Etiology of the disease
Among doctors, cerebral angioma is considered to be a congenital disease or hereditary pathology. However, doctors identify a number of reasons that can provoke the onset of the disease:
- Open and closed skull injuries;
- Brain infections;
- Pathological changes in the vascular system;
- Abnormal development of internal organs;
- Suppressed immunity;
- Pregnancy with a complicated history.
Angioma can present as single or multiple lesions. Vascular tumors occur in any area of the brain.
Most often, benign angioma formation is observed in the cerebellum, frontal, temporal and parietal lobes.
Types of neoplasms are classified according to several parameters. One of the ways of ordering is morphological. So angiomas are divided into:
- Capillary, which are formed from networks of microvasculature vessels.
- Venous are formed from a tangle of venules, which form the common efferent duct.
- Cavernous include a tangle of small pathological vessels of any type. Includes many cavities that are filled with blood and cerebrospinal fluid. The cavities are separated from each other by tissue membranes or trabeculae.
The second sign is the location of the tumor in the cranial cavity. Depending on the topography, the clinical manifestations of the disease change significantly. Classification by place of education:
- Frontal lobe. The changes mainly concern behavioral problems, depression, and emotional disturbances.
- Crown area. In this case, problems arise in the gastrointestinal tract, and problems with sensations may appear.
- If the disease affects the cerebellum, the functioning of the cardiovascular system is disrupted, and problems with lung function and breathing are possible. Coordination of movements is necessarily impaired.
- Right hemisphere. The pathology affects a person’s cognitive and speech functions. There is a problem with dragging out words.
- Left hemisphere. Tissue hypoxia followed by paralysis is observed.
After the appearance of the tumor, rapid tumor growth occurs. Which leads to increased intracranial pressure and leads to stroke and death.
Venous angioma
This disease is a vascular tumor that forms from newly formed cells of blood vessels or lymph nodes. Moreover, this type of pathology is called lymphangioma. Venous-type angiomas are the most common formations associated with changes in the structures of blood vessels. Up to 60% of cerebrovascular malformations are statistically venous angiomas.
According to topography, venous angioma can be:
- In the right frontal lobe. Which significantly affects a person’s performance.
- In the left frontal lobe. Affects the supply of tissue to organs.
- Vascular malformation of the right parietal lobe. This leads to problems with the digestive organs.
- In the cerebellum.
- In the hemispheres of the brain.
Any of the types poses a serious danger to a person’s future performance and life. If the patient is exposed to physical or psycho-emotional stress, the walls may rupture. The consequences depend on the speed of first aid.
Cavernous angioma
Cavernous angioma is the most dangerous among all types of disease. It is a collection of blood vessels in a pathological state. It can be located anywhere in the central nervous system, including the spinal cord. Other names for the pathology: cavernoma, cerebral cavernous malformation or cavernous type hemangioma.
The symptoms of the disease depend entirely on its location in the brain. Thus, cavernous angioma of the left temporal lobe impairs memory, deteriorates vision, and may cause problems with oculomotor function. Lesions in other parts lead to epileptic seizures, hemorrhages and migraines.
Capillary angioma
This morphological change in the vessels of the brain, in addition to veins and arteries, can also affect the microvasculature. At the same time, the smallest venules and arterioles begin to increase in size. They are difficult to find during examinations and practically do not cause any inconvenience to the patient. No transformation into malignant tumors is observed.
Classification of angiomas is based on various characteristics. Depending on the type of vessels, hemangiomas (tumors of blood vessels) and lymphangiomas (tumors of lymphatic vessels) are distinguished.
Based on histological characteristics, they are distinguished:
- Monomorphic angiomas are formations originating from the same type of cells of the vascular wall of arteries/veins (hemangiopericytomas, leiomyomas, hemangioendotheliomas).
- Polymorphic angiomas are formations that combine different cells of the wall of an artery or vein.
