stress and nervous strain, meditation, yoga, and auto-training are recommended;
- moderate physical activity with adaptation to health status;
- daily walks in any weather outdoors;
- It is worth reducing noise and vibration processes associated with types of work activity.
Drug therapy
The following drugs are used for drug treatment:
- Diuretics that have a beneficial effect on the kidneys and stabilize their function: furosemide, idapamide, dichlothiazide, veroshpiron;
- ACE inhibitors, which reduce the risk of heart attack and stroke, protect the kidneys and blood vessels: captopril, enalapril, lisinopril, fozonopril, perindopril;
- Blockers (sartans) of angiotensin-2 receptors (sometimes prescribed for intolerance to ACE inhibitors), treat the disease, normalize blood pressure: aprovel, candesartan, converium, teveten, micardis, losartan;
- Beta blockers that have a beneficial effect on the cardiovascular system, helping with angina pectoris, severe heart failure, heart rhythm pathologies, as well as people who have had a heart attack: nebivolol (nebicard), Dilatrend, bisoprolol, propranolol, metoprolol;
- Calcium channel blockers (calcium antagonists) are indicated when hypertension is combined with heart rhythm problems, chronic kidney disease, coronary heart disease: nifediline, lerkamen, amlodipine, felodipine;
- Drugs that have a sedative effect, reducing the level of excitement of the nervous system: infusion of valerian, motherwort, Corvalol, diazepam;
- 2nd line medications that also reduce high blood pressure, but have more side effects: physiotens, clonidine, methyldopa, coenzyme Q10.
- Combined drugs consisting of several (2-3) active ingredients from different classes that lower blood pressure using different methods: tonorma, triampur, Enap-n, captopres, vazar-n, liprazide, bi-prestarium, Zia.
https://youtu.be/UFObrdKnO5w
Main reasons
The complexity of the pathology is that it is difficult to diagnose in the initial stages. This occurs due to existing problems in the functioning of the heart and blood vessels.
Causes of increased pressure in primary hypertension:
- Consuming a lot of salt. Its amount in a volume of more than 5.5 g during the day has a negative effect on the condition of the body. Excess fluid accumulates in it, as a result the blood vessels narrow and blood pressure rises.
- Heredity. If you have relatives who already suffer from high blood pressure, you should be more careful about your health. This will prevent the development of the disease in time.
- Arterial pathology. A problem with blood vessels, their deformation, low elasticity leads to the fact that blood flow is disrupted. This is reflected in the level of indicators on the tonometer.
- History of diabetes mellitus. The level of glucose in the blood is regulated by the hormone insulin, which allows it to enter the body's cells and has a beneficial effect on the functioning of blood vessels. If this process is disrupted, diabetes mellitus develops, and high blood pressure inevitably appears.
- Excess body weight. Excess weight is a problem that threatens swelling, problems in the functioning of the heart and arteries. Muscle tone decreases, blood vessels become clogged, and blood pressure increases.
- Age. Over the years, blood vessels wear out, which leads to disruption of the circulatory system. As a result, the pressure begins to rise.
The situation can be aggravated by:
- smoking, alcohol abuse;
- poor nutrition;
- stress, anxiety;
- sedentary lifestyle;
- chronic kidney disease, inflammatory processes.
Complications such as increased blood pressure can be avoided if these factors are excluded.
If you do not adjust your lifestyle and do not take care of your health, then over time large arteries are affected, and more serious pathologies may develop.