Based on the type of tumor structure, there are:
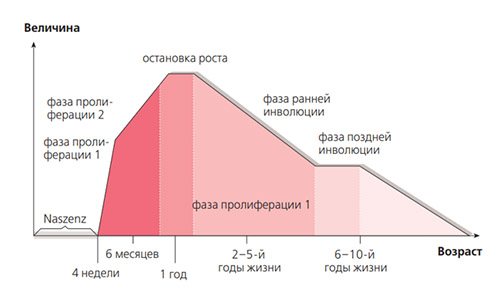
- Simple (capillary) hemangioma - is formed as a result of the proliferation of endothelial cells of newly formed small venous/arterial vessels and capillaries. The predominant localization is the skin and mucous membranes of any part of the body. Arterial ones appear as a bright red spot, and venous ones as a bluish-purple spot of various sizes. Forms a wrinkled papule that rises above the surface of the skin.
- Cavernous (cavernous) hemangioma - formed in dilated blood vessels, consists of wide spongy cavities that are filled with blood and its decay products. Leads to slower blood flow. The predominant localization is inside organs (brain, liver, eyes). Externally, it is a knot with a lumpy surface of a soft-elastic consistency of a purplish-bluish tint.
- Branched angioma is a plexus of dilated tortuous capillary trunks. The predominant localization is the skin of the face.
- Combined hemangiomas are a combination of simple and cavernous forms.
- Cystic angioma - develops mainly in the intestinal mesentery and on the neck, presented in the form of elastic cysts.
- Bacillary angiomatosis is formed as a result of infection with bacteria of the genus Bartonella. The morphological basis of the manifestations of bartonellosis on the skin is the abnormal proliferation of endothelial cells protruding into the lumen of superficially located capillary vessels with the development of skin angiomatosis in any part of the body.
- Lymphangioma is a relatively rare type of angiomas. There is a simple form, which consists of widened tissue gaps filled with lymph and lined with endothelium. They look like flat, colorless thickenings in the muscles of the lips and tongue, painless on palpation. The cavernous form is a multi-chamber cavity formed by lymphatic vessels and having thick walls of muscle and fibrous tissue. Visually noticeable in the form of a swelling without clear boundaries, reddish-yellowish in color, localized on the lips and cheeks. Cystic lymphangiomas are formed according to the type of chylous cysts. They are found mainly in the retroperitoneal tissue, in the intestinal mesentery, neck area, and groin. When a secondary infection occurs, they can cause prolonged lymphorrhea.
According to their shape, angiomas are classified as flat, sickle-shaped, nodular, or stellate.
Medicines for angioma

You will immediately have to disappoint those respondents who are trying to beg the doctor for some kind of pill that will allow them to get rid of the problem, being afraid to decide on surgical intervention. But to date, a panacea for the disease in question in the form of tablets or injections has not yet been found. Only if, for some reason, surgical treatment of angiomas is not permissible, then the doctor has no choice but to prescribe medications belonging to the pharmacological group of hormonal drugs in the treatment protocol.
Mostly in such a situation, a specialist prescribes prednisolone. Instead, other drugs - its analogues - may be prescribed. For example, medopred, prednisolone 5 mg yenapharm, prednihexal, decortin, salt - decortin, inflanefran, novo-prednisolone, prednisol, prednisolone acetate, sherizolon and others.
The glucocorticosteroid prednisolone is taken in a dosage that is calculated based on the patient’s body weight and height. Taking this drug leads to blocking the growth of the tumor and provokes drying out of the pathological vascular branching.
The starting daily dose is prescribed in the range of 20 - 30 mg. This dosage is gradually reduced. The schedule for taking and reducing the dose of the drug is prescribed by the attending physician. The medication is taken under his own supervision.
For small patients, this daily dosage is calculated according to the formula - 1 - 2 mg per kilogram of the baby’s weight. The resulting amount of the drug is distributed into four to six doses.
The only contraindication for the use of this drug in the treatment protocol is increased intolerance by the body to prednisolone or one of the components of its composition.
Doctors also recommend taking a larger dosage of the drug in the first half of the day, and a smaller one in the afternoon.
Some protocols for such treatment also include cytostatic drugs, which are designed to inhibit or suppress the processes of pathological cell division and growth of connective tissues. This could be one of these drugs: ralitrexed, busulfan, methotrexate, thiotepa, docetaxel, mitomycin, bleomycin, vincristine, fludarabine, gemcitabine, cytarabine, capecitabine, epirubicin, idarubicin, cisplatin, edercolomab, polyestradiol and many others. You just have to remember that it is unacceptable to self-attribute any of these drugs to yourself. This is fraught with negative consequences for the body.
The alkylating agent treosulfan is administered by intravenous infusion over 15 to 30 minutes. The dosage of the drug is indicated at the rate of 8 g per one square meter of the patient’s body area, administered once for three to four weeks.
Contraindications for the administration of this drug include inhibition of bone marrow hematopoiesis, hypersensitivity to the components of treosulfan (including treosulfan), pregnancy and breastfeeding of the newborn.
This pharmacological agent belongs to the combined vitamin preparations. The main components of the medicine are vitamins C (ascorbic acid) and P (rutin). Therefore, as a vitamin stimulator of the body, ascorutin can be very useful for angioma.

The recommended dosage for adult patients is one tablet three times a day. This stimulation regimen will boost the patient’s immunity, helping the body more actively fight the problem.
As a preventive measure, ascorutin can be taken in a dose of one tablet twice a day. The duration of the treatment course is three to four weeks. The duration of treatment is prescribed by the doctor depending on the nature and severity of the disease.
Contraindications for taking this drug include the patient’s individual intolerance to vitamin C or P, the first trimester of pregnancy, the patient’s history of diabetes mellitus, severe urolithiasis, thrombophlebitis, gout, a high level of blood clotting and the age of a small patient under three years.
[5], [6], [7], [8], [9]
Timolol for angioma
Beta-blockers are prescribed by a doctor if it is necessary to block beta-adrenergic receptors in the patient’s body. If the pathology in question affects the eye area, then in the treatment of this disease a drug such as timolol, which is one of the representatives of beta-blockers, can be used.
The drops are applied in a dosage of one drop once or twice a day into the problematic eye. Initially, they begin to use the drug with a concentration of 0.25%. If the expected result is not observed, then the concentration of the drug is increased to 0.5%.
Contraindications for its use include:
- Individual intolerance to one or more components of the composition.
- History of bronchial asthma.
- Obstructive pathology of lung tissue.
- Acute or chronic form of cardiac dysfunction.
- Cardiogenic shock.
- Decreased heart rate.
- Sick sinus syndrome.
- Dystrophy of the ocular cornea.
- Tendency to allergic reactions.
- Breastfeeding period.
- The first years of a baby's life.
A derivative routine related to the treatment of chronic venous insufficiency is troxevasin. An angioprotective drug primarily affects capillaries and veins. It reduces pore parameters in the spaces of endothelial cells due to the restructuring of the fibrous matrix. Inhibits aggregation, shows anti-inflammatory characteristics and activates the deformability of red blood cells.
This medicine is allowed for use in case of diagnosing angioma.
It is taken orally, two capsules before meals, once or one capsule twice a day. If therapeutic effectiveness is not observed, the dosage can be increased, but all these prescriptions can only be made by a specialist. If the drug is prescribed in gel form, then it is applied and gently rubbed into the sore spot twice a day: after waking up and before going to bed.
You just need to make sure that Troxevasin gel does not get into the eyes, damaged areas of the skin, or mucous membranes.
Contraindications for taking this drug include the patient’s individual intolerance to the component composition of the drug (including rutosides), the first trimester of pregnancy, ulcerative and erosive lesions of the gastric and duodenal mucosa, the acute phase of chronic gastritis, and severe renal failure.
What is venous angioma, how is it formed?
The blood vessels of the brain, with the participation of lymphatic tissue, can create “tangles” that impede blood flow and nutrition of brain cells. For example, blood from an artery immediately enters a vein, as a result, the tissues do not receive oxygen. Such vascular formations are called venous angiomas; they can be malignant or benign. Their main danger lies in compression of brain structures, possible rupture of vessel walls and hemorrhagic stroke.
Hemorrhage can occur due to the thinness of the tumor walls with a slight increase in pressure, trauma, or emotional stress. If a person did not know about the presence of such structures, then he can only rely on the experience of doctors in making an accurate diagnosis in case of sudden manifestations of the disease (paralysis, significant sensory disturbances, stroke).
With a small size, a brain angioma may not show itself in any way throughout life, which explains the difficulty of diagnosis.
Angiomas grow slowly, from the period of intrauterine development of a person. They are detected during unscheduled examinations, or suspicions of the presence of neoplasms of various natures in the brain.
Placement of the neoplasm:
- skin surface;
- internal organs;
- brain.
Venous angioma can grow on the skin or in internal organs or the brain, causing painful symptoms.
- venous angioma of the right frontal lobe of the brain;
- angioma of the frontal lobe of the left hemisphere of the brain;
- venous angioma of the right temporal lobe;
- angioma of the left temporal lobe;
- angioma of the parietal lobe;
- venous angioma of the left hemisphere of the cerebellum;
- angioma of the right cerebellar hemisphere;
- angioma of the basal ganglia.
For a long time, angioma is asymptomatic in organisms. It manifests itself over time and intensifies as the disease progresses. The most noticeable symptoms of this disease are localized in the brain. General symptoms of the disease:
- headache;
- speech problems;
- dizziness;
- nausea;
- fainting;
- lack of coordination;
- vomit;
- noise;
- blurred vision;
- change in tastes;
- convulsions;
- pathologies of the heart and blood;
- partial paralysis;
- heaviness;
- dullness of mental activity;
- epilepsy.
Venous angioma of the brain can cause pain, convulsions, loss of coordination, and deterioration in the functioning of the senses.
Laser removal of angioma
Of course, it is easier and more effective to combat any pathology during the period of its inception and development. If angioma is detected early, the number of procedures is minimal. Sometimes just one is enough to make the problem go away. One of the most effective and innovative methods for relieving the problem is laser removal of angioma.
If the case is advanced and the appearance of radial blood processes is observed, the situation becomes more complicated. With this clinical picture, excision of the central blood supply arteriole does not give the expected result. Since in this case the efferent radial capillaries will not be empty, due to the fact that they are also nourished thanks to numerous collateral connections with the tissues of the skin.
In this case, to remove the star-shaped neoplasm, doctors mainly resort to the laser method of eliminating the angioma. In this case, the patient should prepare to undergo a number of procedures. And the more advanced the case, the more there will be.

The main advantage of this treatment method:
- Minimal injury.
- Highly effective results.
- The ability to minimize the extent of damage to healthy tissue.
- After the procedure, a small scar is formed, which resolves on its own over time.
- The procedure itself is carried out quite quickly, in a matter of minutes.
- This “operation” is not very painful, but if the patient wishes, local anesthesia can be used.
- For some time, the spot formed at the site of the operation will differ in color, since during the procedure the melanin cells in this area are destroyed, but over time this defect disappears and pigmentation is restored.
- The number of complications and relapses is minimal.
Recently, this technique has been given increasing preference in solving the problem considered in this article.
After any surgical intervention, each patient undergoes a rehabilitation (recovery period). Moreover, after removing angiomas with a laser, this period of time is minimal. The process of regeneration of skin cells occurs quite actively and quickly.
Initially, the cauterization site will be covered with a crust. It will fall off quickly enough, revealing an already healed wound. Mostly, if the case is not advanced, removal occurs in one step, but if the case is complex, the patient may have to undergo staged removal.
Immediately after the operation, the patient receives a number of recommendations that should be followed over the next few days (from five to seven days).
- The cauterization site should be protected from getting wet.
- You should not scratch the wound.
- Do not allow the crust that forms at the site of the wound to break; at some point it will come off on its own.
- Avoid prolonged exposure to sunlight.
As practice in recent years has shown, laser removal of angioma is the most effective and least traumatic method of treatment in modern cosmetic dermatology.
But it is worth remembering that only a specialist is able to assess the situation and choose the most appropriate method for getting rid of the tumor for a given clinical picture.
Causes of the disease
According to statistics, venous angioma occurs during the natal period of development. That is, in the womb. Only 1 in 20 patients becomes ill after birth. The exact etiology of the disease does not currently exist. However, factors that contribute to the disease have been identified:
- Disturbances or morphological changes in the natal period of development of the fetal cardiovascular system due to maternal health problems, which include: infectious diseases, unhealthy lifestyle, and others. Also, the disease appears due to a lack of vitamins.
- Mechanical damage to the head, especially when passing through the birth canal.
- Diseases of an infectious nature that lead to complications before the age of 6 years.
- The appearance of pathological processes or conditions of part of the visceral organs, especially the liver, gonads, and organs of the gastrointestinal tract. Such problems are often observed in cirrhosis.
If the disease was acquired during intrauterine development, then formation is observed in the first 3 months of development.
Cavernous angioma is a hereditary disease that is transmitted in autosomes under the condition of dominance. The probability of disease reaches 50%. The neoplasm can develop in a single number, with subsequent development throughout life. In addition to congenital cavernous pathologies, there are also sporadic ones that arise due to external factors. The risk group includes all people with disorders in the functioning of the cardiovascular system, as well as those who are often exposed to high levels of stress.
Causes of angioma
The etiology of angiomas is constantly being studied as the disease becomes more common. There are several possible ways for this type of formation to appear in the body:
- congenital defect (hereditary factor), in which the epithelial tissue of the vascular walls grows uncontrollably;
- mechanical injury;
- diseases in which demyelination of the membranes of the brain occurs;
- previous infectious brain disease;
- constant contact with chemicals;
- other types of cancer that have migrated to the brain.
Uncontrolled division of vascular cells (mutation) can stop or accelerate under the influence of external factors (hormonal changes, chemical exposure).
Consequently, symptoms can appear at any age, but it is worth paying special attention to neurological complaints during transitional periods (puberty, menopausal disorders, pregnancy).
Degeneration into a malignant tumor occurs if there has been prolonged contact with a negative environment, a hormonal imbalance has occurred, or malignant neoplasms have appeared in another organ.
D18 is a code according to ICD 10, which means any type of angioma by location and origin.
For successful treatment, it makes sense to distinguish between venous and cavernous angiomas. The first type occurs in the veins, as an expansion of one or more venous vessels. The pressure in the veins is low and the walls are quite strong, so the risk of rupture is low.
The cavernous type includes in its structure not only blood vessels, but also small cavities of the brain. The tumor completely fills the caverns, and its boundaries are thin membranes. With this type of disease, there remains a high risk of hemorrhagic stroke with profuse hemorrhage.
For treatment, the location of the tumor, the type of benign or malignant, and the activity of changes in size (constantly growing or has clear, unchanged boundaries) are important.
Reliable causes of angiomas have not been found to date. However, according to existing data, they are congenital in nature and are associated with dysregulation of the process of angiogenesis in the fetus at an early stage of pregnancy (5–8 weeks) and are caused by the loss of signals that inhibit angiogenesis or the predominance of signals that inhibit apoptosis or promote angiogenesis.
It is assumed that factors such as severe constant stress, extensive and frequent injuries, alcohol consumption during pregnancy, and taking certain medications can affect the growth of angioma.
What causes hemorrhage?
Increasing in size and putting pressure on the brain matter, the neoplasm can cause hemorrhage in the brain, which often leads to death. Various factors can provoke hemorrhage:
- significant increase in angioma;
- injuries, bruises;
- compression of the medulla;
- deficiency of oxygen and nutrients in the brain;
- arterial hypertension;
- head injuries, even minor bruises;
- sudden bends and turns of the head;
- significant physical and emotional stress;
- childbirth;
- jumping;
- stress.
Localization and symptoms
Like all diseases of the central nervous system, the topography of the pathological formation directly affects the degree of damage and clinical manifestations. Since the brain is the most energy-dependent organ, the level of vascularization is quite high. Therefore, there are several main topographic areas in which angioma can develop.
There are also general symptoms. Manifestations do not begin to develop immediately after the formation of the venous or capillary plexus. However, as linear dimensions increase, pressure on brain structures increases, which leads to dysfunction.
The most common signs are:
- Severe headaches.
- Constant feeling of discomfort.
- Noise in ears.
- Speech disorders.
- Memory problems.
Local symptoms depend on the topography of the tumor.
Frontal lobes
This part of the brain is responsible for higher cognitive activity, such as reactions such as decision making, responsibility and other processes. A person with angioma of the frontal lobe of the brain, regardless of whether it is on the right or left, has problems with logical and analytical thinking and decision making.

If complications develop, changes in character, lack of responsibility for actions and the inability to solve some everyday problems are possible. A person's ability to perform work suffers. Possible depressive syndrome. Sensitivity to temperature decreases.
Parietal lobes
If these areas are affected, the patient will experience:
- decreased sensitivity to pain;
- lack of sensation of temperature;
- problems with touch perception.
The disease can lead to the inability to navigate through a read text. This is direct evidence of damage to the speech center.
Cerebellum
The organ that is responsible for correcting movements is divided into two lobes. If the cerebellar venous angioma is located in the left hemisphere, then the following symptoms may appear:
- impaired coordination of movements;
- gait changes;
- nystagmus;
- frequent dizziness;
- problems with simultaneous movement of limbs.
Damage to the right hemisphere (right hemisphere of the cerebellum) is characterized by:
- tremor of the limbs;
- decreased speed of movement and speech;
- changes in handwriting.
Temporal lobes
The disease in this localization is characterized by an asymptomatic course. In later stages of development, the following signs may appear:
- seizures;
- psychomotor skills;
- speech dysfunction;
- disturbances of perception and hallucinations.
Occipital lobes
If the tumor is located in the posterior structures of the brain, problems with visual fields may occur. Seizures of epilepsy are observed, which are preceded by a flash of bright light in the eyes.
https://www.youtube.com/watch?v=Le6T-EEGTr4
Neurological symptoms that appear over a long period of time and cannot be relieved “help” in making a diagnosis.
A patient with an angioma periodically experiences headaches, non-food nausea, sensory disturbances, and fainting. Depending on which part of the brain the neoplasm is localized and what its nature is (veins, capillaries, or caverns are involved), specific symptoms will appear:
- Venous angioma of the occipital lobe:
- spasmodic sensations in the muscles of the back of the head;
- visual hallucinations (the appearance of long-term images and short-term sparkling).
- Venous angioma of the right temporal lobe:
- Damage to the left temporal lobe, just like the right, disrupts speech and the ability to perceive it. Strong emotional surges are added for no apparent external reasons.
- Venous angioma of the right parietal lobe:
- lack of “right-left” distinction when exposed to stimuli;
- unconscious paralysis.
- Damage to the left parietal lobe leads to loss of orientation not relative to one’s body, but in space (inability to determine distances or read a map).
- Venous angioma of the right frontal lobe:
- emotional instability;
- inability to control your actions;
- euphoric mood;
- loss of the ability to competently construct sentences of any length.
- With a tumor of the left frontal lobe, the patient cannot move on to the verbal formulation of thoughts (he thinks, but cannot speak), and has little control over his own behavior.
In general, capillary angiomas can occur in any part of the brain, and venous angiomas mainly in the cerebellum, the white matter of the brain.
The prognosis depends on the size of the tumor, its benign or malignant quality, and location. Most formations are treatable.
Possible complications
Due to the growth of venous angioma of the right hemisphere of the cerebellum, a rupture of the wall of the damaged vessel may occur, which will provoke the opening of intracranial hemorrhage with all the ensuing consequences: paralysis on the right side, impaired facial expressions on the side of the damage and other disorders of the motor function of the body.
Therefore, if a patient has been diagnosed with a similar vascular pathology, then he should be as attentive as possible to his health. Namely, it is necessary to eliminate stress from life, prevent an increase in blood pressure, reduce physical stress on the body and not make sudden turns and tilts of the head.
The growth of angioma leads to compression of the tissues of the brain or spinal cord. The following complications are possible:
- deterioration/loss of hearing and vision;
- headache;
- vertebrogenic pain syndrome;
- epileptic seizures;
- increased blood pressure;
- impaired coordination of movements;
- deterioration of speech;
- paresis;
- rupture of the vessel walls and hemorrhage into the surrounding tissue.
The prognosis for cerebral venous angioma is usually favorable. Normal life does not suffer from this. Especially if the education is single.
The prognosis may be affected by:
- other problems with the cardiovascular system;
- arterial hypertension or hypertension;
- topography of the neoplasm;
- patient's work.
Meningioma
Directory of codes of all-Russian classifiers. ClassInform - all codes of all-Russian classifiers. Benign neoplasms. Benign neoplasm of the brain and other parts of the central nervous system. Excluded: angioma D of the brain above the tentorium. The brain is under the tentorium.
Cavernous angiomas of the brain Cavernomas of the brain are congenital pathological vascular cavities in the substance of the brain, internally separated by trabeculae and filled with blood, belonging to the class of hemangiomas. Clinically, brain cavernomas are manifested by the occurrence of epileptic seizures when localized in the cerebral hemispheres or hemorrhages into the substance of the brain.
Diagnostic methods
Incidental detection of angioma occurs when other diseases are detected. The patient complains when the node reaches a large size. For brain examination, the following is prescribed:
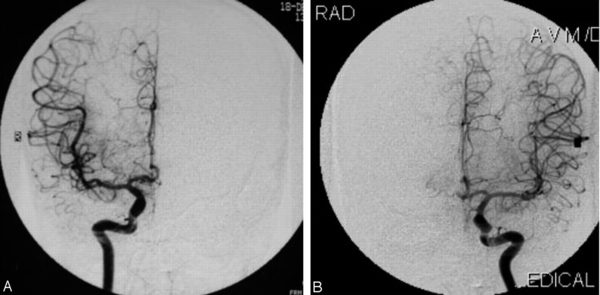
- Magnetic resonance imaging. The method is aimed at studying the condition of soft tissues. The most accurate picture of the organ and blood vessels is obtained, which allows you to draw up a treatment plan. MRI does not expose the patient to radiation.
- Carrying out computed tomography with the introduction of a contrast agent is based on transillumination of the organ using radiation. The contrast agent is administered at the discretion of the physician. CT and MRI scan the organ layer by layer and detect the slightest changes and neoplasms in tissues and blood vessels.
- Angiography with intra-arterial contrast allows you to determine the location of the tumor, its type and size.
Definition of angioma in the brain
To avoid serious consequences, it is important to diagnose angioma on time. To do this, you need to contact specialized specialists:
- neurosurgeon;
- vascular surgeon;
- phlebologist;
- angiosurgeon;
- dermatologist;
- homeopath;
- dermatocosmetologist;
- oncologist.
Diagnosis of angioma, depending on its location, will include tests and hardware examination.
- CT;
- MRI;
- angiography;
- radiography;
- Ultrasound;
- spinal tap.
An appeal to a neurologist with complaints of systemic headaches, nausea, sensory disturbances is the reason for MRI and contrast angiography.
Sometimes we are talking about a neoplasm that is significant in size and significantly affects the performance of the brain. A tumor of this type can be detected in the middle and late stages by performing a non-routine CT or MRI of the head with contrast.
Modern diagnostic methods make it possible to accurately determine the location, size of the tumor, and type of vascular formation.
Venous angioma on MRI
Venous angioma of the right frontal lobe is indicated in the photo by an arrow
Treatment
There are cases when angioma resolves on its own. But often it is necessary to resort to radical methods of treatment, since other methods are ineffective. For example, medications can help relieve painful symptoms, but they cannot untangle the vascular tangle. For this, patients are prescribed painkillers, antihypertensives, and sedatives.
The operation is not performed when diagnosing a small tumor that does not threaten human life, as well as for people with venous angioma, which is characterized by a low risk of choroid plexus rupture.
If the tumor is large and rapidly growing, the following is carried out:
- Traditional way. Removal using a method in which the choroid plexuses are excised.
- Radiosurgical method. Removal of the tumor by blocking the vessels that formed the tangle. In this case, blood will not enter their cavity.
- Sclerotherapy . This method involves blocking the vessels using special catheters through which sclerosing drugs are administered.
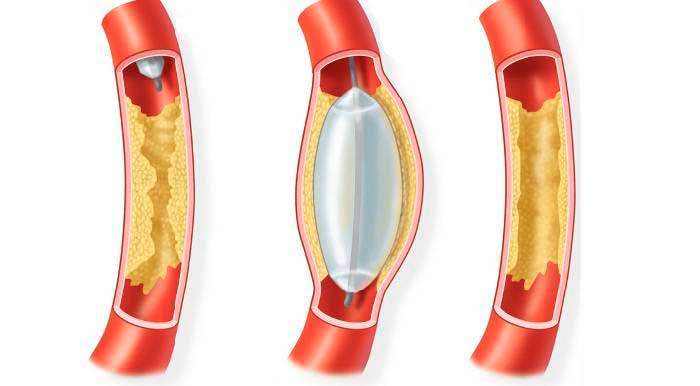
- Angioplasty . Allows you to restore the vascular lumen by reconstructing veins and arteries. To restore cerebral circulation and expand the lumen, special metal meshes and balloons are implanted into the affected arteries.
- Liquid embolization . Involves the introduction of a substance into the problem vessels, disconnecting them from the general blood flow. Over time, the damaged vessel is replaced by connective tissue.
- Embolization . This method of treatment allows you to clog and “disconnect” blood vessels from the general circulation by introducing a special spiral.
The choice of one or another method of operation depends on the clinical manifestations, location, size of the tumor, age, and general condition of the patient. Modern specialists try to use minimally invasive treatment methods, as they minimally injure surrounding healthy tissue and significantly reduce the rehabilitation period. Radiosurgical methods using a Gamma Knife or Cyber Knife destroy pathology by exposing it to radio wave beams of radiation.
Health care
Depending on the type of venous angioma, treatment may consist of different blocks. For a benign tumor, the complex of medical care includes
Surgical methods are used if the tumor is on the surface of the brain in a safe zone. These include all tumors on the surface of the brain, where access is not obstructed by adjacent tissues. Otherwise, they try to gain access to the tumor through the vessels themselves, since the risk of injury to the brain itself is less than with full-fledged invasion.
During the minimally invasive procedure, substances are introduced into the formation that block the flow of blood into pathologically growing vessels. This creates a new path for blood flow, bypassing the problematic blocked area.
The malignant nature of the tumor means unambiguous surgical excision and chemotherapy of a separate area of the brain.